Abstract
By manufacturing a single-particle system in two particulate forms (i.e., micrometer size and nanometer size), we have designed a bacterial vaccine form that exhibits improved efficacy of immunization. Microstructural properties are adapted to alter dispersive and aerosol properties independently. Dried “nanomicroparticle” vaccines possess two axes of nanoscale dimensions and a third axis of micrometer dimension; the last one permits effective micrometer-like physical dispersion, and the former provides alignment of the principal nanodimension particle axes with the direction of airflow. Particles formed with this combination of nano- and micrometer-scale dimensions possess a greater ability to aerosolize than particles of standard spherical isotropic shape and of similar geometric diameter. Here, we demonstrate effective application of this biomaterial by using the live attenuated tuberculosis vaccine bacille Calmette–Guérin (BCG). Prepared as a spray-dried nanomicroparticle aerosol, BCG vaccine exhibited high-efficiency delivery and peripheral lung targeting capacity from a low-cost and technically simple delivery system. Aerosol delivery of the BCG nanomicroparticle to normal guinea pigs subsequently challenged with virulent Mycobacterium tuberculosis significantly reduced bacterial burden and lung pathology both relative to untreated animals and to control animals immunized with the standard parenteral BCG.
Keywords: bacillus Calmette–Guérin, inhaled particles, live-attenuated vaccines, spray drying, tuberculosis
Aerosol vaccination via the lungs targets an epithelium critical to host defense against inhaled pathogens (1), potentially avoids needle injection, and provides an exciting opportunity in the development of a newer and more effective tuberculosis (TB) vaccine. Published studies of inhaled vaccines for measles, influenza, and TB (2) have mostly involved nebulized solutions, a process that necessitates large volumes of water with long administration times; dried forms of vaccines, as formed traditionally by freeze drying and recently by spray drying (15), present an alternative to nebulization but pose risks to the integrity of dried bacteria and produce powders with suboptimal dispersive characteristics. Here, we show that by designing bacterial vaccines via rapid drying we can exploit the natural tendency of dried bacteria to assume elongated shapes and achieve remarkably effective airborne properties that combine the positive attributes of their submicrometer radial axes and micrometer-scale longitudinal axes. We demonstrate vaccine delivery from an inhaler designed for delivery to newborns. Furthermore, we report better TB protection with an aerosol form of bacillus Calmette–Guérin (BCG) than is achievable by standard s.c. and intradermal injection using a low-inoculum, aerosol infection and challenge in the sensitive guinea pig model.
Results
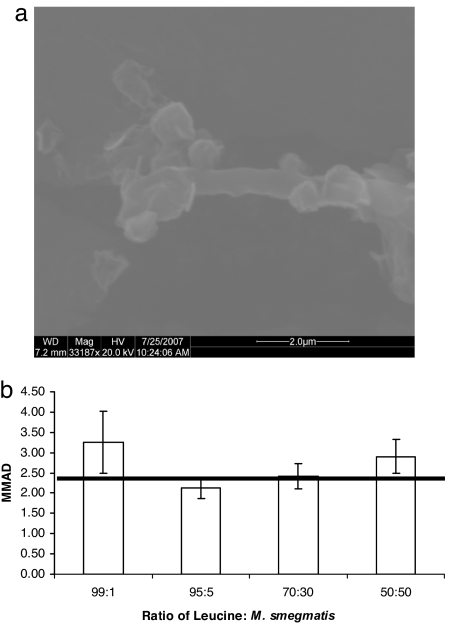
In initial experiments, powders of dry bacteria were prepared by spray drying with a model nonpathogenic Mycobacterium, Mycobacterium smegmatis. We added a second material, the amino acid leucine, in relatively large proportions to diminish bacteria–bacteria physical interactions in the dry-powder state. Visual assessment of the different powders confirmed the existence of individual dried bacteria that form rod-like structures with length ≈1–4 μm and diameter ≈200–400 nm, whereas the leucine particles form sphere-like particles with mean geometric diameter 2.3 ± 1.2 μm as determined by light scattering sizing of a 100% leucine powder. The sphere-like leucine particles act as physical buffers to prevent bacteria–bacteria interactions. The rod-like bacteria particles appear to act as “scavengers” of the smallest leucine particles (see Fig. 1a), and less frequently associated with leucine particles approaching the mean geometric size, i.e., >1 μm.
