Abstract
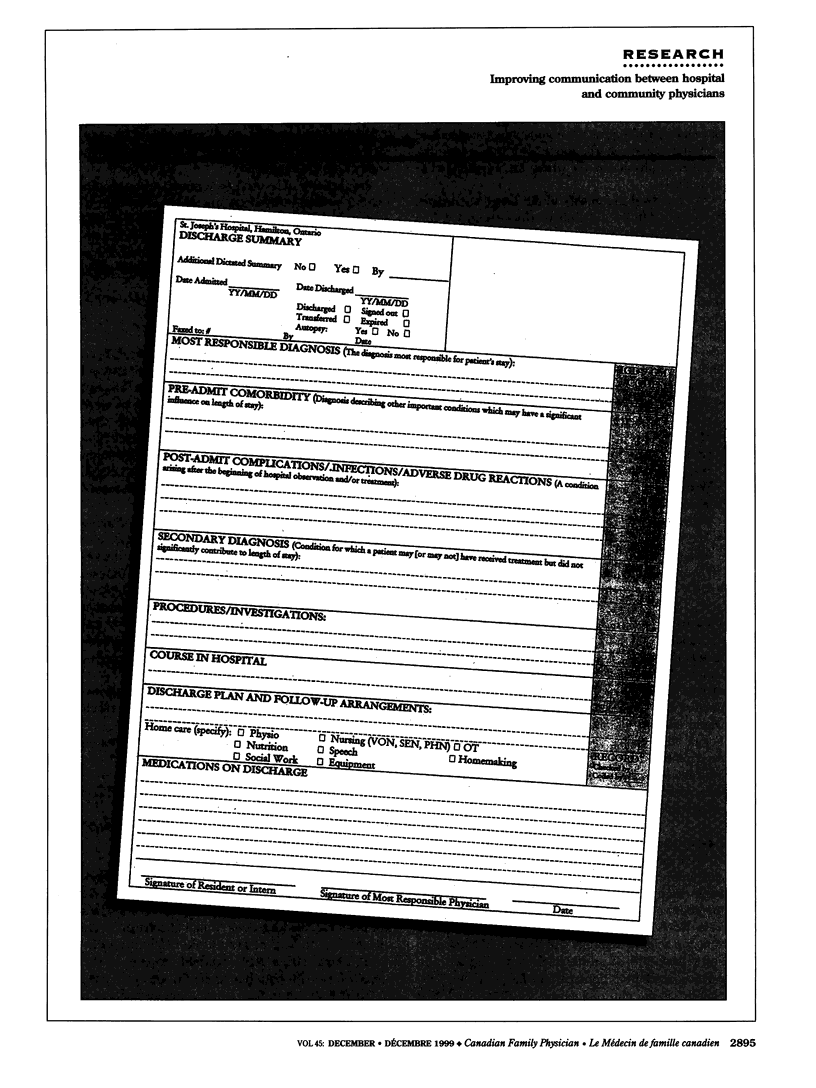
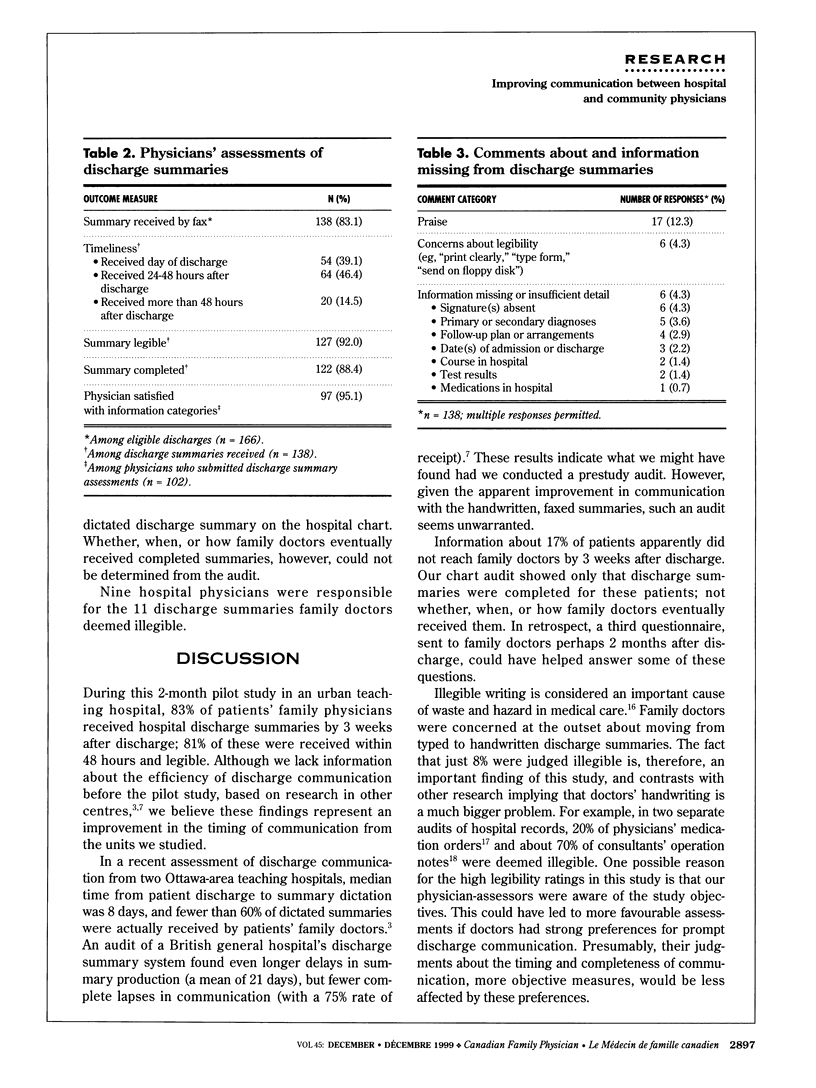
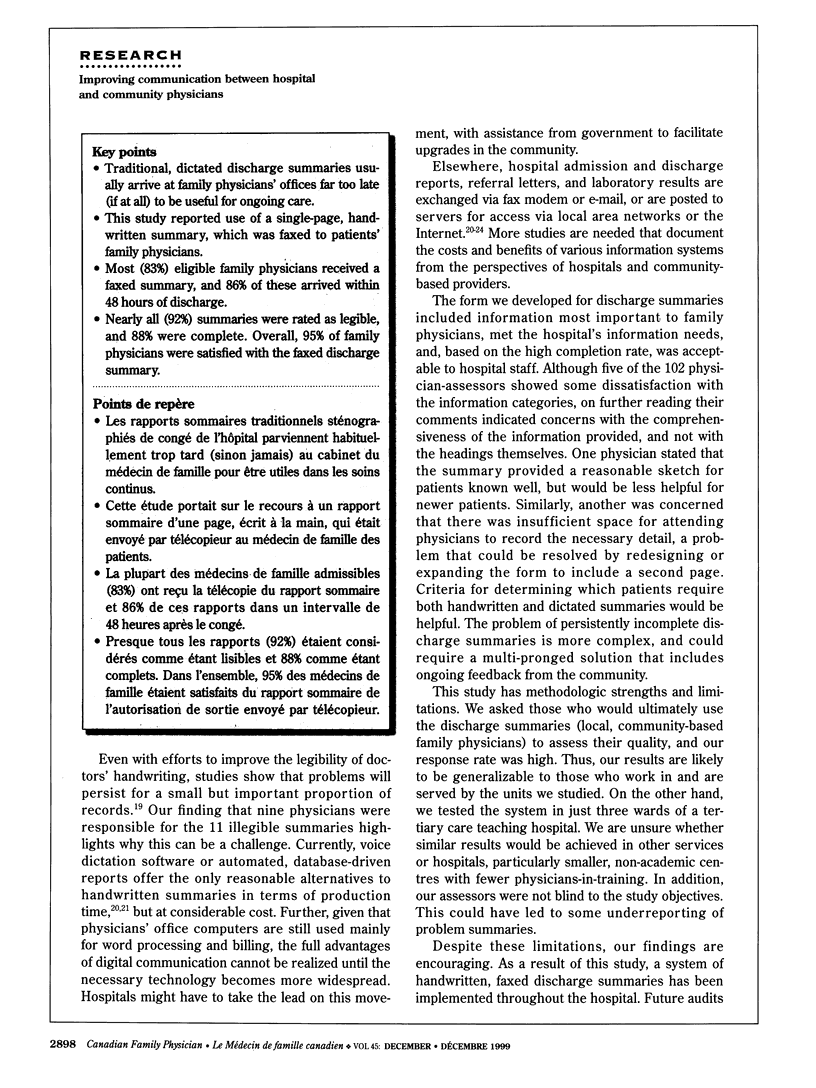
OBJECTIVE: To assess the timing, legibility, and completeness of handwritten, faxed hospital discharge summaries as judged by family physicians and to obtain their opinion on the information categories on a standardized discharge summary form. DESIGN: Fax survey of physicians for consecutive patients discharged from hospital over 8 weeks. SETTING: Three wards in a tertiary care teaching hospital. PARTICIPANTS: One hundred two family physicians and general practitioners practising in Hamilton, Ont. MAIN OUTCOME MEASURES: Proportions of summaries that were received, received within 48 hours of discharge, legible, and complete; types of information missing from incomplete summaries; proportion of physicians satisfied with the information categories. RESULTS: Of 271 consecutive patient discharges, 195 (72%) were eligible for study. Among those ineligible, 22 patients (8%) did not have a family doctor identified on their hospital records. Among records that did have a family physician identified, fax numbers were unavailable or unknown for 54 physicians (20%). One hundred two physicians completed 166 discharge summary assessments for a response rate of 85% (166/195). By 3 weeks after discharge, 138 discharge summaries (83%) had been received by patients' family doctors. Among those received, 86% were received within 48 hours of discharge; 92% were legible; and 88% were complete. Hospital doctors' signatures, patients' diagnoses, and follow-up plans were most frequently missing. Ninety-five percent of physicians were satisfied with the information categories included on the standardized form. CONCLUSIONS: Handwritten, faxed hospital discharge summaries were acceptable to family physicians for most patients. Criteria are needed for determining which patients require both handwritten and dictated discharge summaries.