Abstract
FOLLOWING STROKE, PATIENTS MAY HAVE REDUCED DIETARY intake, swallowing impairments (dysphagia) and other neurological deficits that could affect their nutritional and hydration status and lead to aspiration pneumonia. Impaired nutritional status is associated with reduced functional improvement, increased complication rates and prolonged hospital stays. This article is aimed at primary care physicians and others caring for stroke patients. We discuss the need for assessing the nutritional status of stroke patients and provide strategies for the management of dysphagia and patients' food and fluid intakes. In addition, we review clinical and radiological options for the diagnosis of dysphagia as well as oral and enteral feeding alternatives.
Articles to date in this series
Case
Mr. B is a 56-year-old man who has hypertension and type 2 diabetes mellitus. He was well until the day of his admission to hospital. He presents with an occipital headache, tingling in the right hand, ataxia of the right limb, a hoarse voice, dysphagia, nausea, vomiting and vertigo. On examination he appears to be a well-nourished, physically fit but fatigued man. His blood pressure is elevated (190/110 mm Hg), and although no focal weakness is noted during the physical examination he is falling to the right. He has decreased pain and temperature sensation on the left side of his body, ptosis of the right eyelid and a diminished gag reflex. A CT scan demonstrates the presence of an infarct of the right lateral medulla oblongata. A chest radiograph shows the presence of pneumonia in both lungs; antibiotic therapy is initiated.
What is dysphagia and how is it diagnosed and managed? What is the relation between nutrition and stroke?
People who have had a stroke are nutritionally and medically vulnerable because dysphagia and other neurologic deficits can contribute to aspiration and decreased dietary intake, and potentially malnutrition. Malnourished states can lead to adverse outcomes (e.g., increased complication rates, a poorer functional outcome, a prolonged hospital stay and decreased quality of life),1 and dysphagia is a frequent cause of aspiration pneumonia. In this article, we review practical strategies for the diagnosis and management of dysphagia by primary care physicians and others caring for stroke patients.
Nutritional status and related functional outcomes in stroke patients
Stroke may affect and be affected by nutrition and diet. An important clinical goal should be the prevention of, or identification and treatment of, dysphagia and inadequate nutritional and feeding states in patients with stroke to help them reach their full potential for rehabilitation.
Nutritional status should be monitored by means of routine nutritional screenings or comprehensive assessments every week or 2 weeks. Further information about nutritional assessment is given in the online Appendix 1 (see www.cmaj.ca/cgi/content/full/169/10/1041/DC1). After acute stroke, the prevalence of malnutrition has been reported to increase from about 16% on admission to 22%–35% at about 2 weeks.2,3 Of patients with severe stroke and longer hospital stays, over half were reported to be malnourished.4 Of rehabilitation patients, about 50% were found to be malnourished at 2–3 weeks after the stroke; this proportion dropped to 19% at 2–4 months.5 For acute and rehabilitating stroke patients, hypoalbuminemia and malnutrition have been associated with poorer functional outcomes,6,7 higher complication rates6 and reduced rate of functional improvement7 compared with those who were not malnourished or hypoalbuminemic.
Dysphagia
Dysphagia is simply defined as any difficulty with swallowing. Normal swallowing consists of 4 phases: oral preparatory, oral, pharyngeal and esophageal. Stroke usually affects the first 3 phases by interrupting the voluntary control of chewing and moving food around the mouth (more common with cerebral lesions) or delaying the pharyngeal reflex (more common with brainstem lesions).
Dysphagia is common after acute stroke, occurring in 29%–64% of patients,8,9,10 depending on the diagnostic method used. During rehabilitation after stroke, dysphagia has been reported to decline from 47% at 2–3 weeks to 17% at 2–4 months.5
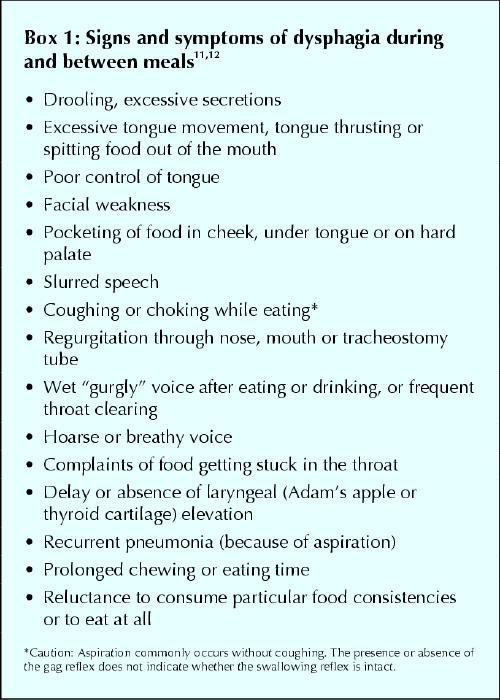
Warning signs of dysphagia are listed in Box 1.11,12 The presence or absence of a gag reflex does not necessarily predict whether dysphagia is occurring. Physicians and allied health professionals must pay attention to other manifestations of dysphagia (e.g., coughing, drooling and facial weakness) during their assessments.