Fig. 1.
Morphology and aerosol properties of M. smegmatis: l-leucine dry powder. (a) ESEM photograph of 95:5 M. smegmatis:l-leucine powder. The rod-like M. smegmatis appears associated with sphere-like leucine particles. (b) MMAD for various ratios of leucine to M. smegmatis. Horizontal red line indicates geometric size (d50) measured at 2 bar for spray-dried 100% leucine at 2.3 μm.
We evaluated the aerosol properties of the various dry-bacteria powders, as shown in Fig. 1b. The mass-median aerodynamic diameter (MMAD) is smallest for the 95:5 leucine:M. smegmatis powder relative to larger and smaller ratios of leucine to M. smegmatis. Further, as illustrated by the dashed horizontal line in the figure (the mean geometric diameter of the pure leucine powders), the MMAD is statistically identical to the geometrical diameter for the 95:5 (and 70:30) powder, whereas it exceeds the leucine geometric diameter at the larger and smaller leucine:M. smegmatis ratios. This distinction reflects the tendency of airborne agglomerates to increase aerodynamic diameter relative to geometric diameter, a tendency common to most dry-particle aerosol forms (3).
The effectiveness of an inhaler appropriate for newborns in low-income settings was assessed in terms of emitted dose delivery of four different dry bacterial formulations of placebo powders from a prototype device [see supporting information (SI) Appendix]. Results revealed that for all but the lowest leucine:M. smegmatis ratios, emitted dose from the infant inhaler was large, with yields of 99.05 ± 6.01% for the 99% leucine, 92.59 ± 16.73% for the 95% leucine, 85.17 ± 9.23% for the 70% leucine, and only 68.02 ± 6.43% for the 50% leucine.
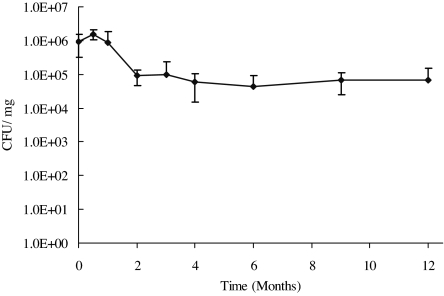
Given these preliminary findings, we designed a TB vaccine dry powder with the standardized live BCG in place of M. smegmatis (95:5 leucine:BCG). We evaluated the physical and biological activity properties of the TB aerosol vaccine over time after a 9-month stability study at refrigerated (4°C) conditions in sealed enclosures. Under refrigerated conditions, the vaccine MMAD remained constant, starting at 2.1 ± 1.2 μm at day 1 and ending at 1.9 ± 1.1 μm at month 9. Similarly, the viability of the bacteria, measured in cfu, remained statistically unchanged, from 4.8 × 105 ± 8.8 × 104 cfu/mg at day 1 to 4.5 × 104 ± 1.2 × 104 cfu/mg at the conclusion of month 9 (Fig. 2).
Fig. 2.
Stability of the 95:5 leucine:BCG powder (cfu/mg) over the 12-month study at 4°C and 20% relative humidity.
As a measure of the ability to induce cell-mediated immunity, the size of tuberculin reactions to purified protein derivative [PPD, 100 tuberculin units (TU)] was compared in guinea pigs immunized with 2 × 106 cfu of BCG by the s.c., intradermal or pulmonary routes (Table 1). At this dose, all animals developed comparable delayed-type hypersensitivity tuberculin reactions; However, animals immunized with 2 × 105 cfu BCG by the pulmonary route exhibited reduced skin reaction size compared with those receiving the same dose by the s.c. route. As expected, no skin reactions were observed in the site of PPD injection in untreated control animals.
Table 1.
