Abstract
Eastern equine encephalitis virus (EEEV) causes sporadic epidemics of human and equine disease in North America, but South American strains have seldom been associated with human neurologic disease or mortality, despite serological evidence of infection. In mice, most North American and South American strains of EEEV produce neurologic disease that resembles that associated with human and equine infections. We identified a South American strain that is unable to replicate efficiently in the brain or cause fatal disease in mice yet produces 10-fold higher viremia than virulent EEEV strains. The avirulent South American strain was also sensitive to human interferon (IFN)-α, -β, and -γ, like most South American strains, in contrast to North American strains that were highly resistant. To identify genes associated with IFN sensitivity and virulence, infectious cDNA clones of a virulent North American strain and the avirulent South American strain were constructed. Two reciprocal chimeric viruses containing swapped structural and nonstructural protein gene regions of the North American and South American strains were also constructed and found to replicate efficiently in vitro. Both chimeras produced fatal disease in mice, similar to that caused by the virulent North American strain. Both chimeric viruses also exhibited intermediate sensitivity to human IFN-α, -β, and -γ compared to that of the North American and South American strains. Virulence 50% lethal dose assays and serial sacrifice experiments further demonstrated that both structural and nonstructural proteins are important contributors to neurovirulence and viral tissue tropism. Together, the results of this study emphasize the complex and important influences of structural and nonstructural protein gene regions on EEEV virulence.
Eastern equine encephalitis virus (EEEV) is a mosquito-borne alphavirus (family Togaviridae, genus Alphavirus) that was first identified as an etiologic agent of central nervous system disease following its isolation from the brains of horses in 1933 (25, 54) and a human in 1938 (22). Sporadic epizootics in horses and outbreaks in humans have been reported ever since then in eastern North America, and equine epizootics have been identified in South America.
The EEEV possesses a single-stranded, positive-sense RNA genome of approximately 11.7 kb that is capped at the 5′ end and polyadenylated at the 3′ end. The genome encodes four nonstructural proteins (nsP1 to nsP4) that are essential for replication and polyprotein processing and three structural proteins (one capsid and two envelope proteins, E1 and E2) that are involved in receptor recognition, virus attachment and penetration, membrane fusion, and virion assembly.
The EEEV is considered the most deadly of the mosquito-borne alphaviruses due to the high case fatality rate associated with apparent infections, reaching as high as 90% in horses. In humans, the estimated fatality rate following symptomatic infection approaches 80%, and many survivors exhibit crippling sequelae such as mental retardation, convulsions, and paralysis (21, 33). Although the number of human cases is relatively low, EEEV has a strong social and economic impact in the United States due to the high cost associated with vector control and surveillance. An increase in the number of equine cases during recent years has raised public health concerns and demonstrates the continuing importance of EEEV as an emerging arboviral threat. In addition, EEEV is listed by the National Institute of Allergy and Infectious Diseases as a category B priority agent due to its virulence and its potential use as a biological weapon and the lack of a licensed vaccine or an effective treatment for human infections.
Previous studies recognized four antigenic subtypes of EEEV. One antigenic subtype comprises strains from North America and some from the Caribbean, and the remaining three are found in Central and South America (9, 14, 15, 39, 44). These subtypes exhibit important differences in their transmission cycles and virulence. In addition, the North American and South American subtypes differ by 25 to 38% at the nucleotide level (9). In general, EEEV strains from Central and South America appear to be less virulent for humans than North American strains (2). The former can occasionally cause disease and death in horses, but human infections are rarely recognized and seldom result in neurologic disease. In contrast, human infections with North American strains can sometimes result in severe disease with neurologic complications (51, 60). The cause of the apparent differences in human virulence remains unknown; however, our recent study suggests that it may be associated with viral sensitivity to interferons (IFNs) (1).
In experimentally infected laboratory mice, EEEV produces neurologic disease that resembles that following human and equine infections. Virus is detected in the brain as early as day 1 postinfection (PI) (59), and signs of disease are evident as early as days 3 to 4 PI. Clinical signs of murine disease include ruffled hair, anorexia, vomiting, lethargy, posterior limb paralysis, convulsions, and coma. Histopathological studies reveal extensive involvement of the brain, including neuronal degeneration, cellular infiltration, and perivascular cuffing, similar to the pathological changes of the central nervous system that are described in naturally infected humans (20, 59). Thus, understanding the mechanism of EEEV virulence in the mouse model could aid in the understanding of EEEV virulence in humans.
Recently, we identified a natural, murine-attenuated EEEV strain. Most North American and South American strains of EEEV are highly virulent in mice and cause mortality rates as high as 70 to 90% following subcutaneous infection. In contrast, the avirulent South American strain BeAr436087, which was isolated from a mosquito pool in Brazil, causes no mortality in adult mice even when the strain is inoculated intracranially (P. V. Aguilar, unpublished data). Similar to other South American strains, this isolate is sensitive to human IFN-α, -β, and -γ, whereas North American EEEV strains are resistant to the same human IFN-α, -β, and -γ concentrations (1).
To establish whether the structural and/or nonstructural protein genes of EEEV determine sensitivity or resistance to human IFNs as well as virulence in the mouse model, an infectious cDNA clone of a North American strain that causes 80 to 90% mortality in mice, as well as a clone of the avirulent South American strain BeAr436087, was constructed. Two reciprocal chimeric viruses containing swapped structural and nonstructural protein genome regions of the North American and South American strains were also produced. In vitro and in vivo studies with the infectious clones and the chimeric viruses reveal that both the structural and the nonstructural protein regions of EEEV contribute to mouse virulence and sensitivity to human IFNs.
MATERIALS AND METHODS
Viruses.
EEEV strains BeAr436087 and FL93-939 were provided by the University of Texas Medical Branch World Reference Center for Emerging Viruses and Arboviruses. Strain BeAr436087 was isolated in 1985 from a mosquito pool collected in Fortaleza, Brazil. The virus was passaged twice in newborn mouse brains prior to RNA extraction for this study. Strain FL93-939 was isolated from Vero cells from a 1993 Florida pool of Culiseta melanura mosquitoes and passaged once in newborn mouse brains to generate RNA. For mouse brain passages, 2- to 3-day-old mice were inoculated intracranially with each virus strain, and a 10% suspension of homogenized brain tissue was prepared after morbidity or mortality was observed. Virus stocks were titered by plaque assay with Vero cells. Table 1 summarizes the differences in nucleotide and amino acid sequences between the North American and South American EEEV strains used in this study.
TABLE 1.
Nucleotide and amino acid sequence differences between the NA strain FL93-939 and the SA strain BeAr436087
| Protein | Nucleotide difference (%) | Amino acid difference (%) |
|---|---|---|
| nsP1 | 11.6 | 7.8 |
| nsP2 | 24.2 | 8.5 |
| nsP3 | 28.9 | 24.8 |
| 2.5a | 2.5b | |
| nsP4 | 22.7 | 7 |
| C | 21.5 | 4.2 |
| E3 | 20.5 | 9.8 |
| E2 | 24.2 | 16 |
| 6K | 19 | 9 |
| E1 | 22.8 | 9.5 |
Indicates nucleotide deletions.
Indicates codon deletions.
RNA extraction.
RNA was extracted from virus stocks as described previously (64). A 250-μl volume of the 10% homogenized brain tissue was mixed with 750 μl of Trizol LS (Gibco-BRL, Gaithersburg, MD), and RNA was extracted following the manufacturer's protocol.
RT-PCR.
