Abstract
Study Objective:
There is a relatively small body of literature looking at sleep disordered breathing (SDB) in acutely ill inpatients. The aim of this study was to assess the frequency of SDB in acutely ill patients admitted to tertiary care centers referred for an inpatient polysomnogram and to identify associations between SDB and patient characteristics.
Methods:
The study was a retrospective chart review of 100 polysomnograms and medical records of all patients who had polysomnography while hospitalized at 2 tertiary care centers between January 2003 and September 2004. Main outcome measures included the frequency of and the association between SDB and specific characteristics, including age, sex, body mass index, and admission disease condition.
Results:
There was a high frequency of SDB in the sample (77%). There was an increase in the odds ratio (OR) of SDB with increasing body mass index (OR 1.08; 95% confidence interval; 95%CI 1.02, 1.15). Increasing BMI categories were associated with more severe SDB (p = 0.005). Adjusting for age and BMI, men had a reduced OR of sleep apnea, as compared with women (OR 0.32; 95%CI 0.10, 1.0), and women with SDB were more likely to have more severe disease than men (p = 0.003). There was a significant association of SDB with decompensated CHF (p = 0.01).
Conclusions:
There is a high frequency of SDB in hospitalized patients referred for polysomnography, especially in patients with underlying cardiopulmonary disease. Further investigation of the impact of SDB on acute exacerbations of cardiopulmonary disease is needed, given the high frequency of SDB in hospitalized patients.
Citation:
Goring K; Collop N. Sleep disordered breathing in hospitalized patients. J Clin Sleep Med 2008;4(2):105–110.
Keywords: Inpatient, polysomnography, sleep disordered breathing, comorbidity, sex, congestive heart failure
Sleep disordered breathing (SDB) is a prevalent problem with clinical expression ranging from snoring to severe obstructive sleep apnea (OSA). The OSA syndrome affects at least 5% of the adult population.1 A growing body of literature attests to significant morbidity associated with even mild OSA. Undiagnosed OSA with or without symptoms has been independently associated with an increased likelihood of systemic hypertension,2 cardiovascular disease,3 stroke, and diminished quality of life.4,5 In addition, there is a well-recognized association between OSA, sleepiness, and automobile accidents in both commercial and noncommercial drivers.6,7
Severe sleep apnea causes oxygen desaturation, which triggers a catecholamine surge and elevations in blood pressure.4 This can lead to decompensated congestive heart failure (CHF) and acute stroke in the susceptible indvidiual.3,4 It has been recognized that the combination of chronic obstructive pulmonary disease and sleep apnea worsens gas-exchange abnormalities during sleep in patients with chronic obstructive pulmonary disease, leading to increased morbidity.5 In effect, SDB is associated with a myriad of systemic complications.
In contrast with the wealth of descriptive information regarding SDB in the outpatient setting, relatively little is known regarding SDB in acutely ill patients. Most studies note the effect of the inpatient setting on sleep quality and quantity.8 Other studies have described a high frequency of arrhythmias in subjects with SDB.9
To date, there is no description of the association between SDB and acute exacerbations of cardiopulmonary disease in a large inpatient population. The primary aims of this study are to assess the prevalence of SDB in patients referred for inpatient polysomnography in a tertiary care center and to assess the odds of association of SDB with the underlying acute illness, as well as with patient characteristics. A secondary aim is to evaluate the quality of sleep and type of apneas in the sample.
METHODS
The study involved a retrospective chart review of polysomnographic reports and medical records of all patients who had studies done while hospitalized at Johns Hopkins Hospital or Bayview Medical Center between January 2003 and September 2004. Consent for this project was obtained from the Johns Hopkins Institutional Review Board.
Total sleep time, sleep stages, sleep efficiency, the presence of SDB, type of apnea, and occurrence of hypoxemia and arrhythmias were noted. Body mass index (BMI) and inpatient diagnoses were recorded as well as the specialty of the physician referring the patient for the sleep study.
After discharge, it was noted if the patient had a repeat polysomnogram as an outpatient and if continuous positive airway pressure equipment was arranged for outpatient use, when applicable.