Delayed hypersensitivity reactions to 100 TU of PPD in guinea pigs 6 weeks after immunization with the different formulations of BCG by the different routes (average ± SD, n = 6)
| Treatment groups | Route of administration | Dose | Diameter of induration, mm |
|---|---|---|---|
| BCG soln. | s.c. | 2 × 105 cfu | 15.8 ± 3.4 |
| BCG soln. | s.c. | 2 × 106 cfu | 17.0 ± 1.6 |
| BCG part. | s.c. | 2 × 106 cfu | 17.3 ± 1.2 |
| BCG soln. | i.d. | 2 × 106 cfu | 15.8 × 2.9 |
| BCG part. | Pulmonary | 2 × 105 cfu | 10.0 × 2.5* |
| BCG part. | Pulmonary | 2 × 106 cfu | 15.3 ± 3.5 |
| Untreated control | 0 ± 0** |
*, significantly smaller than the untreated control (P < 0.05).
**, significantly smaller than any other treatment (P < 0.05).
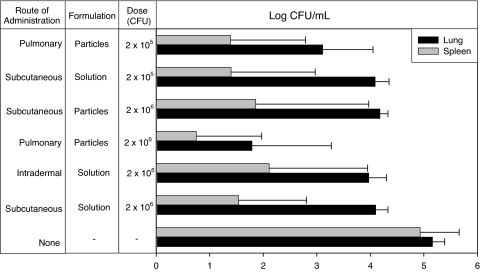
Having demonstrated the immunogenicity of BCG in the aerosol formulation, experiments were undertaken to establish the protective efficacy of the BCG vaccine against challenge of guinea pigs with virulent Mycobacterium tuberculosis. Ten weeks after immunization and 4 weeks after infectious challenge with an aerosolized suspension of M. tuberculosis strain H37Rv (2 × 105 cfu), the bacterial burden in the lungs of immunized animals was, as expected, significantly lower than that of unimmunized controls, regardless of the BCG dose (2 × 105 or 2 × 106 cfu) or the route of administration (s.c. or intradermal) (Fig. 3). In addition, the bacterial burden in the lungs of animals receiving parenteral immunization with BCG was comparable across dose (2 × 105 or 2 × 106 cfu), route of administration (s.c. or intradermal), and formulation (s.c. administration of particles or solution). Significantly, whereas the cfu in spleens were comparable between the aerosol and parenteral BCG immunizations, the bacterial burden in the lungs of animals immunized by the pulmonary route with 2 × 105 cfu of BCG nanoparticles was significantly lower than that of animals immunized by the parenteral route (with either solution or particles). Moreover, the bacterial burden of lungs of animals immunized by the pulmonary route with 2 × 106 cfu of BCG particles was significantly lower than that of animals immunized with 2 × 105 cfu of BCG particles or those immunized by the parenteral route (with either solution or particles). The results of the present studies confirm the findings of our preliminary studies.†† Thus, these results in the highly sensitive guinea pig system to M. tuberculosis infection suggest that pulmonary immunization with this type of stable powder vaccine has significant potential as a candidate delivery system for TB vaccines.
Fig. 3.
Number of viable bacteria per milliliter of tissue homogenate (cfu/ml) at necropsy in lung and spleen tissues after bacterial challenge of animals immunized with the particles or BCG solution by the different routes (average ± SD, n = 6). The ranking of lung bacterial burden in terms of statistical significance is relative to untreated animals: none > s.c. solution 2 × 106 cfu (P < 0.0001) > pulmonary particles 2 × 105 cfu (P = 0.0002) > pulmonary particles 2 × 106 cfu (P = 0.0003), and relative to animals immunized by the s.c. route: s.c. solution 2 × 106 cfu > pulmonary particles 2 × 105 cfu (P = 0.0002) > pulmonary particles 2 × 106 cfu (P = 0.0036). The ranking of spleen bacterial burden in terms of statistical significance is relative to untreated animals: none > s.c. solution 2 × 106 cfu (P = 0.0002) > pulmonary particles 2 × 105 cfu (P < 0.0001) > pulmonary particles 2 × 106 cfu (P < 0.0001), and relative to animals immunized by the s.c. route: s.c. solution 2 × 106 cfu > pulmonary particles 2 × 106 cfu (P < 0.0001).