Reverse transcription (RT) was carried out in a 20-μl reaction mixture containing 1 μM of the antisense primer T25-NotI (−) or EEEV-7514 (−) (Table 2), 1× First Strand buffer, 1 mM of each deoxynucleoside triphosphate, 80 U RNasin RNase inhibitor (Promega, Madison, WI), and 200 U of Superscript II reverse transcriptase (Invitrogen, Carlsbad, CA). cDNA was synthesized by incubation at 42°C for 1 h. The EEEV genomes of strains FL93-939 and BeAr436087 were divided into five overlapping fragments spanning appropriate restriction sites. Briefly, the PCRs were carried out by using 2.5 U of high-fidelity Pfu Turbo polymerase (Stratagene, La Jolla, CA) in a 50-μl reaction mixture containing 1× Pfu buffer, 300 nM of sense and antisense primers (Table 2), 1 mM MgCl2, 0.2 mM of each deoxynucleoside triphosphate, and 5 μl of the cDNA reaction. PCR amplification was carried out using 30 cycles. Amplicons were gel purified using the QIAquick extraction kit (Qiagen, Valencia, CA) and, in some cases, were subcloned into the pGEM vector (Promega, Madison, WI) according to the manufacturer's protocol. Purified PCR products and clones were then sequenced using a BigDye Terminator cycle sequencing ready reaction kit (Applied Biosystems, Foster City, CA).
TABLE 2.
Primer sequences used for amplification and sequencing of the complete genome of the NA strain FL93-939 and the SA strain BeAr436087
| EEEV primera | Sequence (5′→3′) |
|---|---|
| 1V (+) | ATAGGGTATGGTGTAGAGGC |
| SA strain BeAr436087-T7-SacI (+) | GGAGAGGATAATACGACTCACTATAGATAGGGTATGGTGTAGAG |
| 366 (+) | GACAAATGTATTGCCTCTAAG |
| 900 (+) | GTRAAGAAGATTACCATCAG |
| 1948 (−) | CAATGTGGTGTAAGTAAC |
| 2050 (+) | GATATTGATGCCAGAAAATGCGTC |
| 2480 (+) | CCAAAGAAAGTGGTATTGTGTGGA |
| 3020 (+) | GCAGCGATGTTTACCAGAATAAAG |
| 3720 (−) | CTGATARTGGTGRTGCTTGT |
| 4440 (−) | GTTTCCCAYTGTTTGTCCAGACAGTAG |
| 4740 (−) | GAGAGTATGAMYAGYATYCGCTCTAAGTG |
| 4908 (+) | CTGTAATCCTGTATTTC |
| 5050 (−) | GACGTCCRGCYCCACCAG |
| 6510 (−) | TCCATTACGAACCTATCCATTG |
| 6896 (−) | AAGCGKGTSCCTGTAGGTAAGTG |
| 7514 (+) | TAACCCTCTACGGCTGAC |
| 7514 (−) | GTCAGCCGTAGAGGGTTA |
| 8860 (−) | CATTGAGCCAGGATGTAATAG |
| 8710 (+) | AGAGATTTGGAMACYCATTTCAC |
| 9210 (−) | CACTTCCTGTTGTCAATC |
| 9010 (+) | GATCAAGGCCATTATGTAGAAATGCAC |
| 9792 (+) | CAGACGACACCTTGCAAG |
| 10850 (−) | GTGCACTCAGTAATTTTACATTCCAG |
| 11599 (−) | AAAAGACAGCATTATGCG |
| T25-NotI (−) | GCGGCCGCTTTTTTTTTTTTTTTTTTTTTTTTTGAAATATTAAAAACAAAATAAAAACA |
Numbers indicate genome positions. +, sense; −, antisense.
Construction of infectious cDNA clones.
To generate the pM1-EEEV-FL93-939 (North American) and the pM1-EEEV-BeAr436087 (South American) infectious clones, the low-copy ampicillin-resistant plasmid vector pM1 (4) was used for the final construction. Fragments were sequentially cloned using appropriate, unique restriction sites. Each cloning step was confirmed by restriction digestion and sequence analysis of the junctions to ensure that no aberrant mutations were introduced during the cloning process.
Construction of chimeric viruses.
To construct the chimeric infectious clone pM1-EEEV-NA/SA, the subclone covering the entire structural protein gene region generated during the construction of the pM1-EEEV-BeAr436087 (South American [SA]) infectious clone was ligated into the pM1-EEEV-FL93-939 (North American [NA]) backbone. The 3′ untranslated genome regions (UTR) were matched to the origin of the other cis-acting elements (the 5′ end and the 26S promoter) to ensure the compatibility required for efficient alphavirus replication. For strain BeAr436087 (South American), two PCR products, (i) PCR-1, using primers EEE-SA-11,157 (CCACAAGCTTACCAGCGTAGTCACCTGC) and EEE-SA(E1)/NA(3′)-R (TATGTGGTTGACAAGATGTTAGTGTTTGTGGGTGA), and (ii) PCR-2, using primers EEE-SA(E1)/NA(3′)-F (TCACCCACAAACACTAACATCTTGTCAACCACATA) and pGEM-R (ACTCAAGCTATGCATCCAACGCGTTGGGA), were generated. A third PCR amplification was performed with primers EEE-SA(E1)/NA(3′)-F and pGEM-R, using PCR-1 and -2 products as templates in the same reaction mixture. The resultant PCR product of about 700 bp was subcloned into the pGEM vector. The fragment containing the 26S genome region and the exchanged 3′ end was replaced in the North American infectious clone by using SfiII/NotI restriction sites; the SfiII site was located a few nucleotides downstream of the capsid-encoding region; however, the beginning of the capsid protein gene was highly conserved between the two EEEV strains, and no amino acid changes within the capsid protein were introduced into the final chimera construct. Figure 1A illustrates the genetic organization of the pM1-NA/SA chimera.
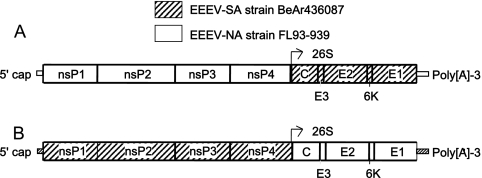
FIG. 1.
Schematic representation of the chimeric strains of EEEV. (A) The NA/SA chimera contains the 5′ UTR, the nsP1 to nsP4 genes, the subgenomic promoter (26S), and the 3′ UTR of the North American strain FL93-939 and the structural protein genes (including the capsid [C] and envelope [E2 and E1] proteins) of the South American strain BeAr436087. (B) The SA/NA chimera contains the 5′ UTR, the nsP1 to -4 genes, the subgenomic promoter (26S), and the 3′ UTR of the South American strain BeAr436087 and the structural genes (including C, E2, and E1) of the North American strain FL93-939.
To construct the second chimera, pM1-EEEV-SA/NA, the subclone covering the entire structural protein gene region of strain FL93-939 (North American strain), generated during the construction of the pM1-EEEV-FL93-939 (North American) infectious clone, was used. As described above, the 3′ end of strain FL93-939 (North American) was swapped for the 3′ end of strain BeAr436087 (South American) in the subgenomic clone. The two PCR products generated were (i) PCR-3, using primers EEE-NA-11,068 (CCACAAGCTTCACTGCAAACATCCATC) and EEE-NA(E1)/SA(3′)-R (GGTAATTTACTGCTAGTATTAATGTCTATGGAAGA), and (ii) PCR-4, using primers EEE-NA(E1)/SA(3′)-F (TCTTCCATAGACATTAATACTAGCAGTAAATTACC) and pGEM-R (ACTCAAGCTATGCATCCAACGCGTTGGGA). A third PCR amplification was performed with primers EEE-NA(E1)/SA(3′)-F and pGEM-R, using PCR-3 and -4 products as templates in the same reaction mixture. The resultant PCR product of about 700 bp was subcloned into the pGEM vector. The final plasmid, containing the 26S genomic region and the exchanged 3′ end, was engineered into the plasmid harboring the nonstructural genes of the South American strain by SfiII/NotI digestion. Figure 1B illustrates the genetic organization of the pM1-SA/NA chimeric construct. In all cases, the fragments were joined in a single ligation reaction by using high-concentration T4 DNA ligase (Invitrogen, Carlsbad, CA).
RNA transcription and transfection.
Plasmids were purified by using a Maxiprep kit (Qiagen) and linearized with NotI to produce cDNA templates for RNA synthesis. In vitro transcription was performed as previously described (4), using the T7 RNA polymerase promoter and the m7G(5′)ppp(5′)G RNA cap structure analog (New England Biolabs, Beverly, MA). The RNAs were transfected into baby hamster kidney (BHK)-21 cells by electroporation, as described previously (4, 42), and virus was harvested 18 to 24 h later when cytopathic effects were evident.
