Abstract
Ebola hemorrhagic fever is a rapidly progressing acute febrile illness characterized by high virus replication, severe immunosuppression, and case fatalities of ca. 80%. Inhibition of phosphorylation of interferon regulatory factor 3 (IRF-3) by the Ebola VP35 protein may block the host innate immune response and play an important role in the severity of disease. We used two precisely defined reverse genetics-generated Ebola viruses to investigate global host cell responses resulting from the inhibition of IRF-3 phosphorylation. The two viruses encoded either wild-type (WT) VP35 protein (recEbo-VP35/WT) or VP35 with an arginine (R)-to-alanine (A) amino acid substitution at position 312 (recEbo-VP35/R312A) within a previously defined IRF-3 inhibitory domain. When sucrose-gradient purified virus was used for infection, host cell whole-genome expression profiling revealed striking differences in human liver cell responses to these viruses differing by a single amino acid. The inhibition of host innate immune responses by WT Ebola virus was so potent that little difference in interferon and antiviral gene expression could be discerned between cells infected with purified WT, inactivated virus, or mock-infected cells. However, infection with recEbo-VP35/R312A virus resulted in a strong innate immune response including increased expression of MDA-5, RIG-I, RANTES, MCP-1, ISG-15, ISG-54, ISG-56, ISG-60, STAT1, IRF-9, OAS, and Mx1. The clear gene expression differences were obscured if unpurified virus stocks were used to initiate infection, presumably due to soluble factors present in virus-infected cell supernatant preparations. Ebola virus VP35 protein clearly plays a pivotal role in the potent inhibition of the host innate immune responses, and the present study indicates that VP35 has a wider effect on host cell responses than previously shown. The ability to eliminate this inhibitory effect with a single amino acid change in VP35 demonstrates the critical role this protein must play in the severe aspects this highly fatal disease.
Mortality associated with human outbreaks of hemorrhagic fever caused by filoviruses such as Zaire ebolavirus is extraordinarily high (ca. 80 to 90%) (28). Massive viral replication in the liver and spleen leads to rapidly progressing disease with hemorrhagic manifestations within days after symptoms appear (21, 31). Because of the rapid nature by which Ebola hemorrhagic fever progresses, death or survival of infected individuals is probably determined very soon after infection. Survivors of infection most likely are able to mount a more rapid and more effective innate immune response which curbs virus replication sufficiently to allow time for the development of adaptive immune responses. Studies have shown that survivors of Ebola infection have 100- to 1,000-fold lower peak viremia and significantly greater virus-specific antibody responses than fatal cases, who exhibit marked immunosuppression (1, 22, 23, 31).
The innate immune system has an extensive early sensing mechanism to immediately detect viral pathogens, alert neighboring cells to the presence of an invading virus, and initiate the expression of genes designed to limit virus replication and spread (reviewed in references 8, 15, and 19). Virus infection is first detected when viral RNA activates the cytoplasmic sensors RIG-I or MDA5 (termed the classical or cytosolic pathway) or when engulfed viral material within endosomes activates TLR-3, -7, -8, or -9 (the TLR pathway). Both pathways result in the activation via phosphorylation of the transcription factors interferon regulatory factor 3 (IRF-3), IRF-7, AP-1, and NF-κB. These transcription factors induce expression of alpha/beta interferon (IFN-α/β) and several other early antiviral genes (e.g., MDA-5, iNOS, ISG-15, ISG-54, ISG-56, RANTES, and interleukin-15). Secreted IFN-β acts in both an autocrine and a paracrine manner by binding to its specific receptor, which results in the expression of a large number of genes with antiviral activity (e.g., PKR, MxA, OAS, and ADAR, among others).
Ebola virus has developed several mechanisms to overcome the potent effects of the innate immune system, at least three of which are mediated via the VP35 protein. VP35 inhibits activation of both IRF-3 and protein kinase R and also serves as an RNA-silencing suppressor (2, 3, 7, 14). In addition to its role as an inhibitor of the innate immune system, VP35 has an essential role in virus transcription and replication. It functions as a cofactor for the viral polymerase and is an integral member of the ribonucleoprotein complex along with the NP, VP30, and L proteins (25). The present study focuses on the role of VP35-mediated IRF-3 inhibition on cellular antiviral gene expression.
