Abstract
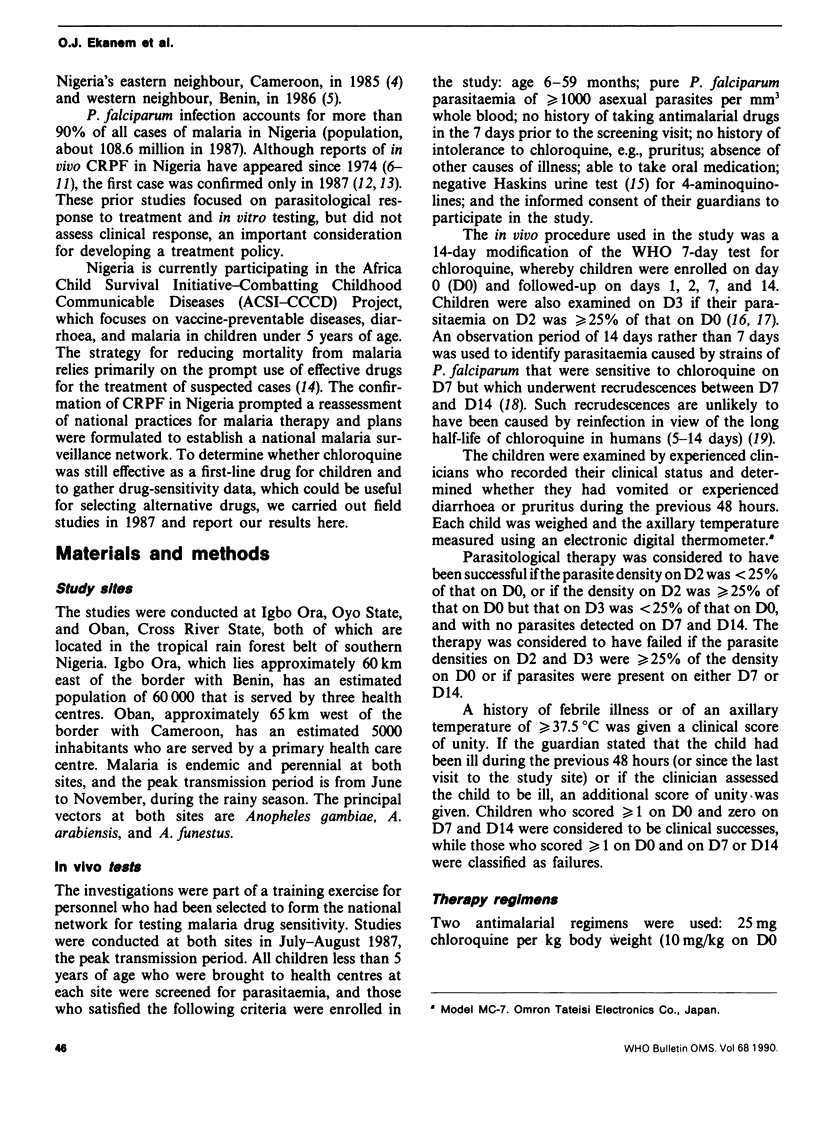
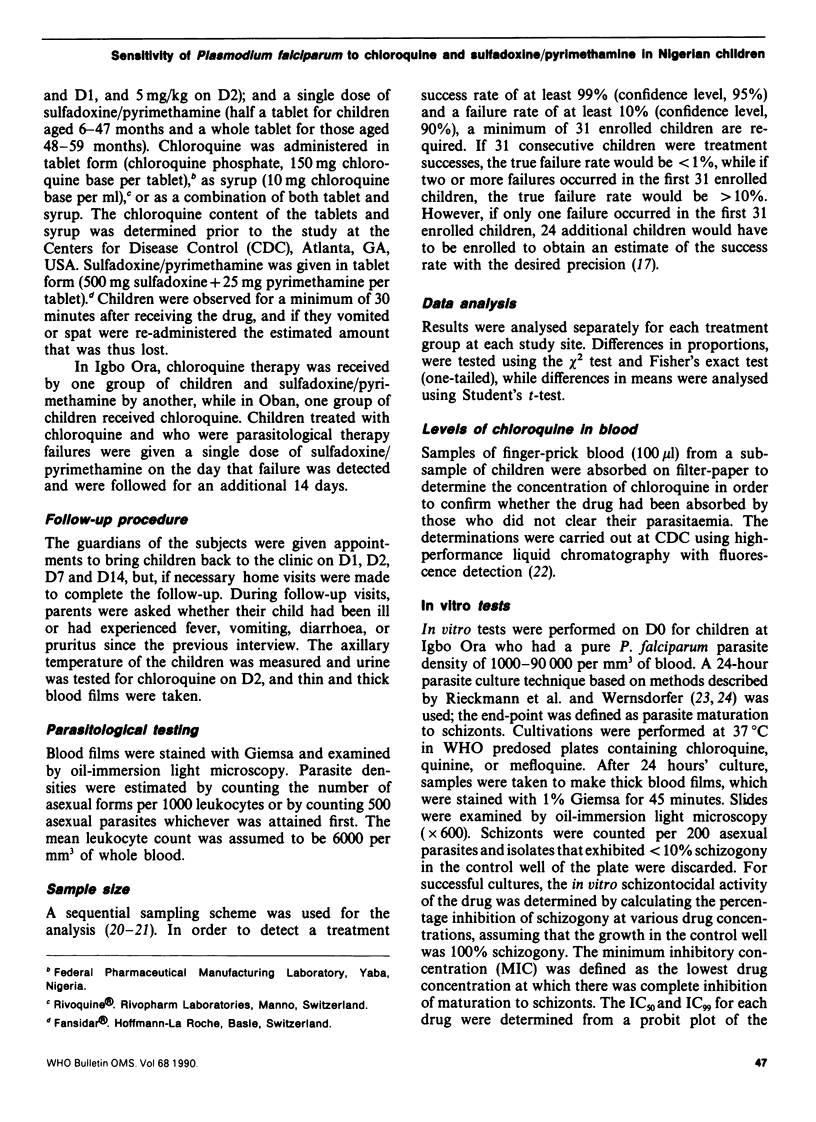
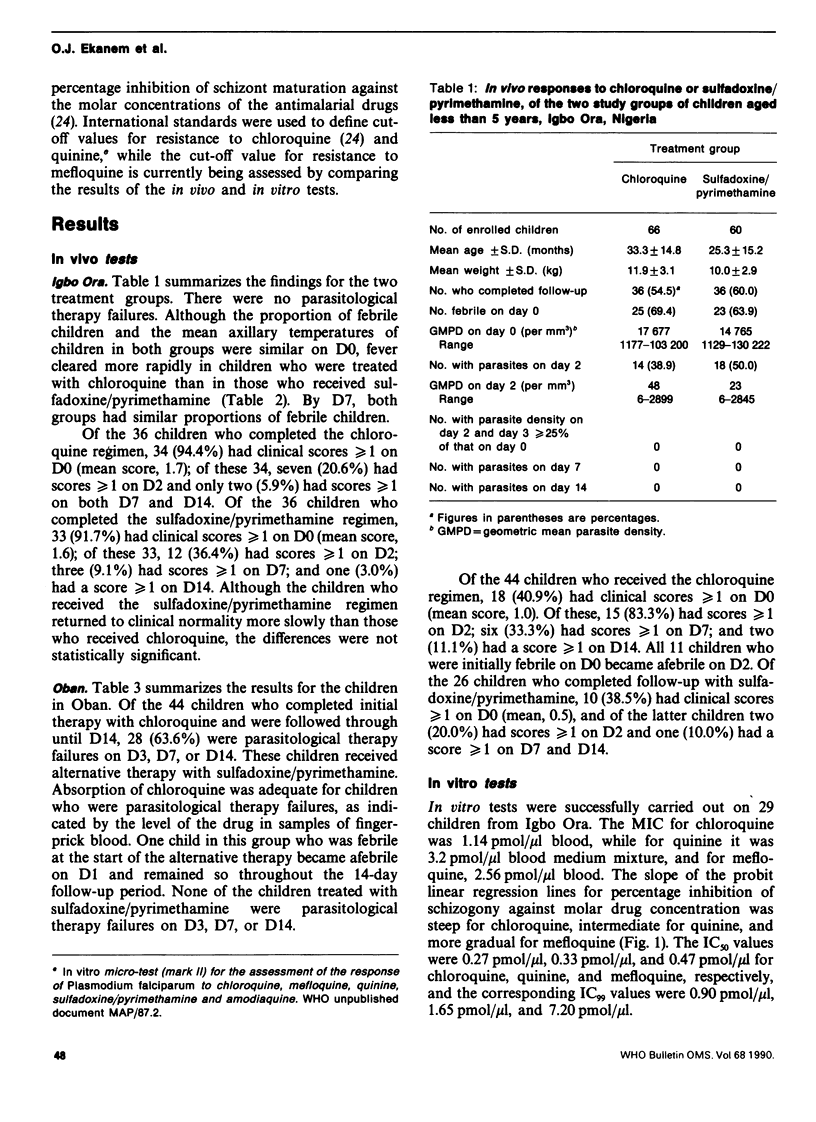
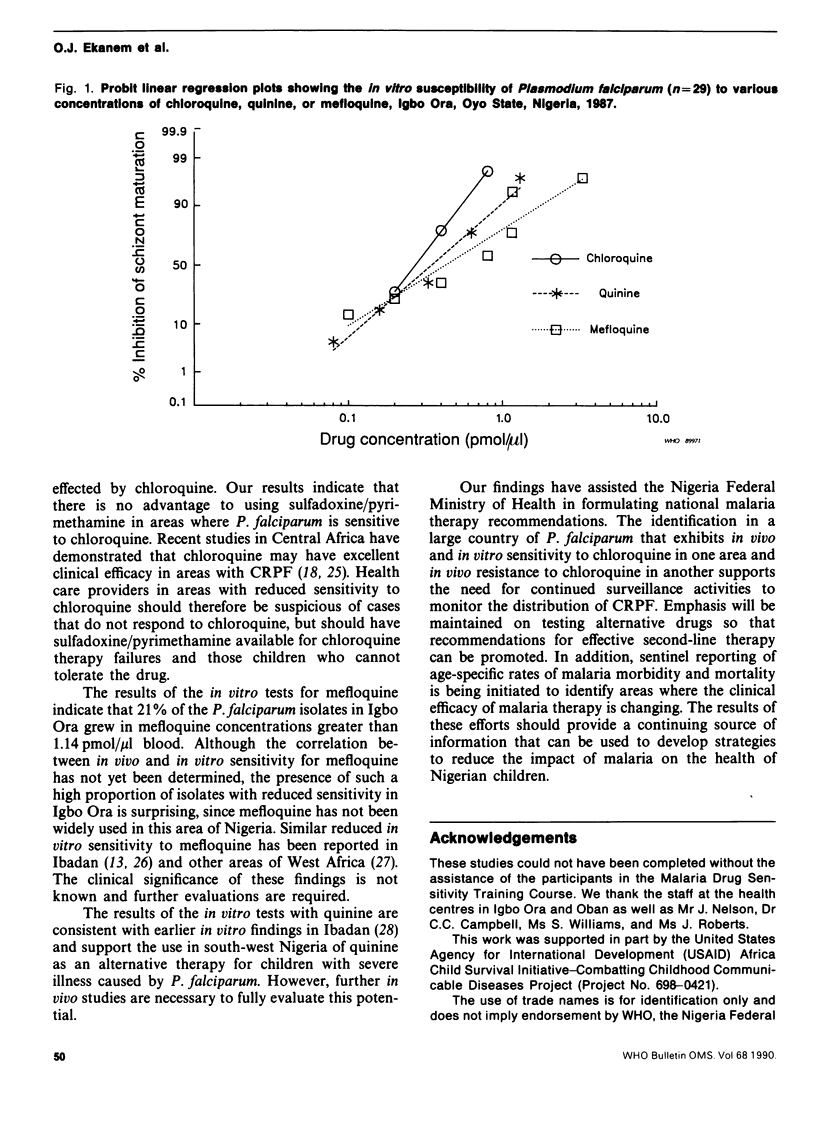
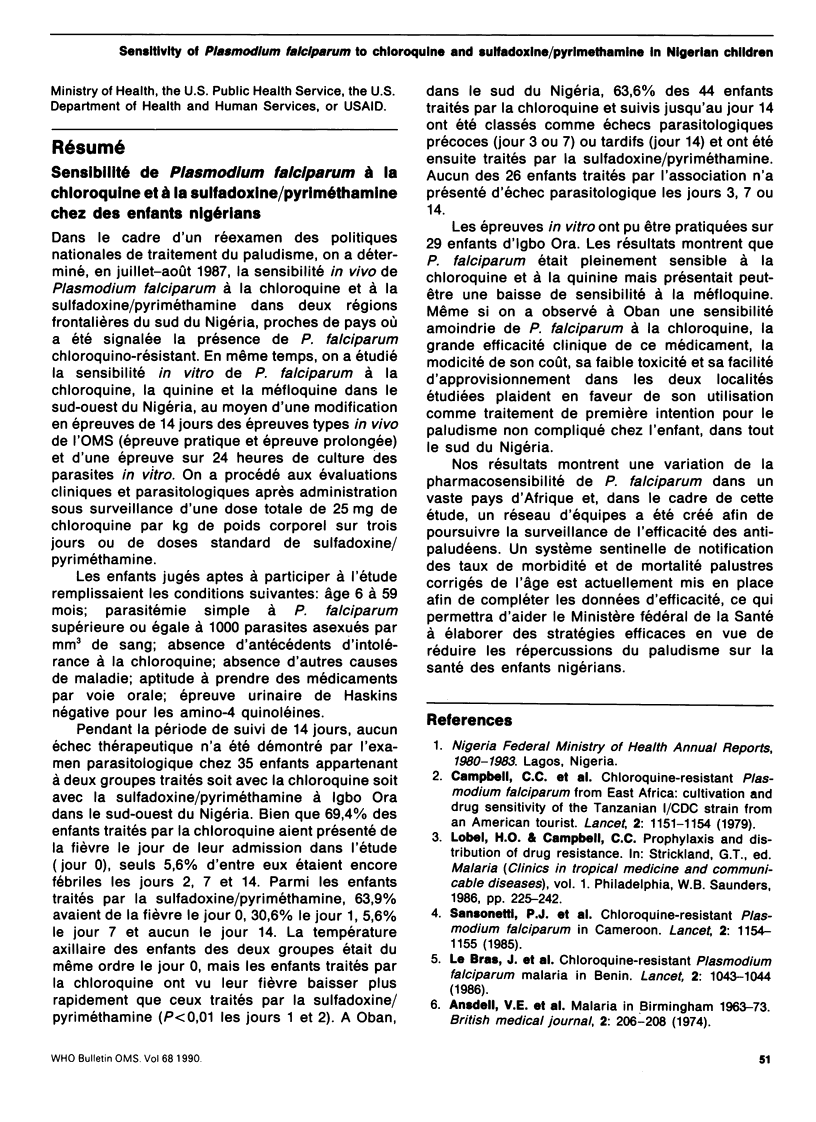
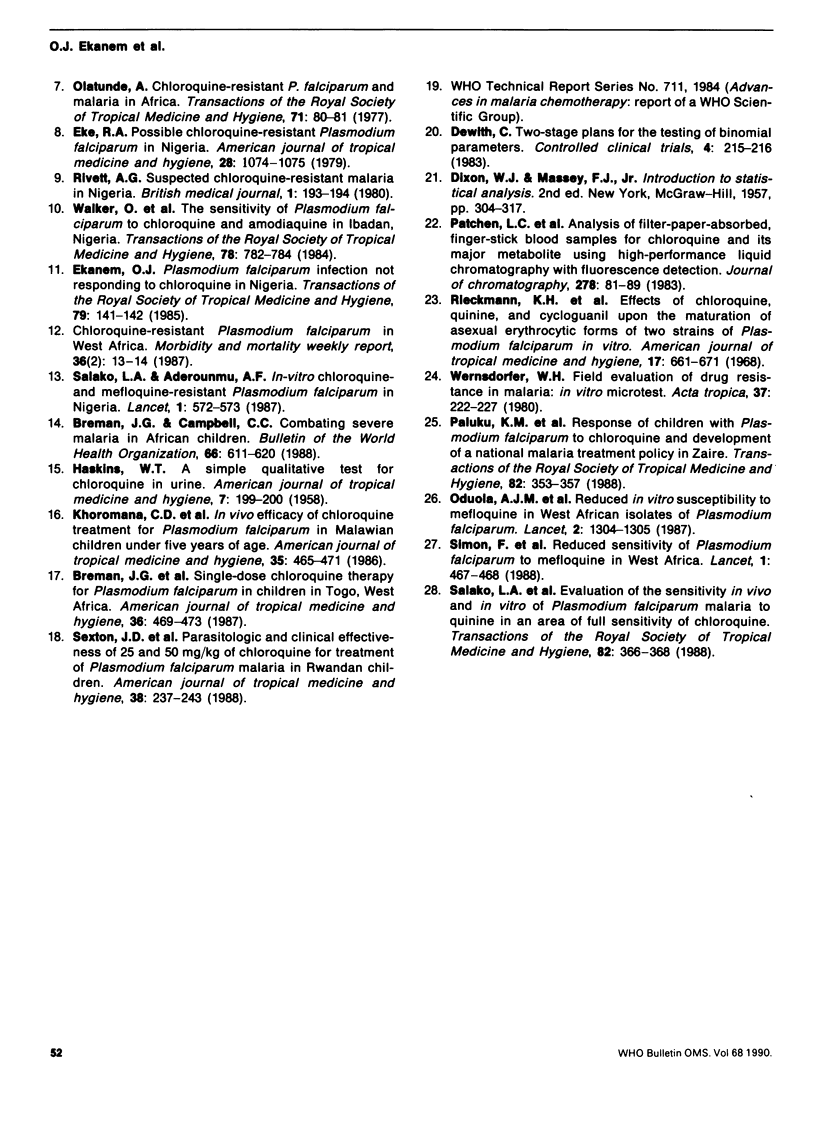
The in vivo sensitivity of Plasmodium falciparum to chloroquine and sulfadoxine/pyrimethamine was evaluated in children under 5 years of age