Abstract
High expressed emotion (EE) attitudes among parents are associated with an increased likelihood of relapse among bipolar patients, but the origins of these attitudes are unclear. This study examined characteristics of bipolar disorder in adolescents that might be associated with high EE attitudes among parents. We hypothesized that an earlier onset of mood disorder and greater current illness severity would predict higher levels of criticism and emotional overinvolvement among parents. Demographic, diagnostic, and EE data were collected from interviews with parents of 44 bipolar adolescents (mean age 14.5 yrs.). Current illness severity and functioning were not associated with high-EE attitudes. Parents of girls, however, were more likely to be high in criticism than parents of boys. Parents of girls expressed more critical comments when the child had an adolescent compared to a childhood onset of bipolar disorder, whereas the reverse pattern was evident among parents of boys. We encourage prospective investigations of the developmental correlates of parental EE attitudes in larger, more heterogeneous samples of bipolar adolescents and children.
Keywords: Expressed Emotion, Age at Onset, Bipolar Disorder, Gender, Developmental Psychopathology
Early-onset bipolar disorder is characterized by severe and maladaptive shifts in mood, energy level, and behavior (Lewinsohn, Klein, and Seeley, 2000; Wilkinson, Taylor, & Holt, 2002). Symptoms of irritability, especially if phasic or episodic, are believed to be behavioral precursors of more classic bipolar symptoms in later childhood or adulthood (Fergus et al., 2003; Leibenluft, Cohen, Gorrindo, Brook, & Pine, 2006). Between 50% and 67% of bipolar patients experience illness onset before the age of 18, and 13% – 28% before age 13 (Perlis et al., 2004).
Factors that influence the onset of bipolar disorder may differ from factors that influence the course of the illness once diagnosed. Although heritability plays a central role in the etiology of the disease (Faraone, Glatt, & Tsuang, 2003), the family environment accompanying illness episodes may influence the frequency and timing of relapses. Bipolar adults who live with highly critical, hostile, or emotionally overinvolved (high expressed emotion, or high-EE) parents are significantly more likely to experience a relapse within one year after an acute episode than adult patients whose parents are low in EE (Miklowitz, Goldstein, Nuechterlein, Snyder, and Mintz, 1988; Yan, Hammen, Cohen, Daley, & Henry, 2004).
Pediatric bipolar patients are usually under the direct care of their parents, and appear to be highly susceptible to variations in the emotional climate of the family (Jarbin, Grawe, & Hansson, 2000; Kim, Miklowitz, Biuckians, & Mullen, 2007; Fristad & Goldberg, 2003). However, few studies have examined the role of EE or other family environmental factors in the course of childhood bipolar disorder. Among patients with prepubertal or early adolescent bipolar disorder, Craney and Geller (2003) found that children whose mothers were rated low in warmth were 4.1 times more likely to experience a recurrence in the 4 years after recovery than children whose mothers were high in warmth. In bipolar teens receiving pharmacotherapy and family-focused treatment, Miklowitz, Biuckians, and Richards (2006) found that those teens with at least one high-EE parent had higher depressive and manic symptom ratings over 2 years than teens whose parents were low in EE.
Despite the consistent prospective association between EE and patients’ courses of illness, there has been relatively little success in identifying variables that are cross-sectionally correlated with EE attitudes among the caregivers of adults or youth (Hooley, 1998). Isolated accounts of correlations between familial EE and various characteristics of adult patients have appeared in the literature, but no consistent findings have emerged to explain why some relatives are highly critical, hostile, or overprotective during or following illness episodes and some are not. Some studies have found that patients in high- and low-EE families differ in the concurrent severity of symptoms and level of functional impairment at the time of the EE assessment. Nonetheless, these patient variables do not account for the prospective association between EE and relapse (e.g., Vaughn & Leff, 1976; Nuechterlein, Snyder, & Mintz, 1992; Hooley & Gotlib, 2000).
One illness characteristic that may help explain the association between EE and relapse in bipolar disorder is the age of onset of the illness and its corresponding duration. Possibly, parents of young-onset patients become increasingly critical as the illness unfolds over the course of development. The duration of illness has been found to be positively correlated with the number of critical comments expressed by relatives in schizophrenia studies, suggesting that levels of EE may increase as the illness becomes more chronic and recurrent (MacMillan, Gold, Crow, Johnson, & Johnstone, 1986; Hooley & Richters, 1995). McFarlane and Cook (2007) found that mothers of offspring with established schizophrenic or mood disorder diagnoses had higher levels of rejection, protectiveness, and fusion, and lower levels of warmth than mothers of offspring who were in the prodromal phases of their psychiatric disorders. Moreover, levels of maternal EE increased with longer prodromes of the patients’ illnesses.