Plaque assays.
Plaque assays were performed as described previously (41), using Vero cells in either 6-well or 12-well plates. Dilutions of virus (10-fold) were adsorbed to the monolayers for 1 h at 37°C. A 3-ml overlay consisting of minimum essential medium (MEM) with 0.4% agarose was added, and the cells were incubated at 37°C for 48 h. Cell monolayers were fixed with 10% formaldehyde for 30 min to inactivate virus. After monolayers underwent fixation, agar plugs were removed, and the cells were stained with 0.25% crystal violet in 20% methanol.
Hemagglutination (HA) assays.
The assay was performed as previously described (36). Briefly, viral antigens were acetone extracted from identical amounts (PFU) of each infectious clone-derived virus and chimera before being resuspended in saline solution (pH 9.0). Serial dilutions of the viral antigens were then assayed for their abilities to agglutinate goose red blood cells at pH 6.0 to 7.0.
Virus replication in vitro.
Vero (monkey) and C710 (mosquito) cells were seeded into 12-well plates and infected at a multiplicity of infection (MOI) of 0.1 or 10 PFU/cell. Medium was removed from the cells, and viruses were allowed to adsorb for 1 h at 37°C. After cells were incubated, they were washed twice with 0.09% NaCl, and fresh medium was added. Supernatant fluids were collected at 0, 8, 24, 32, and 48 h PI and titrated by plaque assay.
IFN sensitivity assays.
The IFN assay was performed as previously described (1). Initially, the sensitivities of the North American and South American strains to IFNs were evaluated at a range of different concentrations. Selected concentrations were chosen for detailed studies because the differences in sensitivity between the North American and South American strains were more evident and because replication of both North American and South American strains was still detected. Briefly, Vero cells were seeded in 12-well plates and pretreated for 24 h with either 50 IU/ml of human IFN-α, 5 IU/ml of human IFN-β, or 25 IU/ml of human recombinant IFN-γ (National Institutes of Health, Bethesda, MD). After incubation, samples of the culture media containing IFN were removed, the cells were washed three times with phosphate-buffered saline (PBS) to remove excess IFN, and 10,000 PFU of EEEV was added to IFN-treated cells in triplicate. Negative controls consisted of infected cells not exposed to IFN. At 24 h and 48 h PI, the supernatant fluid was collected, the cells were washed twice with PBS, and new medium containing the appropriate concentration of IFN was added to the plates. Collected supernatant fluids were titrated by plaque assay on Vero cells.
Mouse infections.
For viremia and mortality comparisons, parental, infectious clone-derived and chimeric viruses (1,000 PFU) were inoculated subcutaneously into 5- to 6-week-old NIH Swiss mice (10 mice/cohort) (Harlan Laboratories, Indianapolis, IN). Five mice were bled at 24, 48, and 72 h PI, and the sera were titrated for virus by plaque assay. All animals were monitored daily for clinical signs of disease, including fever, lethargy, paralysis, or death.
For 50% lethal dose (LD50) experiments, 6-week-old NIH Swiss mice (10 mice/cohort) were infected subcutaneously with doses ranging from 1 to 6 log10 PFU of virus. Animals were monitored daily for survival, and the LD50 values were calculated using the Reed and Muench method (43).
To examine virus replication levels in the brain and other organs, 6-week-old NIH Swiss mice were inoculated subcutaneously (1,000 PFU) with infectious clone-derived and chimeric viruses (15 mice/cohort). At days 1, 2, 3, 5, and 7 PI, three mice/cohort were bled and perfused with PBS, and the brains, hearts, lungs, livers, spleens, and kidneys were collected from each sacrificed mouse for virus titration. Depending on the virulence of the virus, there were sometimes only one or two mice available on the day of sacrifice.
Statistical analysis.
For viral replication and viremia titers, statistical comparisons were performed using either Student's t test or one-way analysis of variance (ANOVA), followed by Dunn's multiple comparison test. Survival data were analyzed by using the log rank test (GraphPad; Prism, San Diego, CA). For the IFN sensitivity assay, the reduction in virus titer was determined by dividing the mean log10 viral titer of untreated samples by the log10 viral titers of the IFN-treated samples. Thus, the higher the bar, the more sensitive the virus was to the effects of IFN. One-way analysis of variance followed by Tukey's multiple comparison test was used to compare IFN sensitivities between viruses at 24 and 48 h PI (GraphPad; InStat, San Diego, CA). Values of P ≤ 0.05 were considered significant.
RESULTS
Characterization of viruses derived from infectious clones.
In vitro replication of the North American and South American infectious clone-derived EEEVs was compared to that of the parental viruses at 0, 8, 24, 32, and 48 h PI in monkey (Vero)-derived and mosquito (C710)-derived cells. There were no significant differences in virus production between the pM1-EEEV-FL93-939 (North American) infectious clone-derived virus and the parental virus in Vero or C710 cells (data not shown). Similarly, there were no significant differences in virus yield between the pM1-EEEV-BeAr436087 (South American) infectious clone virus and the parental virus in Vero and C710 cells (data not shown).
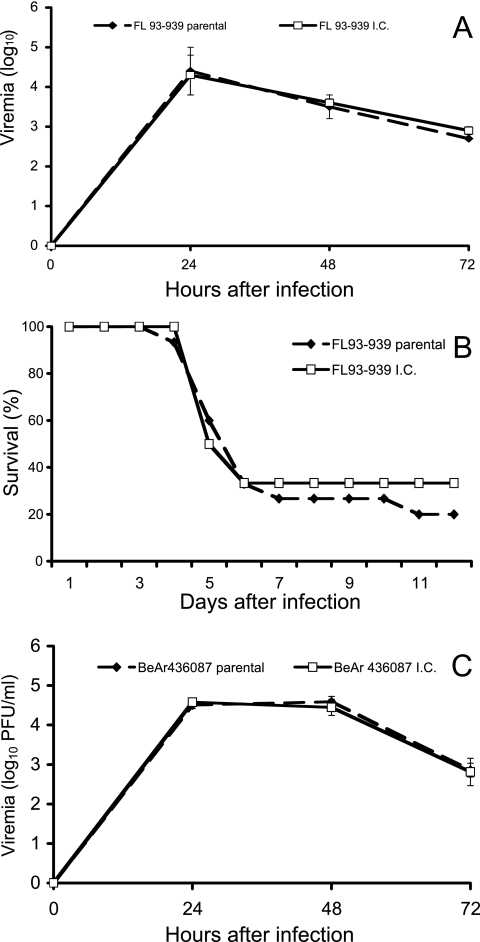
To compare the in vivo replication of the parental and the infectious clone-derived viruses, cohorts of five mice were infected subcutaneously with 1,000 PFU. Mice were bled daily, and viremia was determined by plaque assay. Figure 2A shows the viremia associated with NA-FL93-939 parental and infectious clone-derived virus infections; there was no significant difference. All animals infected with strain NA-FL93-939 developed clinical signs of disease beginning on day 3 PI. Animals became lethargic and anorexic, and ruffling of hair was evident, consistent with previously published observations of murine EEEV infection (59). By day 5 PI, mice developed more evidence of central nervous system involvement, and posterior limb paralysis was observed with the majority of the animals, which were euthanized. Figure 2B shows the survival of mice infected with the NA-FL93-939 strain, which killed 70 to 80% of the animals; there was no significant difference between the survival of mice infected with the parental virus and those infected with the infectious clone-derived viruses of this strain.
FIG. 2.
Survival and in vivo replication of parental and infectious clone (I.C.)-derived EEEVs in 5- to 6-week-old NIH Swiss mice. (A) Viremia in mice after subcutaneous infection (1,000 PFU) with either the North American parental strain FL93-939 or the North American I.C.-derived virus (5 mice/cohort). (B) Survival of mice infected with either the North American parental strain FL93-939 or the North American I.C.-derived virus in which cohorts of 10 mice were infected subcutaneously with 1,000 PFU. (C) Viremia in mice after subcutaneous infection (1,000 PFU) with either the South American parental strain BeAr436087 or the South American I.C.-derived virus (5 mice/cohort). Error bars indicate the standard deviations (panels A and C).