Our previous studies identified an IRF-3 inhibitory domain within the C terminus of VP35 (18). Within VP35, mutation of arginine 312 to alanine (R312A) significantly abolished the ability of VP35 to inhibit IRF-3 phosphorylation but did not adversely affect the ability of VP35 to promote efficient replication and transcription (17). A recombinant infectious Ebola virus containing the R312A mutation within VP35 (recEbo-VP35/R312A) induced higher levels of IRF-3 phosphorylation (17) than a similar virus expressing wild-type (WT) VP35. In addition, a recombinant mouse-adapted Ebola virus containing the R312A mutation in VP35 was completely attenuated in mice (16). The present study uses microarray analysis to precisely examine global cellular gene expression induced by the recEbo-VP35/WT and recEbo-VP35/R312A viruses. We demonstrate that the WT virus is remarkably effective in suppressing the activation of many cellular antiviral and IFN gene expression pathways. The single R312A mutation in VP35 dramatically reverses that inhibition of antiviral gene activation. The results provide detailed evidence that VP35 plays a significant role in the inhibition of innate antiviral gene expression by Zaire ebolavirus.
MATERIALS AND METHODS
Cell culture.
Human hepatocellular carcinoma (HepG2) cells (ATCC HB-8065) were grown in complete Dulbecco modified Eagle medium (DMEM) supplemented with 0.1 mM nonessential amino acids. Complete DMEM is defined as DMEM containing 4,500 mg of glucose/liter, 2 mM l-glutamine and penicillin-streptomycin, 1.0 mM sodium pyruvate (all reagents obtained from Gibco, Invitrogen Corp., Carlsbad, CA) and, unless otherwise indicated, 10% fetal bovine serum (FBS; HyClone, Logan, UT). For virus propagation, Vero E6 cells were maintained in complete DMEM supplemented with 10% FBS.
Generation and purification of viruses.
The generation of recEbo-VP35/WT and recEbo-VP35/R312A viruses and a description of the backbone clone have been described previously (17, 30). First-passage stocks of both viruses were diluted 1:10 and propagated in Vero E6 cells. After significant cytopathic effect was evident, the supernatants were harvested and clarified by centrifugation (1,500 × g for 10 min). Polyethylene Glycol-8000 (PEG-8000) and NaCl were both added to the clarified supernatants to give final concentrations of 7.5% (wt/vol) and 0.5 M, respectively. The supernatants were incubated at 4°C for 4 h with periodic mixing to precipitate the virus. After precipitation, the viruses were pelleted by centrifugation at 10,000 × g for 30 min using a Beckman JA-20 rotor. The resulting pellets were resuspended in 2 ml of 1× TNE buffer (10 mM Tris, 150 mM NaCl, 1 mM EDTA [pH 7.4]). Pellets of the same virus stock were combined and incubated on ice overnight. The next day, the pellets were sonicated briefly to disrupt any aggregates. The viruses were then purified by ultracentrifugation through a 20 to 60% sucrose step gradient. The samples were subjected to ultracentrifugation in an SW28 rotor at 50,000 × g (19,000 rpm) for 2 h at 4°C. The visible band at the interface was collected and transferred to a new SW28 centrifuge tube. The virus was diluted with TNE buffer and centrifuged again at 50,000 × g for 2 h at 4°C. The pellets were resuspended in 3 ml of DMEM containing 10% FBS and incubated overnight on ice. The following day, the viruses were sonicated to disrupt aggregates, and a small amount was removed for titration by plaque assay. The concentrated, purified virus was stored in liquid nitrogen. For virus controls, half of each purified virus stock was inactivated by exposure to 5 × 106 rads of Cobalt-60 radiation from a Gammacell irradiator. All work with infectious virus was performed within positive-pressure suits within the biosafety level 4 laboratory at the Centers for Disease Control and Prevention (CDC; Atlanta, GA).
Infection of cells.
HepG2 cells were seeded in six-well plates (2 × 106 cells per well in 2 ml of complete DMEM). The following day, the cells were infected with the indicated viruses at a multiplicity of infection of 2. There were five conditions: recEbo-VP35/WT, recEbo-VP35/R312A, irradiated recEbo-VP35/WT, irradiated recEbo-VP35/R312A, and mock infected. After a 1-h adsorption period at 37°C, the inocula were removed, and each well was washed three times with phosphate-buffered saline (PBS). The cells were cultured for the designated length of time in 2 ml of DMEM containing 2% FBS. Samples were harvested in triplicate at 0, 6, 12, 24, and 48 h postinfection (hpi). At the time of harvest, each well was washed one time with PBS, and then 1 ml of Tripure reagent (Roche, Palo Alto, CA) was added, followed by incubation for 10 to 15 min to ensure complete lysis of the cells before transfer to an Eppendorf tube. RNA was extracted by using RNA matrix solution (Qbiogene, Irvine, CA) and standard protocols.