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Adams D. C., Bristol J. B., Poskitt K. R. Surgical discharge summaries: improving the record. Ann R Coll Surg Engl. 1993 Mar;75(2):96–99. [PMC free article] [PubMed] [Google Scholar]
- Baigrie R. J., Dowling B. L., Birch D., Dehn T. C. An audit of the quality of operation notes in two district general hospitals. Are we following Royal College guidelines? Ann R Coll Surg Engl. 1994 Jan;76(1 Suppl):8–10. [PubMed] [Google Scholar]
- Berwick D. M., Winickoff D. E. The truth about doctors' handwriting: a prospective study. BMJ. 1996 Dec 21;313(7072):1657–1658. doi: 10.1136/bmj.313.7072.1657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booth A. O. Using a computer-linked fax in patient discharge. Prof Nurse. 1996 Aug;11(11):764–766. [PubMed] [Google Scholar]
- Branger P. J., van der Wouden J. C., Schudel B. R., Verboog E., Duisterhout J. S., van der Lei J., van Bemmel J. H. Electronic communication between providers of primary and secondary care. BMJ. 1992 Oct 31;305(6861):1068–1070. doi: 10.1136/bmj.305.6861.1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brazy J. E., Langkamp D. L., Brazy N. D., De Luna R. F. Do primary care physicians prefer dictated or computer-generated discharge summaries? Am J Dis Child. 1993 Sep;147(9):986–988. doi: 10.1001/archpedi.1993.02160330076024. [DOI] [PubMed] [Google Scholar]
- Castleden W. M., Stacey M. C., Norman P. E., Lawrence-Brown M. M., Brooks J. G. General practitioners' attitudes to computer-generated surgical discharge letters. Members of the Department of General Surgery, Fremantle Hospital. Med J Aust. 1992 Sep 21;157(6):380–382. doi: 10.5694/j.1326-5377.1992.tb137245.x. [DOI] [PubMed] [Google Scholar]
