Abstract
Context
Understanding the temporal sequencing of alcohol use disorders (AUDs) and comorbid mood and anxiety disorders may help to disentangle the etiological underpinnings of comorbidity. Methodological limitations of previous studies, however, may have led to inconsistent or inconclusive findings.
Objective
To describe the temporal sequencing of the onset of AUDs relative to the onset of specific comorbid mood and anxiety disorders using a large, nationally representative survey.
Results
AUD onset tended to follow the onset of 2 of the 9 mood and anxiety disorders (specific and social phobia). The onset of alcohol abuse tended to precede the onset of 5 of the 9 mood and anxiety disorders (GAD, panic, panic with agoraphobia, major depression, and dysthymia), whereas the onset of alcohol dependence tended to precede the onset of only 2 of the 9 mood and anxiety disorders (GAD and panic). Lag times between primary and subsequent disorders generally ranged from 7–16 years. Comorbid individuals whose alcohol dependence came after panic with agoraphobia, hypomania, and GAD had increased risk of persistent alcohol dependence.
Conclusion
Alcohol abuse, but not dependence, precedes many mood and anxiety disorders. If the primary disorder does in fact play a causative or contributing role in the development of the subsequent disorder, this role can best be described as “temporally distal.” However, in assessing the risk for persistent alcohol dependence, clinicians should not only consider the type of comorbid mood/anxiety disorder, but also the temporal ordering of these disorders.
Keywords: age of onset, mood disorders, anxiety disorders, alcohol use disorders, comorbidity, NESARC, epidemiology
1. INTRODUCTION
Consistently high rates of comorbidity have been found between alcohol use disorders (AUDs) and a number of mood and anxiety disorders in both national epidemiological surveys (Dawson et al., 2005a; De Graaf et al., 2003; Grant et al., 2004; Hasin et al., 2007; Kessler et al., 1996; Regier et al., 1990; Swendsen et al., 1998) and clinical samples (Hesselbrock et al., 1985; Ross et al., 1988; Swendsen and Merikangas, 2000). For instance, studies using nationally representative data from the National Epidemiological Survey on Alcohol and Related Conditions have reported significant 12-month and lifetime associations between AUDs and any mood disorder (odds ratios ≥ 2.2 and 2.4, respectively) and any anxiety disorder (odds ratios ≥ 1.7 and 2.3, respectively) (Grant et al., 2004; Hasin et al., 2007;). Individuals with comorbidity present great challenge to treatment since they have more severe symptoms (Grant et al., 1996) and greater disability (Burns and Teesson, 2002) than individuals with AUDs only, and may pose a greater economic burden to society due to their higher utilization of treatment services (Burns and Teesson, 2002; Kessler et al., 1996).
In an effort to understand the etiological underpinnings of mood/anxiety disorder and AUD comorbidity, Lehman et al. (1989) reviewed several theoretical causal pathways where: a) the mood/anxiety disorder causes the AUD (e.g., as individuals engage in “self-medication” attempting to alleviate psychological distress); b) the AUD causes the mood/anxiety disorder (e.g., as alcohol exacerbates or induces psychological symptoms); c) both disorders are initially unrelated, yet exacerbate each other; and d) an unknown antecedent factor gives rise to both disorders.
Disentangling the temporal sequencing of these disorders is a step toward establishing the real-life plausibility of these pathways. To this end, researchers have distinguished between primary versus secondary disorders (Compton, et al., 2000; De Graaf et al., 2003; Grant et al., 1996; Hesselbrock et al., 1985; Kessler et al., 1996; Kessler, et al., 1997; Swendsen, et al., 1998; Zilberman et al., 2003). Operationally, a “primary” disorder is one whose age of onset precedes that of another “secondary” disorder. Thus, by comparing the age of onset of psychological and alcohol use disorders among comorbid individuals, and consequently determining the likelihood of their primary versus secondary status, the existence of some etiological pathways may be supported while others may be ruled out.
Previous temporal sequencing studies have led to inconsistent or inconclusive findings. For example, Kessler et al. (1997) found that major depression was 1.7 times more likely to precede alcohol abuse in women, whereas De Graaf et al. (2003) reported the opposite, that alcohol abuse was 1.3 times more likely to precede major depression in women. This and other inconsistencies may be potentially due to a variety of methodological differences and/or limitations including a) use of differing versions of DSM criteria to obtain clinical diagnoses (Cho et al., 2002; De Graaf et al., 2003; Hesselbrock et al., 1985; Kessler et al., 1996; Kessler et al., 1997; Merikangas et al., 1998; Powell et al., 1987; Ross et al., 1988; Swendsen et al., 1998) b) aggregating data across genders (Kessler et al., 1996; Merikangas et al., 1998; Swendsen et al., 1998), psychological disorders (Bakken et al., 2003; Cho et al., 2002; Kessler et al., 1996; Merikangas et al., 1998; Swendsen et al., 1998), and any AUDs (Ross et al., 1988; Swendsen et al., 1998) versus analyzing them separately and c) using clinical versus epidemiological samples (Bakken et al., 2003; Hesselbrock et al., 1985; Powell et al., 1987; Ross et al., 1988).
Although a number of epidemiological studies have reported the age of onset of psychological disorders and AUDs in the general population (Burke et al., 1990; Christie et al., 1988; Kessler et al., 2005), few have systematically examined the age of onsets of these disorders and their lag times among comorbid individuals. De Graaf et al. (2003) reported lag times between the onset of mood disorder and alcohol dependence in comorbid men and women. In their analysis, however, mood disorders were aggregated and treated as one group, thus obscuring potential differences in lag times among specific mood disorders. Similarly, Kessler et al. (1996) compared the onsets of aggregated “mental disorder” and “addictive disorder” classes. Other studies reported the age of onset of major depression and any AUD in comorbid individuals, according to temporal sequencing status (Grant et al., 1996; Hanna and Grant, 1997). These studies, however, aggregated alcohol abuse and dependence, and did not provide data on other mood or anxiety disorders.
A number of studies have documented an association between comorbidity and negative clinical correlates, such as disorder severity (Cho et al., 2002; Grant et al., 1996; Hanna and Grant, 1997; Hasegawa et al., 1991; Hesselbrock et al., 1985; Powell et al., 1987; Swendsen et al., 1998). Less is known, however, whether the clinical risk associated with comorbidity varies as a function of temporal sequencing status. In other words, which groups of comorbid individuals, if any, have a worse prognosis: those with primary mood/anxiety disorders or those with primary AUDs? Most studies investigating this line of research questions have focused on major depression (Grant et al., 1996) or bipolar disorder only (Goldstein et al., 2006) or have aggregated across disorders (Kessler et al., 1996), thus ignoring the independent impact of specific disorders. Other studies have evaluated the impact of specific primary psychological disorders, but not primary AUDs, in predicting persistence of AUD (Kessler et al., 1997; Ross, 1995).
The present study addresses the aforementioned limitations and gaps in the literature by using data from the NESARC (2001–2002). The NESARC is the largest known epidemiological comorbidity survey conducted to date (n=43,093) and is based on a nationally-representative U.S. sample. Most importantly for the present study, the NESARC utilizes DSM-IV criteria to obtain lifetime diagnoses for a number of psychiatric conditions, including alcohol abuse and dependence, and nine mood and anxiety disorders (MADs). The large sample size utilized for the assessment of age of onset of these disorders allows for more reliable temporal sequencing estimates.