Polysomnography
Overnight polysomnography was performed using the Compumedics Portable PS-2 System (Abbottsville, Australia) attended by a technologist at the bedside. Sensors were placed and equipment was calibrated by a certified technician. Data collection included 2 central electroencephalographic leads; right and left electrooculograms, bipolar submental electromyogram, thoracic and abdominal excursions (inductive plethysmography bands), airflow (detected by a nasal pressure transducer and nasal-oral thermistor), oximetry (finger pulse oximetry), and electrocardiogram and heart rate (using a bipolar electrocardiogram lead), and body position (using a mercury gauge sensor). The data were then downloaded to computers where it was scored and subsequently analyzed by a board-certified pulmonologist with sleep medicine expertise.
Scoring of the polysomnograms was done by experienced polysomnographic technologists. Sleep stages were scored according to the guidelines developed by Rechtschaffen and Kales.12 Stages 3 and 4 sleep were combined (slow-wave sleep). Arousals were identified according to American Sleep Disorders Association (American Academy of Sleep Medicine) criteria.13 An apnea was defined as a complete or almost complete cessation of airflow (< 25% of baseline), as measured by the amplitude of the nasal and nasal-oral flow signal, lasting 10 seconds or longer. A hypopnea was defined as a reduction in airflow associated with a fall in oxygen saturation of at least 4% or an arousal.
Study Sample
All records of patients admitted to Johns Hopkins Hospital or Bayview Hospital who had inpatient sleep studies between January 2003 and September 2004 were reviewed. Patients with a total sleep time of less than 2 hours, patients with open tracheostomies, or those whose BMI was unknown were excluded from further evaluation.
Definitions and Statistical Analysis
The percentage time in each sleep stage was calculated based on the total time asleep. Sleep efficiency was defined as the percentage of total time asleep, divided by the total time in bed after lights off to the time of final awakening. BMI, calculated as weight in kilograms divided by the square of height in meters, was categorized into quartiles that are commonly considered as identifying degree of obesity, (Class 1 ≤ 25 kg/m2, Class 2 = 25 to 29.9 kg/m2, Class 3 = 30 to 39.9 kg/m2, and Class 4 ≥ 40 kg/m2). SDB was defined as an apnea-hypopnea index (AHI) of 10 or higher. Overall apneas were described according to which type of apnea was responsible for more than 50% of the events on the polysomnogram.
The diagnoses listed were assigned to patients by the inpatient attending physician. The hospital discharge summaries were accessed via the electronic patient records, and discharge diagnosis, referral for CPAP therapy, and referral to the Hopkins sleep clinic were noted.
All statistical analyses were performed using the STATA 9.0 statistical software package. Age and BMI were categorized into 3 and 4 categories, respectively. AHI was categorized into 4 groups corresponding to severity of SDB. Logistic regressions were performed to assess the extent of the relationship between having sleep apnea and the subject's personal characteristics and disease on admission. Because of separation issues (or areas of perfect prediction) in the logistic regression analyses stemming from the condition indicator variables, Fisher exact tests were also performed to evaluate the relationship between having sleep apnea and each variable of interest.
RESULTS
Sample Characteristics
During the sample period, there were 117,444 adult admissions to the Johns Hopkins Hospital (77,478) and Bayview Medical Center (39,966). Therefore, the number referred for an inpatient sleep study represented 0.086% of all adult admissions. Of the 100 charts reviewed, 6 were excluded from further analysis due to incomplete data (missing weight, height) or due to the presence of an open tracheostomy. The mean age of the patients was 54.0 ± 13.9 years (range 20-82). There was a higher proportion of women (54%) than men (46%) in the sample. The mean BMI was 40.17 ± 10.6 kg/m2 (range 18-70 kg/m2). Overweight patients (BMI 25-30 kg/m2) comprised 8.5% of the total, and obese patients (BMI > 30 kg/m2) made up 86.2% of the total sample. (Table 1)
Table 1.