Q-RT-PCR assay for Zaire ebolavirus.
Quantitative reverse transcription-PCR (Q-RT-PCR) to detect RNA from Zaire ebolavirus, as well as generation of in vitro transcripts for use as a standard curve, was performed as described previously (32). The standard curves generated from the amplification plot of a 10-fold serial dilution of transcripts showed a linear correlation between the CT values and the initial RNA load over a 5-log range (R2 > 0.99). No amplification was detected in the negative control.
Microarray.
Total RNA (500 ng) was amplified in a single-round of in vitro transcription amplification that allowed incorporation of biotin-labeled nucleotides using the Illumina TotalPrep RNA amplification kit (Ambion, Inc., Austin, TX) according to the manufacturer's instructions. cRNA (850 ng) of each sample was hybridized to an Illumina HumanRef-8 V1BeadChip (containing probes to 23,961 RefSeq gene sequences) at 55°C for 18 h according to the manufacturer's instructions (Illumina, Inc., San Diego, CA). This was followed by washing, blocking, and streptavadin-Cy3 staining steps, followed by scanning with a high-resolution Illumina bead array reader confocal scanner, all carried out according to the manufacturer's instructions. For every array at all time points, a rigorous quality check was carried out to ensure good performance before the array data were extracted. The data extraction was performed by using Illumina Bead Studio software and then uploaded into GeneSpring GX7.3 (Silicon Genetics, Redwood City, CA) software for downstream analysis.
Array normalization.
We followed the standard normalization procedures recommend by the GeneSpring software for one-color array data. In brief, data transformation was corrected for a low signal, with values recorded at <0.01 increased to the minimum (0.01). Per-chip (mean) normalization accounted for chip variability by dividing all of the measurements on each chip by a 50th percentile value. Per-gene normalization accounted for variability between probe sets for different genes. Genes that were not confidently detected in at least two samples were excluded from future analysis, leaving about 12,600 genes available for differential expression.
Selection of differentially expressed genes from microarray data.
Differentially expressed genes were selected from the normalized data by using a procedure known as significance analysis of microarrays (SAM) (33), as installed in GeneSpring GXV7.3 software. In brief, the statistic used in SAM is given as d = (μ1 − μ2)/(s − s0), where the numerator is the group mean difference, s is the standard error, and s0 is a regularizing constant. Setting s0 = 0 will yield a t-statistic. This value, called the fudge constant, is found by removing the trend in d as a function of s in moving windows across the data to reduce false-positive results (33). Since the statistic is not t-distributed, significance is computed by using a permutation test. Genes with a computed statistic larger than the threshold are called significant. The false discovery rate associated with the given threshold can also be calculated from the permutation data. To select differentially expressed genes, a SAM cutoff of 10%, with an additional filter of a minimum twofold difference in expression between groups, together with a minimum detection threshold in the positive-expressing group, was used.
TaqMan low-density array (TLDA).
Total RNA (2ul) was reverse transcribed by using a high-capacity cDNA archive kit (Applied Biosystems, Foster City, CA). The reverse transcriptase reaction was performed at 25°C for 10 min and then 37°C for 2 h, followed by 85°C for 5 s. cDNA converted from 0.1 μg of RNA was resuspended in 50 μl of buffer was added to 50 μl of TaqMan Universal Master Mix (2X; Applied Biosystems) and then immediately loaded into a Micro Fluidic card (3M Company; Applied Biosystems). The card was spun twice at 1,200 rpm for 1 min each time to distribute the PCR mix into the wells of the card before it was sealed and loaded into the ABI 7900HT sequence detection system. Default thermal cycling conditions were used (50°C for 2 min with 100% ramping, 94.5°C for 10 min with 100% ramping, and finally 40 cycles of 97°C for 30 s with 50% ramping and 59.7°C for 1 min with 100% ramping), and data were analyzed by using SDS2.2 software (Applied Biosystems). The data were imported into in GeneSpring GXV 7.3, and an analysis of variance t test (assuming unequal variances) was run on the data to selected differently expressed genes.
Gene ontology clustering.