The major aims of the present study are four-fold:
To document the age of onset of DSM-IV AUDs and MADs in the general and comorbid population in the United States.
To describe the temporal sequencing of the onset of AUDs relative to the onset of specific comorbid MADs.
To estimate the lag times between the onsets of AUDs and comorbid MADs disorders.
To determine if the onset order of prior-to-past-year AUDs relative to comorbid MADs is associated with the persistence of AUDs, as indicated by the presence of past-year AUDs.
All study aims are investigated by gender.
2. METHODS
2.1. Data
The NESARC is a national household survey designed and conducted by the National Institute of Alcohol Abuse and Alcoholism (NIAAA). Wave 1 NESARC used a multistage stratified probability sample representative of civilian, noninstitutionalized adults (age 18 and older) residing in the United States, including all 50 states and the District of Columbia. Military personnel living off base and persons living in non-institutionalized group quarters housing, such as boarding houses, shelters, and dormitories, were also included (Grant et al., 2003). The sampling frames for housing units and group quarter units were derived from the Census 2000/2001 Supplementary Survey and the Census 2000 Group Quarters Inventory, respectively. The NESARC over-sampled Blacks, Hispanics, and young adults (ages 18–24) to allow for more reliable estimates of these groups. Data were collected via face-to-face, computer-assisted interviews in household settings. From each household, one adult was selected for interview. The overall response rate for NESARC was 81 percent, derived from a sampling frame response rate of 99 percent, a household response rate of 89 percent, and a person response rate of 93 percent. Details of the NESARC sampling design and methodology can be found in “Source and Accuracy Statement for Wave 1 of the 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions” (Grant et al., 2003).
Respondents with a lifetime DSM-IV AUD or at least one of the nine MADs (including 4 mood disorders: major depression, dysthymia, mania, and hypomania; and 5 anxiety disorders: panic without agoraphobia, panic with agoraphobia, specific phobia, social phobia, and general anxiety disorder) were selected as the study sample (N = 19,504).
2.2. Measures
2.2.1. Clinical Disorder Assessment
All clinical diagnoses in this study are lifetime diagnoses. They were ascertained by the NIAAA Alcohol Use Disorders and Associated Disabilities Interview Schedule – DSM-IV Version (AUDADIS-IV) (Grant et al., 2001), a state-of-the-art structured diagnostic interview designed for use by lay interviewers. The AUDADIS-IV uses an extensive list of symptom questions to operationalize separate diagnoses on the basis of DSM-IV criteria.
AUDADIS-IV diagnoses for alcohol abuse and dependence required respondents to meet DSM-IV criteria for at least 1 of 4 abuse criteria and at least 3 of 7 dependence criteria, respectively. Symptoms of dependence were required to cluster together within the same 1-year period in order for a respondent to meet dependence criteria. In this paper, the category “alcohol abuse” is limited to individuals with alcohol abuse only and not in combination with alcohol dependence, whereas the category “alcohol dependence” includes dependent individuals with or without alcohol abuse. The test-retest reliabilities of the AUDADIS-IV alcohol disorder diagnoses were excellent, exceeding kappa (k)=.74 (Grant et al., 2004). The validity of these diagnoses has been well-documented in a number of studies (Grant et al., 2004; Harford and Grant, 1994; Hasin et al., 1997a; Hasin et al., 1997b; Hasin and Paykin, 1999; Nelson et al., 1999; Ustun et al., 1997).
The NESARC also provided diagnoses for all mood disorders (i.e., major depression, dysthymia, mania, and hypomania) and anxiety disorders (i.e., panic without agoraphobia1, panic with agoraphobia, general anxiety disorder (GAD), specific phobia, and social phobia). Consistent with the DSM-IV, these diagnoses were classified as syndromes such that to meet criteria for a particular disorder, respondents had to endorse the requisite number of symptoms within a specified time frame. The data set includes both hierarchical and non-hierarchical diagnoses (i.e., including those induced by medical conditions or substance use). For the purpose of the current study, the latter were used in the analysis since all mood and anxiety disorders, regardless of their original causes, could possibly precipitate or be precipitated by the onset of an AUD and consequently play a role in the continued persistence of the AUD, one of the key outcomes of this study. The AUDADIS-IV test-retest reliabilities of these diagnoses ranged from fair to good (k=.42 for specific phobia to k=.64 for major depression) (Grant et al., 2004). The validity of these diagnoses was demonstrated by the high statistical significance of most of these diagnoses as predictors of mental disability using the Short-Form-12v2 (Grant et al., 2004; Ware et al., 2002).
2.2.2. Age of Disorder Onset and Lag Time
Age of disorder onset was retrospectively obtained from retrospective self reports. Respondents meeting criteria for a particular lifetime disorder were asked how old they were when they had the first episode of that disorder2. Answers were recorded as age in years. Missing data for age of disorder onset among individuals with a given psychiatric disorder ranged from 1% (major depression) to 9.5% (alcohol abuse). Lag times between two comorbid disorders were calculated by subtracting the age of onset of the earlier-occurring disorder from the age of onset of the later-occurring disorder.
2.2.3. Temporal Sequencing
Individuals with lifetime comorbidity of a MAD and AUD were categorized into one of three temporal sequencing groups based on the relative age of disorder onset:
MAD Primary – the age of onset of the MAD preceded the age of onset of the AUD
Concurrent – the MAD and the AUD both initially occurred at the same age
Alcohol Disorder Primary – the age of onset of the AUD preceded the age of onset of the MAD
2.2.4. Persistence of AUD
A dichotomous outcome variable was created to describe whether individuals with a prior-to-past-year AUD still met criteria for a past-year AUD (coded 1) or had sustained partial or full AUD remission (coded 0).
2.3. Analysis
Descriptive statistics were calculated for the mean age of onset of all disorders and for the corresponding lag times between the onset of AUDs and MADs. In order to determine the extent to which one disorder precedes the other, for each MAD, an alcohol primacy ratio (APR) was also calculated by dividing the proportion of primary AUD by the proportion of primary MAD. An APR greater than 1 indicates a tendency for the AUD to occur before the MAD, whereas an APR less than 1 indicates a tendency for the MAD to occur before the AUD.
Logistic regression models were used to assess whether the onset order of AUDs relative to MADs, among individuals with prior-to-past-year AUD, is associated with the outcome, persistence of AUDs, as measured by the presence of past-year AUD. The models estimated odds ratios (ORs) (and 95% confidence intervals (CIs)) for past-year AUD. The main predictor of interest was temporal sequencing status, a three-level categorical variable, including two prior-to-past-year, temporal sequencing groups (i.e., MAD primary and AUD primary) as well as a non-comorbid referent group consisting of individuals with prior-to-past-year AUD without the MAD in question. For convenience, this referent group is referred to as the AUD only group. Individuals with no history of AUD (i.e., MAD only) were excluded from these models since the outcome is conceptualized as persistence of AUD. All ORs were adjusted for the number of years since the onset of the AUD to account for the fact that a) individuals with more recent AUD onset are more likely to have past-year AUD (Dawson et al., 2005b), and b) the temporal sequencing groups are confounded by this variable. For instance, respondents in the MAD primary group were more likely to have a more recent AUD onset than those in the AUD primary group.
All statistics and models presented were estimated separately for men and women. In addition, the significance of sex differences was evaluated using z-score tests (for APR differences), t-tests (for lag time differences), and via the interaction between sex and temporal sequencing status (in the pooled persistence models). The significance of APRs was assessed using the Taylor series linearization method with the Proc Ratio procedure of SUDAAN (Research Triangle Institute, 2005). All analyses were conducted using SUDAAN to adjust for the complex sampling design effect of the NESARC.