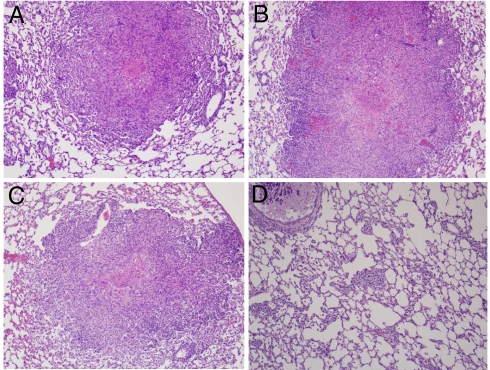
The results of lung bacteriology were mirrored by lung histopathology. The findings after histopathological analysis of lung tissue were comparable among animals immunized with 2 × 106 cfu of BCG by parenteral routes. Less than 5% of the lung tissue in these animals was affected by small to medium granulomas, and <25% of them were affected by minimal to mild necrosis. In contrast, at least 20% of lung tissue in untreated animals was affected by medium-size granulomas, most of them exhibiting mild necrosis. Histopathological analysis also revealed that <1% of the lung tissue in animals immunized by the pulmonary route with 2 × 106 cfu of BCG particles was affected by small granulomas, and none of them exhibited caseous necrosis (Fig. 4). Similarly, in animals immunized with 2 × 105 cfu of BCG, the granulomas in the lungs of those immunized by the pulmonary route did not exhibit caseous necrosis, unlike those immunized by the s.c. route.
Fig. 4.
Lung histopathology after bacterial challenge of animals immunized with the particles or BCG solution by the different routes. (A) Untreated controls. (B–D) Animals immunized with s.c. BCG solution at 2 × 106 cfu (B), s.c. particles at 2 × 106 cfu (C), and insufflated particles at 2 × 106 cfu (D).
A comparable trend was observed in spleen tissue. Although almost 90% of the white pulp in the spleen of untreated animals was affected by medium to large granulomas exhibiting mild caseous necrosis, <10% of the white pulp in the spleens of animals immunized parenterally was affected by small to medium granulomas that exhibited minimal caseous necrosis. Furthermore, in animals immunized with 2 × 106 cfu of BCG particles by the pulmonary route, <1% of the white pulp in the spleen was affected by small granulomas that did not have necrosis, thus confirming the results of bacteriology in demonstrating the effectiveness of this approach in the prevention of TB. These results indicate that pulmonary immunization by BCG nanoparticle aerosols led to reduced lung pathology after virulent M. tuberculosis infection.
Discussion
The idea of mixing spherical and rod-like particles to form an efficient dry-powder aerosol as a basis for an effective inhaled vaccine derives from several decades of aerosol and vaccine research. Early researchers used relatively large “carrier” particles of lactose and other safe inert materials to overcome the adhesive aggregation forces between small micrometer-size drug particles intended for pulmonary delivery (4). These mixtures aimed to enable the excellent aerosolization properties of the small drug particles and the good flow properties of the large particles. In recent years, researchers (5) have improved on the classical carrier powder mixtures [which possess the drawback that the large particles do not aerosolize well (they are intended to fall out in the mouth), and the small drug particles lose lung penetration capacity as a consequence (6)] by designing aerosol powders with a single kind of “porous” or low-density particle drug or vaccine and whose physical characteristics are both “large” (>1–3 μm) and aerodynamically “small” (in the 1- to 3-μm MMAD window ideal for lung deposition). These characteristics lead to a much more efficient aerosol for lung deposition and delivery than the classical carrier powder formulations (6). The large, porous particle design, although a significant improvement over the classical medical aerosol particle design, possesses the practical limitation that particle density can be lowered to only a certain degree, whereas other parameters, including surface morphology, frequently play a significant competitive role. The present work turns to the aerosol science research history of rod-like particles that begins with the theoretical work of Fuchs (3) and Davies (7) and includes subsequent decades of experimental studies (8, 9), including the use of drugs (5, 10) that confirm the unique ability of airborne rods to traverse the air as very small particles while behaving in powder form as larger particles (11, 12), albeit with a significant tendency to aggregation (13, 14). We find that by maintaining a low-weight concentration of bacteria in our powders, leucine can play the role of carrier particle, conferring flow properties associated with the sphere-like leucine particles, but, once airborne, the bacteria travel with the excellent aerosol properties of rod-like structures. This effect, which may be due in part to the scavenging of small leucine particles by the bacteria-containing particles, leading to less cohesive attraction between the larger leucine particles by increasing void volume in the dry powder state, combines the advantages of carrier and porous particle systems.