Personal Characteristics of the 94 Patients Comprising the Study Population
| No. | % | |
|---|---|---|
| Sex | ||
| Women | 51 | 54 |
| Men | 43 | 46 |
| Age, y | ||
| 20–49 | 37 | 39 |
| 50–69 | 43 | 46 |
| 70+ | 14 | 15 |
| BMI, kg/m2 | ||
| 18–24 | 5 | 5 |
| 25–29 | 7 | 8 |
| 30–39 | 36 | 38 |
| 40+ | 46 | 49 |
Sleep Architecture
The analysis of sleep stages are shown in Table 2. A comparison of the sleep stages with a distribution from a normal population matched for age is given in Figure 1. There was a higher percentage of stage 1 and less rapid eye movement (REM) sleep, as compared with an age-matched normal population.
Table 2.
Sleep-Stage Analysis
| Characteristic | Mean ± SD | Range |
|---|---|---|
| TST, min | 225.1 ± 69.9 | 124–402 |
| Sleep efficiency, % | 76 ± 15.6 | 30–100 |
| NREMa | 89.2 ± 10.1 | 57–100 |
| REMa | 10.9 ± 10.2 | 0–43 |
NREM (non-rapid eye movement) and rapid eye movement (REM) sleep are shown as a percentage of total sleep time (TST).
Figure 1.
Sleep-stage percentage of inpatients versus age-matched normal control subjects. This figure shows sleep stages 1, 2, 3+4, and rapid eye movement (REM) as a percentage of total sleep time in the inpatient population studied, compared with age-matched normal controls.16
SDB Characteristics
SDB was present in 77% of patients. The majority of those with SDB had obstructive apneas (95%). For the group, the average low oxygen saturation was 89% in non-REM sleep and 82% in REM sleep. Forty-two percent of patients were on oxygen throughout the study; however, there was as equal a likelihood of desaturation below 90% in those on oxygen as compared with those not requiring oxygen supplementation.
There was a statistically significant increase in the odds of having sleep apnea with increasing BMI (odds ratio; [OR] 9.81; 95% confidence interval; [CI] 1.0, 91.7) (Table 3). Comparing BMI class 4 with class 1, there was no clear linear increase in the odds of sleep apnea with a doubling of the BMI. An investigation of the composition of the BMI categories by age and sex categories did not reveal any patterns that might explain the lack of linearity in the relationship between BMI and odds of sleep apnea.
Table 3.
Multivariable Logistic Regression Analysis of Sleep Apnea with Subject's Characteristics (N=94)
| Included in model: | Odds ratio (95% CI) |
|---|---|
| Age (years) | 1.02 (0.98, 1.06) |
| Age category (50-69) a | 0.87 (0.25, 3.0) |
| Age category (70+) a | 4.33 (0.42, 44.9) |
| BMI (kg/m2) | 1.08* (1.02, 1.15) |
| BMI category (25-29) b | 5.13 (0.26, 102.) |
| BMI category (30-39) b | 1.83 (0.20, 16.6) |
| BMI category (40+) b | 9.81* (1.0, 91.7) |
| Gender c | 0.32* (0.10, 1.0) |
compared to lowest age category (20–49)
compared to lowest BMI category (18–24)
0 = female: 1= male
p < 0.05
Multivariable logistic regression analyses of sleep apnea on baseline characteristics was performed (Table 4). There was a statistically significant increase in the OR of sleep apnea with every unit increase in BMI (OR 1.08; 95%CI 1.02, 1.15) adjusting for all other variables. Adjusting for age and BMI, men had a statistically significant reduced odds ratio of sleep apnea compared to women (OR 0.32; 95% CI 0.10, 1.0).
Table 4.