3. RESULTS
3.1. Age of Onset of Lifetime AUDs and MADs in the General Population
Table 1 shows that, in the general population, alcohol dependence appeared at an earlier mean age of onset than six MADs: panic, panic with agoraphobia, GAD, mania, major depression and dysthymia. Alcohol dependence appeared at about the same mean age of onset as hypomania (24.1 yrs vs. 23.3 yrs). Alcohol dependence appeared at a later mean age of onset than two disorders: specific phobia and social phobia. Results were similar for alcohol abuse, which appeared at a slightly earlier mean age of onset than alcohol dependence. In general, the same pattern of results held when men and women were examined separately.
Table 1.
Prevalence and Mean Age of Onseta of Lifetime DSM-IV Disorders in the General Population, NESARC 2001–2002.
| Total | Men | Women | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pop. Prevalence | Age of Onset | Pop. Prevalence | Age of Onset | Pop. Prevalence | Age of Onset | ||||||||||
| DSM-IV Disorder | % | SE | n | Mean (yrs) | SE | % | SE | n | Mean (yrs) | SE | % | SE | n | Mean (yrs) | SE |
| Alcohol Use Disorders | |||||||||||||||
| Alcohol Abuse Only | 17.8 | 0.25 | 6427 | 22.5 | 0.11 | 24.6 | 0.39 | 4104 | 22.5 | 0.14 | 11.5 | 0.26 | 2323 | 22.5 | 0.18 |
| Alcohol Dependence | 12.5 | 0.21 | 4696 | 24.1 | 0.15 | 17.4 | 0.35 | 2906 | 23.9 | 0.18 | 8.0 | 0.23 | 1790 | 24.4 | 0.25 |
| Anxiety Disorders | |||||||||||||||
| Specific Phobia | 9.5 | 0.19 | 3922 | 14.6 | 0.22 | 6.2 | 0.22 | 1103 | 14.3 | 0.42 | 12.5 | 0.28 | 2819 | 14.7 | 0.26 |
| Social Phobia | 5.0 | 0.13 | 1949 | 15.2 | 0.30 | 4.3 | 0.18 | 719 | 14.9 | 0.45 | 5.8 | 0.19 | 1230 | 15.4 | 0.38 |
| Panic w/ Agoraphobia | 1.1 | 0.06 | 487 | 28.5 | 0.70 | 0.7 | 0.08 | 132 | 26.0 | 1.39 | 1.5 | 0.09 | 355 | 29.6 | 0.75 |
| Panic | 4.4 | 0.13 | 1765 | 32.3 | 0.41 | 2.9 | 0.16 | 517 | 32.3 | 0.74 | 5.7 | 0.19 | 1248 | 32.3 | 0.49 |
| General Anxiety Disorder | 4.5 | 0.12 | 1878 | 33.3 | 0.43 | 3.1 | 0.16 | 552 | 32.8 | 0.74 | 5.8 | 0.19 | 1326 | 33.5 | 0.49 |
| Mood Disorders | |||||||||||||||
| Hypomania | 2.4 | 0.09 | 980 | 23.2 | 0.39 | 2.5 | 0.15 | 434 | 22.2 | 0.55 | 2.3 | 0.11 | 546 | 24.1 | 0.55 |
| Mania | 3.6 | 0.12 | 1480 | 25.4 | 0.39 | 3.5 | 0.17 | 608 | 23.5 | 0.57 | 3.7 | 0.15 | 872 | 27.0 | 0.51 |
| Major Depression | 18.2 | 0.23 | 7754 | 29.7 | 0.20 | 13.1 | 0.30 | 2400 | 29.7 | 0.37 | 22.9 | 0.33 | 5354 | 29.7 | 0.23 |
| Dysthymia | 4.9 | 0.13 | 2124 | 31.2 | 0.41 | 3.5 | 0.17 | 629 | 30.4 | 0.72 | 6.2 | 0.19 | 1495 | 31.6 | 0.49 |
The prevalence and mean age of onset is provided for all individuals with the specific disorder, regardless of the presence of comorbid disorders.
3.2. Temporal Sequencing of Lifetime AUDs and Other MADs among Comorbid Individuals
3.2.1. Alcohol Dependence
In general, the temporal sequencing of alcohol dependence relative to other MADs (Table 2) among comorbid individuals reflects the relative mean age of onset of these disorders observed in the general population. Alcohol dependence tended to precede (or to be temporally primary to) two of the MADs: panic and GAD. Alcohol dependence tended to follow two MADs: specific phobia and social phobia. For five MADs, the data showed an equal balance of cases where alcohol dependence was primary to the MAD or vice versa: panic with agoraphobia (though borderline significance is achieved in this case), dysthymia, major depression, hypomania, and mania. Note, that this does not mean that alcohol dependence and the MAD tended to be experienced concurrently. Concurrent appearance of both alcohol dependence and a MAD was relatively infrequent, ranging from 3–14%. All of these results showed the same pattern for both men and women.
Table 2.
Temporal Sequencing of Mood and Anxiety Disorders Relative to Alcohol Dependence among Lifetime Comorbid Individuals by Comorbid Mood and Anxiety Disorder, NESARC 2001–2002.
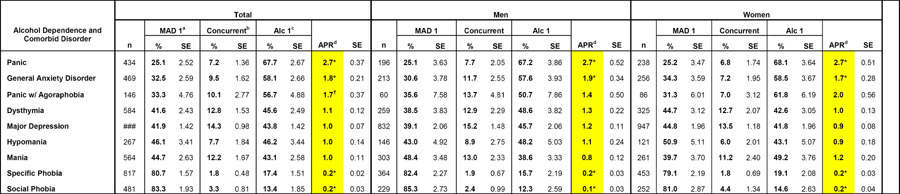 |
MAD Primary – the age of onset of the mood or anxiety disorder preceded the age of onset of the alcohol use disorder.
Concurrent – the mood or anxiety disorder and the alcohol use disorder both initially occurred at the same age.
Alcohol Disorder Primary – the age of onset of the alcohol use disorder preceded the age of onset of the mood or anxiety disorder.
Alcohol Primacy Ratio – calculated by dividing the proportion of primary alcohol use disorder by the proportion of primary mood or anxiety disorder.
APR significantly different than 1 (p<.05);
(p<.07). Significance was assessed using the Proc Ratio command of SUDAAN.
APRs for men are significantly different than APRs for women (p<.05).
Percentages may not sum to 100% due to rounding.
3.2.2. Alcohol Abuse
Results for alcohol abuse (Table 3) were somewhat more pronounced than those for alcohol dependence. In this case there were five (instead of two) disorders where abuse was primary to the MAD: GAD, panic, panic with agoraphobia, major depression, and dysthymia. MADs tended to be primary to alcohol abuse for two disorders: specific phobia and social phobia. For two disorders, the data showed an equal balance of cases where alcohol dependence was primary to the MAD or vice versa: hypomania and mania. Again results among men and women were similar, except that men were significantly more likely than women to have alcohol abuse occur before major depression and GAD.
Table 3.
Temporal Sequencing of Mood and Anxiety Disorders Relative to Alcohol Abuse among Lifetime Comorbid Individuals by Comorbid Mood and Anxiety Disorder, NESARC 2001–2002.