This study examined the relationships between current and historical illness characteristics and parental EE among bipolar teens. Using data collected from 44 bipolar adolescents prior to their enrollment in a family treatment study, we examined age of illness onset, lifetime duration of illness, severity of current symptoms, and degree of impairment as predictors of EE in parents. We hypothesized that an earlier onset of bipolar disorder and a longer illness duration would be associated with higher levels of parental EE – notably critical comments – at the time of onset of an episode of mood disorder. Furthermore, we hypothesized that adolescents with more severe current symptoms and functional impairment would have parents with correspondingly higher levels of EE criticism or overinvolvement. Finally, given that boys and girls can have very different courses of mood disorder depending on their ages at onset (e.g., Hankin et al., 1998), we explored whether these hypothesized relationships were moderated by the gender of the child.
Method
Participants
Adolescents were recruited for an open trial (n = 20) or a randomized trial of family-focused treatment and pharmacotherapy (n = 35) for bipolar disorder conducted by the University of Colorado (Miklowitz et al., 2004, 2006). They were recruited from outpatient clinics, private clinicians, hospitals, and support groups. Entry to the study required that adolescents experience a manic, depressed, or mixed episode in the 3 months prior to the initiation of psychosocial treatments. Data for the present study were based only on pretreatment assessments; for more detail concerning the design of these trials, see Miklowitz et al. (2006).
This study included 44 (21 male and 23 female; mean age 14.50 years, SD= 1.53, range 13–17) of the 55 adolescents who participated in the larger trials. There were 6 participants from whom parental EE data were unavailable; 5 other participants were recruited for the treatment trials after the presented study had been completed. There were a total of 71 parents of these 44 adolescents (40 mothers or stepmothers and 31 fathers or stepfathers); of these, 11 were single parent family units and 33 were dual-parent family units.
This study was approved by the University of Colorado’s Human Research Committee. All adolescents and parents signed an approved informed consent or assent form following an explanation of the study’s procedures.
Procedure
The hypothesized predictors of parental EE in this study were age at illness onset and symptom severity and functional impairment in the 3 months prior to entry into the treatment trials. The sources of these data were two audiotaped interviews with parents conducted at study entry: the Camberwell Family Interview (CFI; Vaughn & Leff, 1976) and the Kiddie Schedule for Affective Disorders and Schizophrenia, Present and Lifetime Version (KSADS-PL; Chambers et al., 1985; Kaufman et al., 1997).
Measures
Camberwell Family Interview (CFI) for rating EE
Each parent was interviewed for approximately 1 – 1 and 1/2 hrs by a staff research assistant at the time of consent for the treatment trials. The standard version of the CFI (Vaughn & Leff, 1976) assesses the relative’s reactions to the development of the patient’s most recent episode of mood disorder, with particular emphasis on the 3 months prior to interview. Trained raters evaluated tapes of these interviews on three primary dimensions: critical comments (e.g., “When I talk to him, I get upset that he just shuts down. It’s like there’s no one there!”), hostility, (personal, generalized criticism of the patient; e.g., “I like nothing about him”), and emotional overinvolvement (EOI), or the tendency to be overconcerned, overprotective, or to use inordinately self-sacrificing behaviors in the patient’s care (e.g., “I don’t invite people to the house ’cause Allen [son] doesn’t like it”).
Family members who expressed 6 or more critical comments, showed evidence of hostility, or who obtained a score of 4 (high) or 5 (extremely high) on a 0–5 scale of overinvolvement were classified as high-EE; those who did not meet these criteria were considered low-EE. Of the 71 parents whose CFI data were available, 37 were rated high EE and 34 were rated low EE. Of the 44 families, 27 were classified as high EE and 17 as low EE. Following the standard rating conventions for the CFI (Vaughn & Leff, 1976), families were classified as high-EE if at least one parent was so designated. Thus, a high-EE family could have had only one single high-EE parent (n = 6), one high-EE and one low-EE parent (n = 9) or two high-EE parents (n = 9). If the single parent was rated low-EE (n = 4) or both parents in a dual-parent family were rated low-EE (n = 8), the family was classified as low-EE. EE data were unavailable on the second parent in 8 dual-parent families; these families were classified as high-EE (n = 3) or low-EE (n = 5) based on the rating of the one available parent. In most cases, the second parent was living separately from the family and had little interaction with the adolescent. The primary CFI rater had previously established interrater reliability with a second rater on number of critical comments ([intraclass r = .82, 10 independent ratings), hostility (r = .93), and emotional overinvolvement (intraclass r = .80; for all, p < .001).
Diagnosis and symptomatology: KSADS-PL
The KSADS-PL is a well-established semistructured diagnostic interview conducted with the child and at least one parent. The use of the KSADS-PL as a diagnostic instrument in the larger treatment trials has been described elsewhere (Miklowitz et al., 2006). Briefly, parents and adolescents were separately interviewed and consensus scores were tabulated for each psychiatric symptom item. Subjects were asked about the presence and severity of each symptom in the prior three months, as well as in the adolescent’s lifetime. Then, diagnoses were generated for the primary disorder and any comorbid disorders.
