Abstract
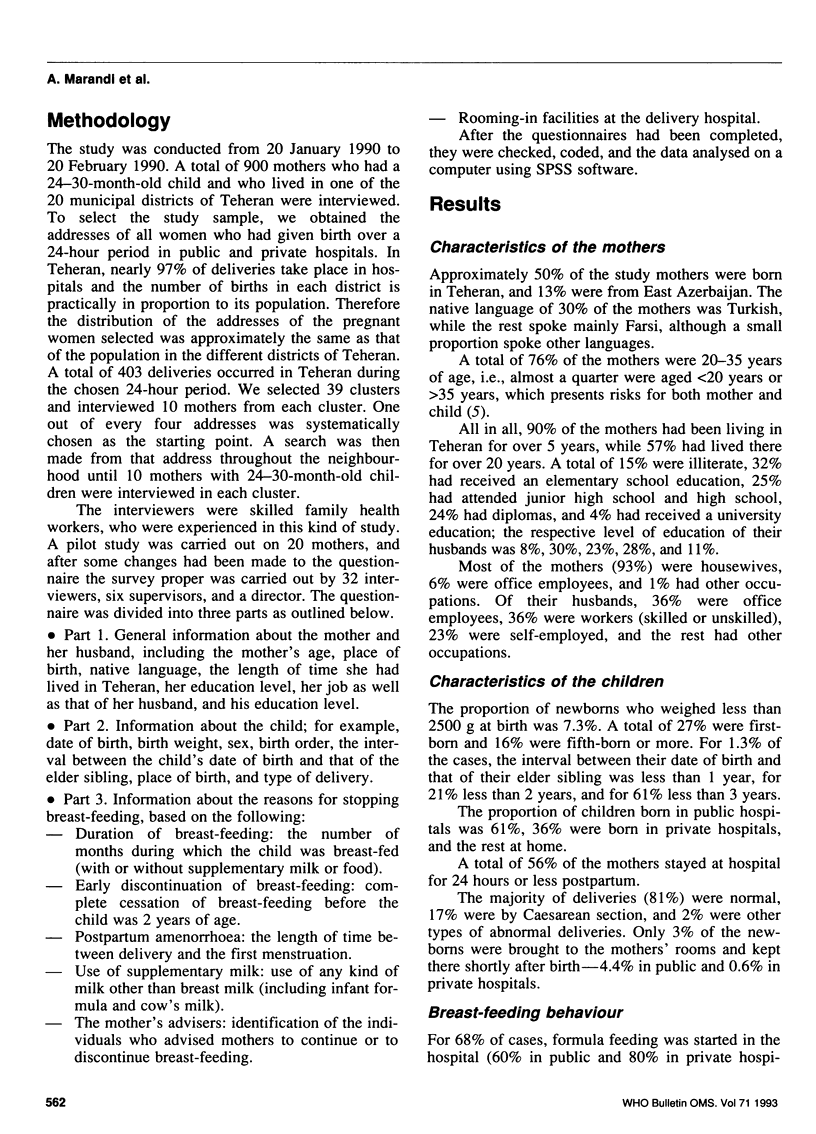
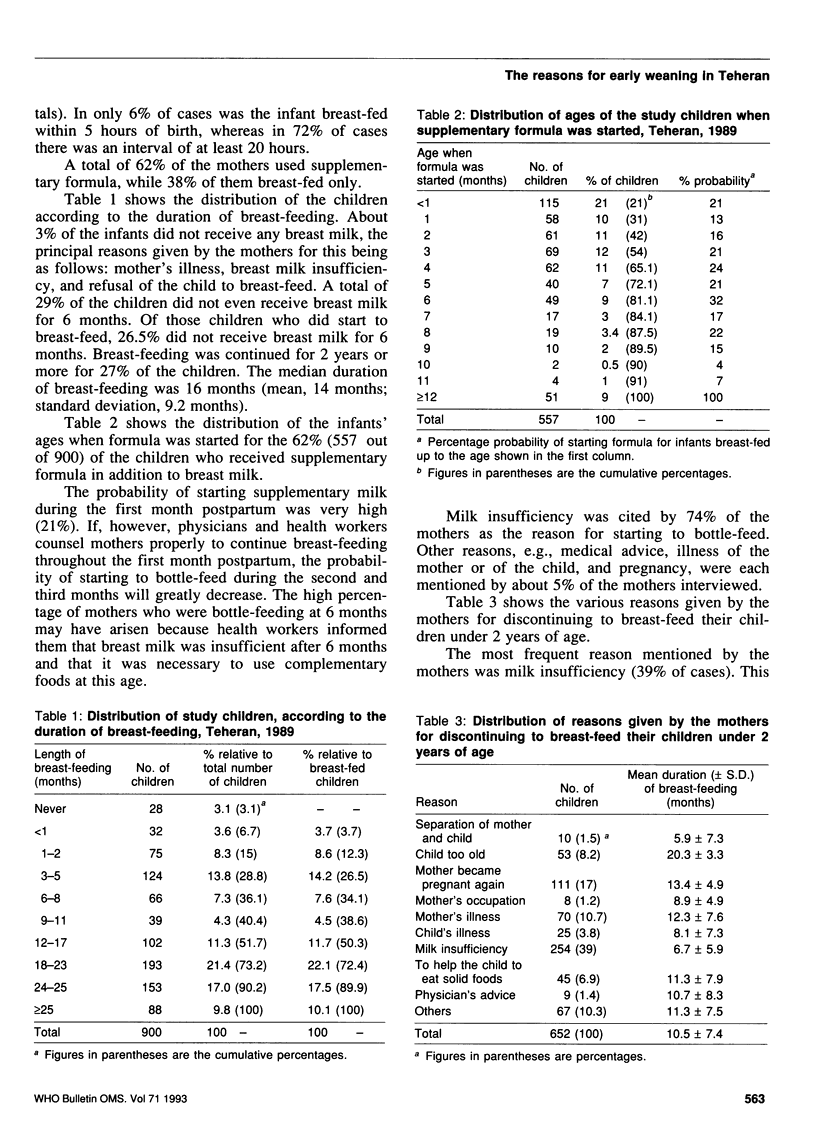
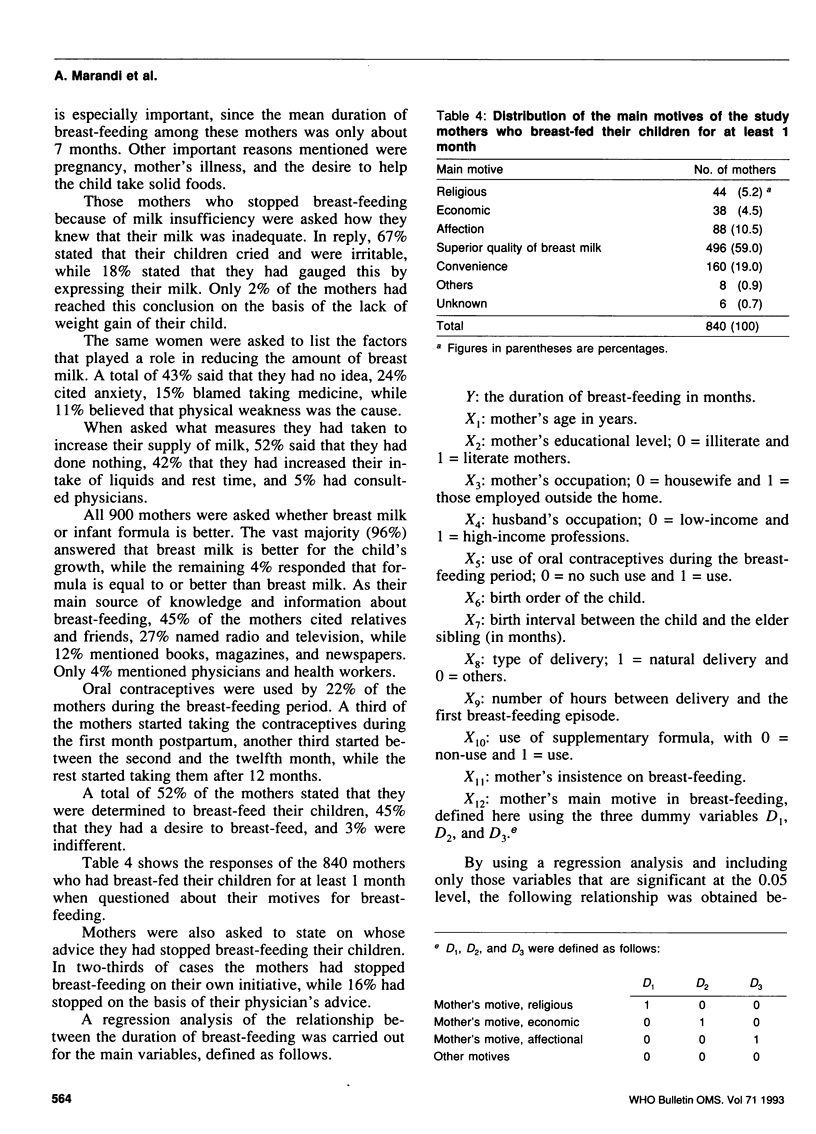
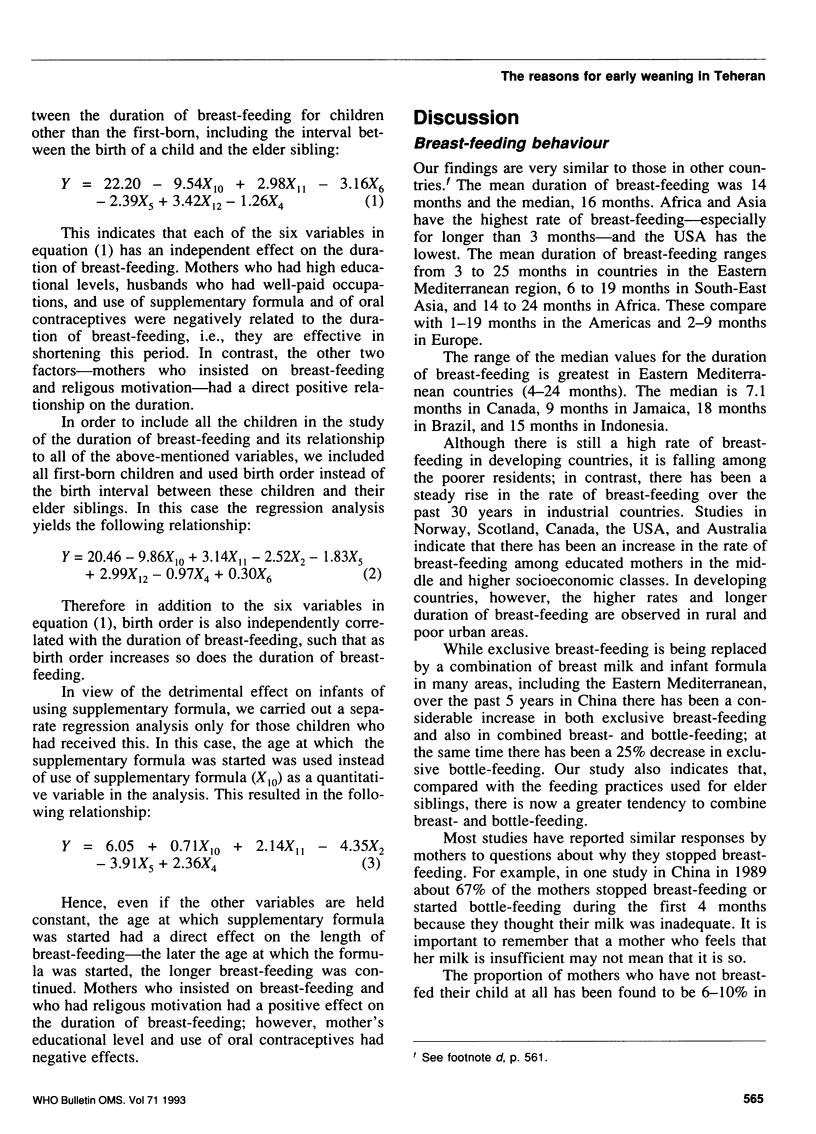
In order to identify the reasons for early weaning in Teheran, we interviewed 900 mothers using a systematic randomized sampling method. A total of 15% of the mothers were illiterate, 93% were housewives, and 97% had given birth in hospitals. Only 3% of the newborns benefited from rooming-in facilities in hospital, and 68% were bottle-fed while still in hospital. In 3.1% of cases the mother had not breast-fed her newborn at all. Of those who had breast-fed their infant, 38% used only their own milk, whereas 62% used a combination of breast milk and infant formula. The median duration of breast-feeding was 16 months (mean, 14 months). A total of 74% of mothers who used supplementary formula and 39% of those who had completely stopped breast-feeding blamed milk insufficiency, although 67% of these mothers