in two areas of southern Nigeria in 1987. A modification of the WHO Standard Field and Extended Tests (in vivo) was used, with follow-up on days, 2, 3, 7, and 14 after treatment with 25 mg chloroquine per kg body weight given over 3 days, or with standard doses of sulfadoxine/pyrimethamine. Clinical and parasitological evaluations were performed. At Igbo Ora, in Oyo State, where by day 7 chloroquine was clinically successful in 94.4% of 36 children and sulfadoxine/pyrimethamine in 91.7% of 36 children, there were no parasitological failures in either treatment group. Fever regressed significantly more rapidly with chloroquine than with sulfadoxine/pyrimethamine. At Oban, in Cross River State, initial parasite densities decreased markedly with the chloroquine regimen but 63.6% of 44 children were parasitological failures on days 3, 7, or 14; and all of the 26 children who failed parasitologically and completed follow-up were successfully treated with sulfadoxine/pyrimethamine. By day 7, clinical success was demonstrated for 77.3% of the children treated with chloroquine. The in vitro sensitivity to chloroquine, quinine, and mefloquine at Igbo Ora indicated that isolates of P. falciparum were sensitive to chloroquine and quinine, but had reduced sensitivity to mefloquine. Because of its continued clinical efficacy, chloroquine remains the recommended treatment for children with uncomplicated malaria in Nigeria. Health providers are, however, encouraged to maintain supplies of sulfadoxine/pyrimethamine as an alternative and to refer patients promptly if necessary.
