Abstract
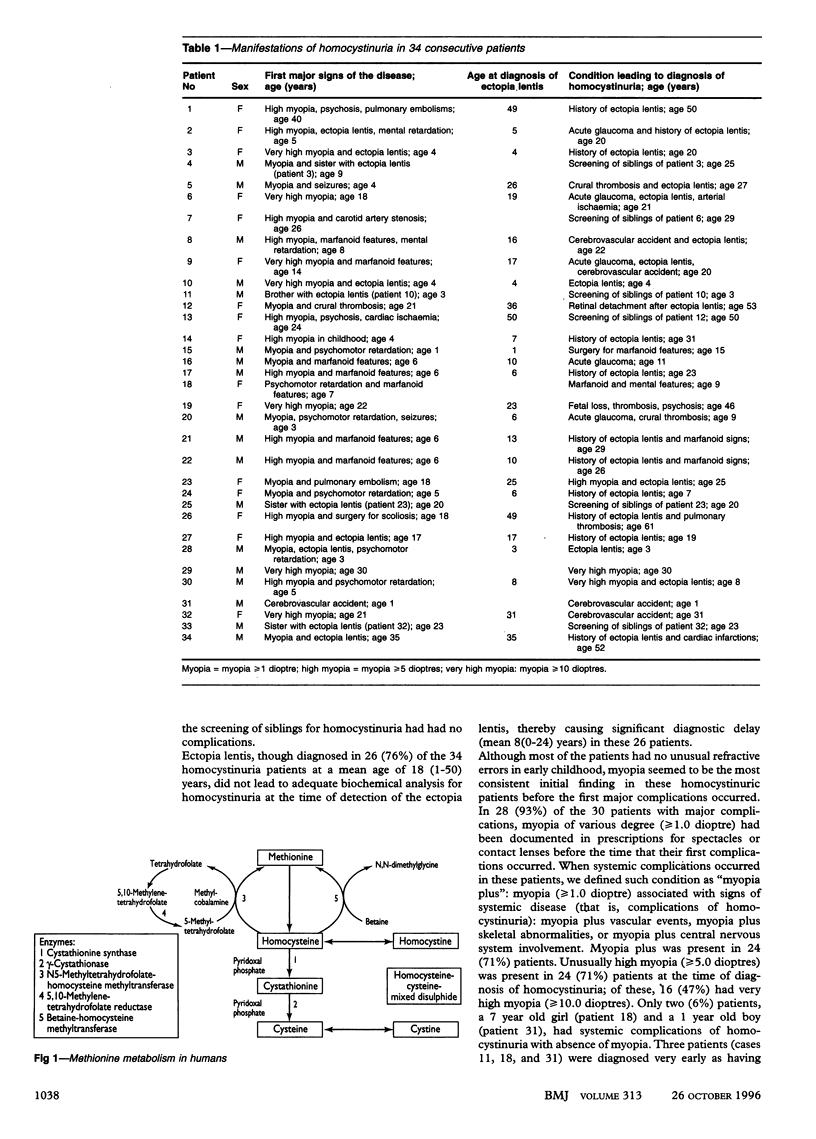
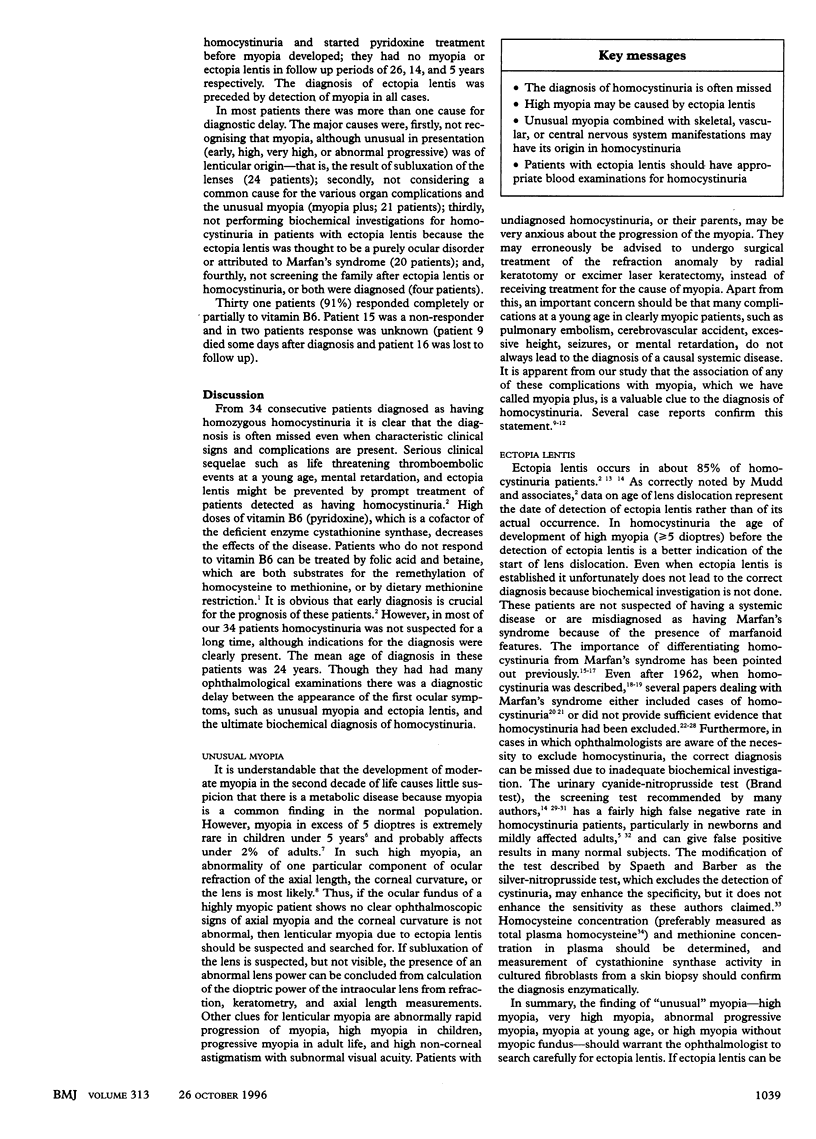
OBJECTIVE: To assess the causes for delay in the diagnosis of homocystinuria. DESIGN: Clinical and laboratory data were collected from patients diagnosed as having homocystinuria due to cystathionine synthase deficiency, with special reference to the ages at which the patients had their first major signs of the disease, ectopia lentis was established, and homocystinuria was diagnosed. SETTING: University hospital in the Netherlands. SUBJECTS: 34 patients (18 males) in whom homocystinuria due to cystathionine synthase deficiency was diagnosed in the period 1970-94. RESULTS: Among 34 consecutively detected homocystinuria patients the mean age at diagnosis of homocystinuria was 24 (range 1-61) years. Despite frequent ocular manifestations, serious complications in the vascular, skeletal, and central nervous systems, and repeated examinations performed in these patients by clinicians of various disciplines, there was a mean delay of 11 (0-43) years between the first major signs of the disease (at mean age 13 (1-40) years) and the ultimate diagnosis of homocystinuria. Even when ectopia lentis was diagnosed (in 26 (76%) patients, mean age 18 (1-50) years), this did not lead to adequate biochemical analysis for homocystinuria at the time of detection, causing a mean diagnostic delay of 8 (0-24) years in these patients. CONCLUSIONS: Three factors should have precipitated the diagnosis of homocystinuria: early recognition that unusual myopia (high, very high, abnormal progressive, or at young age) was caused by subluxation of the ocular lenses; awareness that the occurrence of myopia combined with systemic complications ("myopia plus") might be due to homocystinuria; and appropriate biochemical investigations carried out in patients with ectopia lentis and in their siblings.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Applegarth D. A., Vallance H. D., Seccombe D. Are patients with homocystinuria being missed? Eur J Pediatr. 1995 Jul;154(7):589–589. doi: 10.1007/BF02074844. [DOI] [PubMed] [Google Scholar]
- Blika S., Saunte E., Lunde H., Gjessing L. R., Ringvold A. Homocystinuria treated with pyridoxine. Acta Ophthalmol (Copenh) 1982 Dec;60(6):894–906. doi: 10.1111/j.1755-3768.1982.tb00620.x. [DOI] [PubMed] [Google Scholar]