For the present study, independent raters listened to audiotapes of the parents’ KSADS-PL and CFI assessments a second time to gather as much information as possible about (1) the degree to which the child had shown five specific mood and psychosis symptoms (depression, euphoria, irritability, anxiety, and psychosis) over the prior 3 months, 2) his or her level of functioning in four areas (school/work, home, community, and behavior toward others), as rated on the Child and Adolescent Functional Assessment Scale (CAFAS; Hodges & Wong, 1996); and 3) the extent of his or her difficulties with sleep, attention, and energy dysregulation. All symptom and functioning variables were rated concerning the prior 3 months. A subset of six cases was coded on each of these 12 variables by two independent raters. Interrater reliabilities, determined based on absolute agreement, are presented in Table 1.
Table 1.
Interrater Agreement on Functioning and Symptom Variables
| Variable | Percentage agreement (N = 6) |
|---|---|
| Functioning | |
| Academic | 66.7% |
| Peers | 100.0% |
| Home | 100.0% |
| Community | 83.3% |
| Symptoms | |
| Depression | 100.0% |
| Euphoria | 66.7% |
| Irritability | 83.3% |
| Anxiety | 100.0% |
| Psychosis | 100.0% |
| Sleep | 50.0% |
| Energy | 66.7% |
| Attention | 100% |
Note: Percentage agreements were calculated based on absolute agreements between two independent raters.
The five symptom variables were rated using the K-SADS Depression and Mania Rating Scale (1 to 6) system (Kaufman et al., 1997; Axelson et al., 2003). These Likert-type items capture the frequency, duration, and severity of each symptom. Additional information from the CFI was used to cross-validate these ratings. For example, to assess euphoria, references to giddy mood, feeling on top of the world, and seeming “too happy,” in either the CFI or in direct response to structured K-SADS inquiries were noted. Information about sleep, attention, and energy dysregulation gathered from the two interviews was used to rate the child on an improvised 4-point scale with the following anchors: 1) no problems over the prior 3 months; 2) problems at times; 3) symptom is present more often than not, but at a mild level; 4) symptom is present continuously at the moderate to severe level. Children could be rated as having energy dysregulation if they showed distinct periods of having too little or too much energy.
CAFAS Psychosocial Functioning
Raters used the information gathered from the CFI and K-SADS to make CAFAS ratings of the child’s functioning over the prior 3 months. The following areas were rated: academic performance, relationships with peers, functioning within the home, and functioning in the community. The CAFAS assesses a child’s degree of impairment in day-to-day functioning due to emotional, behavioral, psychological, psychiatric, or substance use problems. A rater chooses from a list of behavioral descriptions, thus generating scores on subscales such as school, home, and community functioning. The CAFAS has been shown to be reliable and valid, with total CAFAS score interrater reliabilities ranging from .92 to .96 (Hodges and Wong, 1996; Hodges, 2004). In the present study, interrater reliability for CAFAS items ranged from 66.7% to 100% (Table 1), based on absolute agreement.
Age at onset of bipolar disorder
Illness onset information was retrieved from the CFI and KSADS-PL interviews, as well as from all treatment history data gathered in the context of the treatment trials. Age at onset of bipolar disorder was defined as the estimated age at first bipolar diagnosis by a mental health professional. When diagnostic information was unavailable, we tabulated the age at first onset of significant mood symptoms that would have met DSM-IV criteria (American Psychiatric Association, 2000) for a manic, hypomanic, or mixed episode. Earlier examination of the data suggested different developmental patterns of symptoms and functioning for children diagnosed before and after puberty, so we maintained this distinction by treating age at illness onset as a categorical variable (childhood versus adolescence).
Parents often dated illness onset to the immediate post-pubescent period rather than to a particular age. Because no formal assessment of puberty was undertaken, these youths were simply classified as having adolescent onset. Reliability between two independent raters for the categorical age at onset distinction was 84% (Kappa = .69, p < .005) in a subsample of 19 cases.
We also tabulated the age at first treatment, defined as the first mental health contact for any significant psychiatric symptom (including attentional problems) which resulted in a treatment recommendation, whether or not this recommendation was consistent with a bipolar diagnosis. Interrater reliability on this dimensional variable was .86 (intraclass correlation coefficient, p < .0001, n = 19). The lifetime duration of symptoms was calculated as the difference between the current age and the age at first treatment.
Results
Hypotheses
We hypothesized that children with an earlier onset of bipolar disorder and longer lifetime durations of illness would be more likely to have high-EE parents than children with a later onset. We also predicted that adolescents with more severe recent symptoms and functional impairment would have parents with higher criticism or emotional overinvolvement scores. Gender was examined as a moderator of these associations.