In our in vivo results, a 1.0–1.1 log reduction in lung cfu was obtained in animals immunized by parenteral routes with respect to untreated controls. Strikingly, however, a 3.2 log reduction in lung cfu was obtained after pulmonary immunization with BCG particles, compared with untreated controls, showing improved protection against virulent M. tuberculosis challenge with this formulation in the highly sensitive guinea pig TB model.
Our results compare favorably with the work of Rosenthal et al. (17) and Lagranderie et al. (18). In the pioneering work by Rosenthal et al. in 1968 (17), guinea pigs, children, and medical students were exposed to BCG aerosols generated by nebulization. The measure for immunization in this work was the rate and size of the tuberculin reaction after exposure to BCG aerosols. Lacking a challenge with virulent bacteria and with variability in the nebulizer output, the results of these early studies were inconclusive. Lagranderie et al. (18) studied the effects of dose in guinea pigs receiving intradermal or aerosol immunizations with BCG. The protection provided by aerogenic BCG was comparable with that of parenteral administration in the studies by Lagranderie et al., whereas within our study, the powder formulation provided better protection than parenteral immunization against bacterial challenge.
The relative success of the approach to immunization obtained in our studies appears to result from a combination of the alternate route of administration and the unique particulate form of the BCG aerosol. It may have relevance to other bacterial vaccines, including Mycobacterium avium complex, Mycobacterium ulcerans or Mycobacterium leprae for nontuberculous mycobacterial diseases, Bordetella pertussis for whooping cough, Bacillus anthracis for anthrax, Franciscella tularensis for tularemia, Yersinia pestis for plague, and Streptococcus pneumoniae for pneumonia. The principles and preparations described here to be effective for bacterial vaccine delivery may also be effective in delivery of other live vaccines, including those for viral diseases.
Methods
Spray-drying solutions were prepared by mixing l-leucine (Sigma) solution and previously prepared M. smegmatis or Mycobacterium bovis BCG suspensions in various desired ratios (wt/wt). Spray-drying parameters, bacterial culture, lyophilization, and vial-filling methods can be found in ref. 15. Powder was collected immediately for characterization and stored as described below. A single ratio of 95:5 leucine to M. smegmatis (or leucine:BCG) was used for the animal studies.
Characterization of Spray-Dried Powders.
Serial dilution plating was used to assess the number of viable colony-forming untis of M. smegmatis or M. bovis bacteria in cell suspensions before spray drying and in powders after spray drying. Powders were dispersed in PBS and 0.05% Tween 80 to dissolve excipient and vortexed to resuspend the bacteria homogeneously. To assess the stability of bacterial viability, in colony-forming units, powders were stored at 4°C, 20% relative humidity (refrigerated conditions) in individual vials and plated at monthly intervals (months 1, 2, 3, 4, 6, 9, and 12).
To determine the fine particle fraction (proportion of mass with particle size <5.8 μm) of viable bacteria of each powder for filing purposes we used a six-stage Anderson cascade impactor (ACI-6; Thermo Andersen). Capsules containing 10 ± 2.5 mg of powder were placed in a hand-held dry powder inhaler device (Plastiape). The capsule in the inhaler was punctured, and a pump simulating an inspiration (28.3 liters/min for 4.2 s) deposited the dried bacteria powder on different stages depending on the aerodynamic diameter of the particles. Powder was collected at each stage and plated on 7H10 agarose plates to determine the number of colony-forming units of each powder on each stage. MMAD was determined by measuring the mass distribution of powder per stage, using the aerodynamic diameter calibration of each stage. The aerodynamic diameter D, which is defined in terms of the geometric diameter d by
with ρ the particle density and ξ a dimensionless shape factor of value unity for perfect spheres, is then determined gravimetrically. This value can be measured and compared with the mass-median geometric diameter d to determine the shape factor ξ per power. For cylindrical particles with length D1 and diameter D2, the shape factor can be expressed as Eq. 2
 |
The size range of M. bovis is ≈1–4 μm in length and 0.2–0.4 μm in axial diameter (D2) (16); assuming a cylindrical shape, this size gives an approximate shape factor of 0.6.