- Boers G. H., Fowler B., Smals A. G., Trijbels F. J., Leermakers A. I., Kleijer W. J., Kloppenborg P. W. Improved identification of heterozygotes for homocystinuria due to cystathionine synthase deficiency by the combination of methionine loading and enzyme determination in cultured fibroblasts. Hum Genet. 1985;69(2):164–169. doi: 10.1007/BF00293290. [DOI] [PubMed] [Google Scholar]
- Boers G. H., Polder T. W., Cruysberg J. R., Schoonderwaldt H. C., Peetoom J. J., Van Ruyven T. W., Smals A. G., Kloppenborg P. W. Homocystinuria versus Marfan's syndrome: the therapeutic relevance of the differential diagnosis. Neth J Med. 1984;27(6):206–212. [PubMed] [Google Scholar]
- Boers G. H., Smals A. G., Drayer J. I., Trijbels F. J., Leermakers A. I., Kloppenborg P. W. Pyridoxine treatment does not prevent homocystinemia after methionine loading in adult homocystinuria patients. Metabolism. 1983 Apr;32(4):390–397. doi: 10.1016/0026-0495(83)90049-5. [DOI] [PubMed] [Google Scholar]
- Brenton D. P., Dow C. J., James J. I., Hay R. L., Wynne-Davies R. Homocystinuria and Marfan's syndrome. A comparison. J Bone Joint Surg Br. 1972 May;54(2):277–298. [PubMed] [Google Scholar]
- CARSON N. A., NEILL D. W. Metabolic abnormalities detected in a survey of mentally backward individuals in Northern Ireland. Arch Dis Child. 1962 Oct;37:505–513. doi: 10.1136/adc.37.195.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cernea P., Zbranca E. L'homocystinurie et le syndrome de Marfan. Ann Ocul (Paris) 1972 Feb;205(2):167–178. [PubMed] [Google Scholar]
- Cross H. E., Jensen A. D. Ocular manifestations in the Marfan syndrome and homocystinuria. Am J Ophthalmol. 1973 Mar;75(3):405–420. doi: 10.1016/0002-9394(73)91149-5. [DOI] [PubMed] [Google Scholar]
- Croxatto J. O., Lombardi A., Malbran E. S. Inflamed eye in Marfan's syndrome with posteriorly luxated lens. Ophthalmologica. 1986;193(1-2):23–26. doi: 10.1159/000309674. [DOI] [PubMed] [Google Scholar]
- Cullom R. D., Jr, Cullom M. E., Kardon R., Digre K. Two neuro-ophthalmic episodes separated in time and space. Surv Ophthalmol. 1995 Nov-Dec;40(3):217–224. doi: 10.1016/s0039-6257(95)80028-x. [DOI] [PubMed] [Google Scholar]
- Fusco G., Carlomagno S., Romano A., Rinaldi E., Cedrola G., Cianciaruso L., Curto A., Rosolia S., Auricchio G. Type I hyperprolinemia in a family suffering from aniridia and severe dystrophia of ocular tissues. Ophthalmologica. 1976;173(1):1–10. doi: 10.1159/000307812. [DOI] [PubMed] [Google Scholar]