Figure 2C shows the viremia of SA-BeAr436087 parental and infectious clone-derived viruses; there was no significant difference in viremia between the SA-BeAr436087 parental and the infectious clone-derived viruses. Unlike mice infected with the NA-FL93-939 strain, mice infected with the SA-BeAr436087 strain did not develop detectable disease and survived until the experiment was terminated on day 12 (data not shown). In summary, the in vitro and in vivo data demonstrated that the EEEV infectious clones produced viruses that replicated to levels that were similar to those of the parental viruses and caused similar clinical disease in mice.
Construction and in vitro characterization of the NA/SA and SA/NA chimeric viruses.
Previously, we demonstrated that the North American strain FL93-939 is highly resistant to the antiviral effects of human IFN-α, -β and -γ, whereas the South American strain BeAr436087 is sensitive to the same IFN treatment in Vero cells (1). To localize the genetic determinants of human IFN resistance exhibited by the EEEV strain FL93-939 to the structural and/or nonstructural protein regions of the viral genome, reciprocal chimeric viruses were constructed with the South American strain BeAr436087. The NA/SA chimera contained the 5′ UTR, nonstructural protein genes, the subgenomic promoter, and the 3′ UTR of the North American strain FL93-939, and the structural protein genes of the South American strain BeAr436087; the SA/NA chimera contained the 5′ UTR, nonstructural genes, the subgenomic promoter, and the 3′ UTR of the South American strain BeAr436087, and the structural protein genes of North American strain FL93-939 (Fig. 1).
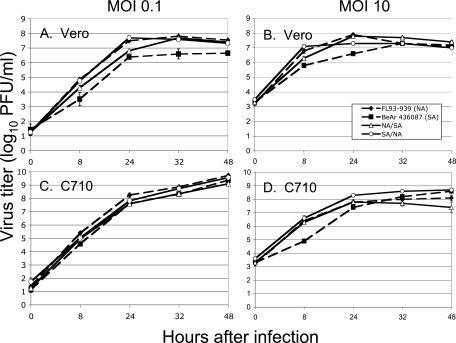
The in vitro replication of the NA/SA and the SA/NA chimeras was compared to the replication of infectious clone-derived viruses FL93-939 and BeAr436087 in Vero cells (Fig. 3A and B) and C710 (Fig. 3C and D), using high (10) and low (0.1) MOIs. Some differences in replication were observed between the North American and South American strains at 8 and 24 h PI with Vero cells at high and low MOIs (P < 0.05). However, both the NA/SA and the SA/NA chimeras replicated efficiently in Vero and C710 cells and their replication values were similar to those of the North American and South American infectious clone-derived viruses.
FIG. 3.
In vitro replication of infectious clone (I.C.)-derived and chimeric strains of North American and South American EEEVs. Infectious clone (I.C.)-derived strains included the North American strain FL93-939 and the South American strain BeAr 436087, and the chimeric strains included NA/SA and SA/NA strains. Three replicate assays per virus strain were performed at MOIs of 0.1 (panels A and C) and 10 (panels B and D) PFU/cell in Vero (panels A and B) and C710 (panels C and D) cells. Error bars indicate the standard deviations.
Sensitivity of infectious clone-derived viruses and chimeric EEE viruses to human IFNs.
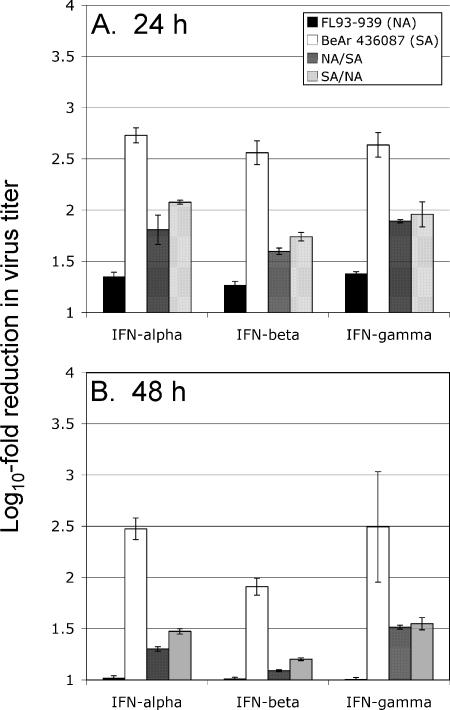
Viruses rescued from the North American and South American EEEV infectious clones behaved like their parental counterparts and did not differ significantly in their sensitivities to human IFNs (data not shown). Consistent with previous findings (1), the South American strain BeAr436087 was significantly more sensitive to IFN-α, -β, and -γ at 24 and 48 h PI than the North American strain FL93-939 was (Fig. 4).
FIG. 4.
Sensitivity of infectious clone (I.C.)-derived and chimeric strains of North American and South American EEEVs to IFNs. Vero cells were initially treated with human IFN-α, -β, or -γ, and 24 h later, the cells were infected in triplicate with either the North American strain FL93-939, the South American strain BeAr436087, the NA/SA chimera, or the SA/NA chimera at an MOI of 1.0 PFU/cell. Supernatants were collected from mock-treated and IFN-treated cultures at 24 and 48 h PI, and the virus titer was measured in the supernatants by plaque assay. The y axis represents the reduction (log10-fold) of virus replication in Vero cells at 24 (panel A) and 48 (panel B) h after treatment with IFN-α, -β, or -γ (as shown on the x axis). Error bars indicate standard deviations.
To ascertain whether the determinants of IFN sensitivity/resistance are located in the nonstructural or the structural protein region of the EEEV genome, chimeric viruses harboring reciprocal nonstructural and structural proteins of the North American and South American strains were tested for their sensitivities to human IFNs. Overall, the chimeric viruses showed intermediate sensitivity to human IFNs compared to that of the North American parent strain FL93-939 and the South American parent strain BeAr436087, at MOIs of 0.1 (data not shown) and 1.0 (Fig. 4). At 24 and 48 h PI, there were no significant differences in IFN sensitivities between the chimeric viruses, but the reduction in virus yield in the IFN-treated cells PI with either the NA/SA or the SA/NA chimeric virus was, in most cases, significantly different from that of the North American and South American viruses. These results suggest that both the structural and the nonstructural proteins of EEEV were responsible for differences in IFN sensitivity/resistance during infection.
Comparison of infectious virus titers and HA activity of EEEVs.
To eliminate the possibility of differences in plaque-forming efficiency among the infectious clone-derived and chimeric EEEVs, we used both infectious and noninfectious assays to quantify the amounts of virus used for the mouse infections. Equal PFU amounts of infectious virus (approximately 8.6 log10) exhibited similar HA activity, a surrogate for the total quantities of the E1 protein in the virus preparations. Parental and chimeric viruses agglutinated red blood cells at the same pH (6.0), with identical titers (1:320), strongly suggesting that the viruses used for this study had comparable particle/PFU ratios.
Viremia and survival of mice infected with chimeric EEEV.
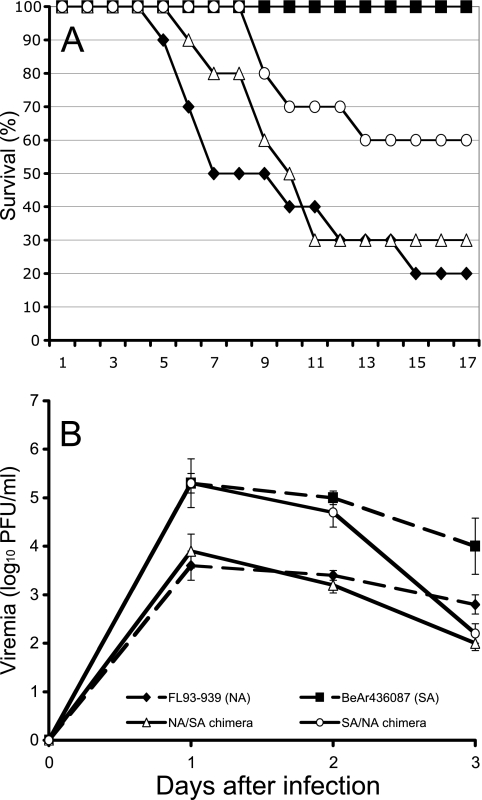
In experimentally infected laboratory mice, the South American strain BeAr436087 is avirulent but induces 10-fold higher viremia than other EEEV strains (1). In contrast, the North American strain FL93-939, like most EEEV strains, causes about 80% mortality in adult mice after subcutaneous infection. To study the contributions of the structural and nonstructural protein genome regions to the virulence phenotypes, cohorts of 10 mice were infected with 1,000 PFU of the chimeric viruses. Both chimeras resulted in paralysis and death of mice, beginning on either day 6 or day 9 PI (Fig. 5A). Although no significant differences in mortality between the chimeras and the North American virus were observed, differences in median survival times were evident (with North American strain, 8.5 days; with NA/SA chimera, 10.5 days; with SA/NA chimera, >17 days), suggesting that a larger cohort may have revealed small but significant differences.