Proportion of Subjects with Sleep Apnea in Each Disease Category Versus Proportion in Sample Without Disease
| Disease | Total sample, no. | Sample with sleep apnea, no. (%) |
p Valuea | |
|---|---|---|---|---|
| Disease absent | Disease present | |||
| COPD | 13 | 62 (77) | 11 (85) | 0.73 |
| CHF | 18 | 55 (72) | 18 (100) | 0.01 |
| COPD-CHF | 6 | 68 (77) | 5 (83) | 1.00 |
| Hypercapnea | 10 | 67 (80) | 6 (60) | 0.22 |
| ILD | 8 | 69 (80) | 4 (50) | 0.07 |
| HIV | 2 | 72 (78) | 1 (50) | 0.40 |
| PE | 2 | 71 (77) | 2 (100) | 1.00 |
| Pulmonary HTN | 8 | 66 (77) | 7 (88) | 0.68 |
| Miscellaneous | 27 | 54 (81) | 19 (70) | 0.29 |
COPD refers to chronic obstructive pulmonary disease; CHF, congestive heart failure; ILD, interstitial lung disease; PE, pulmonary embolism; HTN, hypertension.
Fisher exact test
Analysis of SDB and Disease Condition
There was a wide spectrum of disease. The majority of patients were admitted with chronic obstructive pulmonary disease, congestive heart failure (CHF). Interstitial lung disease (ILD), acute pulmonary embolism, and pulmonary hypertension were the next most common diseases. The Miscellaneous category captured any other diagnosed conditions.
Fisher exact test was performed to evaluate the relationship between the existence of the condition and of sleep apnea. There was a statistically significant association between sleep apnea and CHF (p = 0.01). There was a suggestion of an association between sleep apnea and ILD (p = 0.07). Due to the small numbers with pulmonary embolism, it was difficult to establish a relationship between sleep apnea and pulmonary embolism (p = 1.00). Further analysis of the association of SDB with each of the disease categories adjusted for age, sex, and BMI was performed.
Multivariable logistic regression analyses were performed on 2 models for each of the 9 condition categories, with the following combinations of the personal characteristics as additional independent variables:
Model 1: Disease condition (see Table 5)
Table 5.
Comparison of AHI Categories and Sex
| AHI, kg/m2 | Sex | p Valuea | |
|---|---|---|---|
| Female | Male | ||
| 0–10 | 13 (30) | 25 (49) | 0.003 |
| 11–30 | 5 (12) | 15 (29) | |
| 31–50 | 8 (19) | 3 (6) | |
| 51+ | 17 (40) | 8 (16) | |
Data are presented as number (%). AHI refers to apnea-hypopnea index.
Fisher exact test.
Model 2: Disease condition, sex, age categories, and BMI categories, where the age and BMI categories were converted to dummy variables using the lowest category as the reference.
The lack of a statistically significant association between sleep apnea and each disease category remained in model 2 if seen in model 1.
For CHF and ILD, the logistic regression analyses showed separation issues because of the complete, or almost complete, predictability of 1 category, and, thus, the full models could not be run. The perfect correlation between sleep apnea and CHF could not be explained by BMI, since there was imperfect correlation between increasing BMI and the probability of sleep apnea. The perfect correlation between sleep apnea and ILD could not be further explored due to the small number with ILD.
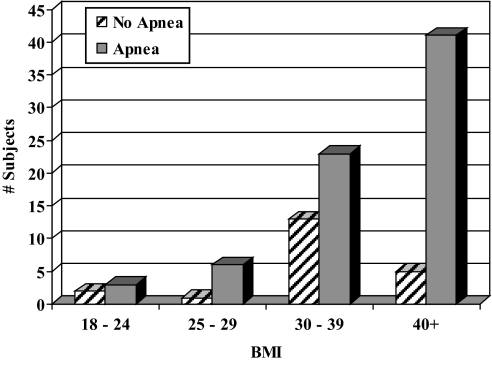
The relationship between BMI and the existence of sleep apnea, which consistently showed significance in the logistic regression analyses, is presented in Figure 2. This graph highlights not only the larger number, but also the larger proportion, of patients having sleep apnea with larger BMI scores.
Figure 2.
Body mass index (BMI) versus sleep apnea. This figure shows how BMI was related to the presence of sleep disordered breathing in the inpatient population studied.