Preliminary Analyses of Demographic data
Table 2 presents demographic and clinical characteristics of the sample as a function of patient gender, including age, age of first psychiatric treatment, age at onset of the mood disorder (childhood versus adolescence), lifetime duration of mood disorder, bipolar subtype (I, II, or not otherwise specified), comorbid diagnoses, and other variables.
Table 2.
Demographic and Clinical Characteristics of Sample (N = 44)
| Variable | Boys | Girls | Total/Grand Mean |
|---|---|---|---|
| (N = 21) | (N = 23) | (N = 44) | |
| Age at entry to study: M (SD) | 14.05 (1.43) | 14.91 (1.53) | 14.50 (1.53) |
| Age at first treatment: M (SD) | 6.58 (3.75) | 9.95 (3.15)** | 8.30 (3.82) |
| Bipolar diagnosis: No. (%) | |||
| Bipolar I | 15 (71.4) | 18 (78.3) | 33 (66.0) |
| Bipolar II | 1 (4.8) | 3 (13.0) | 4 (8.0) |
| Bipolar NOS | 5 (23.8) | 2 (8.7) | 7 (14.0) |
| Presence of comorbid ADHD: No. (%) | 15 (71.4) | 9 (39.1)* | 24 (54.5) |
| Presence of comorbid ADHD, ODD, and CD: No. (%) | 20 (95.2) | 22 (95.7) | 2.59 (1.32) |
| Lifetime duration of illness, yrs., M (SD) | 7.48 (3.35) | 5.14 (2.59)* | 6.28 (3.18) |
| Intact family: No. (%) | 15 (71.4) | 18 (78.3) | 33 (66.0) |
| Prior Hospitalization, No. (%) | 7 (33.0) | 11 (47.8) | 18 (40.9) |
| Taking medication: No. (%) | 19 (90.5) | 20 (87.0) | 39 (78.0) |
| Onset: No. (%) | |||
| Childhood | 15 (71.4) | 6 (26.1)** | 21 (42.0) |
| Adolescence | 5 (23.8) | 17 (73.9)** | 22 (44.0) |
| EE: No. (%) | |||
| Low | 10 (47.6) | 7 (30.4) | 17 (38.6) |
| High, overall | 11 (52.4) | 16 (69.6) | 27 (61.4) |
| High, Critical | 3 (14.3) | 14 (60.9)** | 17 (38.6) |
| High, EOI | 10 (47.6) | 9 (38.1) | 19 (38.0) |
| Total critical comments: M (SD) | 3.29 (2.65) | 6.17 (3.69)** | 4.80 (3.52) |
| Total EOI score: M (SD) | 2.67 (1.11) | 2.22 (1.04) | 2.43 (1.09) |
| Functioning: M (SD)1 | |||
| Academics | 2.75 (.64) | 2.48 (.99) | 2.60 (.85) |
| Peers | 2.20 (.62) | 1.96 (.77) | 2.07 (.70) |
| Home | 2.50 (.83) | 2.35 (.94) | 2.42 (.88) |
| Community | 1.65 (.88) | 2.04 (.82) | 1.86 (.86) |
| Symptoms: M (SD)2 | |||
| Depression | 3.75 (1.52) | 4.48 (1.04)* | 4.14 (1.32) |
| Euphoria | 3.70 (.73) | 3.52 (.73) | 3.60 (.73) |
| Irritability | 4.25 (.91) | 4.26 (.75) | 4.30 (.82) |
| Anxiety | 2.80 (1.32) | 2.78 (1.28) | 2.79 (1.28) |
| Psychosis | 1.90 (1.17) | 1.87 (1.06) | 1.88 (1.10) |
| Sleep | 2.70 (1.03) | 3.13 (.97) | 2.93 (1.01) |
| Energy regulation | 3.05 (1.00) | 3.26 (1.01) | 3.16 (1.00) |
| Attention | 3.55 (.89) | 3.35 (1.07) | 3.44 (.98) |
denotes differences significant at the p < .05 level,
p < .01 level; NOS = not otherwise specified; ADHD = attention deficit hyperactivity disorder; ODD = oppositional defiant disorder; CD = conduct disorder; EE = expressed emotion; EOI = emotional overinvolvement. Data on age at onset was missing for one boy.
Functioning scores were based on the Child and Adolescent Functioning Assessment Scale, which uses 1 (low impairment) to 4 (high impairment) scales.
The depression, euphoria, irritability, anxiety, and psychosis items were rated on the 1 – 6 Kiddie-Schedule for Affective Disorders and Schizophrenia Depression and Mania Rating Scales scales of severity. The sleep, energy regulation, and attention items were rated on 1–4 scales of severity.