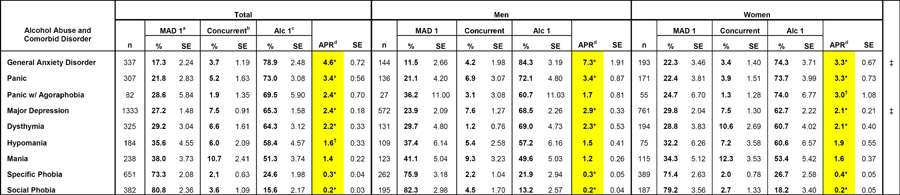 |
MAD Primary – the age of onset of the mood or anxiety disorder preceded the age of onset of the alcohol use disorder.
Concurrent – the mood or anxiety disorder and the alcohol use disorder both initially occurred at the same age.
Alcohol Disorder Primary – the age of onset of the alcohol use disorder preceded the age of onset of the mood or anxiety disorder.
Alcohol Primacy Ratio – calculated by dividing the proportion of primary alcohol use disorder by the proportion of primary mood or anxiety disorder.
APR significantly different than 1 (p<.05);
(p<.07). Significance was assessed using the Proc Ratio command of SUDAAN.
APRs for men are significantly different than APRs for women (p<.05).
Percentages may not sum to 100% due to rounding.
As shown in both Tables 2 and 3, even where the APR's were approximately equal to one, it does not mean that the timing of the alcohol use disorder and the MAD were concurrent. Thus, an examination of the lag time between the onset of one condition and the other can be revealing.
3.3. Lag Times between Onset of Lifetime AUDs and MADs
3.3.1. When the AUD is Primary
In general, the lag times between primary AUDs and subsequent MADs were quite long, even in cases where the APR approached unity (Table 4). The average lag time from alcohol dependence to MADs ranged from 7.6 years (hypomania) to 12.2 years (GAD), which was generally shorter than that from alcohol abuse to MAD, ranging from 8.9 years (hypomania) to 16.3 years (GAD). The shorter lag times were mostly due to the earlier onset of MADs among individuals with primary alcohol dependence than among those with primary alcohol abuse. When analyzed separately by sex, women, as compared to men, had significantly shorter lag times from alcohol abuse to panic, major depression, dysthymia, and GAD (all p’s<.05).
Table 4.
Mean Age of Onset and Lag Time among Comorbid Individuals where the Alcohol Use Disorder is Temporally Primary, NESARC 2001–2002.
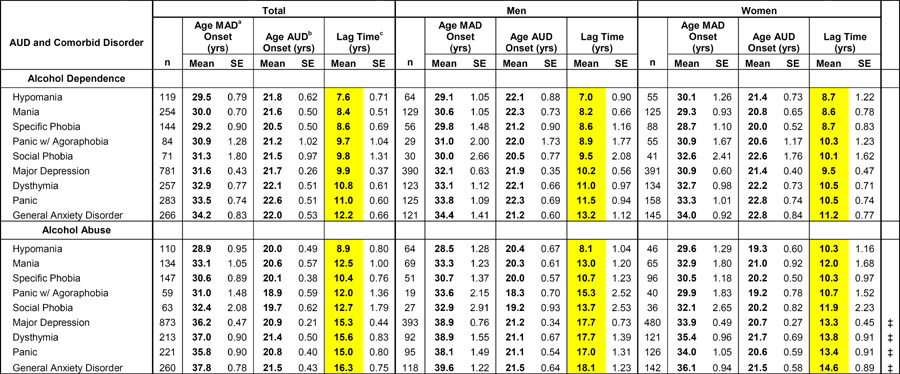 |
MAD – mood or anxiety disorder.
AUD – alcohol use disorder.
Lag Time – calculated by subtracting the age of onset of the earlier-occurring disorder from the age of onset of the later-occurring disorder.
All estimates are significantly different than zero (p<.05).
Mean lag times for men are significantly different than mean lag times for women (p<.05).
Due to rounding, the lag times may not exactly equal the age of onset of the mood or anxiety disorder minus the age of onset of the alcohol use disorder.
3.3.2. When the MAD is Primary
The lag times from the onset of MADs to subsequent alcohol dependence were generally similar to those of subsequent alcohol abuse. These ranged from 7.1 years (dysthymia) to 14.0 years (specific phobia) (Table 5). However, for panic with agoraphobia the lag time to alcohol dependence was significantly shorter than that to alcohol abuse. This was mostly due to the later onset of panic with agoraphobia among individuals with alcohol dependence as compared to individuals with alcohol abuse. Conversely, the lag time from social phobia to alcohol dependence was significantly longer than that to alcohol abuse. This was mostly due to the later onset of alcohol dependence than abuse among those with social phobia. Results were similar for men and women, except for alcohol abuse comorbid with panic and social phobia.
Table 5.
Mean Age of Onset and Lag Time among Comorbid Individuals where the Mood or Anxiety Disorder is Temporally Primary, NESARC 2001–2002.
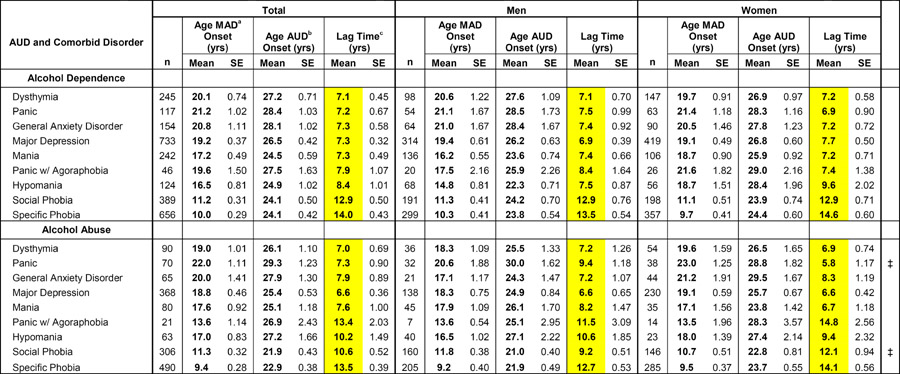 |
MAD – mood or anxiety disorder.
AUD – alcohol use disorder.
Lag Time – calculated by subtracting the age of onset of the earlier-occurring disorder from the age of onset of the later-occurring disorder.
All estimates are significantly different than zero (p<.05).
Mean lag times for men are significantly different than mean lag times for women (p<.05).
Due to rounding, the lag times may not exactly equal the age of onset of the mood or anxiety disorder minus the age of onset of the alcohol use disorder.
3.4. Temporal Sequencing Groups as Predictors of AUD Persistence
3.4.1. Alcohol Dependence
In general, individuals with a history of comorbid MADs were more likely to have persistent alcohol dependence than individuals with alcohol dependence only, as suggested by the large number of ORs greater than 1.0 for the two comorbid groups compared to the non-comorbid referent group in Table 6. However, this increased risk associated with comorbidity was only statistically significant when the following three MADs came before alcohol dependence: panic with agoraphobia, hypomania, and GAD. Noteworthy is the fact that compared with non-comorbid individuals (i.e., those with prior alcohol dependence only), no significant increase in the risk of persistent alcohol dependence was found among comorbid individuals with primary alcohol dependence. No gender differences were observed in these patterns.
Table 6.