SAM-generated differentially expressed gene lists were analyzed for gene ontology information by using Ingenuity Pathways analysis software (Ingenuity Systems), which looks for both known canonical pathways and networks of genes. The canonical pathways are described in the library of the Ingenuity Pathways knowledge base and are based on well-known established textbook literature where molecular links are known. The networks are built from a compilation of literature searches. The connecting lines in the network diagrams may be one or many publications implying a connection between the genes. The Ingenuity program is updated monthly to reflect new publications.
Selection of genes was based on a statistical ranking approach. For canonical pathways, the significance of the association was measured in two ways: (i) by the ratio of the number of genes from the data set that map to the pathway divided by the total number of genes in that pathway and (ii) by using the Fisher exact test to calculate a P value determining the probability that the association between the genes in the data set and the canonical pathway is explained by chance alone. For the networks, Ingenuity Pathways analysis computes a score for each network according to the fit of the user's set of significant genes. The score is derived from the likelihood that the focus genes in a network are together due to chance alone. A score of 2 is equivalent to a P value of 0.01.
For the network generation, the SAM list containing gene identifiers and corresponding expression values was uploaded into in the application and overlaid onto a global molecular network developed from information contained in the Ingenuity Pathways knowledge base, which then displays the best-fit network of 35 genes and/or proteins. Networks of these focus genes were then algorithmically generated based on their connectivity. A network is a graphical representation of the molecular relationships between genes or gene products. Genes or gene products are represented as nodes, and the biological relationship between two nodes is represented as an edge (line). All edges are supported by at least one reference from the literature, from a textbook, or from canonical information stored in the Ingenuity Pathways knowledge base. The intensity of the node color indicates the degree of up (red)- or down (green)-regulation. Nodes are displayed using various shapes that represent the functional class of the gene product. Edges are displayed with various lines that describe the nature of the relationship between the nodes.
RESULTS
Our previous studies had shown that an R312A amino acid change in VP35 resulted in a virus that no longer efficiently inhibits phosphorylation of the transcription factor IRF-3 but was still able to promote efficient viral transcription and replication (17). To more precisely examine the role of this domain within VP35 in blocking host innate antiviral response pathways, a microarray analysis was initiated to compare global gene expression induced in liver cells by infection with reverse genetics generated Ebola viruses encoding WT (recEbo-VP35/WT) or mutant (recEbo-VP35/R312A) VP35 proteins.
The human liver hepatocyte cell line HepG2 was chosen for these studies because viral infection of the liver plays a prominent role in Ebola virus infections. Severe virus-induced necrosis of the liver is a hallmark of both human and animal models of Ebola hemorrhagic fever, and extremely high viral loads are found in the livers of experimentally infected animals (4, 10, 11). HepG2 cells are highly susceptible to Ebola virus infection, with ca. 80% of the cells infected by 48 hpi (data not shown).
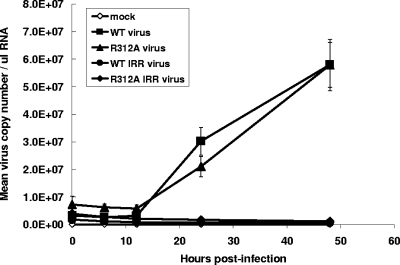
The R312A mutant and WT viruses were generated entirely from plasmids by reverse genetics (17). HepG2 cells were infected with WT, R312A mutant, the corresponding gamma-irradiated (IR) versions of these two viruses (inactivated controls), or media only (uninfected control). Total cellular RNA was harvested in triplicate at several time points postinfection for microarray analysis. Virus replication was seen in lysates of cells infected with either the WT or the R312A viruses by 24 and 48 hpi as detected by Q-RT-PCR (Fig. 1), and results were similar when the cell supernatant was tested (data not shown).
FIG. 1.
Replication of Ebola virus in HepG2 cells. Total cellular RNA was extracted from HepG2 cells at 0, 6, 12, 24, and 48 hpi. Q-RT-PCR was performed using primers and probe specific for the NP gene of Zaire ebolavirus (32). A standard curve was generated using in vitro transcripts and used to determine the mean virus copy number per microliter of sample. Each data point represents the average of three biological and two technical replicates. Standard deviation bars are shown for the WT and recEbo-VP35/R312A mutant virus samples.