FIG. 5.
Survival and viremia of 6-week-old NIH Swiss mice PI with infectious clone (I.C.)-derived and chimeric strains of North American and South American EEEVs. Mice were infected subcutaneously (1,000 PFU) with either the North American strain FL93-939, the South American strain BeAr436087, the NA/SA chimera, or the SA/NA chimera. (A) Survival (10 mice/cohort). (B) Viremia (5 mice/cohort). Error bars indicate standard deviations.
Viremia induced by the NA/SA strain was comparable to that produced by the North American parental strain, reaching 3.6 to 3.9 log10 PFU/ml at 24 h PI (Fig. 5B). Interestingly, serum titers for the SA/NA chimera were similar to those of the South American parental virus. Both the SA/NA chimera and the South American parental virus induced more than 10-fold higher viremia (peak titer, 5.3 log10 PFU/ml) in mice than the North American strain and the reciprocal NA/SA chimera (P < 0.05). These results suggest that viremia levels do not correlate with EEEV neurovirulence, since the avirulent strain BeAr436087 induced more than 10-fold higher viremia than the virulent strain FL93-939. Similarly, the NA/SA and SA/NA chimeras differed by 14-fold in peak viremia levels yet exhibited comparable virulence in mice.
LD50 of infectious clone-derived and chimeric EEEVs.
To elucidate more precisely the relative contribution of the nonstructural and structural proteins to virulence, mice were infected subcutaneously with a wide range of doses of the infectious clone-derived and chimeric viruses, and mortality was monitored daily. The North American strain had the highest virulence phenotype, with an LD50 of 1.5 log10 PFU, whereas the NA/SA chimera had an LD50 of 2.6 log10 PFU. The reciprocal SA/NA chimera was less virulent, with an LD50 of 5.0 log10 PFU, more than a 3 log10 attenuation compared to that of the North American strain. The South American strain failed to cause fatal disease in the mice, even at the highest virus inoculum tested (6 log10 PFU). These results suggest that the nonstructural proteins of the North American strain are important determinants of neurovirulence.
Replication of infectious clone-derived and chimeric EEEVs in different organs of the mouse.
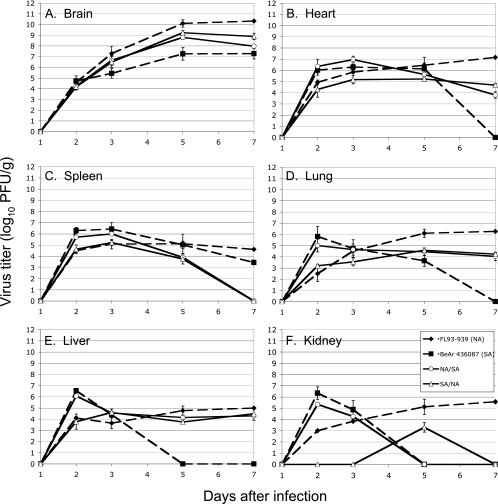
To compare the replication kinetics of the infectious clone-derived and the chimeric viruses in the brain and other organs of mice, serial sacrifice experiments were performed (Fig. 6). Although viremia was detected at day 1 PI, no viruses were detected in the tissues at this time. Possible reasons for this discrepancy may be that replication in the tissues was below the limit of detection (2 log10 PFU/g) or because replication was occurring in other tissues not assayed in this study (59). In the brain, the North American strain replicated to a 30-fold higher titer than the South American strain by day 5 PI, whereas both chimeras replicated to intermediate titers compared to that of the North American and South American parental strains (Fig. 6A). At days 1 and 2 PI, there were no significant differences in mean viral titers in the brain between virus strains. On day 3 PI, there was only a significant difference between the North American and the South American strains. On day 5 PI, there were significant differences between the North American and the South American strains, the North American strain and both of the chimeras, and the South American strain and the SA/NA chimera. By day 7 PI, two NA/SA- and two SA/NA-infected mice were alive, and only one North American-infected mouse survived.
FIG. 6.
In vivo replication of infectious clone (I.C.)-derived and chimeric strains of North American and South American EEEVs in various organs of 6-week-old NIH Swiss mice. Mice were infected subcutaneously (1,000 PFU) with the North American strain FL93-939, the South American strain BeAr436087, the NA/SA chimera, or the SA/NA chimera (15 mice/cohort). At days 1, 2, 3, 5, and 7 PI, 1 to 3 mice/cohort were sacrificed, and the brain (A), heart (B), spleen (C), lung (D), liver (E), and kidney (F) were collected and titrated for virus by plaque assay. The limit of detection for the assay is 2 log10 PFU/g. Error bars indicate standard deviations.
Interestingly, the South American strain and the NA/SA chimera replicated to similarly high titers in the heart, spleen, lung, liver, and kidney by days 2 and 3 PI (Fig. 6B to F). Animals infected with the South American and the NA/SA strains were found to either completely or partially clear the virus from these organs by day 5 or day 7 PI. Compared to the North American and chimeric viruses, the South American virus was effectively cleared from the heart, lung, liver, and kidney by day 5 or 7, but the virus remained present in the spleen until day 7 PI.
Compared to the South American and the NA/SA viruses, the North American and the SA/NA viruses replicated to lower titers by days 2 and 3 PI (Fig. 6B to F). In most cases, the North American virus continued to replicate in the heart, spleen, lung, liver, and kidney to high titers on days 5 and 7 PI compared to those of the SA/NA virus. In the same organs, the SA/NA virus titer either remained the same on days 5 and 7 PI (Fig. 6B, D, and E) or was completely cleared by day 7 PI (Fig. 6C and F). Interestingly, the replication of the SA/NA virus in the kidney did not occur until day 5 PI, before being cleared by day 7 PI.
The results of this experiment suggest a complex interaction between EEEV and the host, in that virus replication in different tissues during the course of infection appeared to be influenced by both the structural and nonstructural protein genes of the virus.
DISCUSSION
In North America, EEEV is responsible for sporadic cases of neurological disease that are associated with high morbidity and mortality rates in humans (up to 80%) and horses (70 to 90%) (49, 62). Thus, EEEV is considered one of the most deadly arboviruses because of the high mortality rate in apparently infected individuals and because many survivors develop permanent sequelae, including motor nerve paralysis, mental retardation, and seizures. However, little is known about the mechanism of EEEV pathogenesis and, more importantly, the genetic determinants that are crucial for neurovirulence and sensitivity to human IFNs. This information is important for developing effective measures for treatment and vaccination against EEE.
Similar to our findings, previous work with other alphaviruses has also suggested that both structural and nonstructural genes are important for virulence (7, 18, 23, 26, 28, 29, 35, 41, 45, 48, 50, 55, 65). Most of these studies focused on the structural proteins, and in particular, the E2 glycoprotein. The contributions to virulence of several mutations in the E1 and E2 glycoproteins of Venezuelan equine encephalitis virus (VEEV) and Sindbis virus (SINV) in mice have been well characterized (5, 7, 18, 29). Mutations in the E2 glycoprotein of SINV, VEEV, and Ross River virus (RRV) result in enhanced binding to heparin sulfate in vitro and are associated with rapid clearance of viremia and decreased virulence in mice after subcutaneous but not intracranial infection (5, 7, 12, 13, 31, 34, 46). Further studies are needed to rule out the possible role of heparin sulfate binding in the attenuation of the South American EEEV strains.