Prior-to-Past-Year Comorbid Temporal Sequencing Groups as Predictors of the Past-Year Persistence of Alcohol Dependence and Abuse by Comorbid Mood or Anxiety Disorder, NESARC 2001–2002.
| Alcohol Dependence
|
Alcohol Abuse
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Mood or Anxiety Disorder Primary
|
Alcohol Dependence Primary
|
Mood or Anxiety Disorder Primary
|
Alcohol Abuse Primary
|
|||||
| Comorbid Disorder | ORa | 95% CIb | OR | 95% CI | OR | 95% CI | OR | 95% CI |
| Total | ||||||||
|
|
||||||||
| Panic w/ Agoraphobia | 3.39* | 1.06 – 10.81 | 1.52 | 0.63 – 3.70 | 0.40 | 0.07 – 2.27 | 1.85 | 0.84 – 4.06 |
| Hypomania | 2.14* | 1.28 – 3.60 | 1.08 | 0.49 – 2.34 | 0.71 | 0.33 – 1.54 | 0.73 | 0.38 – 1.39 |
| General Anxiety Disorder | 1.84* | 1.14 – 2.97 | 1.20 | 0.69 – 2.09 | 0.66 | 0.32 – 1.37 | 0.67 | 0.41 – 1.09 |
| Mania | 1.42 | 0.94 – 2.14 | 0.80 | 0.48 – 1.32 | 0.68 | 0.33 – 1.41 | 0.44* | 0.20 – 0.96 |
| Dysthymia | 1.35 | 0.91 – 2.01 | 1.19 | 0.73 – 1.92 | 0.22* | 0.09 – 0.55 | 0.46* | 0.23 – 0.93 |
| Major Depression | 1.19 | 0.92 – 1.54 | 1.03 | 0.77 – 1.39 | 0.71* | 0.51 – 0.99 | 0.80 | 0.60 – 1.05 |
| Panic | 1.18 | 0.67 – 2.08 | 1.08 | 0.66 – 1.77 | 0.36* | 0.15 – 0.87 | 0.51* | 0.29 – 0.90 |
| Social Phobia | 1.16 | 0.81 – 1.67 | 1.58 | 0.56 – 4.49 | 0.49* | 0.31 – 0.77 | 1.44 | 0.66 – 3.14 |
| Specific Phobia | 1.04 | 0.80 – 1.35 | 0.59 | 0.29 – 1.20 | 0.69* | 0.48 – 0.97 | 0.65 | 0.36 – 1.17 |
|
|
||||||||
| Men | ||||||||
|
|
||||||||
| Panic w/ Agoraphobia | 13.76* | 1.23 – 154.56 | 1.86 | 0.43 – 8.08 | – | – – – | 2.72 | 0.67 – 11.05 |
| Hypomania | 1.84 | 0.92 – 3.67 | 1.59 | 0.49 – 5.19 | 0.70 | 0.27 – 1.84 | 0.82 | 0.39 – 1.75 |
| General Anxiety Disorder | 1.65 | 0.78 – 3.49 | 1.34 | 0.66 – 2.73 | 1.14 | 0.44 – 2.98 | 0.74 | 0.37 – 1.52 |
| Mania | 1.44 | 0.83 – 2.50 | 0.84 | 0.43 – 1.64 | 0.75 | 0.30 – 1.90 | 0.36 | 0.12 – 1.10 |
| Dysthymia | 1.29 | 0.72 – 2.30 | 1.00 | 0.48 – 2.11 | 0.38 | 0.13 – 1.07 | 0.82 | 0.35 – 1.93 |
| Major Depression | 1.34 | 0.91 – 1.97 | 1.19 | 0.78 – 1.82 | 0.58* | 0.34 – 0.99 | 0.89 | 0.61 – 1.31 |
| Panic | 0.80 | 0.38 – 1.68 | 1.16 | 0.58 – 2.34 | 0.27* | 0.08 – 0.90 | 0.88 | 0.42 – 1.84 |
| Social Phobia | 1.09 | 0.67 – 1.80 | 2.52 | 0.63 – 10.11 | 0.54 | 0.29 – 1.01 | 1.33 | 0.40 – 4.39 |
| Specific Phobia | 1.16 | 0.79 – 1.68 | 1.24 | 0.44 – 3.49 | 0.80 | 0.49 – 1.31 | 0.84 | 0.35 – 1.97 |
|
|
||||||||
| Women | ||||||||
|
|
||||||||
| Panic w/ Agoraphobia | 1.93 | 0.56 – 6.59 | 1.58 | 0.60 – 4.16 | 0.85 | 0.14 – 5.20 | 2.07 | 0.75 – 5.73 |
| Hypomania | 2.96* | 1.32 – 6.65 | 0.57 | 0.17 – 1.87 | 0.66 | 0.19 – 2.24 | 0.52 | 0.16 – 1.69 |
| General Anxiety Disorder | 2.58* | 1.40 – 4.78 | 1.36 | 0.56 – 3.33 | 0.47 | 0.14 – 1.57 | 0.69 | 0.35 – 1.38 |
| Mania | 1.44 | 0.80 – 2.60 | 0.90 | 0.40 – 2.03 | 0.60 | 0.20 – 1.80 | 0.64 | 0.22 – 1.87 |
| Dysthymia | 1.87* | 1.07 – 3.27 | 1.85 | 0.97 – 3.54 | 0.08* | 0.01 – 0.44 | 0.19*‡ | 0.06 – 0.64 |
| Major Depression | 1.43 | 0.99 – 2.07 | 1.18 | 0.73 – 1.92 | 1.01 | 0.66 – 1.55 | 0.95 | 0.63 – 1.42 |
| Panic | 2.20 | 0.92 – 5.24 | 1.30 | 0.64 – 2.64 | 0.50 | 0.15 – 1.75 | 0.32* | 0.14 – 0.74 |
| Social Phobia | 1.47 | 0.85 – 2.56 | 1.22 | 0.18 – 8.35 | 0.50* | 0.26 – 0.96 | 1.99 | 0.72 – 5.49 |
| Specific Phobia | 1.18 | 0.79 – 1.78 | 0.35 | 0.11 – 1.12 | 0.71 | 0.44 – 1.15 | 0.70 | 0.32 – 1.57 |
OR – odds ratio.
CI – confidence interval.
OR significantly different than 1 (p<.05).
Significant sex differences in OR according to sex by temporal sequencing status interaction obtained in the pooled model (p<.05).
Note: All logistic regression models control for the number of years since the onset of the AUD. In each model, the reference group is non-comorbid individuals having only the AUD and not the mood or anxiety disorder. Results for the concurrent temporal sequencing group are not included because small sample sizes result in unreliable estimates.
Interpretation: “The odds of having persistent alcohol dependence in the past-year are 1.19 times greater among individuals with major depression onset prior to alcohol dependence onset (both disorders prior-to-past-year) than individuals with prior-to-past year alcohol dependence and no depression.”
3.4.2. Alcohol Abuse
In contrast to alcohol dependence, the majority of ORs for persistent alcohol abuse in the total sample were less than 1.0 (Table 6), suggesting that both comorbid groups (i.e., MAD primary and alcohol abuse primary) were less likely to have persistent alcohol abuse than the alcohol abuse only referent group. Few gender differences were observed, except that women with alcohol abuse primary to dysthymia were less likely than men to have persistent alcohol abuse.
4. CONCLUSION AND DISCUSSION
The ages of onset of the lifetime DSM-IV disorders presented in this study are in line with those found in previous major epidemiological studies, with phobias having the earliest onset, other anxiety disorders and mood disorders having the latest onset, and AUDs having an onset in between (Christie et al., 1988; Kessler et al., 2005). With age of onset generally occurring before age 35, psychiatric disorders have been called “chronic diseases of the young” (Insel and Fenton, 2005, p. 590). This is even more true in comparison to the onset of chronic physical disorders, which are most likely to occur in late middle-age or old age (Murray and Lopez, 1996).