Box 1.
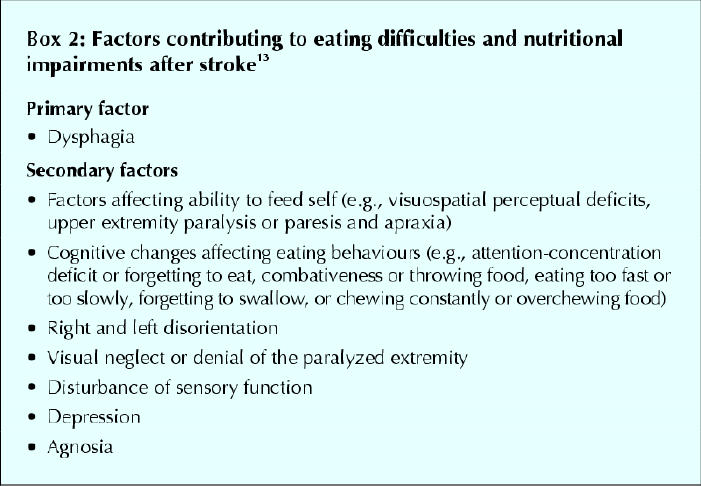
Dysphagia has been associated with weight loss and malnutrition, fluid depletion, aspiration and pneumonia. Aspiration is defined as the entry of material into the airway below the level of the true vocal cords. Many stroke patients with dysphagia do not aspirate, but those who do are usually dysphagic and are at increased risk of pneumonia. Secondary problems related to stroke often adversely affect dietary intake as well (see Box 213).
Box 2.
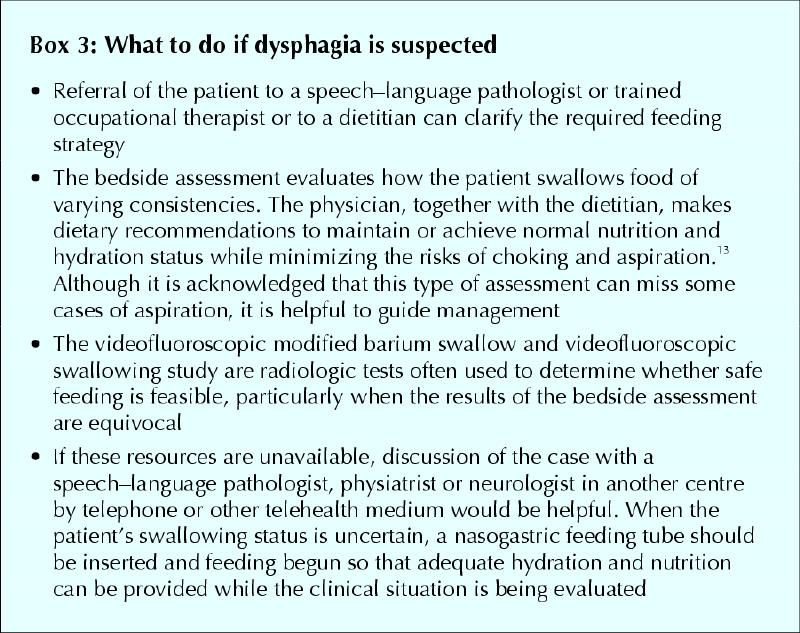
If a patient is unable to consume food or fluid orally or is unable to consume sufficient quantities, or if the risk of aspiration is high, enteral nutrition (tube feeding) should be provided until swallowing improves and oral intake is adequate. Further information about enteral feedings, including formula selection, routes of access, methods of administration and complications, is described in the online Appendix 2 (see www.cmaj.ca/cgi/content/full/169/10/1041/DC1). Box 314 identifies the clinical and radiological tests that are often used for the evaluation of dysphagia.
