Abstract
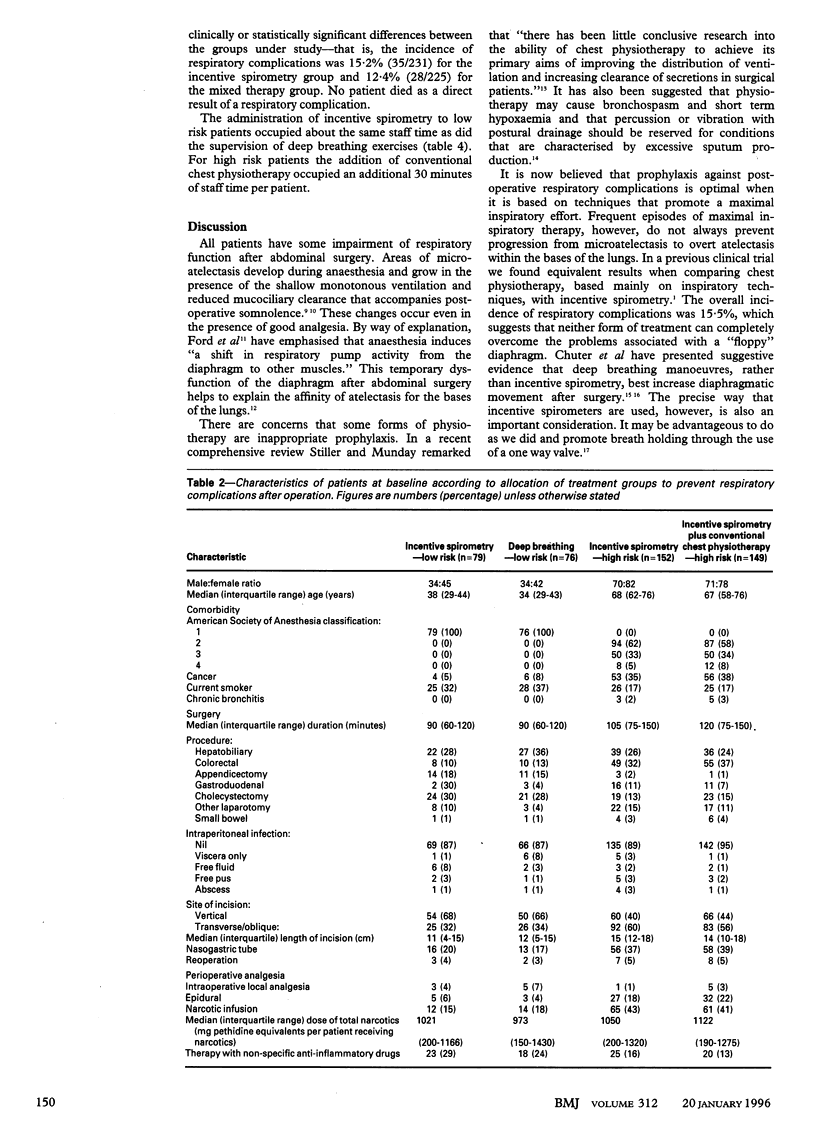
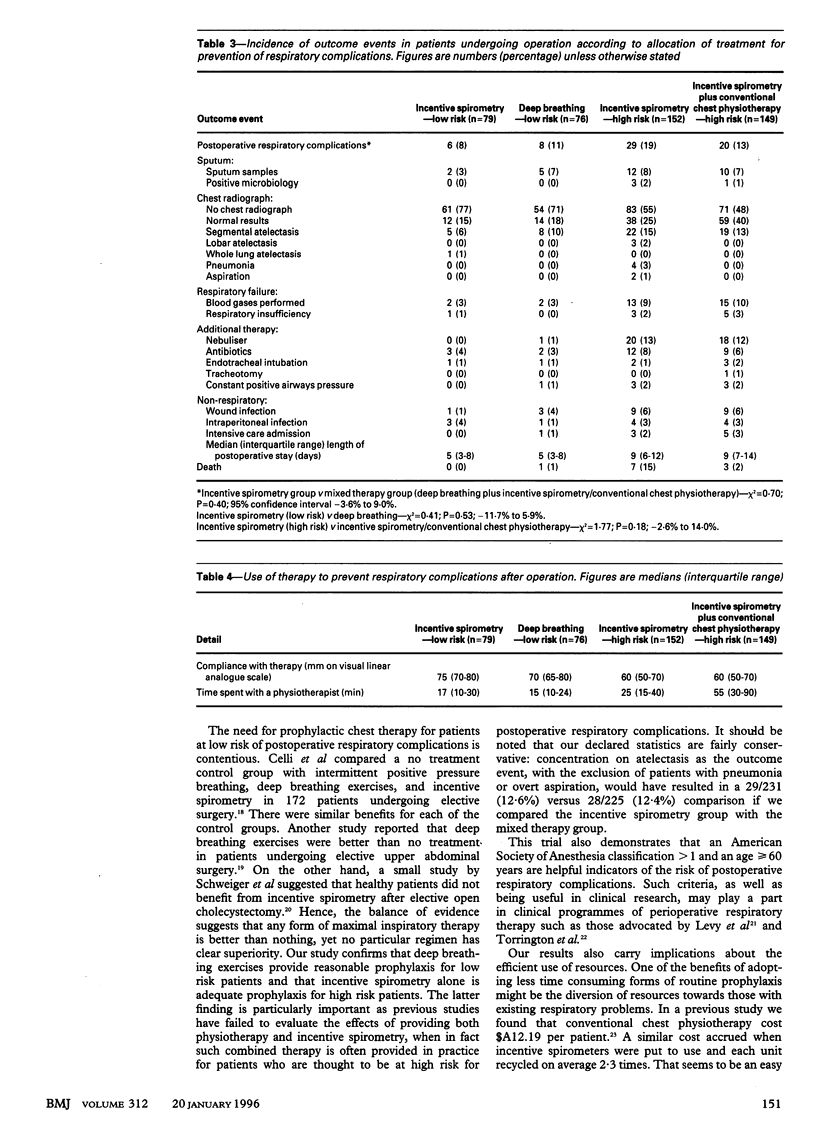
OBJECTIVE--To evaluate the prevention of respiratory complications after abdominal surgery by a comparison of a global policy of incentive spirometry with a regimen consisting of deep breathing exercises for low risk patients and incentive spirometry plus physiotherapy for high risk patients. DESIGN--Stratified randomised trial. SETTING--General surgical service of an urban teaching hospital. PATIENTS--456 patients undergoing abdominal surgery. Patients less than 60 years of age with an American Society of Anesthesia classification of 1 were considered to be at low risk. OUTCOME MEASURES--Respiratory complications were defined as clinical features consistent with collapse or consolidation, a temperature above 38 degrees C, plus either confirmatory chest radiology or positive results on sputum microbiology. We also recorded the time that staff devoted to prophylactic respiratory therapy. RESULTS--There was good baseline equivalence between the groups. The incidence of respiratory complications was 15% (35/231) for patients in the incentive spirometry group and 12% (28/225) for patients in the mixed therapy group (P = 0.40; 95% confidence interval -3.6% to 9.0%). It required similar amounts of staff time to provide incentive spirometry and deep breathing exercises for low risk patients. The inclusion of physiotherapy for high risk patients, however, resulted in the utilisation of an extra 30 minutes of staff time per patient. CONCLUSIONS--When the use of resources is taken into account, the most efficient regimen of prophylaxis against respiratory complications after abdominal surgery is deep breathing exercises for low risk patients and incentive spirometry for high risk patients.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baker W. L., Lamb V. J., Marini J. J. Breath-stacking increases the depth and duration of chest expansion by incentive spirometry. Am Rev Respir Dis. 1990 Feb;141(2):343–346. doi: 10.1164/ajrccm/141.2.343. [DOI] [PubMed] [Google Scholar]