One of the major findings of this study is that temporal sequencing patterns vary considerably across MADs, even within the same disorder class. For instance, among anxiety disorders, the phobias, at one extreme, are about 5 times more likely to occur before than after alcohol abuse, whereas at the other extreme, GAD is 4.6 times more likely to occur after than before alcohol abuse. These results argue against the practice of aggregating across MADs in temporal sequencing studies. Furthermore, the variation of these temporal sequencing patterns in the comorbid population is consistent with the pattern of age of onset of disorders in the general population — disorders with an earlier age of onset in the general population are more likely to be primary in comorbid individuals.
Although temporal primacy is a necessary (but not sufficient) condition to establish causality (Hill, 1965), the temporal sequencing results of the present study help elucidate the etiological underpinnings of comorbid disorders. The fact that AUDs are much more likely to precede than to follow 5 of the 9 MADs (panic, panic with agoraphobia, GAD, major depression, and dysthymia) is consistent with the notion that primary AUDs may cause (or exacerbate) these MADs. At the very least, it casts doubt on the likelihood that these MADs caused the AUD in the majority of cases. In the literature, several mechanisms have been offered as to how a primary AUD could potentially lead to the development of a subsequent MAD. For example: a) alcohol intoxication or withdrawal may cause acute, substance-induced psychological symptoms; b) long-term alcohol use may cause changes in brain physiology leading to the psychological sequelae; or c) alcohol intoxication may limit the repertoire of coping strategies to stressful situations, leading to feelings of helplessness, inadequacy, negative affect and anxiety (Baving and Olbrich, 1996; Lehman et al., 1989).
The present study found that only 2 of the 9 MADs assessed (specific phobia and social phobia) are usually primary to AUDs. The temporal primacy of the phobias is in accord with findings from the majority of the temporal sequencing studies (Cho et al., 2002; De Graaf et al., 2003; Hesselbrock et al., 1985; Kessler et al., 1997; Ross et al., 1988; Swendsen et al., 1998) and is expected due to the early onset of these disorders in childhood and early adolescence. The overwhelming proportion of phobias that are primary to AUDs makes it very unlikely that AUDs caused these MADs in most cases. On the contrary, if anything, the phobias may have had some influence in contributing to or causing the AUD. In this regard, self-medication hypotheses have been offered in the literature to explain the path by which psychological distress may lead to the onset of problem drinking (Baving and Olbrich, 1996; Lehman et al., 1989). It is plausible that a subset of the primary phobic individuals may have “self-medicated” with alcohol to reduce their fear-based symptoms, ultimately leading to the development of subsequent AUDs.
While the temporally sequencing analyses presented here are useful first step to examine causality, it should be duly noted that temporal primacy by itself is only suggestive of causality. Thus, while it is theoretically plausible, and perhaps tempting, to conclude that the primary disorder caused the secondary disorder, it is also possible that common underlying factors not assessed in this study (e.g., genetic, biologic or psychosocial factors) may have contributed to the development of independent, casually unrelated disorders (Lehman et al., 1989).
In addition to describing the age of onset of MADs in the general population, a major advance of this study was to also provide epidemiological data on the age of onset and lag times among the comorbid population. The present study shows that lag times between AUDs and MADs, regardless of which came first, were generally quite long (most ranging from 7 to 16 years). Thus, if the primary disorder does in fact play a causative or contributing role in the development of the secondary disorder, this role can best be described as “temporally distal.” Interestingly, lag times between primary alcohol dependence and subsequent MADs were shorter than lag times between primary alcohol abuse and subsequent MADs. Further examination revealed that this was mostly a result of the earlier onsets of the dependence-comorbid MADs as compared to abuse-comorbid MADs. If one assumes that dependence symptoms are more severe or dehabilitating than abuse symptoms, it would make sense that subsequent MADs occur sooner among dependent individuals, as compared to abuse individuals, since these dependent individuals may have an increased psychological vulnerability.
While sex differences are commonly noted in the general alcohol research literature, the present study found few significant differences in the temporal sequencing patterns and lag times between men and women. This result is most similar to De Graaf et al. (2003) who found no sex differences in temporal sequencing between AUDs and mood disorders. The few sex differences found in the present study showed that women were more likely than men to have primary major depression and GAD relative to alcohol abuse. These findings are similar to those of Kessler et al. (1997), who, using the 1990–92 National Comorbidity Study (NCS), reported that women generally had larger proportions of primary anxiety and affective disorders than men. However, for some disorders, the effects for each sex were in opposite directions. For example, men were more likely to have primary alcohol abuse than primary depression, whereas women were more likely to have primary depression than primary alcohol abuse. In contrast, the temporal sequencing patterns found in the present study were in the same direction for both sexes across all MADs. These discrepancies may be potentially due to methodological differences between the NCS and the NESARC. For example, the NESARC employed the DSM-IV AUD criteria, while the NCS used the DSM-III-R AUD criteria. In addition, changes over time may contribute to these discrepancies as the NCS was conducted 10 years prior to the NESARC. However, further research is necessary to fully understand the cause for the few discrepancies in gender patterns between the two studies. Similar to that in the temporal sequencing patterns, the current study found that gender differences among lag times were more the exception than the norm. The few differences ranged from 3 to 4 years and were most apparent when alcohol abuse was primary to the MADs.
While previous studies only examined the risk of persistent AUDs among comorbid individuals whose MAD is primary to the AUD (Kessler et al., 1996; Kessler et al., 1997; Ross, 1995), the current study contributes to the literature by also examining the risk for those comorbid individuals whose MAD is secondary to the AUD. The main finding was that, contrary to expectations, the risk of persistent AUDs is not always higher among comorbid individuals than individuals with prior AUDs only. Rather, the risk of persistent AUDs depends on several factors, including the type of comorbid MAD, which comorbid disorder came first, and whether the outcome is the persistence of alcohol dependence or alcohol abuse. For instance, as expected, across most temporal sequencing groups and MADs, having a prior comorbid MAD tended to increase the risk for continued alcohol dependence. However, contrary to expectations, having a prior comorbid MAD tended to decrease the risk for continued alcohol abuse. Although this pattern of results has been found in some previous studies (Kessler et al., 1997; Ross, 1995), it is unclear why MAD comorbidity should lessen the risk of persistent alcohol abuse. A possible explanation is that people with comorbid alcohol abuse are more likely than those with alcohol abuse only to a) directly seek alcohol treatment for their alcohol abuse, and/or b) seek psychological treatment services for the comorbid MAD, and in doing so the alcohol abuse gets treated as well. We conducted a follow-up analysis using the NESARC data and confirmed that people with lifetime alcohol abuse comorbid with major depression, mania, and dysthymia were indeed significantly more likely than people with only alcohol abuse to seek alcohol treatment. However, Falk and Yi (2006) found that the higher rates of alcohol treatment seeking among comorbid people also apply to those with alcohol dependence. Thus, the increased use of alcohol treatment services among alcohol abuse comorbid people does not in and of itself clarify the opposite effects of comorbidity found in the present study.
