Abstract
Costa Rica is a middle-income country with a strong governmental emphasis on human development. For more than half a century, its health policies have applied the principles of equity and solidarity to strengthen access to care through public services and universal social health insurance.
Costa Rica’s population measures of health service coverage, health service use, and health status are excellent, and in the Americas, life expectancy in Costa Rica is second only to that in Canada. Many of these outcomes can be linked to the performance of the public health care system.
However, the current emphasis of international aid organizations on privatization of health services threatens the accomplishments and universality of the Costa Rican health care system.
For several years, international development agencies, including the World Bank and the International Monetary Fund, have promoted the role of for-profit health care facilities and programs in the delivery of health care services in developing countries while narrowing the role of the not-for-profit sector in disease control.1 Using as an example the experience of Costa Rica, we question the privatization of health care policy promoted by international aid agencies.
During a 2001 press conference, former World Bank president James D. Wolfensohn recognized Cuba for having done a “terrific job” in the area of health.2 His laudatory comments were remarkable given that Cuba is well known for evading World Bank and International Monetary Fund recommendations. Jo Ritzen, the World Bank’s vice president for development policy at the time, provided a clue to Wolfensohn’s lack of hesitation in acknowledging Cuba by suggesting that the Cuban experience might not be replicable in other countries.3 We would say that the Cuban policy was not exportable, at least not without its authoritarian regime.
What would World Bank senior officers have said about Costa Rica, which is a benchmark democracy by international standards?4 Its health policy also differs radically from the health policies of international loaning agencies. Despite resisting the recommendations of the World Bank and International Monetary Fund, Costa Rica has accomplished a great deal in the health arena; for example, compared with all the countries in the Americas, Costa Rica’s life expectancy is second only to Canada’s.5 Although the country’s per capita income is approximately the same as that of Mexico and one fourth that of the United States, total health expenditures in Costa Rica are one ninth those of the United States. Moreover, other health and equity indicators in Costa Rica rank close to the United States and well above Mexico (Table 1 ▶).
TABLE 1—
Health and Equity Indicators for Costa Rica, the United States, and Mexico
| Costa Rica | United States | Mexico | |
| GDP per capita, $a | 9 460 | 34 320 | 8 430 |
| Health expenditure per capita, $ | 562 | 4 887 | 544 |
| Infant mortalityb | 9 | 7 | 24 |
| Life expectancy at birthc | 78.0 | 77.0 | 73.3 |
| Gini indexd | 46.5 | 40.8 | 54.6 |
Note. GDP = gross domestic product. All data are for 2001 with the exception of the Gini index, which reflects 2000 figures. Data were derived from the United Nations Development Programme.5,36
aPurchasing power parity.
bProbability of dying between birth and exactly 1 year of age, expressed per 1000 live births.
cNumber of years a newborn infant would live if prevailing patterns of age-specific mortality at the time of the infant’s birth were to stay the same throughout his or her life.
dMeasurement of inequality in the distribution of income or consumption within a country, expressed as a percentage. A value of 0 represents perfect equality and a value of 100 represents perfect inequality.
Certainly Costa Rica’s achievements are not simply the product of good health services. Indeed, the country maintained annual growth rates (gross domestic product [GDP] per capita) of 1.2% between 1975 and 2001 and 2.8% between 1995 and 2001, even though it never rose to the high-income category (GDP per capita of $9206 or more in 2001).5 Since 1995, Costa Rica has occupied a stable position among countries with high scores (0.80 or above) on the human development index (which measures average achievement in 3 basic dimensions of human development: quality of life, knowledge, and standard of living).5
Despite the potential contributions of economic development to health outcomes, it would be unfair to credit the health achievements in Costa Rica mainly to rapid income growth, as the World Development Report did in its spotlight on Costa Rica and Cuba in 2004.7 Such an attribution overlooks the sensitivity to health service performance of indicators such as infant and maternal mortality. In the case of both indicators, Costa Rica has shown equal or better performance than its Latin American neighbors Chile,1 Venezuela, Panama, Colombia, and Mexico, countries in the same income group and with comparable health care expenditures (Table 2 ▶).
TABLE 2—
Infant and Maternal Mortality, Health Expenditure, and Economic Growth in Selected Years: Costa Rica, Chile, Venezuela, Panama, Colombia, and Mexico
| Infant Mortalitya | |||||||
| 1970 | 2001 | Reductionb in Infant Mortality,a 1970–2001 | Maternal Mortality,c 1985–2001 | Health Expenditure per Capita,d 2001, $ | GDP per Capita,d 2001, $ | GDP per Capita Annual Growth Rate, 1975–2001, % | |
| Costa Rica | 62 | 9 | 7 | 29 | 562 | 9460 | 1.2 |
| Chile | 78 | 10 | 8 | 23 | 792 | 9190 | 4.1 |
| Venezuela | 47 | 19 | 2 | 60 | 386 | 5670 | 0.9 |
| Panama | 46 | 19 | 2 | 70 | 458 | 5750 | 0.8 |
| Colombia | 69 | 19 | 4 | 80 | 356 | 7040 | 1.5 |
| Mexico | 79 | 26 | 3 | 55 | 544 | 8430 | 0.9 |
Note. GDP = gross domestic product. Data were derived from the United Nations Development Programme,5,36 the United Nations Children’s Fund,8 and the World Bank.9
aProbability of dying between birth and exactly 1 year of age, expressed per 1000 live births.
bCalculated from 1970 and 2001 figures.
cAnnual number of deaths of women from pregnancy-related causes per 100 000 live births (data refer to the most recent year available during the period specified, adjusted for underreporting and misclassification).
dPurchasing power parity.