For microarray analysis, we utilized the Illumina HumanRef-8 V1BeadChip, which contains more than 23,000 genes. The SAM procedure was used to determine differentially expressed genes from the normalized data (see Materials and Methods) (33). No significant gene expression differences were seen at the early time points (data not shown). Significantly differentially expressed genes were not detected before 48 hpi, which was similar to findings of Kash et al. in an earlier microarray analysis of WT Zaire ebolavirus infections (20).
In our initial experiments, HepG2 cells were infected using supernatant medium harvested from virus-infected cell monolayers as the inoculum. This is a common method of infection and was the method used in the earlier microarray analysis of WT Zaire ebolavirus infections (20). This early study by Kash et al. demonstrated that numerous cellular genes were downregulated in Ebola virus-infected cells relative to mock-infected cells. Our initial comparison of WT-infected cells to mock-infected cells yielded similar results, with Ebola virus infection appearing to downregulate numerous cellular genes. However, we failed to observe reproducible clear-cut gene expression differences between infectious virus and identically prepared IR noninfectious control virus, or between our WT Ebola virus and the R312A VP35 mutant virus using these infection conditions (data not shown). This raised the concern that cytokines and chemokines present in conditioned media used as the inoculum may be making a major contribution to the cellular responses being measured by ourselves and others in these sorts of microarray experiments. In order to ensure that the differences observed were strictly in response to virus infection, we gradient purified our virus stocks prior to their use as an inoculum to initiate infections. Purification of virus stocks by banding on sucrose gradients should effectively remove cytokines and other secreted active molecules that may have been present within infected cell culture supernatants.
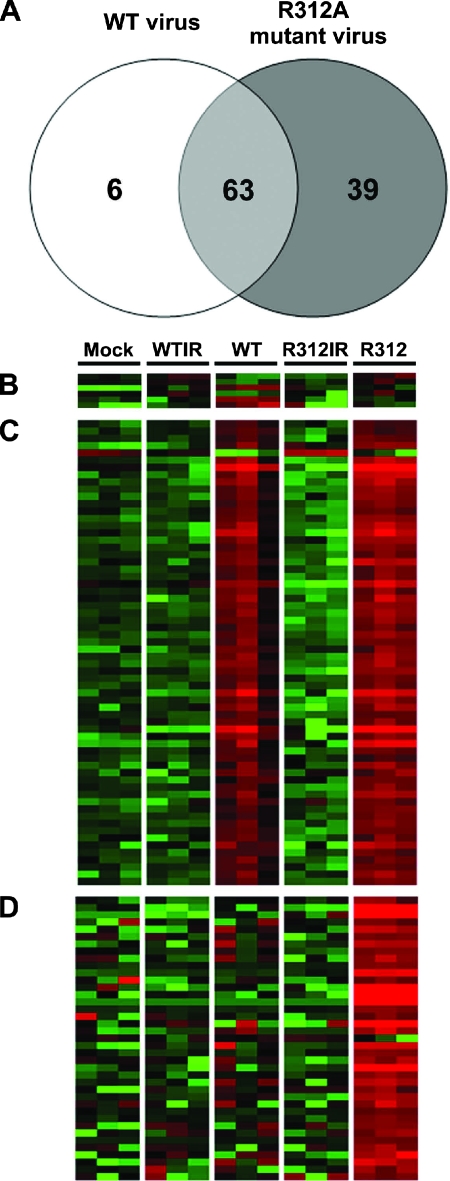
Ebola virus infections initiated with purified virus yielded strikingly different results on microarray analysis. Under these conditions, only a total of 108 genes were found to be significantly differentially expressed at 48 hpi (Fig. 2A). Six genes were uniquely expressed in WT-infected cells compared to all other conditions (Fig. 2B and see Table S1 in the supplemental material), 63 genes were differentially expressed in cells infected with both the WT and R312A viruses compared to their irradiated controls and mock-infected cells (Fig. 2C and see Table S2 in the supplemental material), and 39 genes were uniquely expressed in cells infected with the R312A mutant virus compared to all other conditions (Fig. 2D and see Table S3 in the supplemental material).
FIG. 2.
Differential gene expression determined by microarray. (A) Venn diagram representing the 108 genes that were significantly differentially expressed when either the recEbo-VP35/WT or recEbo-VP35/R312A viruses were compared to the irradiated and mock-infected controls. For a complete listing of all 108 genes, see Tables S1 to S3 in the supplemental material. (B) Heat map of six genes unique to cells infected with recEbo-VP35/WT virus. (C) Heat map of the 63 genes differentially expressed in cells infected with both the recEbo-VP35/WT and the recEbo-VP35/R312A viruses. (D) Heat map of the 39 genes unique to cells infected with the recEbo-VP35/R312A virus. Each sample was run in triplicate, which is represented by the three columns. Red represents an increase in gene expression compared to uninfected controls, while green represents a decrease.