Full text
PDF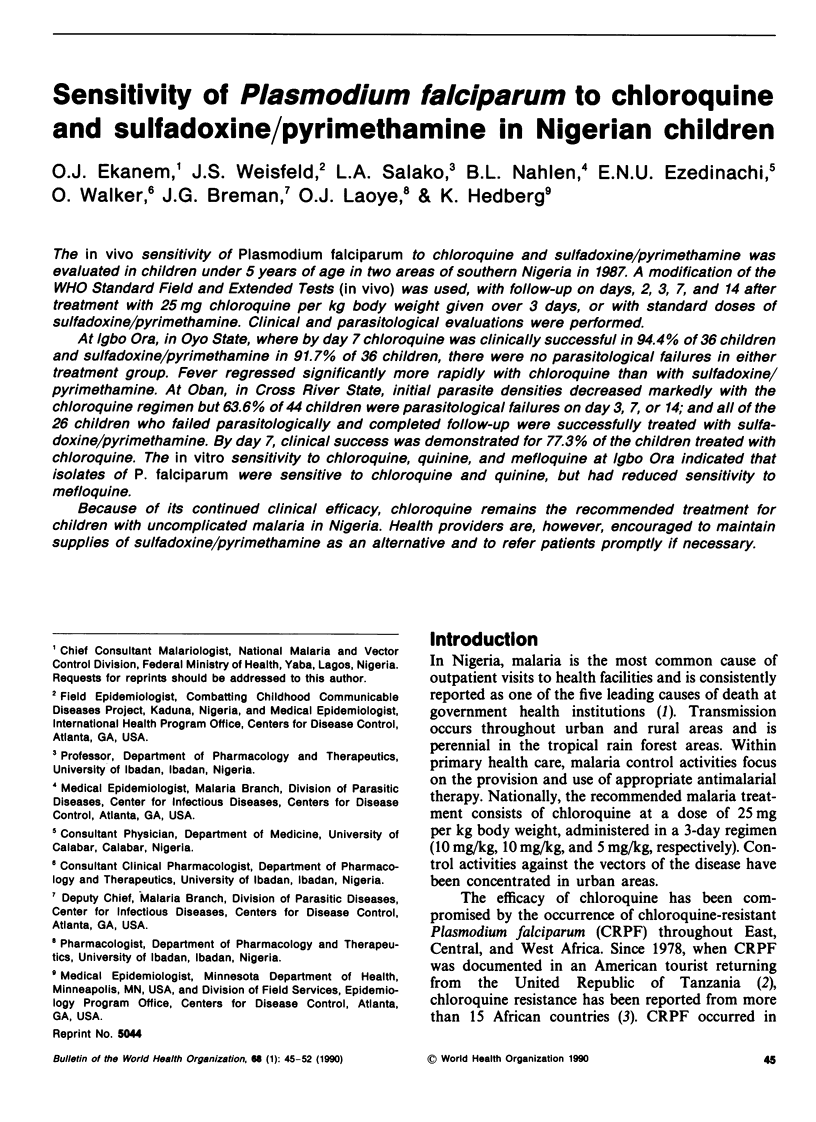
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ansdell V. E., Boosey C. M., Geddes A. M., Morgan H. V. Malaria in Birmingham 1968-73. Br Med J. 1974 Apr 27;2(5912):206–208. doi: 10.1136/bmj.2.5912.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breman J. G., Campbell C. C. Combating severe malaria in African children. Bull World Health Organ. 1988;66(5):611–620. [PMC free article] [PubMed] [Google Scholar]
- Breman J. G., Gayibor A., Roberts J. M., Sexton J. D., Agbo K., Miller K. D., Karsa T., Murphy K. Single-dose chloroquine therapy for Plasmodium falciparum in children in Togo, West Africa. Am J Trop Med Hyg. 1987 May;36(3):469–473. doi: 10.4269/ajtmh.1987.36.469. [DOI] [PubMed] [Google Scholar]
- Campbell C. C., Chin W., Collins W. E., Teutsch S. M., Moss D. M. Chloroquine-resistant Plasmodium falciparum from East Africa: cultivation and drug sensitivity of the Tanzanian I/CDC strain from an American tourist. Lancet. 1979 Dec 1;2(8153):1151–1154. doi: 10.1016/s0140-6736(79)92383-3. [DOI] [PubMed] [Google Scholar]
- Ekanem O. J. Plasmodium falciparum infection not responding to chloroquine in Nigeria. Trans R Soc Trop Med Hyg. 1985;79(1):141–142. doi: 10.1016/0035-9203(85)90268-8. [DOI] [PubMed] [Google Scholar]
- Eke R. A. Possible chloroquine-resistant Plasmodium falciparum in Nigeria. Am J Trop Med Hyg. 1979 Nov;28(6):1074–1075. doi: 10.4269/ajtmh.1979.28.1074. [DOI] [PubMed] [Google Scholar]
- HASKINS W. T. A simple qualitative test for chloroquine in urine. Am J Trop Med Hyg. 1958 Mar;7(2):199–200. doi: 10.4269/ajtmh.1958.7.199. [DOI] [PubMed] [Google Scholar]