- Del Mar C. B., Lowe J. B., Adkins P., Arnold E., Baade P. Improving general practitioner clinical records with a quality assurance minimal intervention. Br J Gen Pract. 1998 Jun;48(431):1307–1311. [PMC free article] [PubMed] [Google Scholar]
- Lenhard R. E., Jr, Buchman J. P., Achuff S. C., Kahane S. N., Macmanus C. J. AUTRES--the Johns Hopkins Hospital automated resume. J Med Syst. 1991 Jun;15(3):237–247. doi: 10.1007/BF00996553. [DOI] [PubMed] [Google Scholar]
- Lockwood E., McCallum F. M. Patients discharged from hospital: an aspect of communication in the Health Service. Health Bull (Edinb) 1970 Apr;28(2):75–80. [PubMed] [Google Scholar]
- Long A., Atkins J. B. Communications between general practitioners and consultants. Br Med J. 1974 Nov 23;4(5942):456–459. doi: 10.1136/bmj.4.5942.456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mageean R. J. Study of "discharge communications" from hospital. Br Med J (Clin Res Ed) 1986 Nov 15;293(6557):1283–1284. doi: 10.1136/bmj.293.6557.1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manning R. T. Dictation of the discharge resumé: a forgotten link between the spoken and written word. J Gen Intern Med. 1989 Sep-Oct;4(5):453–456. doi: 10.1007/BF02599699. [DOI] [PubMed] [Google Scholar]
- Penney T. M. Delayed communication between hospitals and general practitioners: where does the problem lie? BMJ. 1988 Jul 2;297(6640):28–29. doi: 10.1136/bmj.297.6640.28-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rawal J., Barnett P., Lloyd B. W. Use of structured letters to improve communication between hospital doctors and general practitioners. BMJ. 1993 Oct 23;307(6911):1044–1044. doi: 10.1136/bmj.307.6911.1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reddy S., Niewiadomska-Bugaj M., Reddy Y. V., Galfalvy H. C., Jagannathan V., Raman R., Srinivas K., Shank R., Davis T., Friedman S. Experiences with ARTEMIS--an Internet-based telemedicine system. Proc AMIA Annu Fall Symp. 1997:759–763. [PMC free article] [PubMed] [Google Scholar]