From 1970 on, Costa Rica needed less than one third of the Chilean economic growth rate to achieve reductions in infant mortality similar to those achieved in Chile.10 With economic growth rates similar to Colombia, Costa Rica had twice the reduction in infant mortality. Costa Rica also achieved twice the reduction in infant mortality rates as Mexico with similar economic growth rates and health care expenditures.
In the 1970s, Costa Rica departed from the Latin American pattern of stagnation and closed the gap with the industrialized world in terms of infant mortality. According to Rosero-Bixby,11,12 only one fifth of the country’s spectacular infant mortality reduction can be accounted for by economic growth, whereas three fourths can be attributed to improvements in public health services. Such impressive achievements in themselves make the Costa Rican health system worthy of study.
However, the results of a MEDLINE search we conducted for the period 1975 through 2004 suggested a lack of interest among the scientific community in the Costa Rican experience, with only 122 papers published on Costa Rica as compared with 249 for Colombia and 424 for Chile. The Costa Rican health policy experience has also been largely ignored by international decisionmakers. We sought to address this knowledge gap and to derive important implications from the Costa Rican experience for international aid agencies and health policies.
METHODOLOGY
We complimented our MEDLINE search with reports and evaluations of the Costa Rican government and publications on health policy and Latin America in general. We made field visits to the 2 existing hospitals and a representative selection of primary care centers (n=10) in the 8 health zones (secondary division of regions in Costa Rica) of Costa Rica’s Atlantic region (Huetar Atlántica) in August 2004, October 2005, and March 2006. Also, we visited health centers in the central and southern Pacific regions.
We conducted 3 focus group discussions (n=47) with health care providers, as well as key informant interviews with all available providers in the health structures we visited (n=32) and with decisionmakers and administrative staff at the regional and national levels (n=14). Our data synthesis relied on systematic triangulation of the findings from our literature review, field visits, and stakeholder discussions and interviews, framed in a model of the different variables addressed. Our model of the relationships among Costa Rican developmental achievements, health service outputs (utilization and coverage rates), health service characteristics, and observed health policy features is shown in Figure 1 ▶.
FIGURE 1—
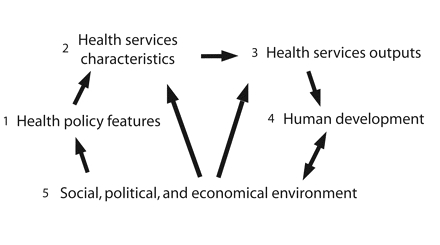
Relationships between the variables addressed.
FINDINGS
Health Policy Features
Until 1940, health care delivery in Costa Rica was based in hospitals and other facilities of the Ministry of Health, public charities, and banana companies. Since the creation of Costa Rica’s Social Security Administration (CCSS; Caja Costarricense de Seguro Social) in 1941, the country has had a social security system for wage-earning workers in place, with coverage gradually being extended to dependents.10
In 1973, the CCSS assumed control over the Ministry of Health and charitable health facilities with the exception of first-line health service facilities (i.e., facilities providing a first means of contact for health care users from an ascribed target population), which would be added some years later. The CCSS became the sole delivery institution of public hospital care, with 29 hospitals (23.9% of total health expenditures were devoted to public hospitals, as compared with 2% for private hospitals). This dominant quasi-monopolistic position of public hospitals was in contrast to the promotion by international aid agencies of multiple, competing providers, largely in the private sector. Because its health care system was unified from the outset, Costa Rica avoided the social insurance stratification typical of other Latin American countries and achieved a high degree of integration of its health care facilities.
Also in 1973, 5 years before the Alma Alta conference on primary health care, Costa Rica launched its Rural Health Program (Programa de Salud Rural) to extend comprehensive primary care services to rural areas.14 In 1976, the Community Health Program (Programa de Salud Comunitaria) was established, and this program applied the same principles of improving access to primary care services to suburban neighborhoods. A few years later, the 2 programs merged into a single primary health care department.