- Celli B. R., Rodriguez K. S., Snider G. L. A controlled trial of intermittent positive pressure breathing, incentive spirometry, and deep breathing exercises in preventing pulmonary complications after abdominal surgery. Am Rev Respir Dis. 1984 Jul;130(1):12–15. doi: 10.1164/arrd.1984.130.1.12. [DOI] [PubMed] [Google Scholar]
- Chuter T. A., Weissman C., Mathews D. M., Starker P. M. Diaphragmatic breathing maneuvers and movement of the diaphragm after cholecystectomy. Chest. 1990 May;97(5):1110–1114. doi: 10.1378/chest.97.5.1110. [DOI] [PubMed] [Google Scholar]
- Chuter T. A., Weissman C., Starker P. M., Gump F. E. Effect of incentive spirometry on diaphragmatic function after surgery. Surgery. 1989 Apr;105(4):488–493. [PubMed] [Google Scholar]
- Dureuil B., Cantineau J. P., Desmonts J. M. Effects of upper or lower abdominal surgery on diaphragmatic function. Br J Anaesth. 1987 Oct;59(10):1230–1235. doi: 10.1093/bja/59.10.1230. [DOI] [PubMed] [Google Scholar]
- Ford G. T., Rosenal T. W., Clergue F., Whitelaw W. A. Respiratory physiology in upper abdominal surgery. Clin Chest Med. 1993 Jun;14(2):237–252. [PubMed] [Google Scholar]
- Hall J. C., Hall J. L., Christiansen K. A comparison of the roles of cefamandole and ceftriaxone in abdominal surgery. Arch Surg. 1991 Apr;126(4):512–516. doi: 10.1001/archsurg.1991.01410280116019. [DOI] [PubMed] [Google Scholar]
- Hall J. C., Tapper J., Tarala R. The cost-efficiency of incentive spirometry after abdominal surgery. Aust N Z J Surg. 1993 May;63(5):356–359. doi: 10.1111/j.1445-2197.1993.tb00402.x. [DOI] [PubMed] [Google Scholar]
- Hall J. C., Tarala R. A., Hall J. L., Mander J. A multivariate analysis of the risk of pulmonary complications after laparotomy. Chest. 1991 Apr;99(4):923–927. doi: 10.1378/chest.99.4.923. [DOI] [PubMed] [Google Scholar]
- Hall J. C., Tarala R., Harris J., Tapper J., Christiansen K. Incentive spirometry versus routine chest physiotherapy for prevention of pulmonary complications after abdominal surgery. Lancet. 1991 Apr 20;337(8747):953–956. doi: 10.1016/0140-6736(91)91580-n. [DOI] [PubMed] [Google Scholar]