Ebola virus activates genes related to RNA processing and the hematological system.
To gain insight into the effect of Ebola virus infection on cellular gene expression in general, we performed gene ontology analysis on the 63 genes (Fig. 2A) that were differentially expressed in cells infected with both the WT and R312A viruses (Fig. 2C and see Table S2 in the supplemental material). Using the Ingenuity Pathways analysis software, the 63 genes were analyzed for known “canonical” pathways with selection based on a statistical ranking approach (see Materials and Methods). Pathway analysis revealed that death receptor signaling was the top canonical pathway (P = 4.25 × 10−3; ratio, 2/62 [data not shown]), with the genes TANK and caspase-6 pointing to the activation of this process.
We also performed Ingenuity Pathway network analysis, and the results revealed that the two top networks were “RNA posttranscriptional modification” and “hematological system development and function” (Fig. 3). Both networks scored 29 (scores of >3 are considered significant [P < 0.001]) with 13 genes identified in each network. Network diagrams showing the known interactions between these two groups of genes are shown in Fig. 3. Since this group of genes was identified by both the WT and the R312A viruses (two independent experiments with three replicates each), the confidence that these gene differences are real is high. The six genes uniquely expressed in cells infected with WT virus compared to all other conditions (Fig. 2B and see Table S1 in the supplemental material) did not have a significant pathway or network association.
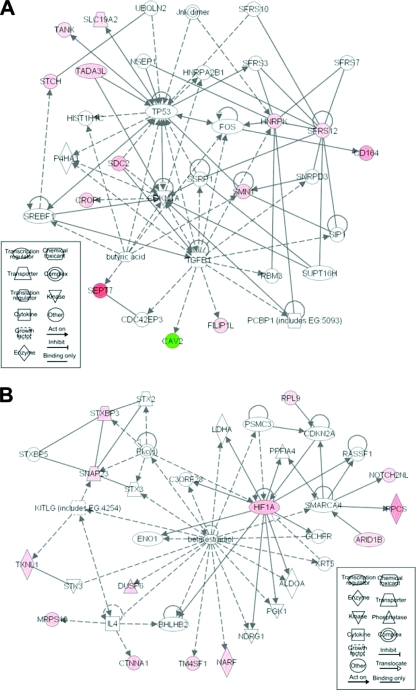
FIG. 3.
Gene networks identified in both recEbo-VP35/WT- and recEbo-VP35/R312A-infected cells compared to mock-infected and irradiated controls. The networks of genes related to RNA posttranscriptional modification (A) and hematological system development and function (B) are shown. The networks were generated from Ingenuity Pathways analysis. The lines in between genes represent known interactions, with solid lines representing direct interactions and dashed lines representing indirect interactions. Red shading indicates an increase in gene expression, and green indicates a decrease in gene expression compared to uninfected controls. The intensity of shading is proportional to the fold difference in gene expression. An explanation of gene names and synonyms can be found in Table S2 in the supplemental material. Network pathway images were created by using Ingenuity Systems software.
The recEbo-VP35/R312A mutant virus is defective in controlling innate antiviral gene expression.
Of the genes upregulated by WT virus infection, none were related to the IFN or antiviral system. This suppression of antiviral gene expression was dramatically reversed by the presence of the single R312A mutation in the IRF-3 inhibitory domain of VP35. Of the 39 genes uniquely expressed in R312A mutant virus-infected cells, many were related to innate antiviral immunity, including MDA-5, RANTES, ISG-15, ISG-54, ISG-56, STAT1, IRF-9, OAS, and MX1 (Table 1). A full description of the 39 genes (Fig. 2D) differentially expressed in cells infected with R312A virus compared to all other conditions can be found in Table S3 in the supplemental material.
TABLE 1.