During the 1978 through 1982 government of Rodrigo Carazo, community participation was made the centerpiece of the social agenda. Health committees were activated in rural health posts under the Unit for People’s Participation (Unidad de Participación Popular), a newly created program division in the Ministry of Health. Meanwhile, the international context was changing. The Alma Ata concept of comprehensive primary health care, which stressed community participation, was challenged by the so-called strategy of selective primary health care, a package of low-cost technical interventions designed to address the primary disease problems of poor countries.15,16
When the United Nations Children’s Fund and the World Health Organization abandoned the notion of comprehensive primary health care for selective primary health care, Carazo’s successor and political opponent Luis Alberto Monge suspended the budget of the Unit for People’s Participation and renamed the unit the Community Promotion and Fomentation Program (Programa de Pro-moción y Fomento de la Comunidad). The unit was quietly dismantled in 1985.17
With the health system still lacking democratization, the plea for users’ and communities’ participation in the management of health facilities gained strength and was reinforced by the 1993 Deconcentration Law (Ley de Desconcentración Hospitalaria). At the peripheral level, users were now represented by elected health boards, together with social security representatives, employers, and social organizations. Although participation did not reach its full potential, a civil audit on the quality of the country’s democratic processes assigned a high ranking to health care provision as a result of its contribution to the population’s well-being.18,19
The employment drop of the 1980s was followed by an attempt on the part of the country to ensure that social security benefits were accessible to self-employed individuals and the state-subsidized poor. By the year 2000, social health insurance coverage was available to 82% of the Costa Rican population.20
The number of primary health care clinics (EBAIS; Equipos Básicos de Atención Integral en Salud) in the country began to increase in 1994. Health committees occasionally co-manage these clinics. In theory, there is 1 health committee (Junta de Salud y Seguridad Social) for each of the 83 administrative cantons of Costa Rica (cantons are not identical to the health subdivisions of areas and zones), but not all health committees are functional. The EBAIS share the market of first-line health services with the private sector (15.7% of total health expenditures are devoted to public first-line services, as compared with 14.4% for private first-line services).
After a failed pilot experiment with a capitation system in the 1980s under President Óscar Arias,21 contracting within the country’s publicly oriented services (hereafter “contracting in”) became the cornerstone of the Costa Rican health policy. As part of a World Bank project, the CCSS introduced performance agreements22 in 1996. Outputs of 5 priority programs for chronic and preventive care were defined on a negotiated basis by central and local decisionmakers. Failure to comply would prevent health services from gaining “budget bonuses.” However, in contradiction to international agencies’ policies, Costa Rica contracted with private, for-profit services only on a limited scale (e.g., as a means of reducing waiting lists or accessing expensive technology).
The government has provided the lion’s share of total health expenditures in Costa Rica. During the 1990s, approximately 7% of the GDP was allocated to the health sector, more than 70% of which was in the form of public funds and less than 30% in the form of private funds.23 Such a high percentage of public funds was unusual during that period. In most developing countries with more orthodox policies, including Colombia, total health expenditures grew mainly when the bulk of the budget was targeted toward the private, for-profit sector.24
It is interesting to compare the Costa Rican share of public health expenditures with that of high-income countries: Costa Rica is in line with Canada (71% of public funds in 2000), lags behind New Zealand and Sweden (78% and 85%, respectively), and fares far better than the United States (44%).25 These figures demonstrate the high degree of solidarity of the Costa Rican health system. Similarly, public insurance coverage illustrates the system’s equity. As an example, public health insurance coverage in 2000 was universal in Canada, New Zealand, and Sweden; in that same year, the coverage rate in Costa Rica was 82%, as compared with approximately 25% in the United States.26
By and large, Costa Rica’s health policies differ substantially from international aid recommendations. First, the CCSS is, in essence, the single insurer in Costa Rica; private insurance is virtually nonexistent. The World Bank is ambiguous on this issue. On the one hand, it warns against private health insurance, which is subject to market imperfections as a result of information asymmetries and is prone to risk selection.27 On the other hand, privatized health insurance promotes competition between insurers, as in Chile and Colombia.
Second, the CCSS both purchases and provides care services, and the Ministry of Health remains external to these processes. Consequently, no purchaser–provider split occurs in the public sector. This situation explains the low administrative cost (the proportion of the budget related to but not included in service provision or salaries) of between 3% and 4% since 1990,28 in sharp contrast with double-digit numbers among competing private insurers in Chile and Colombia.
Finally, the country’s contracting-in strategy, introduced in 1996, is not sustained by real contracts. Rather, it consists of a yearly negotiation between a CCSS central body (the purchasing directorate) and CCSS area medical officers on a list of performance indicators and targets for a series of programs. Targets are set according to resource availability, population size and density, and historical results. They are used merely to monitor coverage progress; their attainment does not influence health professionals’ incomes, and it influences only marginally their professional resources.
As suggested by the deviations of Costa Rica’s health policies from international aid agency recommendations described here, relations with international agencies have often been strained. When José María Figueres Olsen became president in 1994, he opposed recommendations for privatization of the International Monetary Fund, instead favoring greater government intervention in the economy. The World Bank subsequently withheld $100 million in financing to the country.29
More recently, in 2003, Costa Rica temporarily abandoned the Central American Free Market Agreement (CAFTA) discussions. In the best interest of its citizens, the Costa Rican government hesitated in accepting the US condition of opening up the insurance market.30 Costa Rica resumed negotiations in 2004, and Óscar Arias made joining CAFTA an essential part of his 2006 election platform. Now elected president for a second term, Arias faces considerable opposition of his plan, and the decision of whether to enroll in CAFTA will be decided by in an upcoming referendum.