We measured the volume-median geometric diameter by a laser diffraction optical sizing technique (HELOS system; Sympatec). This apparatus allows measurement of particle size distributions of solids, suspensions, and sprays by using a laser diffraction optics and photosensor array. Based on the assumption of a uniform density per particle, an algorithm to determine mass-median geometric diameter can be adopted. In our experiments, particle size was measured at various pressures (0.5, 1.0, 2.0, and 4.0 bar) to evaluate the effects of particle aggregation. The value for x50 was reported as the volume-median geometric diameter, dg, value and x16 and x84 were used to indicate particle size distribution to obtain geometric standard deviation (GSD) where:
Emitted Dose from a Newborn Inhaler Device.
Emitted doses were sampled from the inhaler by using an electromechanical squeeze fixture mechanism created to allow consistent and reproducible actuation of the inhaler during the testing process (see SI Appendix). Testing was performed on five capsules for each powder formulation. Capsules were filled with ≈10 mg of placebo powder. Powders of leucine and M. smegmatis in ratios of 99:1, 95:5, 70:30, and 50:50 by weight were evaluated. Capsules were filled with ≈10 mg of placebo powder. For each capsule tested, the electromechanical fixture was programmed to actuate for five cycles consisting of a 0.25-s squeeze period followed by a 2-s dwell period. Emitted dose was determined from gravimetric data taken before and after squeeze testing.
Animals and Treatments.
All animal procedures were approved by the University of North Carolina Chapel Hill Institutional Animal Care and Use Committee. Male guinea pigs weighing 479.4 ± 46.7 g were housed in a 12-h light/12-h dark cycle and constant temperature environment of 22°C. A standard diet and water were supplied ad libitum.
Animals were randomly assigned to eight different groups (n = 6 each) and immunized with BCG solutions or particles as follows: s.c. solution at 2 × 105 cfu and 2 × 106 cfu; intradermal solution at 2 × 106 cfu; s.c. particles at 2 × 106 cfu; and pulmonary particles (particles delivered to the lungs) at 2 × 105 cfu. BCG particles were administered to anesthetized animals by insufflation (Penn Century). Untreated animals were used as controls (Table 1). Six weeks after immunization, the delayed-type hypersensitivity response was evaluated in the animals by intradermal injection of PPD solution (100 TU), and the diameter of induration was measured 24 h later.
Bacterial Challenge and Necropsy.
Immediately after assessing the delayed-type hypersensitivity response, animals were challenged by the respiratory route with a suspension of M. tuberculosis, strain H37Rv, employing an aerosol exposure chamber. The parameters of the infection procedure were adjusted to result in the inhalation and retention of ≈10–15 viable, virulent organisms per animal. Necropsy was conducted 4 weeks after challenge, and levels of protection were determined in terms of bacteriology, histopathology, and wet tissue weights.
Four weeks after bacterial challenge, animals were killed by an i.p. lethal dose of sodium pentobarbital. The chest and peritoneal cavities were inspected, and lungs and spleen were removed to evaluate the extent of infection. Levels of protection were determined in terms of bacteriology, histopathology, and wet tissue weights. For bacteriology, the right lower lobe of the lung and a portion of the spleen were homogenized separately in sterile saline solution and inoculated in M7H10 agar plates. The number of viable bacteria was counted after 3 weeks of incubation at 37°C. For histopathology, tissues were preserved in formalin solution, embedded in paraffin, and sectioned at 5 μm. The sections were mounted on a glass slide and stained with hematoxylin/eosin. Microscopic examinations were conducted by a pathologist who was blinded with respect to the treatment received by any of the animals.
Statistics.
The size of tuberculin reactions to PPD and the log-transformed number of bacteria in lung and spleen were assumed to be normally distributed and were analyzed by ANOVA. Differences between treatments were determined by the least-squares significant difference multiple-comparison method. A probability level of 5% (P < 0.05) was considered statistically significant.
Supplementary Material
Acknowledgments.
This work was supported by a grant from the Gates Foundation Grand Challenges.
Footnotes
The authors declare no conflict of interest.
This article contains supporting information online at www.pnas.org/cgi/content/full/0800043105/DC1.
Hickey AJ, et al. (2007) Tuberculosis: From the Lab Research to Field Trials, eds Kaufmann SHE, Smith I, Nathan CF, Keystone Symposia on Molecular and Cellular Biology, Silverthorne, CO, p 97.