A single mutation in the E2 glycoprotein of the VEEV Trinidad donkey (TRD) strain confers a delay in replication in mice and a reduction in pathogenesis (18). In addition, two viral determinants (glycoproteins and the 5′ UTR) are responsible for the IFN-resistant phenotype of the TRD strain (52). The importance of the 5′ UTR in VEEV virulence was demonstrated more conclusively when a virus carrying a single mutation at nucleotide position 3 resulted in avirulence in mice and reduced replication in cell culture (65). Other studies with chimeric viruses have demonstrated that the E2 glycoprotein defines the enzootic and epizootic VEEV subtypes as well as mosquito-borne virus infectivity (10, 11, 28, 63). Both structural and nonstructural protein genes of VEEV have also been implicated as determinants of viral virulence in guinea pigs (27).
Several studies with SINV have also demonstrated that amino acid changes in the envelope glycoproteins are associated with changes in neurovirulence (19, 38, 40, 55, 56). Single mutations in the E1 and E2 glycoproteins of SINV result in mutants with an attenuated phenotype, with neonatal mice (17, 40). More recently, studies of Semliki Forest virus (SFV) and SINV have also demonstrated the importance of nsP2 and nsP3 in alphavirus virulence. Mutation of the opal termination codon near the C terminus of an arginine codon increases the virulence of an SFV strain previously identified as avirulent, and several amino acid changes in the nsP3 gene fully restore neurovirulence in this attenuated strain (57). Similarly, mutations in nsP1 and nsP2 dramatically increase the virulence of SFV, further supporting the role of the nonstructural proteins in SFV pathogenesis (58). Moreover, in SINV, nsP2 plays a role in suppressing the IFN response in infected cells by minimizing virus visibility (23).
Although these studies provide important insights about the role of structural and nonstructural genes in alphavirus virulence, very little is known about the role of these genes in EEEV pathogenesis. Both VEEV and EEEV cause encephalitis in the murine model. However, the diseases are different: EEEV is primarily neurotropic, whereas VEEV begins with a lymphotropic phase that progresses to a neurotropic phase. VEEV also causes systemic infection with pathological lesions in the lung, lymphoid tissues of the gastrointestinal tract, spleen, and peripheral lymph nodes (32). In addition, the mechanisms by which these viruses enter the central nervous system appear to differ. VEEV invades the murine brain via the olfactory bulb (16), whereas EEEV may cross the blood-brain barrier by passive transfer or within infected leukocytes (59). EEEV also causes a different disease than SFV and SINV do in the mouse model. Therefore, the extrapolation of genetic studies among alphaviruses may not necessarily predict the genetic determinants of EEEV virulence.
To identify gene regions of EEEV that are associated with sensitivity to human IFNs and neurovirulence in mice, we generated infectious clones from a highly virulent North American strain and a naturally attenuated South American strain as backbones, and two chimeric EEEVs were constructed. Both chimeras showed an intermediate level of sensitivity to human IFN-α, -β and -γ, suggesting that both the structural and the nonstructural genome regions of EEEV determine sensitivity to IFNs. To our knowledge, this is the first evidence for the role of both the structural and the nonstructural genes of an alphavirus as the determinants of IFN sensitivity. Recently, Frolova et al. (23) showed that nsP2 plays a role in suppressing the IFN response in SINV-infected cells. However, EEEV and VEEV, both New World alphaviruses, appear to use the capsid for inhibiting the IFN response and host cell gene expression (3, 24). Whether nsP2 and/or the capsid is also involved in conferring EEEV sensitivity or resistance to human IFNs remains to be elucidated using gene-specific chimeras. Previous studies have shown the importance of the protein kinase R pathway in controlling alphavirus replication (6, 47, 66), and thus, the question of whether protein kinase R and/or other recently identified antiviral proteins such as ISG15 (37) and ZAP (8, 30) have a role in inhibiting replication of the avirulent South American strain in vivo deserves further investigation.
The nonstructural proteins are essential components during alphavirus RNA replication (53). Our chimera data suggest that the EEEV nonstructural proteins control the level of viral replication in mice. The chimera harboring the nonstructural protein genes of the avirulent South American strain induced levels of viremia similar to those of the avirulent South American strain. Both viruses produced more than a 10-fold higher peak of viremia in mice than the reciprocal NA/SA chimera and the virulent North American strain. Similarly, the chimera harboring the nonstructural genes of the virulent North American strain produced levels of viremia that were comparable to that of the virulent North American strain.
Independently of viremia titers and IFN sensitivity, both EEEV chimeras were equally capable of inducing fatal neurologic disease in mice. These results suggest that both the structural and the nonstructural genome regions of EEEV are important determinants of virulence, in agreement with virulence characterizations of chimeric SIN/EEEV vaccine candidates that include structural EEEV protein genes from either the FL93-939 or the BeAr436087 strain (61). These results also corroborate previous observations obtained with chimeric VEEVs (41). In those studies, the epidemic subtype IAB VEEV caused 100% mortality in guinea pigs, whereas the enzootic IE strain was nonlethal. Similar to our results, chimeras with swapped structural and nonstructural protein genes also revealed that both the structural and the nonstructural genome regions are important determinants of guinea pig virulence. Thus, both studies underscore the importance of both nonstructural and structural protein gene regions in neurovirulence.
Future studies with chimeric viruses will investigate more highly defined genetic determinants in the structural and nonstructural gene regions of EEEV in order to provide a clearer understanding of the mechanism and determinants of neurovirulence. This information will be important to consider during the development of live-attenuated EEEV vaccines and antiviral treatments.
Acknowledgments
We thank Amelia Travassos da Rosa for technical assistance with the HA assay and the National Institute of Health (NIAID Reference Reagent Repository) for providing the interferon reagents.
This work was supported by a grant to S.C.W. from NIAID through the Western Regional Center of Excellence for Biodefense and Emerging Infectious Diseases Research, NIH grant number U54 AI057156. P.V.A. and A.P.A. were supported by the James W. McLaughlin fellowship fund.
Footnotes
Published ahead of print on 19 March 2008.