Health Service Characteristics
The CCSS publicly oriented outpatient facilities include the EBAISs (approximately 1 per 5000 inhabitants), which comprise health centers with a general practitioner, an assistant nurse, a clerk, a pharmacy assistant, and a primary health technician, and second-line clinics (clinics providing first-referral care in the context of a multitiered health care system) located in proximity to the CCSS’s area headquarters. Physical facilities are in remarkably good condition. Individuals knowledgeable about the state of public facilities in most Latin American countries would view the quality, extent, and maintenance of Costa Rica’s hospital equipment as being at surprisingly high levels.
Outpatient facilities are attached to administrative areas (a total of 98 in the country). Both areas and hospitals are attached to medical regions (a total of 7). Several types of hospitals are operated by the CCSS, including 5 specialty national hospitals, 3 general national hospitals, 7 regional hospitals, 13 peripheral hospitals, and 10 major clinics serving as referral centers for the EBAISs. Public expenditures appear to have increased the share of the EBAISs (from 38% to 40% between 1997 and 2001), compared with hospitals (whose share decreased from 62% to 60% in the same time span23). Since the 1993 reforms, these first-line facilities have delivered individual biopsychosocial care services, although to varying degrees.31 They also offer family and community medical services as well as promotion and prevention programs.
The Costa Rican system promotes limited private care. Public facilities may refer patients to the private sector when they are overloaded, or patients may choose to see a private physician to avoid waiting lists. Patients must then pay their full consultation expenditure, but the CCSS reimburses drug and laboratory costs incurred during the private consultation. A similar system exists for corporate businesses, and in 1992, a system of free medical choice (i.e., no referral is needed) was established for consultations with certain specialists.32
The CCSS system has contracted with health cooperatives since 1988. Groups of physicians have been engaged to offer outpatient care; their budgets are determined by the CCSS, which also maintains property rights over infrastructure and equipment. The use of health cooperatives has been limited to the San José capital area, with 4 cooperatives having been organized to date. There are no plans to expand the model. An evaluation of the cooperatives by Gauri et al.33 suggested that the overall cost to the state was the same and changes in the quality of care delivered still had to be assessed. According to Homedes and Ugalde,30 the overall cost to the state increased as a result of unnecessary referrals, without evidence of improved quality.
Finally, the CCSS has signed contracting agreements with the University of Costa Rica and with ASeMeCo (Asociación de Servicios Médicos Costarricense), a private partner, for delivery of outpatient care in 3 areas of San José. The former agreement was evaluated and found to benefit the university more than it did the CCSS.34
All in all, the Costa Rican health system is rational. Its functioning is effective and efficient. It “trains” doctors and nurses by structuring their job and providing the necessary resources. The system’s organization permits and favors individualized, rather than one-size-fits-all, clinical activities. Medical schools offer in-service training within CCSS services. Unlike the case in many developing countries, continuous medical education is based not on seminars but on clinical rotations in well-functioning facilities. Area medical officers involve themselves in clinical medicine and use this experience to provide technical assistance to first-line physicians. Teamwork has been introduced and is practiced by many of the health teams. In fact, the limitations in competition between providers favor cooperation among them. Evaluation is part of the medical culture and is promoted by the system.
Costa Rican health professionals generally display strong motivation for their work and a high level of identification with their health system as a result of several factors, including the following:
Incomes are adequate, and there is a high degree of social prestige associated with their work.
The organizational structure leaves room for creative decisionmaking.
Managers below the regional level are appointed on technical merit, after a selection procedure that includes an examination.
The system is explicitly based on solidarity and equity, which may satisfy the political identities of certain professionals.
Health Service Output
In terms of health service output, although improvements are still needed, use and coverage rates are excellent. Use of medical health services in Costa Rica is high in comparison with other developing countries: there were 0.58 new general practitioner consultations and 0.33 new specialist consultations per capita during 2002, for example, and a hospital admission rate of 8.1%.35 However, there are problems with accessibility, as suggested by the changing share of emergency consultations, which increased from 16% of all medical consultations in 1980 to 38% in 2002. Still, the overall high use rates observed are compatible with a level of acceptable, affordable, and quality health care.
The coverage rates achieved by various types of programs are high. In 2002, for example, 96% of Costa Rican women used some form of contraception,36 and antenatal care services were provided to 87% of all pregnant women.35 Well-baby clinics were accessible to virtually all children aged under 1 year, and the immunization coverage rate was above 91% for all antigens.35,36 Coverage rates among chronic patients in first-line facilities were 73% for hypertensive disorders and 61% for diabetes.35
There has been effective integration between disease control programs and health care delivery services since the initiation of the “integrated care” system established by the 1993 reforms. Up until that time, CCSS units had delivered health care services and Ministry of Health units had provided disease control interventions, hampering integration of these entities.37 This more recent integration process, although still not completed, partly explains the disease control successes achieved in Costa Rica, such as a low malaria incidence of 48 per 100 000 in 2000 and no reported cases of measles in 2002.