Independent sample t-tests were calculated to determine whether significant differences existed between boys and girls on the key variables of interest. The mean age at first psychiatric treatment was significantly younger for boys (M = 6.58, SD = 3.75) than for girls (M = 9.95, SD = 3.15), t(40) = −3.13, p < .01. Consequently, the mean lifetime duration of mood disorder was significantly longer in boys (M = 7.48, SD = 3.35) than girls (M = 5.14, SD = 2.59), t(40) = 2.50, p < .05. Significantly more boys had a childhood onset (prior to age 13) of bipolar disorder (71.4%) and significantly more girls had an adolescent onset (73.9%), χ2(1, N = 43) = 10.23, p < .01. Independent of gender, youths with a childhood onset of bipolar disorder had significantly longer lifetime durations of mood disorder than youths with an adolescent onset (t(38) = 3.30, p < .005).
Significantly more boys exhibited comorbid ADHD within the 3 months prior to study entry than girls, χ2 (1, N = 44) = 4.62, p < .05. In contrast, girls exhibited more severe recent depression than boys, t(42) = 1.88, p <.01. Of the 21 boys, 10 (47.6%) had past and/or current stimulant treatment for ADHD; of the 23 girls, 5 (21.7%) had had stimulant treatment. Only 2 boys and 4 girls were taking stimulants for treatment of ADHD at entry into the study. Of the 10 boys with a history of stimulant treatment, 6 were from high-EE families and 4 were from low-EE families. Of the 5 females, 4 were from high-EE families and 1 was from a low-EE family. The proportions of youths taking stimulants in high- and low-EE families did not differ in either gender (p > .10).
Correlates of Expressed Emotion
Of the 23 girls, 14 (60.9%) had parents with high-EE critical attitudes (i.e., 6 or more critical comments); of the 21 boys, 3 (14.5%) had high-EE critical parents (χ2(1, N = 44) = 10.05, p < .01). Also, parents of girls made more critical comments (M = 6.17, SD = 3.69) than parents of boys (M = 3.29, SD = 2.65; t(42)= 2.96, p =.005; Table 3). There were no differences between parents of boys and girls in emotional overinvolvement scores. No significant correlations emerged between the severity of any recent symptom or functioning variable and EE (Table 3).
Table 3.
Correlations among demographic, EE, and symptom variables (N = 44)
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Gender | 1.0 | - | - | - | - | - | - | - | - | - | |
| 2. Age at first treatment | .45* | 1.0 | - | - | - | - | - | - | - | - | |
| 3. Onset | .49* | .55* | 1.0 | - | - | - | - | - | - | - | |
| 4. Duration | −.37* | −.92* | −.47* | 1.0 | - | - | - | - | - | - | |
| 5. Depression | .28 | .17 | .30 | −.13 | 1.0 | - | - | - | - | - | |
| 6. Sleep | .22 | .19 | .20 | −.09 | .51* | 1.0 | - | - | - | - | |
| 7. Energy | .11 | .09 | .32* | −.10 | .15 | .20 | 1.0 | - | - | - | |
| 8. Low v. High EE | .18 | −.11 | .26 | .14 | −.07 | .04 | .23 | 1.0 | - | - | |
| 9. Low v. High Criticism | .48* | .24 | .31* | −.23 | .06 | .10 | .25 | .63* | 1.0 | - | - |
| 10. Total critical comments | .42* | .09 | .27 | −.06 | .07 | .19 | .20 | .56* | .79* | 1.0 | - |
| 11. Total EOI score | −.21 | −.19 | −.03 | .27 | −.01 | .05 | .11 | .45* | −.10 | −.05 | 1.0 |
significant at the p < .05 level; for gender, 0 = male and 1 = female; for onset, 0 = childhood and 1 = adolescence. EE = expressed emotion; EOI = emotional overinvolvement.
Contrary to our initial hypothesis, children with later ages at onset were more likely to have parents who were high in EE criticism. Of the 22 youths with adolescent onset, 12 (54.5%) had parents rated high in criticism, and 10 (45.5%) had only low criticism parents. Of the 21 youths who had childhood onset, 5 (23.8%) had high-EE, critical parents and 16 (76.2%) had low criticism parents (χ2(1, N = 43) = 4.20, p = .036). The relationship between gender and age at onset, as well as between gender and EE (Table 3) raised the possibility that the association between age at onset and EE was moderated by gender. Two 2 (gender: male vs. female) × 2 (illness onset: child vs. adolescent) analyses of variance (ANOVAs) were conducted with number of critical comments (the highest score obtained by a parent in the family) and emotional overinvolvement score as the dependent variables. As indicated above, there was a significant main effect of gender on number of critical comments, F(1,39) = 6.32, p < .02. Although there was no main effect of age at onset on number of criticisms (F(1, 39) = 0.15, p > .10), there was a significant interaction between gender and age at onset, F(1, 39) = 4.26, p < .05, such that parents of girls exhibited more critical comments when the youth had an adolescent onset of bipolar disorder and fewer critical comments when the youth had childhood-onset. The pattern was reversed for boys, whose parents were most critical when the youth had childhood (versus adolescent) onset (Figure 1).