Analysis of Severity of SDB
The severity of SDB is judged by the AHI, which is traditionally categorized into 4 categories: 0 to 10, 11 to 30, 31 to 50, and more than 50, where the latter 3 categories represent mild, moderate, and severe disease. These categories were then compared with sex and the age and BMI categories using Fisher exact test to evaluate any potential relationships (Tables 5 and 6).
Table 6.
Comparison of AHI Categories and BMI Categories
| AHI | BMI, kg/m2 |
p Valuea | |||
|---|---|---|---|---|---|
| 18–24 | 25–29 | 30–39 | 40+ | ||
| 0–10 | 2 (40) | 4 (57) | 22 (61) | 10 (22) | 0.005 |
| 11–30 | 1 (20) | 2 (29) | 3 (8) | 14 (30) | |
| 31–50 | 0 (0) | 1 (14) | 5 (14) | 5 (11) | |
| 51+ | 2 (40) | 0 (0) | 6 (17) | 17 (37) | |
Data are presented as number (%). AHI refers to apnea-hypopnea index; BMI, body mass index.
Fisher exact test
Among those with SDB, women were more likely than men to have a higher AHI (p = 0.003). There was a nonstatistically significant association between a higher AHI in those younger than 70 years of age, as compared with older subjects (p = 0.055). Those with a higher AHI were more likely to be in the BMI category greater than 30 (p = 0.005).
Description of Arrhythmias
Six percent of patients had either episodic premature ventricular contractions or paroxysmal atrial fibrillation. No study was interrupted secondary to an arrhythmia.
Postdischarge Follow-Up
All of the requests for polysomnography originated from general medicine or medical subspecialty staff. None of the patients found to have SDB had repeat outpatient polysomnography at our institution. There was documentation in 10% of patients with SDB of an attempt to provide home continuous positive airway pressure.
DISCUSSION
Epidemiologic studies suggest at least 5% of the US population has obstructive sleep apnea syndrome.1 It is estimated 1 out of every 5 adults has mild OSA, and 1 of every 15 adults has moderate OSA.1 The prevalence of OSA in patients referred for outpatient sleep studies has been reported between 54% and 85%.22,23 We found that 77% of this referred inpatient population had SDB. Prior studies have described the poor sleep quality of hospitalized patients.2 The inpatient sample we reviewed was similar to other studies in that there was a higher percentage of stage 1 sleep than is seen in normal subjects2; however, unlike other studies, there was a higher average percent of slow wave sleep and reduced amount of REM sleep, when compared with age-matched normal subjects. We postulate that the deeper sleep noted may have been the effect of medication or rebound from earlier sleep deprivation.
This high prevalence of SDB is most likely due to the overwhelming influence of obesity. There is a well-recognized body of literature that has shown weight to be a strong predictor for SDB.10,11 The data showed a statistically significant association between SDB and increasing BMI (OR 9.81 of SDB in morbidly obese subjects, compared with normal weight (95%CI 1.0, 91.7). In this case, there was a probable bias on the part of the referring physicians in targeting obese patients for inpatient polysomnograms, given that 86% of those referred were obese.
SDB was detected in 60% of patients of normal weight who were hospitalized with flares of ILD, neuromuscular disease, and acute pulmonary embolism. It was difficult to draw statistically significant conclusions because of the small numbers of subjects in these categories; however, this is a high prevalence in a cohort that may have had a low pretest probability for SDB due to their normal weight. It has been shown that sleep-induced reduction in minute ventilation in patients with underlying neuromuscular and lung parenchymal disease occurs mainly due to a reduction in the tidal volume, leading to nocturnal desaturation.17 This pathophysiologic process may have been responsible for the SDB detected in this subset.