Integration of care between the EBAISs (on the first line) and hospitals (as referral structures) can be improved. A referral–counterreferral system, although available in theory, is not well used. Significant numbers of primary care consultations occur in hospital emergency rooms, resulting in poor, non-integrated, nonholistic care. Part of this phenomenon can be seen in the administrative structure of the CCSS: the EBAISs have no administrative links with hospitals, area medical officers have no authority over hospitals, and budget allocations take into account past workloads, resulting in EBAISs and hospitals competing for the same patients instead of performing complementary functions.
The ways in which promotion and prevention are implemented also lead to patients being pushed to emergency departments. For example, it is perhaps the case that prevention at the primary health care level is overly standardized. The existence of strong mandatory preventive programs in the EBAISs leads doctors to neglect nonstandard prevention activities during consultations (i.e., activities not included in their established performance agreements, for instance addressing obesity, depression, tobacco, and drug addiction).
In addition, certain disease control programs (especially those focusing on chronic conditions such as diabetes and hypertension) and care services targeting high-risk groups (pregnant women, children younger than 5 years, adolescents, and elderly) overstretch the performance agreements of the EBAISs. As a consequence, the general practitioners in these primary care facilities see their availability for curative services reduced, with hospital emergency departments filling the gap.
An additional explanation for hospitals’ large share of primary care services is that emergency departments are particularly attractive to noncontributors (who are responsible for up to 1 of every 3 hospital consultations) such as migrants and citizens not covered by social insurance.35 There is also room to improve overall health care efficiency, as suggested by the following: (1) EBAISs (as described) do not function particularly well as gatekeepers; (2) between 1997 and 2002, the number of laboratory tests increased by 45% and prescription drug consumption by 24% (or more, given that data from private providers might not be included in these figures)35; (3) average lengths of stay are 3 days or less in some peripheral hospitals,35 possibly as a result of avoidable admissions; and (4) the cesarean section rate was close to 22% in 2002 (UNICEF and World Health Organization guidelines say the maximum acceptable level is 15%).35,36
Effects on Human Development
With its combination of a middle-income population and a policy emphasis on human development, Costa Rica is an exceptional developing country. With 40% of its population still living in rural areas, the following achievements of Costa Rica in 2002 are even more remarkable36:
Only 9.5% of the population was below the $2 per day income poverty level and only 2.0% below $1 per day (vs 22.6% and 8.2%, respectively, in Colombia and 26.3% and 9.9% in Mexico).
Ninety-five percent and 93% of the population had sustainable access to drinking water and sanitation, respectively (vs 91% and 86% in Colombia and 88% and 74% in Mexico).
The literacy rate was 95.8% (vs 92.1% in Colombia and 90.5% in Mexico).
The Gini index, a measurement of inequality in the distribution of income or consumption within a country, expressed as a percentage, with 0 representing perfect equality and 100 representing perfect inequality. was 46.5 (vs 57.6 in Colombia and 54.6 in Mexico).
The country’s gender-empowerment initiatives were superior to those of all other Latin American countries.
Life expectancy at birth was 78 years (second only to Canada in the Americas).
The infant mortality rate was 9 per 1000, representing a 7-times reduction over a 3-decade span (vs 19 per 1000 and a 4-times reduction in Colombia and 24 per 1000 and a 3-times reduction in Mexico).
The tuberculosis prevalence rate was 19 per 100 000 population (vs 69 in Colombia and 44 in Mexico).
Several of these features are related to the social commitments of successive Costa Rican governments. The absence of armed forces, one of the country’s unique features, allowed for strong social investments, with public expenditures on health and education, respectively, of 4.9% and 4.7% of GDP in 2001 (as compared with 3.6% and 4.4% in Colombia and 2.7% and 5.1% in Mexico).6
Numerous indicators suggest effects directly attributable to health services. For example, comparisons of infant and maternal mortality reductions with countries in the same region at similar income levels reveal that Costa Rica has made significant advances (Table 2 ▶). Also, the perinatal mortality rate dropped from 12.0 per 1000 in 1972 to 5.4 per 1000 in 2001,39 which suggests obstetric improvements. Finally, pneumonia-specific mortality among infants aged younger than 1 year dropped from 5.4 per 1000 in 1972 to 0.3 per 1000 in 2001,39 suggesting improved and faster access to health services, and tuberculosis-specific mortality in the general population decreased from 7.2 per 100 000 in 1972 to 4.4 per 100 000 in 20016 despite increased incidence levels, suggesting effective interventions.
Public policies in support of Costa Rica’s health services help explain these high development standards and health status indicators. Whereas the average percentage of private health expenditures at the end of the 20th century was 58% among Latin American countries as a whole, it was only 25% in Costa Rica,40 and only 0.12% of Costa Rican households had suffered a catastrophic health expenditure (in sharp contrast with Colombia, for instance, where 6.26% of households incurred such an expenditure).41 In addition, Costa Rican public health expenditures have focused on equity, with 29% targeting the poorest income quintile and 11% targeting the richest,42 in 2000. This situation differs markedly from that of Ecuador, for example, where the richest quintile accounted for 30%23 of public health expenditures in 2000.