- Siders A. M., Peterson M. Increasing patient satisfaction and nursing productivity through implementation of an automated nursing discharge summary. Proc Annu Symp Comput Appl Med Care. 1991:136–140. [PMC free article] [PubMed] [Google Scholar]
- Smith R. P., Holzman G. B. The application of a computer data base system to the generation of hospital discharge summaries. Obstet Gynecol. 1989 May;73(5 Pt 1):803–807. [PubMed] [Google Scholar]
- Solomon J. K., Maxwell R. B., Hopkins A. P. Content of a discharge summary from a medical ward: views of general practitioners and hospital doctors. J R Coll Physicians Lond. 1995 Jul-Aug;29(4):307–310. [PMC free article] [PubMed] [Google Scholar]
- Wass A. R., Illingworth R. N. What information do general practitioners want about accident and emergency patients? J Accid Emerg Med. 1996 Nov;13(6):406–408. doi: 10.1136/emj.13.6.406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winslow E. H., Nestor V. A., Davidoff S. K., Thompson P. G., Borum J. C. Legibility and completeness of physicians' handwritten medication orders. Heart Lung. 1997 Mar-Apr;26(2):158–164. doi: 10.1016/s0147-9563(97)90076-5. [DOI] [PubMed] [Google Scholar]
- van Walraven C., Duke S. M., Weinberg A. L., Wells P. S. Standardized or narrative discharge summaries. Which do family physicians prefer? Can Fam Physician. 1998 Jan;44:62–69. [PMC free article] [PubMed] [Google Scholar]
- van Walraven C., Weinberg A. L. Quality assessment of a discharge summary system. CMAJ. 1995 May 1;152(9):1437–1442. [PMC free article] [PubMed] [Google Scholar]