Box 3.
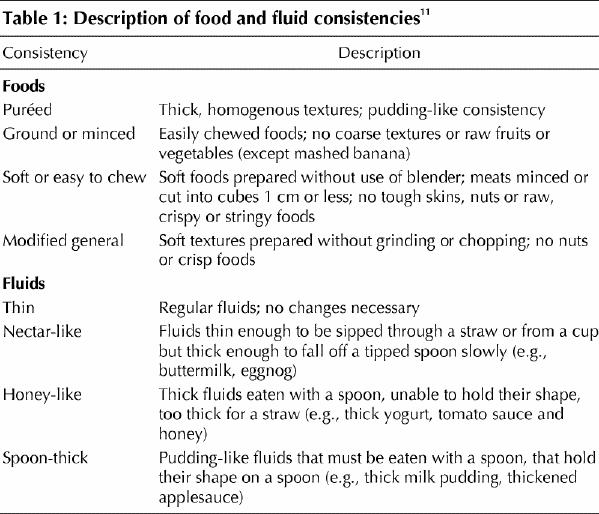
The dysphagia diet
Dysphagia diets are highly individualized. Characteristics of the diet include modification of food texture or fluid viscosity. Foods may be chopped, minced or puréed, and fluids may be thickened. Table 111 lists food and fluid consistencies along with some examples. In general, solid foods are assigned to 1 of 4 groups, which progress from the easiest to the most difficult to swallow. Special attention should be given to the nutritional adequacy of mechanically altered diets, particularly the puréed form. Regular communication with team members about the patient's changing swallowing capabilities is essential if the patient is to progress from a dysphagia diet to a diet of food with normal textures. Appendix 3 (available online at www.cmaj.ca/cgi/content/full/169/10/1041/DC1) describes the steps that the physician and allied health professionals may take in the nutritional management of stroke patients.
Table 1
Fluid requirements
The risk for dehydration in stroke patients is often underappreciated, particularly in patients with dysphagia who are receiving all their nutrition by mouth.15 The most difficult consistency for these patients to control orally is often thin fluids such as water. Even when fluids are thickened to ease control, adequate hydration can be a challenge. For inpatients, physicians should consider ordering overnight intravenous fluid administration, which should not interfere with the patients' participation in any daily rehabilitation therapy.
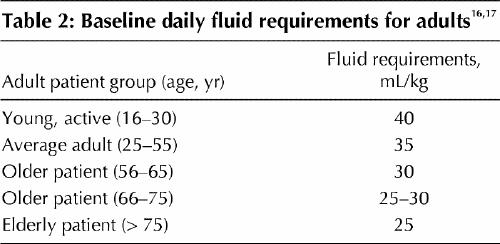
General guidelines for the determination of fluid requirements are given in Table 2.16,17 Fluid requirements should take into account the effects of age, disease and medical treatment. Requirements are increased as a consequence of fever, diarrhea, vomiting, excessive sweating and fistula drainage, and during the administration of hyperosmolar formulas.14,18
Table 2
The case revisited
A lateral medullary infarction is often associated with dysphagia. Mr. B's pneumonia is a strong indicator that aspiration occurred. His pneumonia is a probable sequela of aspirating saliva. Mr. B is not allowed to have anything by mouth when he is admitted to hospital. The speech–language pathologist uses a bedside swallowing assessment to screen for dysphagia and notes that Mr. B coughs and sputters when he has only small amounts of liquid and pudding. Mr. B is clearly at high risk of further aspiration and is fed enterally with an isotonic, fibre-fortified liquid formula through a nasogastric tube for 10 days. He is subsequently transferred to a stroke rehabilitation service.
It becomes clear that Mr. B's dysphagic state will not resolve quickly, and so the nasogastric tube is replaced by a percutaneous endoscopic gastrostomy (PEG) tube for feeding. He requires cloxacillin administration on one occasion because of a subcutaneous infection at the tube site that did not clear with use of local antibiotic ointment. After receiving instructions from the nurses, he administers his own feeding on a cyclical basis using an infusion pump. He continues tube feedings at home after discharge from the stroke rehabilitation service. Over the following 15 months, progressive improvements in his swallowing capabilities are evident on clinical examination and on videofluoroscopic swallowing studies. The percutaneous endoscopic gastrostomy tube is removed. Mr. B retains some residual neurologic and swallowing deficits but is able to live independently and consumes a normal diet.