The Costa Rican approach reduced health inequities between 1980 and 2000 as well; potential years of life lost were reduced by 48% in the poorest quintile of the population and by 39% in the richest.20 Public health expenditures were found to be the most equitable component of social investment,42 with the poorest families receiving the largest proportion of resources. This investment is progressive in that it reduces income inequality. However, those groups that contribute most to social insurance (i.e., the upper income quintiles) are the ones that use its services the least, given their tendency to seek services from private ambulatory providers. This situation may result in reductions in solidarity and support for the CCSS among members of the higher classes.
Not everything in Costa Rica is positive. For example, before showing a reverse trend in 2002, income inequality rose between 1997 and 2001, with households in the richest quintile earning 8 times more than households in the poorest quintile in 1997 and 11 times more in 2001.43 A similar pattern was evident in the human development index, which decreased from 0.889 in 1997 to 0.797 in 2000 and then rose from 0.821 in 2001 to 0.834 in 2004. Public health expenditures decreased from 77% to 71% between 1991 and 2001.23 The major component of the increase in private expenditures was household-level out-of-pocket payments.
The CCSS has continued to contract out more diagnosis and treatment procedures to the private sector as well. As a result, more patients are using private services, in which overprescription is a common practice. For instance, between 1997 and 2002, the number of x-rays requested by private doctors and paid for by the CCSS increased by 41%.35 Of equal concern is that, as the share of private health expenditures has increased, total expenditures on health care have risen steeply.23
All in all, Costa Rica’s health policy during the past 30 years has been effective and equitable. The country’s health system basically comprises a form of compulsory social health insurance, with 50% of contributions from households (25% direct contributions to social insurance and 25% out of pocket), 40% from employers, 5% from the state, and a very small percentage from international loans. Several political and social elements have allowed this relative equity in the dimensions of financing, access, and health outcomes. For example:
Intelligent decisionmakers have been involved in policymaking, some of them educated in Europe (for instance, Calderón Guardia, considered the “father” of Costa Rican social insurance, observed and appreciated the Belgian social security system during his training in that country).
Middle-class groups with a vision and strong trade unions had an impact as well. Moreover, given that the middle classes still use CCSS services, they provide indispensable political support. A certain degree of inequity in use of public expenditures may be the necessary price to pay for a public sector with a high level of political support.
Recently, several factors have jeopardized the Costa Rican political and health systems. First, some of the executive staff of the CCSS have come under attack by the press, leading to the resignation of a CEO and several top executives. Moreover, various former heads of state and 1 ex-president of the CCSS are under investigation. Painful as these events may seem, they may actually lead to an institutional strengthening of Costa Rica, where the vast majority of citizens proudly express confidence in their political and judicial structures.44 Second, for more than 10 years, CCSS executive officers have been selected through a political process. The institution has generally overcome this drawback through the strength of its organization at the operational and middle administration levels.
Third, there is an oversupply of physicians because of increases in private medical faculties. This group could represent a future, powerful lobby for the privatization of primary health care services. Finally, the most worrying phenomenon is the continuing external pressure,30 with clear economic interests, to privatize large sectors of the health delivery system, including primary care. Until now, a majority of health professionals and the Costa Rican population have resisted such threats.
CONCLUSIONS
The impressive advances made by the Costa Rican health system have been the result of an intelligent social and democratic long-term policy and the establishment of a public compulsory social health insurance system. Such coherence in policy might be equally or more important than financing, as highlighted by the poor improvements in the health status of populations in other comparable Latin American countries.
Necessary improvements in the system could target relatively minor issues. Bio-psychosocial and patient-centered care could be promoted in primary health care services, reducing the bureaucratic burden generated by disease control and prevention programs. In-service training and mentoring could be introduced, as well as action research and evaluation applied to health programs. Together, these measures could optimize time management among first-line health professionals, increase efficiency, and reduce waiting lists.
In addition, coordination of primary and hospital care and continuity of care could be improved with the organization of local health systems. Hospital costs could be cut without hampering the quality of health care (for instance, by avoiding unnecessary admissions). The Ministry of Health (in a true role of stewardship) should control the proliferation of private medical schools to avoid a contingent of second-rate professionals. Finally, the CCSS should reevaluate its overstretched contracting-in mechanism (consisting of performance agreements) and carefully analyze its limited experiences in contracting with private, for-profit services.
International entities should pay particular attention to several successful policy features of Costa Rica’s health system:
The unique, unified public system facilitates integration.
Publicly oriented services function as the dominant (but not monopolistic) means of care delivery.
Contracting in is a cornerstone of the national health policy (as opposed to the practice of contracting with private, for-profit services).
Both users and communities participate in health service management (in contrast to the situation in the private, for-profit sector).
Government expenditures represent the bulk of overall health expenditures.
There is, for the most part, no purchaser–provider split or hospital managerial autonomy.
There is a single public insurer (private insurance being virtually nonexistent).
In view of the remarkable and long-lasting achievements of the heterodox Costa Rican social and democratic approach, we believe Costa Rica should become a benchmark for international donors and decisionmakers. In fact, orthodox health policy axioms may need to be reassessed.
Acknowledgments
We are indebted to the Belgian Directorate-general of Development Cooperation for the funding of the research and to Rocío Saenz, MD, ex-minister of health of Costa Rica, for pivotal comments.
Note. The authors are solely responsible for any errors present in this article.