References
- 1.Bivas-Benita M, Ottenhoff THM, Junginger HE, Borchard G. Pulmonary DNA vaccination: Concepts, possibilities and perspectives. J Control Rel. 2005;107:1–29. doi: 10.1016/j.jconrel.2005.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lu D, Hickey AJ. Pulmonary vaccine delivery. Exp Rev Vaccines. 2007;6:213–226. doi: 10.1586/14760584.6.2.213. [DOI] [PubMed] [Google Scholar]
- 3.Fuchs NA. Mechanics of Aerosols. Oxford, UK: Pergamon; 1964. Size and shape of aerosol particles, pp. 1–20. [Google Scholar]
- 4.Bell JH, Hartley PS, Cox JSG. Dry powder aerosols. I. A new powder inhalation device. J Pharm Sci. 1971;60:1559–1564. doi: 10.1002/jps.2600601028. [DOI] [PubMed] [Google Scholar]
- 5.Hickey AJ, Fults KA, Pillai RS. Use of particle morphology to influence delivery of drugs from dry powder aerosols. J Biopharm Sci. 1992;3:107–113. [Google Scholar]
- 6.Edwards D. Large porous particles for pulmonary drug delivery. Science. 1997;276:1868–1871. doi: 10.1126/science.276.5320.1868. [DOI] [PubMed] [Google Scholar]
- 7.Davies CN. Particle fluid interactions. J Aerosol Sci. 1979;10:477–513. [Google Scholar]
- 8.Harris RL, Timbrell V. The influence of fiber shape in lung deposition: Mathematical estimates. In: Walton WH, editor. Inhaled Particles. Vol 4. Oxford, UK: Pergamon; 1977. pp. 75–89. [PubMed] [Google Scholar]
- 9.Kottrappa P. In: Rochester Third International Conference on Environmental Toxicity. Mercer TT, Morrow PE, Stober W, editors. Vol 14. Springfield, IL: CC Thomas; 1970. pp. 249–289. [Google Scholar]
- 10.Chan HK, Gonda I. Aerodynamic properties of elongated particles of cromoglycic acid. J Aerosol Sci. 1989;20:157. [Google Scholar]
- 11.Gonda I, El Khalik AFA. On the calculation of aerodynamic diameter of fibers. Aerosol Sci Tech. 1985;4:233–238. [Google Scholar]
- 12.Crowder TM, Rosati J, Shroeder J, Hickey AJ, Martonen TB. Fundamental effects of particle morphology on lung delivery: Predictions of Stokes' law and the particular relevance to dry powder inhaler formulation and development. Pharm Res. 2002;19:239–245. doi: 10.1023/a:1014426530935. [DOI] [PubMed] [Google Scholar]
- 13.Concessio NM, Hickey AJ. Descriptors of irregular particle morphology and powder properties. Adv Drug Del Rev. 1997;26:29–40. doi: 10.1016/s0169-409x(97)00508-5. [DOI] [PubMed] [Google Scholar]
- 14.Fults KA, Miller IF, Hickey AJ. Effect of particle morphology on emitted dose of fatty acid-treated disodium cromoglycate powder aerosols. Pharm Dev Tech. 1997;2:67–79. doi: 10.3109/10837459709022610. [DOI] [PubMed] [Google Scholar]
- 15.Wong Y-L, et al. Drying a tuberculosis vaccine without freezing. Proc Natl Acad Sci USA. 2007;104:2591–2595. doi: 10.1073/pnas.0611430104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Flynn J. Immunology of tuberculosis and implication in vaccine development. Tuberculosis. 2004;84:93–101. doi: 10.1016/j.tube.2003.08.010. [DOI] [PubMed] [Google Scholar]
- 17.Rosenthal SR, McEnery JT, Raisys N. Aerogenic BCG vaccination against tuberculosis in animal and human subjects. J Asthma Res. 1968;5:309–323. doi: 10.3109/02770906809100348. [DOI] [PubMed] [Google Scholar]
- 18.Lagranderie M, et al. BCG-induced protection in guinea pigs vaccinated and challenged via the respiratory route. Tubercle Lung Dis. 1993;74:38–46. doi: 10.1016/0962-8479(93)90067-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.