Fig. 1.
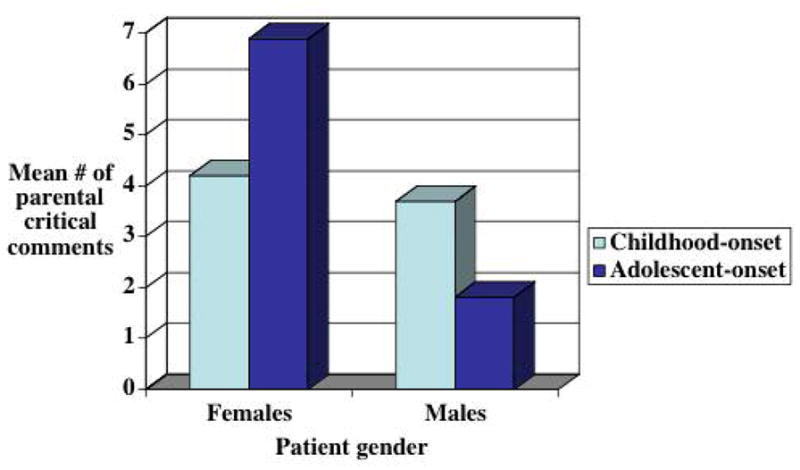
Interaction between gender and age of onset in predicting parental EE-critical comments (F(1,39) = 4.26, p < .05). Data on age at onset were missing for one boy for whom parental EE data were available.
A second gender by onset ANOVA was conducted for total score on the parental emotional overinvolvement scale. Neither gender (F(1,43) = 1.40, p > .10) nor age of illness onset (F(1,43) = 1.0, p > .10) were associated with the amount of parental overinvolvement. In addition, the interaction between gender and time of onset in predicting parental overinvolvement was non-significant (F(1,43) = .15, p > .10).
Discussion
Research has established the prospective relationship between parental EE and patient outcomes across a variety of disorders. Few studies, however, have identified the patient attributes that help explain why some parents are high in EE and some are low. This study examined whether current and historical illness characteristics of juvenile bipolar patients were associated with high parental EE during a child’s adolescence, and whether gender moderated these relationships. Contrary to the hypotheses, the current severity of the bipolar illness and its associated functional impairments – as measured during the same interval in which EE was measured (3 months prior to entry into a treatment trial) - were not associated with parental EE. Consistent with findings from the schizophrenia literature (Hooley & Gotlib, 2000), levels of parental EE do not appear to be a direct function of the level of severity of the patient’s concurrent illness.
We did, however, find a main effect of patient gender on EE: parents of girls were more likely to be highly critical of their child than parents of boys. Even more importantly, girls with an adolescent onset of bipolar illness had parents who expressed more critical comments than girls with childhood onset. In contrast, boys with childhood onset bipolar disorder were more likely to have highly critical parents than boys with adolescent onset.
In this sample, boys were more likely than girls to have had onset of their mood disorder in childhood, whereas girls were more likely to be diagnosed at puberty or during adolescence. Even prior to the bipolar diagnosis, boys were first treated for a psychiatric disorder at a younger age than girls, and, subsequently, had a longer duration of illness in the years leading up to the study. Clearly, age at onset needs to be considered when examining the role of family EE or other environmental contributors to the course of bipolar illness.
There are several plausible explanations for why boys and girls differed in the age of onset and age at first treatment. One possibility is that boys and girls experience onset at similar times, but the manifestation of symptoms is different between the genders. Possibly, boys with childhood onset exhibit more externalizing symptoms (e.g., aggression), whereas girls are more likely to show internalizing symptoms (i.e., depression or anxiety). As a result, the disorder may not be diagnosed in girls until adolescence, even though it may have developed much earlier. Consistent with this hypothesis, girls in this sample had more severe concurrent depressive symptoms than boys, whereas boys were more likely than girls to enter the study with comorbid ADHD. Perhaps the presence of comorbid ADHD in boys led to psychiatric evaluation and a bipolar diagnosis at a younger age. Chang, Howe, Gallelli, & Miklowitz (2006) hypothesized that, among children with a family history of bipolar disorder, ADHD is the first prodromal sign of a developing bipolar illness. Alternatively, early psychostimulant use for ADHD may elicit manic symptoms in children who are genetically at risk for bipolar disorder (Reichart & Nolen, 2004).