Peer Reviewed
Contributors J.P. Unger and P. De Paepe originated the study, implemented the field visits in Costa Rica, and led the writing of the first draft. R. Buitrón and each of the other 3 authors helped to conceptualize ideas and interpret findings for the final version of the article. W. Soors assisted with the study and completed a second version of the article.
References
- 1.Investing in Health: World Development Report. Washington, DC: World Bank; 1993.
- 2.World Bank. Development committee press conference. Available at: http://go.worldbank.org/7UV2WOBB60. Accessed August 8, 2007.
- 3.Lobe J. Learn from Cuba, says World Bank. Available at: http://www.hartford-hwp.com/archives/43b/index-e.html. Accessed August 8, 2007.
- 4.Annual Freedom in the World Country Scores, 1972 Through 2003. Washington, DC: Freedom House; 2004.
- 5.Human Development Report 2003. Millennium Development Goals: A Compact Among Nations to End Human Poverty. New York, NY: United Nations Development Programme; 2003.
- 6.Human Development Report 2004: Cultural Liberty in Today’s Diverse World. New York, NY: United Nations Development Programme; 2004.
- 7.World Bank. Spotlight on Costa Rica and Cuba. Available at: http://econ.worldbank.org/wdr/wdr2004/text-30023. Accessed July 26, 2007.
- 8.The State of the World’s Children 2003. New York, NY: United Nations Children’s Fund; 2003.
- 9.World Development Indicators 2001. Washington, DC: World Bank; 2001.
- 10.Homedes N, Ugalde A. Privatización de los servicios de salud: las experiencias de Chile y Costa Rica [Privatization of Health Services: the Experience of Chile and Costa Rica]. Gac Sanit. 2002;16:54–62. [DOI] [PubMed] [Google Scholar]
- 11.Rosero-Bixby L. Infant mortality in Costa Rica: explaining the recent decline. Stud Fam Plann. 1986; 17:57–65. [PubMed] [Google Scholar]
- 12.Roser-Bixby L. Socioeconomic development, health interventions and mortality decline in Costa Rica. Scand J Soc Med. 1991;46:33–42. [PubMed] [Google Scholar]
- 13.Sauma P, Garnier L. Efecto de las políticas macro-económicas y sociales sobre la pobreza en Costa Rica [The impact of macro-economic and social policies on poverty in Costa Rica]. In: Lanuza E, Taylor L, Morley S, eds. Política macroeconómica y pobreza: América Latina y el Caribe [Macroeconomic Policy and Poverty: Latin America and the Caribbean]. Madrid, Spain: Programa de Naciones Unidas para el Desarrollo; 1998:311–353.
- 14.Seligson MA, Martínez J, Trejos JD. Reducción de la pobreza en Costa Rica: el impacto de las políticas públicas [Poverty reduction in Costa Rica: the impact of public policies]. In: Zevallos JV, ed. Estrategias para re-ducir la pobreza en América Latina y el Caribe [Poverty Reduction Strategies in Latin America and the Caribbean]. Quito, Ecuador: Programa de Naciones Unidas para el Desarrollo; 1997:105–192.
- 15.Walsh JA, Warren KS. Selective primary health care—interim strategy for disease control in developing countries. N Engl J Med. 1979;301:967–974. [DOI] [PubMed] [Google Scholar]
- 16.Cueto M. The origins of primary health care and selective primary health care. Am J Public Health. 2004; 94:1864–1874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morgan LM. International politics and primary health care in Costa Rica. Soc Sci Med. 1990;30:211–219. [DOI] [PubMed] [Google Scholar]
- 18.Programa Estado de la Nación en Desarrollo Humano Sostenible. Equidad e integración social: quinto informe sobre el Estado de la Nación. [Equity and Social Integration: Fifth Report on the State of the Nation]. San José, Costa Rica: Estado de la Nación; 1999.
- 19.Programa Estado de la Nación en Desarrollo Humano Sostenible. Informe de la auditoria ciudadana sobre la calidad de la democracia en Costa Rica. [The Report of the Civil Audit on the Quality of Democracy in Costa Rica]. San José, Costa Rica: Estado de la Nación; 2001.
- 20.Saenz Madrigal R, Acuña Ulate E. Análisis sectorial de salud—Costa Rica. [Health Sector Analysis—Costa Rica]. San José, Costa Rica: Ministerio de Salud; 2002.
- 21.Martínez Franzoni J. ¿Presión o legitimación? Poder y alternativas en el diseño y adopción de la reforma de salud en Costa Rica, [Pressure or Legitimation? Power and Alternatives in the Design and Implementation of Health Reform in Costa Rica]. 1988–1998. Available at: http://www.scielo.br/pdf/hcsm/v13n3/03.pdf. Accessed July 26, 2007. [DOI] [PubMed]
- 22.Performance Agreements. Shaping the Future of Social Protection: Access, Financing and Solidarity. Montevideo, Uruguay: Economic Commission for Latin America and the Caribbean; 2006.
- 23.Gasto y financiamiento de la salud en Costa Rica: situación actual, tendencias y retos. [Health Expenditure and Financing in Costa Rica: Current Situation, Trends and Challenges]. San José, Costa Rica: Pan American Health Organization; 2003.