For persistent alcohol dependence, several primary MADs (i.e., GAD, hypomania, and panic with agoraphobia) were found to be significant risk factors, while primary alcohol dependence disorder was not a significant risk factor. These significant associations were novel findings. Moreover, some of the non-significant associations in the present study (e.g., for primary social phobia, specific phobia, and mania), were in fact significant in the literature (Kessler et al., 1997; Ross, 1995). These differences may be partly due to methodological differences. For instance, the analyses in present study controlled for several important covariates (i.e., age of AUD onset, and the number of years between AUD onset and time of interview) while the other studies reported only simple, bivariate associations.
One limitation of the present study is that it relies on retrospective self-reports to determine the age of onset for the lifetime disorders. Longitudinal investigations, using community samples, have noted that individuals have problematic rates of forgetting previously reported disorders (Wilhelm and Parker, 1994). Moreover, retrospective reports on age of onset are subject to recall bias, especially among older respondents (Labouvie et al., 1997; Prusoff et al., 1988). Nonetheless, two recent long-term prospective studies have found at least moderate test-retest reliability for age of onset questions (Johnson and Mott, 2001; Parra et al., 2003). Until further confirmed by additional prospective research, results based on lifetime retrospective reports should be interpreted with caution.
The high rates of co-occurrence of alcohol disorders and other MADs in the general population have led a number of researchers to recommend that clinicians routinely assess for the presence of comorbid conditions to inform appropriate AUD treatment options (Grant et al., 2004; Hunter et al., 2000; Kessler et al., 1996). While this is generally a sensible idea, the results of the present study suggest that not all comorbid MADs lead to an equally poor prognosis, and moreover, this prognosis is related to the temporal order by which the conditions first appeared. Further research is needed to confirm our findings. However, if these results can be replicated by other studies, then we might qualify the previous recommendation and suggest that clinicians, particularly those treating individuals with alcohol dependence, not only assess for the presence of comorbid MADs (i.e., GAD, hypomania, and panic with agoraphobia), but also take detailed psychiatric histories to determine whether these MADs preceded the alcohol dependence and are thus predictors of poor prognosis.
Supplementary Material
Footnotes
Additional information related to the methods for this study can be viewed by accessing the online version of this paper at http://dx.doi.org by entering doi:xxxxxxxx.
For brevity, panic without agoraphobia will be referred to as “panic” in the remainder of the paper.
NESARC age of onset questions for DSM-IV disorders used for these analyses can be viewed by accessing the online version of this paper at http://dx.doi.org be entering doi:xxxxxxxx.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Bakken K, Landheim AS, Vaglum P. Primary and secondary substance misusers: Do they differ in substance-induced and substance-independent mental disorders? Alcohol Alcohol. 2003;38:54–59. doi: 10.1093/alcalc/agg012. [DOI] [PubMed] [Google Scholar]
- Baving L, Olbrich H. Alcoholism and depression. European Addiction Research. 1996;2:29–35. [Google Scholar]
- Burke KC, Burke JD, Regier DA, Rae DS. Age at onset of selected mental disorders in five community populations. Arch Gen Psychiatry. 1990;47:511–518. doi: 10.1001/archpsyc.1990.01810180011002. [DOI] [PubMed] [Google Scholar]
- Burns L, Teesson M. Alcohol use disorders comorbid with anxiety, depression and drug use disorders: Findings from the Australian National Survey of Mental Health and Well Being. Drug Alcohol Depend. 2002;68:299–307. doi: 10.1016/s0376-8716(02)00220-x. [DOI] [PubMed] [Google Scholar]
- Cho MJ, Bong-Jin H, Suh T, Guk-Hee S, Seong-Jin C, Lee CK. Comorbid mental disorders among patients with alcohol abuse and dependence in Korea. J Korean Med Sci. 2002;17:236–241. doi: 10.3346/jkms.2002.17.2.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christie KA, Burke J, Regier DA, Rae DS, Boyd JH, Locke BZ. Epidemiologic evidence for early onset of mental disorders and higher risk of drug abuse in young adults. Am J Psychiatry. 1988;145:971–975. doi: 10.1176/ajp.145.8.971. [DOI] [PubMed] [Google Scholar]
- Compton WM, Cottler LB, Phelps DL, Ben Abdallah A, Sptiznagel EL. Psychiatric disorders among drug dependent subjects: Are they primary or secondary? Am J Addictions. 2000;9:126–134. doi: 10.1080/10550490050173190. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou PS. Psychopathology associated with alcohol use disorders in the college and general adult populations. Drug Alcohol Depend. 2005a;77:139–150. doi: 10.1016/j.drugalcdep.2004.07.012. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou PS, Huang B, Ruan WJ. Recovery from DSM-IV alcohol dependence: United States, 2001–2002. Addiction. 2005b;100:281–292. doi: 10.1111/j.1360-0443.2004.00964.x. [DOI] [PubMed] [Google Scholar]
- De Graaf R, Bijl RV, Spijker J, Beekman AF, Vollebergh WM. Temporal sequencing of lifetime mood disorders in relation to comorbid anxiety and substance use disorders: Finding from the Netherlands Mental Health Survey and Incidence Study. Soc Psychiatry Psychiatr Epidemiol. 2003;38:1–11. doi: 10.1007/s00127-003-0597-4. [DOI] [PubMed] [Google Scholar]
- Falk D, Yi H. Treatment seeking by comorbid individuals with DSM-IV alcohol dependence and mood and anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). Poster presented at the 29th Annual Scientific Meeting of the Research Society on Alcoholism; Baltimore, Maryland. June 23–28.2006. [Google Scholar]
- Goldstein BI, Levitt AJ. Factors associated with temporal priority in comorbid bipolar I disorder and alcohol use disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2006;67:643–649. doi: 10.4088/jcp.v67n0416. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Hasin DS. The Alcohol Use Disorder and Associated disabilities Interview Schedule – DSM-IV Version. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2001. [Google Scholar]
- Grant BF, Hasin DS, Dawson DA. The relationship between DSM-IV AUDs and DSM-IV major depression: Examination of the primary-secondary distinction in a general population sample. J Affect Disord. 1996;38:113–128. doi: 10.1016/0165-0327(96)00002-x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Kaplan K, Shepard J, Moore T. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2003. [accessed on August 27, 2007]. Source and Accuracy Statement for Wave 1 of the 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions. http://niaaa.census.gov/pdfs/source_and_accuracy_statement.pdf. [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Pickering RP, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood disorders and anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Hanna EZ, Grant BF. Gender differences in DSM-IV AUDs and major depression as distributed in the general population: Clinical implications. Compr Psychiatry. 1997;38:202–212. doi: 10.1016/s0010-440x(97)90028-6. [DOI] [PubMed] [Google Scholar]