Acknowledgments
We gratefully acknowledge the help of Dr. Leonard Bloom, family physician, in reviewing the manuscript.
Footnotes
This article has been peer reviewed.
Contributors: Both authors contributed substantially to the conception, design, analysis and interpretation of the research material, drafted and critically revised the manuscript for important intellectual content and gave final approval of the version to be published.
Competing interests: None declared.
Correspondence to: Dr. Hillel M. Finestone, Department of Physical Medicine and Rehabilitation, Elisabeth Bruyère Health Centre, 43 Bruyère St., Ottawa ON K1N 5C8; fax 613 562-6312; hfinesto@scohs.on.ca
References
- 1.Hoffer LJ. Clinical nutrition: 1. Protein-energy malnutrition in the inpatient. CMAJ 2001;165(10):1345-9. [PMC free article] [PubMed]
- 2.Axelsson K, Asplund K, Norberg A, Alafuzoff I. Nutritional status in patients with acute stroke. Acta Med Scand 1988;224:217-24. [DOI] [PubMed]
- 3.Davalos R, Ricart W, Gonzalez-Huix F, Soler S, Marrugat J, Molins A, et al. Effect of malnutrition after acute stroke on clinical outcome. Stroke 1996;27:1028-32. [DOI] [PubMed]
- 4.Axelsson K, Asplund K, Norberg A, Eriksson S. Eating problems and nutritional status during hospital stay of patients with severe stroke. J Am Diet Assoc 1989;89:1092-6. [PubMed]
- 5.Finestone HM, Greene-Finestone LS, Wilson ES, Teasell RW. Malnutrition in stroke patients on the rehabilitation service and at follow-up: prevalence and predictors. Arch Phys Med Rehabil 1995;76:310-6. [DOI] [PubMed]
- 6.Aptaker RL, Roth EJ, Reichhardt G, Duerden ME, Levy CE. Serum albumin level as a predictor of geriatric stroke rehabilitation outcome. Arch Phys Med Rehabil 1994;75:80-4. [PubMed]
- 7.Finestone HM, Greene-Finestone LS, Wilson ES, Teasell RW. Prolonged length of stay and reduced functional improvement rate in malnourished stroke rehabilitation patients. Arch Phys Med Rehabil 1996;77:340-5. [DOI] [PubMed]
- 8.Gordon C, Hewer RL, Wade DT. Dysphagia in acute stroke. BMJ 1987;295:411-4. [DOI] [PMC free article] [PubMed]
- 9.Barer DH. The natural history and functional consequences of dysphagia after hemispheric stroke. J Neurol Neurosurg Psychiatry 1989;52:236-46. [DOI] [PMC free article] [PubMed]
- 10.Mann G, Hankey GJ, Cameron D. Swallowing function after stroke: progress and prognostic factors at 6 months. Stroke 1999;30:744-8. [DOI] [PubMed]
- 11.Pardoe EM. Development of a multistage diet for dysphagia. J Am Diet Assoc 1993;93:568-71. [DOI] [PubMed]
- 12.American Dietetics Association. The manual of clinical dietetics. 5th ed. Chicago: The Association; 1996. p. 145-63.
- 13.Buelow JM, Jamieson D. Potential for altered nutritional status in the stroke patient. Rehabil Nurs 1990;15:260-3. [DOI] [PubMed]
- 14.Chicago Dietetic Association, South Shore Suburban Dietetic Association and Dietitians of Canada. Manual of clinical dietetics. 6th ed. Chicago: American Dietetic Association; 2000. p. 3-38, 667-93.
- 15.Finestone HM, Foley N, Woodbury MG, Greene-Finestone L. Quantifying fluid intake in dysphagic stroke patients: a preliminary comparison of oral and nonoral strategies. Arch Phys Med Rehabil 2001;82:1744-6. [DOI] [PubMed]
- 16.Blackburn GL, Bell SJ, Mullen JL, editors. Nutritional medicine, case management approach. Philadelphia: WB Saunders; 1989.
- 17.Food and Nutrition Board. Committee on dietary allowances. 9th ed. Washington: National Academy of Sciences; 1980.
- 18.Scientific Review Committee, Department of National Health and Welfare. Nutrition recommendations: the report of the Scientific Review Committee. Ottawa: The Department; 1990. p. 173-7.