- 24.De Groote T, De Paepe P, Unger JP. Colombia: in vivo test of health sector privatization in the developing world. Int J Health Serv. 2005;35:125–141. [DOI] [PubMed] [Google Scholar]
- 25.OECD Health Data 2004: A Comparative Analysis of 30 Countries. Paris, France: Organisation for Economic Co-operation and Development; 2004.
- 26.OECD Health Data 2003: A Comparative Analysis of 30 Countries. Paris, France: Organisation for Economic Co-operation and Development; 2003.
- 27.Preker AS. Health, Nutrition and Population Strategy. Washington, DC: The World Bank; 1997.
- 28.Rodríguez Herrera A. La reforma de salud en Costa Rica. [Health reform in Costa Rica]. Santiago, Chile: Comisión Económica par América Latina y el Caribe; 2006.
- 29.Mkandawire T. Disempowering New Democracies and the Persistence of Poverty. Geneva, Switzerland: United Nations Research Institute for Social Development; 2006.
- 30.Homedes N, Ugalde A. Why neoliberal health reforms have failed in Latin America. Health Policy. 2005;71:83–96. [DOI] [PubMed] [Google Scholar]
- 31.Roser-Bixby L. Spatial access to health care in Costa Rica and its equity: a GIS-based study. Soc Sci Med. 2004;58:1271–1284. [DOI] [PubMed] [Google Scholar]
- 32.Mesa-Lago C. Las reformas de salud en América Latina y el Caribe: su impacto en los principios de la se-guridad social. [Health Reform in Latin America and the Caribbean: Its Impact on the Principles of Social Security]. Santiago, Chile: Naciones Unidas; 2005.
- 33.Gauri V, Cercone J, Briceno R. Separating financing from provision: evidence from 10 years of partnership with health cooperatives in Costa Rica. Health Policy Plann. 2004;19:292–301. [DOI] [PubMed] [Google Scholar]
- 34.Villalobos Solano LB, Chamizo García H, Piedra González M, Navarro Vargas A, Carballo Rosabal M, Vargas Fuentes M. ¿Es la contratación gubernamental de servicios de salud privados en el primer nivel de atención en Centroamérica una opción para asegurar una atención eficiente, equitativa y sostenible? [Is Contracting Private Health Services at First-Line Level an Option for Assuring Efficient, Equitable and Sustainable Care in Central America?]. San José, Costa Rica: Universidad de Costa Rica; 2004.
- 35.Departamento de Información Estadística de los Servicios de Salud. Estadísticas generales de los servicios de atención de la salud, 1980–2002. [Health Care Services, General Statistics, 1980–2002]. San José, Costa Rica: Caja Costarricense de Seguro Social; 2003.
- 36.UNICEF, World Health Organization, United Nations Population Fund (UNFPA). Guidelines for Monitoring the Availability and Use of Obstetric Services. New York, NY: UNFPA; 1997. Available at: http://www.who.int/reproductive-health/publications/unicef/monitoring_obstetric_services.pdf. Accessed September 6, 2007.
- 37.Indicadores básicos: situación de salud en Costa Rica 2003. [Basic Indicators: the Health Situation in Costa Rica 2003]. San José, Costa Rica: Ministerio de Salud; 2003.
- 38.Unger JP, De Paepe P, Green A. A code of best practice for disease control programmes to avoid damaging health care services in developing countries. Int J Health Plann Manage. 2003;18:S27–S39. [DOI] [PubMed] [Google Scholar]
- 39.Departamento de Información Estadística de los Servicios de Salud. Cambios en la morbilidad y mortali-dad por edad y sexo, Costa Rica, 1987, 1992, 1997 y 2002 [Morbidity and Mortality Statistics by Age and Gender, Costa Rica, 1987, 1992, 1997 and 2002]. San José, Costa Rica: Caja Costarricense de Seguro Social; 2003.
- 40.Molina R, Pinto M, Henderson P, Vieira C. Gasto y financiamiento en salud: situación y tendencias. [Health Expenditure and Financing: situation and Trends]. Rev Panam Salud Publica. 2000;8:71–83. [DOI] [PubMed] [Google Scholar]
- 41.Xu K, Evans DB, Kawabata K, Zeramdini R, Klavus J, Murray CJ. Household catastrophic health expenditure: a multicountry analysis. Lancet. 2003;362:111–117. [DOI] [PubMed] [Google Scholar]
- 42.Trejos JD. La equidad de la inversión social en el 2000: Octavo informe sobre el Estado de la Nación en desarrollo humano sostenible. [The Fairness of Social Spending in 2000: Eighth Report on the State of the Nation in Sustainable Human Development]. San José, Costa Rica: Estado de la Nación; 2002.
- 43.Compendio estadístico. [Statistical summary]. Available at: http://www.estadonacion.or.cr/Compen-dio/ind_compendio.html. Accessed August 8, 2007.
- 44.Seligson MA. Toward a Model of Democratic Stability: Political Culture in Central America. Tel Aviv, Israel: Tel Aviv University; 2000.