There is a well-recognized association between SDB and CHF in the form of both obstructive and central sleep apneas. OSA is thought to predispose to CHF by increasing left ventricular afterload from large negative intrathoracic pressure swings and increased catecholamine surges during apneic events.18,19 Central sleep apnea, in the better-recognized form of Cheyne-Stokes respiration, is considered to be a consequence of severe CHF and portends a higher mortality. SDB has been identified in stable outpatients with CHF.20 The extent to which acute decompensated CHF predisposes an individual to more severe SDB is unknown. The data show perfect correlation between SDB and CHF. The majority of the patients with CHF had OSA, and most were in the overweight or obese categories, creating a difficulty in separating the effect of obesity on the likelihood of SDB in those with CHF. Similar to other studies, the data did not reveal an increased association between OSA and chronic obstructive pulmonary disease.21
Adjusting for age and BMI, men had a statistically significantly reduced OR of sleep apnea, as compared with women (OR 0.32; 95%CI 0.10, 1.0). Among those with SDB, however, women were more likely than men to have a higher AHI (p = 0.003). Prior studies have suggested that women with OSA are more likely than men to have a greater incidence of REM-related apnea and more disrupted sleep architecture.12,13 The results from this review support the theory that the difference in sex may alter expression of the disease.
There was a marked lack of referrals from the nonmedical inpatient services. Perhaps preoperative sleep studies were performed on the outpatient service. Fewer than 10% of patients discharged with a diagnosis of SDB were seen in the Johns Hopkins sleep clinics.
There are confounders difficult to disentangle due to the retrospective design of the study. It is unclear to what extent the use of sedatives may have contributed to the occurrence of SDB in this group of patients, given that it was not possible to accurately determine sedative-hypnotic use at the time of the polysomnogram. There is no evidence, however, of this group of referred patients being more likely to have received sedative-hypnotics, as compared with the general inpatient population, lessening the chance of selection bias.
In conclusion, we suggest that there may be more SDB in hospitalized patients than has been recognized and that there is a need for a higher clinical suspicion, especially in patients with underlying cardiopulmonary disease. The decision to test for SDB in the inpatient population should not be limited to the presence of snoring, daytime fatigue, or obesity.
In addition, further investigation of the impact of SDB on acute exacerbations of chronic cardiopulmonary disease is needed, given the high prevalence of SDB in hospitalized patients.
ACKNOWLEDGMENTS
We would like to thank Hartmut Schneider, MD, PhD and Landon King, MD for assistance with this manuscript. We would also like to thank the Bayview Sleep Disorders Center for assistance with this data.
Financial Support: NIH Roadmap: Johns Hopkins Multidisciplinary Clinical Research Career Development Jr. Faculty Award, Grant #K12RR023266 (Clinical Research Scholar); Mechanisms and Treatment of COPD Progression, Grant #P50 HL084945
Footnotes
Disclosure Statement
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Young T, Gottlieb J. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002;165:1217–39. doi: 10.1164/rccm.2109080. [DOI] [PubMed] [Google Scholar]
- 2.Working Group on OSA and Hypertension. Obstructive sleep apnea and blood pressure elevation: what is the relationship? Blood Press. 1993;2:166–82. doi: 10.3109/08037059309077548. [DOI] [PubMed] [Google Scholar]
- 3.Fung JW, Li TS. Severe obstructive sleep apnea is associated with left ventricular diastolic dysfunction. Chest. 2002;121:422–9. doi: 10.1378/chest.121.2.422. [DOI] [PubMed] [Google Scholar]