- Harford TC, Grant BF. Prevalence and population validity of DSM III-R alcohol abuse and dependence: the 1989 National Longitudinal Survey on Youth. J Subst Abuse. 1994;6:37–44. doi: 10.1016/s0899-3289(94)90065-5. [DOI] [PubMed] [Google Scholar]
- Hasegawa K, Mukasa H, Nakazawa Y, Kodama H, Nakamura K. Primary and secondary depression in alcoholism – clinical features and family history. Drug Alcohol Depend. 1991;27:275–281. doi: 10.1016/0376-8716(91)90010-v. [DOI] [PubMed] [Google Scholar]
- Hasin D, Grant BF, Cottler L, Blaine J, Towle L, Ustun B, Sartorius N. Nosological comparisons of alcohol and drug diagnoses: a multisite, multi-instrument international study. Drug Alcohol Depend. 1997a;47:217–226. doi: 10.1016/s0376-8716(97)00092-6. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Van Rossem R, McCloud S, Endicott J. Alcohol dependence and abuse diagnoses: validity in a community sample of heavy drinkers. Alcohol Clin Exp Res. 1997b;21:213–219. [PubMed] [Google Scholar]
- Hasin DS, Paykin A. Alcohol dependence and abuse diagnoses: concurrent validity in a nationally representative sample. Alcohol Clin Exp Res. 1999;23:144–150. [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64:830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- Hesselbrock MN, Meyer RE, Keener JJ. Psychopathology in hospitalized alcoholics. Arch Gen Psychiatry. 1985;42:1050–1055. doi: 10.1001/archpsyc.1985.01790340028004. [DOI] [PubMed] [Google Scholar]
- Hill AB. The environment and disease: association or causation? Proc R Soc Med. 1965;58:295–300. [PMC free article] [PubMed] [Google Scholar]
- Hunter EE, Powell BJ, Penick EC, Nickel EJ, Liskow BI, Cantrell PJ, Landon JF. Comorbid psychiatric diagnosis and long-term drinking outcome. Compr Psychiatry. 2000;41:334–338. doi: 10.1053/comp.2000.8997. [DOI] [PubMed] [Google Scholar]
- Insel TR, Fenton WS. Psychiatric epidemiology: it’s not just about counting anymore. Arch Gen Psychiatry. 2005;62:590–592. doi: 10.1001/archpsyc.62.6.590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson TP, Mott JA. The reliability of self-reported age of onset of tobacco, alcohol and illicit drug use. Addiction. 2001;96:1187–1198. doi: 10.1046/j.1360-0443.2001.968118711.x. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Crum RM, Warner LA, Nelson CB, Schulenberg J, Anthony JC. Lifetime co-occurrence of DSM-IIIR alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Arch Gen Psychiatry. 1997;154:313–321. doi: 10.1001/archpsyc.1997.01830160031005. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Nelson CB, McGonagle KA, Edlund MJ, Frank RG, Leaf PJ. The epidemiology of co-occurring addictive and mental disorders: Implications for prevention and service utilization. Am J Orthopsychiatry. 1996;66:19–31. doi: 10.1037/h0080151. [DOI] [PubMed] [Google Scholar]
- Labouvie E, Bates ME, Pandina RJ. Age of first use: Its reliability and predictive utility. J Stud Alcohol. 1997;58:638–643. doi: 10.15288/jsa.1997.58.638. [DOI] [PubMed] [Google Scholar]
- Lehman A, Myers C, Corty E. Assessment and classification of patients with psychiatric and substance abuse symptoms. Hosp Community Psychiatry. 1989;40:1019–1025. doi: 10.1176/ps.40.10.1019. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Mehta RL, Molnar BE, Walters EE, Swendsen JD, Aguilar-Gaziola S, Bijl R, Borges G, Caraveo-Anduaga JJ, Dewit DJ, Kolody B, Vega WA, Wittchen HU, Kessler RC. Comorbidity of substance use disorders with mood and anxiety disorders: Results of the International Consortium in Psychiatric Epidemiology. Addict Behav. 1998;23:893–907. doi: 10.1016/s0306-4603(98)00076-8. [DOI] [PubMed] [Google Scholar]
- Murray CJ, Lopez AD. Global Health Statistics. Cambridge, Mass: Harvard University Press; 1996. [Google Scholar]
- Nelson CB, Rehm J, Usten B, Grant BF, Chatterji S. Factor structure for DSM-IV substance disorder criteria endorsed by alcohol, cannabis, cocaine and opiate users: Results from the World Health Organization Reliability and Validity Study. Addiction. 1999;94:843–855. doi: 10.1046/j.1360-0443.1999.9468438.x. [DOI] [PubMed] [Google Scholar]
- Parra GR, O’Neill SE, Sher KJ. Reliability of self-reported age of substance involvement onset. Psychol Addict Behav. 2003;17:211–218. doi: 10.1037/0893-164X.17.3.211. [DOI] [PubMed] [Google Scholar]
- Powell BJ, Read MR, Penick EC, Miller NS, Bingham SF. Primary and secondary depression in alcoholic men: An important distinction? J Clin Psychiatry. 1987;48:98–101. [PubMed] [Google Scholar]
- Prusoff BA, Merikangas KR, Weissman MM. Lifetime prevalence and age of onset of psychiatric disorders: Recall 4 years later. J Psychiatr Res. 1988;22:107–117. doi: 10.1016/0022-3956(88)90075-1. [DOI] [PubMed] [Google Scholar]
- Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, Goodwin FK. Comorbidity of mental disorders with alcohol and other drug abuse: Results from the Epidemiologic Catchment Area (ECA) Study. JAMA. 1990;264:2511–2518. [PubMed] [Google Scholar]
- Research Triangle Institute. Software for Survey Data Analysis (SUDAAN), Version 9.0. Research Triangle Park, NC: Research Triangle Institute; 2005. [Google Scholar]
- Ross HE. DSM-III-R alcohol abuse and dependence and psychiatric comorbidity in Ontario: Results from the Mental Health Supplement to the Ontario Health Survey. Drug Alcohol Depend. 1995;39:111–128. doi: 10.1016/0376-8716(95)01150-w. [DOI] [PubMed] [Google Scholar]
- Ross HE, Glaser FB, Germanson T. The prevalence of psychiatric disorders in patients with alcohol and other drug problems. Arch Gen Psychiatry. 1988;45:1023–1031. doi: 10.1001/archpsyc.1988.01800350057008. [DOI] [PubMed] [Google Scholar]
- Swendsen JD, Merikangas KR, Canino GJ, Kessler RC, Rubio-Stipec M, Angst J. The comorbidity of alcoholism with anxiety and depressive disorders in four geographic communities. Compr Psychiatry. 1998;39:176–184. doi: 10.1016/s0010-440x(98)90058-x. [DOI] [PubMed] [Google Scholar]
- Swendsen JD, Merikangas KR. The comorbidity of depression and substance use disorders. Clin Psychol Rev. 2000;20:173–189. doi: 10.1016/s0272-7358(99)00026-4. [DOI] [PubMed] [Google Scholar]
- Ustun B, Compton W, Mager D, Babor T, Baiyewu O, Chatterji S, Cottler L, Gogus A, Mavreas V, Peters L, Pull C, Saunders J, Smeets R, Stipec MR, Vrasti R, Hasin D, Room R, Van den Brink W, Regier D, Blaine J, Grant BF, Sartorius N. WHO Study on the reliability and validity of the alcohol and drug use disorder instruments: Overview of methods and results. Drug Alcohol Depend. 1997;47:161–169. doi: 10.1016/s0376-8716(97)00087-2. [DOI] [PubMed] [Google Scholar]
- Ware JE, Kosinski M, Turnder Bowker DM, Gandek B. How to Score Version 2 of the SF-12 Health Survey. Lincoln, RI: Quality Metrics; 2002. [Google Scholar]
- Wilhelm K, Parker G. Sex differences in lifetime depression rates: Fact or artifact? Psychol Med. 1994;24:97–111. doi: 10.1017/s0033291700026878. [DOI] [PubMed] [Google Scholar]
- Zilberman ML, Tavares H, Blume SB, El-Guebaly N. Substance use disorders: sex differences and psychiatric comorbidities. Can J Psychiatry. 2003;48:5–13. doi: 10.1177/070674370304800103. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