- Jackson C. V. Preoperative pulmonary evaluation. Arch Intern Med. 1988 Oct;148(10):2120–2127. [PubMed] [Google Scholar]
- Jones J. G. Anaesthesia, and atelectasis: the role of VTAB and the chest wall. Br J Anaesth. 1987 Aug;59(8):949–953. doi: 10.1093/bja/59.8.949. [DOI] [PubMed] [Google Scholar]
- Levy P. A., Rutherford H. G., Shepard B. M. Usefulness of preoperative screening tests in perioperative respiratory therapy. Respir Care. 1979 Aug;24(8):701–709. [PubMed] [Google Scholar]
- Roukema J. A., Carol E. J., Prins J. G. The prevention of pulmonary complications after upper abdominal surgery in patients with noncompromised pulmonary status. Arch Surg. 1988 Jan;123(1):30–34. doi: 10.1001/archsurg.1988.01400250032004. [DOI] [PubMed] [Google Scholar]
- Schwieger I., Gamulin Z., Forster A., Meyer P., Gemperle M., Suter P. M. Absence of benefit of incentive spirometry in low-risk patients undergoing elective cholecystectomy. A controlled randomized study. Chest. 1986 May;89(5):652–656. doi: 10.1378/chest.89.5.652. [DOI] [PubMed] [Google Scholar]
- Selsby D. S. Chest physiotherapy. BMJ. 1989 Mar 4;298(6673):541–542. doi: 10.1136/bmj.298.6673.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stiller K. R., Munday R. M. Chest physiotherapy for the surgical patient. Br J Surg. 1992 Aug;79(8):745–749. doi: 10.1002/bjs.1800790807. [DOI] [PubMed] [Google Scholar]
- Strandberg A., Tokics L., Brismar B., Lundquist H., Hedenstierna G. Constitutional factors promoting development of atelectasis during anaesthesia. Acta Anaesthesiol Scand. 1987 Jan;31(1):21–24. doi: 10.1111/j.1399-6576.1987.tb02513.x. [DOI] [PubMed] [Google Scholar]
- Torrington K. G., Henderson C. J. Perioperative respiratory therapy (PORT). A program of preoperative risk assessment and individualized postoperative care. Chest. 1988 May;93(5):946–951. doi: 10.1378/chest.93.5.946. [DOI] [PubMed] [Google Scholar]
- Vacanti C. J., VanHouten R. J., Hill R. C. A statistical analysis of the relationship of physical status to postoperative mortality in 68,388 cases. Anesth Analg. 1970 Jul-Aug;49(4):564–566. [PubMed] [Google Scholar]