Parents who are later classified as high in EE may become more critical and less tolerant of their male offspring as the offspring expresses more externalizing behavior. They may also be more likely than low-EE parents to seek treatment for their male child at an earlier age. In contrast, parents may not react as strongly to the social withdrawal or anergia of depressed girls until these girls enter the adolescent years and become more moody, uncooperative, engage in increasingly risky behavior, or press for more autonomy (Arnett, 1999). For both genders, parents may react with criticism or hostility to the considerable irritability of their child, which may fuel more irritability from the child and increasingly hostile family interactions. Thus, EE may develop as a reaction to the initial, subsyndromal symptoms of bipolar disorder in at risk children, but may subsequently play an independent role in evoking the expression of these symptoms once children are diagnosed (Miklowitz, 2007).
This study had several limitations. First, the design was cross-sectional, so we were unable to determine whether parental high-EE attitudes were present at the first onset of the illness or whether they developed after the parent had dealt with repeated episodes of the disorder. Likewise, we did not examine the relation of EE to prospective outcomes, because some of the children were in a randomized trial and some were in an open trial of family-focused treatment and pharmacotherapy. Therefore, we were not able to determine whether correlates of EE – such as gender or age at onset – account for its prospective relationship with patients’ outcomes. The small sample size and cross-sectional design limited our statistical power to identify multivariate developmental pathways to high-EE attitudes among parents. Finally, the sample was primarily white and middle-class. Thus, we cannot generalize our results to different racial or ethnic backgrounds or socioeconomic levels.
Research on the influence of the family environment on the onset and course of childhood-onset bipolar disorder is critical to the development of preventative interventions. Parents may react to the earliest signs of the disorder, including irritability, depression, impulsiveness, and inattentiveness, with high levels of criticism. The nature of their reactions may vary with the gender of the child and the timing of onset. Family interventions administered early in the course of the illness, perhaps even during the pre-onset period, may derail the development of negative parent/child interactions and decrease the impact of the disorder on the child’s current and future functioning.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, D. C.: American Psychiatric Press; 2000. (Text Revision) (DSM-IV-TR) [Google Scholar]
- Arnett JJ. Adolescent storm and stress, reconsidered. American Psychologist. 1999;54:317–326. doi: 10.1037//0003-066x.54.5.317. [DOI] [PubMed] [Google Scholar]
- Axelson D, Birmaher BJ, Brent D, Wassick S, Hoover C, Bridge J, Ryan N. A preliminary study of the Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children mania rating scale for children and adolescents. Journal of Child and Adolescent Psychopharmacology. 2003;13:463–470. doi: 10.1089/104454603322724850. [DOI] [PubMed] [Google Scholar]
- Chambers WJ, Puig-Antich J, Hirsch M, Paez P, Ambrosini PJ, Tabrizi MA, Davies M. The assessment of affective disorders in children and adolescents by semi-structured interview: test-retest reliability. Archives of General Psychiatry. 1985;42:696–702. doi: 10.1001/archpsyc.1985.01790300064008. [DOI] [PubMed] [Google Scholar]
- Chang K, Howe M, Gallelli K, Miklowitz D. Prevention of pediatric bipolar disorder: integration of neurobiological and psychosocial processes. Annals of the New York Academy of Sciences. 2006;1094:235–247. doi: 10.1196/annals.1376.026. [DOI] [PubMed] [Google Scholar]
- Craney JL, Gller B. A prepubertal and early-adolescent bipolar disorder-I phenotype: review of phenomenology and longitudinal course. Bipolar Disorders. 2003;5:243–256. doi: 10.1034/j.1399-5618.2003.00044.x. [DOI] [PubMed] [Google Scholar]
- Faraone SV, Glatt SJ, Tsuang MT. The genetics of pediatric-onset bipolar disorder. Society of Biological Psychiatry. 2003;53:970–977. doi: 10.1016/s0006-3223(02)01893-0. [DOI] [PubMed] [Google Scholar]
- Fergus EL, Miller RB, Luckenbaugh DA, Leverich GS, Findling RL, Speer AM, Post RM. Is there progression from irritability/dyscontrol to major depressive and manic symptoms? A retrospective community survey of parents of bipolar children. Journal of Affective Disorders. 2003;77:71–78. doi: 10.1016/s0165-0327(02)00176-3. [DOI] [PubMed] [Google Scholar]
- Fristad MA, Goldberg-Arnold JS. Raising a moody child: how to cope with depression and bipolar disorder. New York: Guilford Press; 2003. [Google Scholar]
- Hankin BL, Abramson LY. Development of gender differences in depression: an elaborated cognitive vulnerability-transactional stress theory. Psychological Bulletin. 2001;127:773–796. doi: 10.1037/0033-2909.127.6.773. [DOI] [PubMed] [Google Scholar]