had reached this conclusion only because their infants cried or were irritable. The following factors had a negative influence on the duration of breast-feeding: use of supplementary formula and of estrogen-containing oral contraceptives; fathers with high incomes; and mothers with a high educational level. In contrast, the mother's religious motive to breast-feed and her insistence on breast-feeding had a positive impact. Unfortunately, 21% of the mothers started using supplementary formula during the first month postpartum, and two-thirds before the end of the fourth month. Every month that bottle-feeding was started prematurely shortened the duration of breast-feeding by 20 days.(ABSTRACT TRUNCATED AT 250 WORDS)
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Almroth S., Bidinger P. D. No need for water supplementation for exclusively breast-fed infants under hot and arid conditions. Trans R Soc Trop Med Hyg. 1990 Jul-Aug;84(4):602–604. doi: 10.1016/0035-9203(90)90056-k. [DOI] [PubMed] [Google Scholar]
- Chandra R. K. Prospective studies of the effect of breast feeding on incidence of infection and allergy. Acta Paediatr Scand. 1979 Sep;68(5):691–694. doi: 10.1111/j.1651-2227.1979.tb18439.x. [DOI] [PubMed] [Google Scholar]
- Fallot M. E., Boyd J. L., 3rd, Oski F. A. Breast-feeding reduces incidence of hospital admissions for infection in infants. Pediatrics. 1980 Jun;65(6):1121–1124. [PubMed] [Google Scholar]
- Goodine L. A., Fried P. A. Infant feeding practices: pre- and postnatal factors affecting choice of method and the duration of breastfeeding. Can J Public Health. 1984 Nov-Dec;75(6):439–444. [PubMed] [Google Scholar]
- Kennedy K. I., Rivera R., McNeilly A. S. Consensus statement on the use of breastfeeding as a family planning method. Contraception. 1989 May;39(5):477–496. doi: 10.1016/0010-7824(89)90103-0. [DOI] [PubMed] [Google Scholar]
- Morrow-Tlucak M., Haude R. H., Ernhart C. B. Breastfeeding and cognitive development in the first 2 years of life. Soc Sci Med. 1988;26(6):635–639. doi: 10.1016/0277-9536(88)90028-7. [DOI] [PubMed] [Google Scholar]
- Rea M. F., Berquó E. S. Impact of the Brazilian national breast-feeding programme on mothers in greater São Paulo. Bull World Health Organ. 1990;68(3):365–371. [PMC free article] [PubMed] [Google Scholar]
- Relucio-clavano N. The results of a change in hospital practices: a paediatrician's campaign for breast-feeding in the Philippines. Assignment Child. 1981 Feb;55-56:139–165. [PubMed] [Google Scholar]
- Saadeh R., Benbouzid D. Breast-feeding and child-spacing: importance of information collection for public health policy. Bull World Health Organ. 1990;68(5):625–631. [PMC free article] [PubMed] [Google Scholar]
- Unni J. C., Richard J. Growth and morbidity of breast-fed and artificially-fed infants in urban south Indian families. J Trop Pediatr. 1988 Aug;34(4):179–181. doi: 10.1093/tropej/34.4.179. [DOI] [PubMed] [Google Scholar]