REFERENCES
- 1.Aguilar, P. V., S. Paessler, A. S. Carrara, S. Baron, J. Poast, E. Wang, A. C. Moncayo, M. Anishchenko, D. Watts, R. B. Tesh, and S. C. Weaver. 2005. Variation in interferon sensitivity and induction among strains of Eastern equine encephalitis virus. J. Virol. 7911300-11310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aguilar, P. V., R. M. Robich, M. J. Turell, M. L. O'Guinn, T. A. Klein, A. Huaman, C. Guevara, Z. Rios, R. B. Tesh, D. M. Watts, J. Olson, and S. C. Weaver. 2007. Endemic Eastern equine encephalitis in the Amazon region of Peru. Am. J. Trop. Med. Hyg. 76293-298. [PubMed] [Google Scholar]
- 3.Aguilar, P. V., S. C. Weaver, and C. F. Basler. 2007. Capsid protein of Eastern equine encephalitis virus inhibits host cell gene expression. J. Virol. 813866-3876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anishchenko, M., S. Paessler, I. P. Greene, P. V. Aguilar, A. S. Carrara, and S. C. Weaver. 2004. Generation and characterization of closely related epizootic and enzootic infectious cDNA clones for studying interferon sensitivity and emergence mechanisms of Venezuelan equine encephalitis virus. J. Virol. 781-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bear, J. S., A. P. Byrnes, and D. E. Griffin. 2006. Heparin-binding and patterns of virulence for two recombinant strains of Sindbis virus. Virology 347183-190. [DOI] [PubMed] [Google Scholar]
- 6.Berlanga, J. J., I. Ventoso, H. P. Harding, J. Deng, D. Ron, N. Sonenberg, L. Carrasco, and C. de Haro. 2006. Antiviral effect of the mammalian translation initiation factor 2alpha kinase GCN2 against RNA viruses. EMBO J. 251730-1740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bernard, K. A., W. B. Klimstra, and R. E. Johnston. 2000. Mutations in the E2 glycoprotein of Venezuelan equine encephalitis virus confer heparan sulfate interaction, low morbidity, and rapid clearance from blood of mice. Virology 27693-103. [DOI] [PubMed] [Google Scholar]
- 8.Bick, M. J., J. W. Carroll, G. Gao, S. P. Goff, C. M. Rice, and M. R. MacDonald. 2003. Expression of the zinc-finger antiviral protein inhibits alphavirus replication. J. Virol. 7711555-11562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brault, A. C., A. M. Powers, C. L. Chavez, R. N. Lopez, M. F. Cachon, L. F. Gutierrez, W. Kang, R. B. Tesh, R. E. Shope, and S. C. Weaver. 1999. Genetic and antigenic diversity among Eastern equine encephalitis viruses from North, Central, and South America. Am. J. Trop. Med. Hyg. 61579-586. [DOI] [PubMed] [Google Scholar]
- 10.Brault, A. C., A. M. Powers, E. C. Holmes, C. H. Woelk, and S. C. Weaver. 2002. Positively charged amino acid substitutions in the E2 envelope glycoprotein are associated with the emergence of Venezuelan equine encephalitis virus. J. Virol. 761718-1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brault, A. C., A. M. Powers, D. Ortiz, J. G. Estrada-Franco, R. Navarro-Lopez, and S. C. Weaver. 2004. Venezuelan equine encephalitis emergence: enhanced vector infection from a single amino acid substitution in the envelope glycoprotein. Proc. Natl. Acad. Sci. USA 10111344-11349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Byrnes, A. P., and D. E. Griffin. 1998. Binding of Sindbis virus to cell surface heparan sulfate. J. Virol. 727349-7356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Byrnes, A. P., and D. E. Griffin. 2000. Large-plaque mutants of Sindbis virus show reduced binding to heparan sulfate, heightened viremia, and slower clearance from the circulation. J. Virol. 74644-651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Calisher, C. H., R. E. Shope, W. Brandt, J. Casals, N. Karabatsos, F. A. Murphy, R. B. Tesh, and M. E. Wiebe. 1980. Proposed antigenic classification of registered arboviruses. Intervirology 14229-232. [DOI] [PubMed] [Google Scholar]
- 15.Casals, J. 1964. Antigenic variants of Eastern equine encephalitis virus. J. Exp. Med. 119547-565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Charles, P. C., E. Walters, F. Margolis, and R. E. Johnston. 1995. Mechanism of neuroinvasion of Venezuelan equine encephalitis virus in the mouse. Virology 208662-671. [DOI] [PubMed] [Google Scholar]
- 17.Davis, N. L., F. J. Fuller, W. G. Dougherty, R. A. Olmsted, and R. E. Johnston. 1986. A single nucleotide change in the E2 glycoprotein gene of Sindbis virus affects penetration rate in cell culture and virulence in neonatal mice. Proc. Natl. Acad. Sci. USA 836771-6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Davis, N. L., N. Powell, G. F. Greenwald, L. V. Willis, B. J. Johnson, J. F. Smith, and R. E. Johnston. 1991. Attenuating mutations in the E2 glycoprotein gene of Venezuelan equine encephalitis virus: construction of single and multiple mutants in a full-length cDNA clone. Virology 18320-31. [DOI] [PubMed] [Google Scholar]
- 19.Dropulic, L. K., J. M. Hardwick, and D. E. Griffin. 1997. A single amino acid change in the E2 glycoprotein of Sindbis virus confers neurovirulence by altering an early step of virus replication. J. Virol. 716100-6105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Farber, S., A. Hill, M. L. Connerly, and J. H. Dingle. 1940. Encephalitis in infants and children caused by the virus of the Eastern variety of equine encephalitis. JAMA 1141725-1731. [Google Scholar]
- 21.Feemster, R. F., and W. Haymaker. 1958. Eastern equine encephalitis. Neurology 8882-883. [DOI] [PubMed] [Google Scholar]
- 22.Fothergill, L. D., J. H. Dingle, and J. J. Fellow. 1938. A fatal disease of pigeons caused by the virus of the Eastern variety of equine encephalomyelitis. Science 88549-550. [DOI] [PubMed] [Google Scholar]
- 23.Frolova, E. I., R. Z. Fayzulin, S. H. Cook, D. E. Griffin, C. M. Rice, and I. Frolov. 2002. Roles of nonstructural protein nsP2 and alpha/beta interferons in determining the outcome of Sindbis virus infection. J. Virol. 7611254-11264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Garmashova, N., R. Gorchakov, E. Volkova, S. Paessler, E. Frolova, and I. Frolov. 2007. The Old World and New World alphaviruses use different virus-specific proteins for induction of the transcriptional shutoff. J. Virol. 812472-2484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Giltner, L. T., and M. S. Shahan. 1933. The 1933 outbreak of infectious equine encephalomyelitis in the Eastern states. North Am. Vet. 1425-27. [Google Scholar]
- 26.Glasgow, G. M., H. M. Killen, P. Liljestrom, B. J. Sheahan, and G. J. Atkins. 1994. A single amino acid change in the E2 spike protein of a virulent strain of Semliki Forest virus attenuates pathogenicity. J. Gen. Virol. 75663-668. [DOI] [PubMed] [Google Scholar]
- 27.Greene, I. P., S. Paessler, M. Anishchenko, D. R. Smith, A. C. Brault, I. Frolov, and S. C. Weaver. 2005. Venezuelan equine encephalitis virus in the guinea pig model: evidence for epizootic virulence determinants outside the E2 envelope glycoprotein gene. Am. J. Trop. Med. Hyg. 72330-338. [PubMed] [Google Scholar]
- 28.Greene, I. P., S. Paessler, L. Austgen, M. Anishchenko, A. C. Brault, R. A. Bowen, and S. C. Weaver. 2005. Envelope glycoprotein mutations mediate equine amplification and virulence of epizootic Venezuelan equine encephalitis virus. J. Virol. 799128-9133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Grieder, F. B., N. L. Davis, J. F. Aronson, P. C. Charles, D. C. Sellon, K. Suzuki, and R. E. Johnston. 1995. Specific restrictions in the progression of Venezuelan equine encephalitis virus-induced disease resulting from single amino acid changes in the glycoproteins. Virology 206994-1006. [DOI] [PubMed] [Google Scholar]
- 30.Guo, X., J. W. Carroll, M. R. Macdonald, S. P. Goff, and G. Gao. 2004. The zinc finger antiviral protein directly binds to specific viral mRNAs through the CCCH zinc finger motifs. J. Virol. 7812781-12787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Heil, M. L., A. Albee, J. H. Strauss, and R. J. Kuhn. 2001. An amino acid substitution in the coding region of the E2 glycoprotein adapts Ross River virus to utilize heparan sulfate as an attachment moiety. J. Virol. 756303-6309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jackson, A. C., S. K. SenGupta, and J. F. Smith. 1991. Pathogenesis of Venezuelan equine encephalitis virus infection in mice and hamsters. Vet. Pathol. 28410-418. [DOI] [PubMed] [Google Scholar]
- 33.Johnston, R. E., and C. J. Peters. 1996. Alphaviruses, p. 843-898. In B. N. Fields, D. M. Knipe, and P. Howley (ed.), Fields virology, 3rd ed. Lippincott-Raven Publishers, Philadelphia, PA.
- 34.Klimstra, W. B., Ryman, K. D., and R. E. Johnston. 1998. Adaptation of Sindbis virus to BHK cells selects for use of heparan sulfate as an attachment receptor. J. Virol. 727357-7366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kobiler, D., C. M. Rice, C. Brodie, A. Shahar, J. Dubuisson, M. Halevy, and S. Lustig. 1999. A single nucleotide change in the 5′ noncoding region of Sindbis virus confers neurovirulence in rats. J. Virol. 7310440-10446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lennette, E. H., D. Lennette, and E. T. Lennette. 1995. Diagnostic procedures for viral, rickettsial, and chlamydial infections. American Public Health Association, Washington, DC.