- GERRITSEN T., VAUGHN J. G., WAISMAN H. A. The identification of homocystine in the urine. Biochem Biophys Res Commun. 1962 Dec 19;9:493–496. doi: 10.1016/0006-291x(62)90114-6. [DOI] [PubMed] [Google Scholar]
- Garston J. B., Gordon R. R., Hart C. T., Pollitt R. J. An unusual case of homocystinuria. Br J Ophthalmol. 1970 Apr;54(4):248–251. doi: 10.1136/bjo.54.4.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hindle N. W., Crawford J. S. Dislocation of the lens in Marfan's syndrome. Its effect and treatment. Can J Ophthalmol. 1969 Apr;4(2):128–135. [PubMed] [Google Scholar]
- Jarrett WH I. I. Dislocation of the lens. A study of 166 hospitalized cases. Arch Ophthalmol. 1967 Sep;78(3):289–296. doi: 10.1001/archopht.1967.00980030291006. [DOI] [PubMed] [Google Scholar]
- Matthäus W. Ergebnisse der Kryoextraktion luxierter und stark subluxierter Linsen. Klin Monbl Augenheilkd. 1984 Oct;185(4):253–258. doi: 10.1055/s-2008-1054609. [DOI] [PubMed] [Google Scholar]
- Mudd S. H., Skovby F., Levy H. L., Pettigrew K. D., Wilcken B., Pyeritz R. E., Andria G., Boers G. H., Bromberg I. L., Cerone R. The natural history of homocystinuria due to cystathionine beta-synthase deficiency. Am J Hum Genet. 1985 Jan;37(1):1–31. [PMC free article] [PubMed] [Google Scholar]
- Neetens A., De Smet N., Verschueren C., Zelencova L. Homocystinuria and Marfanoid appearance. Bull Soc Belge Ophtalmol. 1980;191:29–37. [PubMed] [Google Scholar]
- Peyman G. A., Raichand M., Goldberg M. F., Ritacca D. Management of subluxated and dislocated lenses with the vitrophage. Br J Ophthalmol. 1979 Nov;63(11):771–778. doi: 10.1136/bjo.63.11.771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SORSBY A., SHERIDAN M., LEARY G. A., BENJAMIN B. Vision, visual acuity, and ocular refraction of young men: findings in a sample of 1,033 subjects. Br Med J. 1960 May 7;1(5183):1394–1398. doi: 10.1136/bmj.1.5183.1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoonderwaldt H. C., Boers G. H., Cruysberg J. R., Schulte B. P., Slooff J. L., Thijssen H. O. Neurologic manifestations of homocystinuria. Clin Neurol Neurosurg. 1981;83(3):153–162. doi: 10.1016/0303-8467(81)90017-2. [DOI] [PubMed] [Google Scholar]
- Spaeth G. L., Barber G. W. Prevalence of homocystinuria among the mentally retarded: evaluation of a specific screening test. Pediatrics. 1967 Oct;40(4):586–589. [PubMed] [Google Scholar]
- Spaeth G. L. Screening for homocystinuria. Surv Ophthalmol. 1984 Nov-Dec;29(3):230–230. doi: 10.1016/0039-6257(84)90213-3. [DOI] [PubMed] [Google Scholar]