- Hodges K. The Child and Adolescent Functional Assessment Scale (CAFAS) In: Maruish ME, editor. The use of psychological testing for treatment planning and outcome assessment. 3. Mahwah, NJ: Lawrence Erlbaum Associates; 2004. pp. 405–441. [Google Scholar]
- Hodges K, Wong MM. Psychometric characteristics of a multidimensional measure to assess impairment: the child and adolescent functional assessment scale. Journal of Child and Family Studies. 1996;5:445–467. [Google Scholar]
- Hooley JM. Expressed emotion and psychiatric illness: from empirical data to clinical practice. Behavior Therapy. 1998;29:631–646. [Google Scholar]
- Hooley JM, Gotlib IH. A diathesis-stress conceptualization of expressed emotion and clinical outcome. Applied and Preventive Psychology. 2000;9:131–151. [Google Scholar]
- Hooley JM, Richters J. Expressed emotion: A developmental perspective. In: Cicchetti D, Toth SL, editors. Emotion, cognitions, and representations. Rochester, N. Y.: University of Rochester Press; 1995. [Google Scholar]
- Jarbin H, Grawe RW, Hansson K. Expressed emotion and prediction of relapse in adolescents. Nordic Journal of Psychiatry. 2000;54:201–205. [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:98–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Kim EY, Miklowitz DJ, Biuckians A, Mullen K. Life stress and the course of early-onset bipolar disorder. Journal of Affective Disorders. 2007;99 (1):37–44. doi: 10.1016/j.jad.2006.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leibenluft E, Cohen P, Gorrindo T, Brook JS, Pine DS. Chronic versus episodic irritability in youth: a community-based, longitudinal study of clinical and diagnostic associations. Journal of Child and Adolescent Psychopharmacology. 2006;4:456–466. doi: 10.1089/cap.2006.16.456. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Klein DN, Seeley JR. Bipolar disorder during adolescence and young adulthood in a community sample. Bipolar Disorders. 2000;2:281–293. doi: 10.1034/j.1399-5618.2000.20309.x. [DOI] [PubMed] [Google Scholar]
- MacMillan JF, Gold A, Crow TJ, Johnson AL, Johnstone EC. Expressed emotion and relapse in schizophrenia. British Journal of Psychiatry. 1986;148:741–744. [PubMed] [Google Scholar]
- McFarlane WR, Cook WL. Family expressed emotion prior to onset of psychosis. Family Process. 2007;46:185–197. doi: 10.1111/j.1545-5300.2007.00203.x. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ. The role of the family in the course and treatment of bipolar disorder. Current Directions in Psychological Science. 2007;16:192–196. doi: 10.1111/j.1467-8721.2007.00502.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ, George EL, Axelson DA, Kim EY, Birmaher B, Schneck C, Beresford C, Craighead WE, Brent DA. Family-focused treatment for adolescents with bipolar disorder. Journal of Affective Disorders. 2004;82S:S113–S128. doi: 10.1016/j.jad.2004.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ, Goldstein MJ, Nuechterlein KH, Snyder KS, Mintz J. Family factors and the course of bipolar affective disorder. Archives of General Psychiatry. 1988;45:225–231. doi: 10.1001/archpsyc.1988.01800270033004. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, Biuckians A, Richards J. Early-onset bipolar disorder: a family treatment perspective. Developmental Psychopathology. 2006;18:1247–1265. doi: 10.1017/S0954579406060603. [DOI] [PubMed] [Google Scholar]
- Nuechterlein KH, Snyder KS, Mintz J. Paths to relapse: possible transactional processes connecting patient illness onset, expressed emotion, and psychotic relapse. British Journal of Psychiatry. 1992;18(suppl):88–96. [PubMed] [Google Scholar]
- Perlis RH, Miyahara S, Marangell LB, Wisniewski SR, Ostacher M, DelBello MP, Bowden CL, Sachs GS, Nierenberg AA. Long-term implications of early onset in bipolar disorder: data from the first 1000 participants in the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) Biological Psychiatry. 2004;55:875–881. doi: 10.1016/j.biopsych.2004.01.022. [DOI] [PubMed] [Google Scholar]
- Reichart CG, Nolen WA. Earlier onset of bipolar disorder in children by antidepressants or stimulants? An hypothesis. Journal of Affective Disorders. 2004;78(1):81–84. doi: 10.1016/s0165-0327(02)00180-5. [DOI] [PubMed] [Google Scholar]
- Vaughn CE, Leff JP. The influence of family and social factors on the course of psychiatric illness: a comparison of schizophrenia and depressed neurotic patients. British Journal of Psychiatry. 1976;129:125–137. doi: 10.1192/bjp.129.2.125. [DOI] [PubMed] [Google Scholar]
- Wilkinson GB, Taylor P, Holt JR. Bipolar disorder in adolescence: diagnosis and treatment. Journal of Mental Health Counseling. 2002;24:348–357. [Google Scholar]
- Yan LJ, Hammen C, Cohen AN, Daley SE, Henry RM. Expressed emotion versus relationship quality variables in the prediction of recurrence in bipolar patients. Journal of Affective Disorders. 2004;83:199–206. doi: 10.1016/j.jad.2004.08.006. [DOI] [PubMed] [Google Scholar]