- 37.Lenschow, D. J., C. Lai, N. Frias-Staheli, N. V. Giannakopoulos, A. Lutz, T. Wolff, A. Osiak, B. Levine, R. E. Schmidt, A. Garcia-Sastre, D. A. Leib, A. Pekosz, K.-P. Knobeloch, I. Horak, and H. W. Virgin. 2007. IFN-stimulated gene 15 functions as a critical antiviral molecule against influenza, herpes, and Sindbis viruses. Proc. Natl. Acad. Sci. USA 1041371-1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lustig, S., A. C. Jackson, C. S. Hahn, D. E. Griffin, E. G. Strauss, and J. H. Strauss. 1988. Molecular basis of Sindbis virus neurovirulence in mice. J. Virol. 622329-2336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Morris, C. 1988. Eastern equine encephalomyelitis, p. 1-36. In T. P. Monath (ed.), The arboviruses: epidemiology and ecology, vol. III. CRC Press, Boca Raton, FL. [Google Scholar]
- 40.Polo, J. M., and R. E. Johnston. 1990. Attenuating mutations in glycoproteins E1 and E2 of Sindbis virus produce a highly attenuated strain when combined in vitro. J. Virol. 644438-4444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Powers, A. M., A. C. Brault, R. M. Kinney, and S. C. Weaver. 2000. The use of chimeric Venezuelan equine encephalitis viruses as an approach for the molecular identification of natural virulence determinants. J. Virol. 744258-4263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Powers, A. M., K. I. Kamrud, K. E. Olson, S. Higgs, J. O. Carlson, and B. J. Beaty. 1996. Molecularly engineered resistance to California serogroup virus replication in mosquito cells and mosquitoes. Proc. Natl. Acad. Sci. USA 934187-4191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Reed, L. J., and H. Muench. 1938. A simple method of estimating fifty percent endpoints. Am. J. Hyg. 27493-497. [Google Scholar]
- 44.Roehrig, J. T., A. R. Hunt, G. J. Chang, B. Sheik, R. A. Bolin, T. F. Tsai, and D. W. Trent. 1990. Identification of monoclonal antibodies capable of differentiating antigenic varieties of Eastern equine encephalitis viruses. Am. J. Trop. Med. Hyg. 42394-398. [DOI] [PubMed] [Google Scholar]
- 45.Russell, D. L., J. M. Dalrymple, and R. E. Johnston. 1989. Sindbis virus mutations which coordinately affect glycoprotein processing, penetration, and virulence in mice. J. Virol. 631619-1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ryman, K. D., C. L. Gardner, C. W. Burke, K. C. Meier, J. M. Thompson, and W. B. Klimstra. 2007. Heparan sulfate binding can contribute to the neurovirulence of neuroadapted and nonneuroadapted Sindbis viruses. J. Virol. 813563-3573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ryman, K. D., L. J. White, R. E. Johnston, and W. B. Klimstra. 2002. Effects of PKR/RNase L-dependent and alternative antiviral pathways on alphavirus replication and pathogenesis. Viral Immunol. 1553-76. [DOI] [PubMed] [Google Scholar]
- 48.Santagati, M. G., J. A. Maatta, P. V. Itaranta, A. A. Salmi, and A. E. Hinkkanen. 1995. The Semliki Forest virus E2 gene as a virulence determinant. J. Gen. Virol. 7647-52. [DOI] [PubMed] [Google Scholar]
- 49.Schlesinger, S., and M. J. Schlesinger. 1996. Togaviridae: the viruses and their replication, p. 523-539. In B. N. Fields, D. M. Knipe, and P. Howley (ed.), Fundamental virology. Lippincott-Raven, Philadelphia, PA.
- 50.Schoepp, R. J., and R. E. Johnston. 1993. Directed mutagenesis of a Sindbis virus pathogenesis site. Virology 193149-159. [DOI] [PubMed] [Google Scholar]
- 51.Scott, T. W., and S. C. Weaver. 1989. Eastern equine encephalitides virus: epidemiology and evolution of mosquito transmission. Adv. Virus Res. 37277-328. [DOI] [PubMed] [Google Scholar]
- 52.Spotts, D. R., R. M. Reich, M. A. Kalkhan, R. M. Kinney, and J. T. Roehrig. 1998. Resistance to alpha/beta interferons correlates with the epizootic and virulence potential of Venezuelan equine encephalitis viruses and is determined by the 5′ noncoding region and glycoproteins. J. Virol. 7210286-10291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Strauss, J. H., and E. G. Strauss. 1994. The alphaviruses: gene expression, replication, and evolution. Microbiol. Rev. 58491-562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.TenBroeck, C., and M. H. Merrill. 1933. A serological difference between Eastern and Western equine encephalomyelitis virus. Proc. Soc. Exp. Biol Med. 31217-220. [Google Scholar]
- 55.Tucker, P. C., and D. E. Griffin. 1991. Mechanism of altered Sindbis virus neurovirulence associated with a single-amino-acid change in the E2 glycoprotein. J. Virol. 651551-1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tucker, P. C., E. G. Strauss, R. J. Kuhn, J. H. Strauss, and D. E. Griffin. 1993. Viral determinants of age-dependent virulence of Sindbis virus for mice. J. Virol. 674605-4610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tuittila, M., and A. E. Hinkkanen. 2003. Amino acid mutations in the replicase protein nsP3 of Semliki Forest virus cumulatively affect neurovirulence. J. Gen. Virol. 841525-1533. [DOI] [PubMed] [Google Scholar]
- 58.Tuittila, M. T., M. G. Santagati, M. Roytta, J. A. Maatta, and A. E. Hinkkanen. 2000. Replicase complex genes of Semliki Forest virus confer lethal neurovirulence. J. Virol. 744579-4589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Vogel, P., W. M. Kell, D. L. Fritz, M. D. Parker, and R. J. Schoepp. 2005. Early events in the pathogenesis of Eastern equine encephalitis virus in mice. Am. J. Pathol. 166159-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Walder, R., P. B. Jahrling, and G. A. Eddy. 1980. Differentiation markers of eastern equine encephalitis (EEE) viruses and virulence, p. 237-250. In J. Vesenjak-Hirjan (ed.), Arboviruses in the Mediterranean countries. Fisher, Stuttgart, Germany.
- 61.Wang, E., O. Petrakova, A. P. Adams, P. V. Aguilar, W. Kang, S. Paessler, S. M. Volk, I. Frolov, and S. C. Weaver. 2007. Chimeric Sindbis/Eastern equine encephalitis vaccine candidates are highly attenuated and immunogenic in mice. Vaccine 257573-7581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Weaver, S. C. 2001. Eastern equine encephalitis. In M. W. Service (ed.), The encyclopedia of arthropod-transmitted infections. CAB International, Wallingford, United Kingdom.
- 63.Weaver, S. C., M. Anishchenko, R. Bowen, A. C. Brault, J. G. Estrada-Franco, Z. Fernandez, I. Greene, D. Ortiz, S. Paessler, and A. M. Powers. 2004. Genetic determinants of Venezuelan equine encephalitis emergence. Arch. Virol. Suppl. 1843-64. [DOI] [PubMed] [Google Scholar]
- 64.Weaver, S. C., M. Pfeffer, K. Marriot, W. Kang, and R. M. Kinney. 1999. Genetic evidence for the origins of Venezuelan equine encephalitis virus subtype IAB outbreaks. Am. J. Trop. Med. Hyg. 60441-448. [DOI] [PubMed] [Google Scholar]
- 65.White, L. J., J. G. Wang, N. L. Davis, and R. E. Johnston. 2001. Role of alpha/beta interferon in Venezuelan equine encephalitis virus pathogenesis: effect of an attenuating mutation in the 5′ untranslated region. J. Virol. 753706-3718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zhang, Y., C. W. Burke, K. D. Ryman, and W. B. Klimstra. 2007. Identification and characterization of interferon-induced proteins that inhibit alphavirus replication. J. Virol. 8111246-11255. [DOI] [PMC free article] [PubMed] [Google Scholar]