- Khoromana C. O., Campbell C. C., Wirima J. J., Heymann D. L. In vivo efficacy of chloroquine treatment for Plasmodium falciparum in Malawian children under five years of age. Am J Trop Med Hyg. 1986 May;35(3):465–471. doi: 10.4269/ajtmh.1986.35.465. [DOI] [PubMed] [Google Scholar]
- Le Bras J., Hatin I., Bouree P., Coco-Cianci O., Garin J. P., Rey M., Charmot G., Roue R. Chloroquine-resistant falciparum malaria in Benin. Lancet. 1986 Nov 1;2(8514):1043–1044. doi: 10.1016/s0140-6736(86)92657-7. [DOI] [PubMed] [Google Scholar]
- Oduola A. M., Milhous W. K., Salako L. A., Walker O., Desjardins R. E. Reduced in-vitro susceptibility to mefloquine in West African isolates of Plasmodium falciparum. Lancet. 1987 Dec 5;2(8571):1304–1305. doi: 10.1016/s0140-6736(87)91195-0. [DOI] [PubMed] [Google Scholar]
- Olatunde A. Chloroquine-resistant Plasmodium falciparum and malaria in Africa. Trans R Soc Trop Med Hyg. 1977;71(1):80–81. doi: 10.1016/0035-9203(77)90213-9. [DOI] [PubMed] [Google Scholar]
- Salako L. A., Fadeke Aderounmu A. In-vitro chloroquine and mefloquine-resistant Plasmodium falciparum in Nigeria. Lancet. 1987 Mar 7;1(8532):572–573. doi: 10.1016/s0140-6736(87)90221-2. [DOI] [PubMed] [Google Scholar]
- Sexton J. D., Deloron P., Bugilimfura L., Ntilivamunda A., Neill M. Parasitologic and clinical efficacy of 25 and 50 mg/kg of chloroquine for treatment of Plasmodium falciparum malaria in Rwandan children. Am J Trop Med Hyg. 1988 Mar;38(2):237–243. doi: 10.4269/ajtmh.1988.38.237. [DOI] [PubMed] [Google Scholar]
- Walker O., Salako L. A., Obih P. O., Bademosi K., Sodeinde O. The sensitivity of Plasmodium falciparum to chloroquine and amodiaquine in Ibadan, Nigeria. Trans R Soc Trop Med Hyg. 1984;78(6):782–784. doi: 10.1016/0035-9203(84)90019-1. [DOI] [PubMed] [Google Scholar]