- 4.Arzt M, Young T. Association of sleep-disordered breathing and the occurrence of stroke. Am J Respir Crit Care Med. 2005;172:1447–51. doi: 10.1164/rccm.200505-702OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aoki T, Akinori E. Sleep disordered breathing in patients with chronic obstructive pulmonary disease. COPD. 2005;2:243–52. [PubMed] [Google Scholar]
- 6.Howard ME, Pierce RJ. Sleepiness, sleep-disordered breathing, and accident risk factors in commercial vehicle drivers. Am J Respir Crit Care Med. 2004;170:1014–21. doi: 10.1164/rccm.200312-1782OC. [DOI] [PubMed] [Google Scholar]
- 7.Horstmann S, Mathis J. Sleepiness related accidents in sleep apnea patients. Sleep. 2000;23:383–9. [PubMed] [Google Scholar]
- 8.Krachman SL, D'Alonzo GE. Sleep in the intensive care unit. Chest. 1995;107:1713–20. doi: 10.1378/chest.107.6.1713. [DOI] [PubMed] [Google Scholar]
- 9.Mehra R, Benjamin EJ, Shahar E, Gottlieb DJ, et al. Association of nocturnal arrhythmias with sleep-disordered breathing: The Sleep Heart Health Study. Am J Respir Crit Care Med. 2006;173:910–6. doi: 10.1164/rccm.200509-1442OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dixon JB, Scachter LM. Polysomnography before and after weight loss in obese patients. Int J Obes. 2005;29:1048–54. doi: 10.1038/sj.ijo.0802960. [DOI] [PubMed] [Google Scholar]
- 11.Dixon JB, Scachter LM. Predicting sleep apnea and excessive day sleepiness in the severely obese: indicators for polysomnography. Chest. 2003;123:1134–41. doi: 10.1378/chest.123.4.1134. [DOI] [PubMed] [Google Scholar]
- 12.Resta O, Carpannano GE. Gender difference in sleep profile of severely obese patients with obstructive sleep apnea (OSA) Respir Med. 2005;99:91–6. doi: 10.1016/j.rmed.2004.05.014. [DOI] [PubMed] [Google Scholar]
- 13.Jordan AS, McEvoy RD. The influence of gender and upper airway resistance on the ventilatory response to arousal in obstructive sleep apnoea in humans. J Physiol. 2004;558:993–1004. doi: 10.1113/jphysiol.2004.064238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rechtschaffen A, Kales A. A manual of standardized terminology, techniques and scoring systems for sleep stages of human subjects. Los Angeles: UCLA Brain Information Service/Research Institute; 1968. [Google Scholar]
- 15.EEG arousals: scoring rules and examples: a preliminary report from the Sleep Disorders Atlas Task Force of the American Sleep Disorders Association. Sleep. 1992;15:173–84. [PubMed] [Google Scholar]
- 16.Ohayon M, Guilleminault C, Vitiello M. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004;27:1255–73. doi: 10.1093/sleep/27.7.1255. [DOI] [PubMed] [Google Scholar]
- 17.Becker HF, Piper CJ, Sullivan CE. Breathing during sleep in patients with nocturnal desaturation. Am J Respir Crit Care Med. 1999;159:112–8. doi: 10.1164/ajrccm.159.1.9803037. [DOI] [PubMed] [Google Scholar]
- 18.Shivalkar B, Van de Heyning C, Vrints C. Obstructive sleep apnea syndrome: more insights on structural and functional cardiac alterations, and the effects of treatment with continuous positive airway pressure. J Am Coll Cardiol. 2006;47:1433–9. doi: 10.1016/j.jacc.2005.11.054. [DOI] [PubMed] [Google Scholar]
- 19.Parish JM, Somers VK. Obstructive sleep apnea and cardiovascular disease. Mayo Clin Proc. 2004;79:1036–46. doi: 10.4065/79.8.1036. [DOI] [PubMed] [Google Scholar]
- 20.Ferrier K, Campbell A, Neal A. Sleep-disordered breathing occurs frequently in stable outpatients with congestive heart failure. Chest. 2005;128:2116–22. doi: 10.1378/chest.128.4.2116. [DOI] [PubMed] [Google Scholar]
- 21.Weitzenblaum E, Chaouat A. Sleep and chronic obstructive pulmonary disease. Sleep Med Rev. 2004;8:281–94. doi: 10.1016/j.smrv.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 22.Chervin R, Murman D. Cost utility of three approaches to the diagnosis of sleep apnea: Polysomnogram, home testing, and empiric therapy. Ann Intern Med. 1999;130:496–505. doi: 10.7326/0003-4819-130-6-199903160-00006. [DOI] [PubMed] [Google Scholar]
- 23.Deegan PC, McNicholas WT. Predictive value of clinical features for the obstructive sleep apnoea syndrome. Eur Respir J. 1996;9:117–24. doi: 10.1183/09031936.96.09010117. [DOI] [PubMed] [Google Scholar]