Summary of microarray and TLDA results showing fold increases in gene expression after infection with the recEbo-VP35/R312A virus
| Accession no. | Symbol | Synonym | Fold increase in gene expressiona |
|||||
|---|---|---|---|---|---|---|---|---|
| R312A vs R312A IR |
R312A vs WT |
R312A vs mock |
||||||
| Array | TaqMan | Array | TaqMan | Array | TaqMan | |||
| NM_022168 | IFIH1 | MDA-5 | 2.8 | 2.8 | 2.9 | 3.4 | 3 | 3.8 |
| NM_002985 | CCL5 | RANTES | 248 | 47 | 114 | 73 | 22 | 36 |
| NM_002038 | G1P3 | IFI6 | 5.1 | 7 | 5.9 | 5.6 | 6.9 | 5.3 |
| NM_005101 | G1P2 | ISG-15 | 3.1 | 3.3 | 2.9 | 2.7 | 3.1 | 3.3 |
| NM_001547 | IFIT2 | ISG-54 | 3,038 | 295 | 3,038 | 82 | 3,038 | 168 |
| NM_001548 | IFIT1 | ISG-56 | 18.6 | 7.2 | 16.7 | 5.5 | 21.3 | 5.2 |
| NM_139266 | ISGF3 | STAT1 | 2.5 | 2 | 2.5 | 1.6 | 2.7 | |
| NM_006084 | ISGF3G | IRF-9 | 2.7 | 3.4 | 3.3 | 3.5 | 3.3 | 3.3 |
| NM_002534 | OAS1 | OAS | 2.8 | 4.2 | 2.7 | 3.9 | 4 | 2.9 |
| NM_002462 | Mx1 | Mx1 | 9.9 | 4.5 | 39.4 | 4.2 | 9.7 | 3.6 |
| NM_016323 | HERC5 | CEBP1 | 60 | 55 | 89 | 67 | 3,006 | 59 |
| NM_173468 | MOBKL1A | MOB1 | 6.7 | 0.7 | 2.1 | 0.7 | 2.3 | |
| NM_033405 | PRIC285 | PRIC285 | 2.6 | 2.6 | 2.5 | 2.4 | 2.3 | 2.9 |
| NM_005132 | REC8L1 | REC8 | 3.1 | 3.4 | 2.9 | 2.4 | 2.6 | 3.3 |
| NM_000422 | KRT17 | KRT17 | 18.8 | 21 | 13.7 | 4 | 178.5 | 17 |
| NM_002982 | CCL2 | MCP-1 | 108 | 108 | 108 | |||
| NM_014314 | DDX58 | RIG-I | 1.9 | 1.9 | ||||
| NM_001549 | IFIT3 | ISG60 | 7.7 | 8 | 5.1 | |||
All fold increases were statistically significant (P < 0.05).
These 39 genes were analyzed for known canonical pathways by using Ingenuity Pathways analysis, and the results were very clear. IFN signaling was the only significant canonical pathway affected (P = 1.11 × 10−10; ratio, 5:29 [data not shown]). Clearly, the IFN pathway is activated in cells infected with the R312A mutant virus, whereas this pathway remains remarkably inhibited in WT-virus-infected cells despite evidence of virus replication in cells infected with the WT virus (Fig. 1). In fact, the absence of expression of these 39 genes in WT-infected cells was strikingly similar to mock-infected cells, as well as to cells infected with inactivated virus, indicating that the WT virus was able to completely shut off expression of these genes.
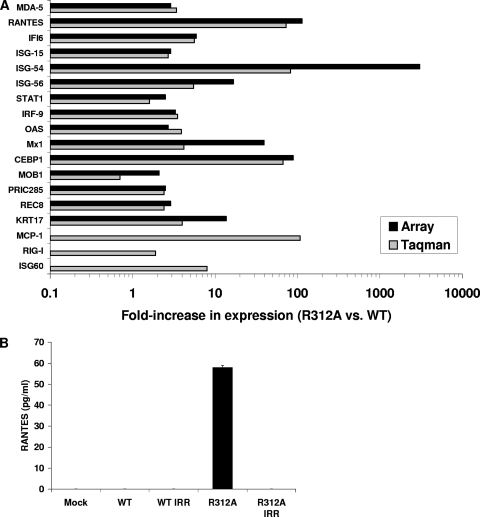
The finding that the R312A mutant virus failed to suppress the IFN pathway, including genes known to be members of the innate antiviral pathways, led us to investigate this pathway further. We constructed a TLDA card to specifically look at this pathway in more detail and to confirm the microarray results. TLDA analysis revealed that the antiviral and chemokine genes were highly significant (Fig. 4A). The fold increases in gene expression found by microarray were very similar when the same RNA sample was tested by TLDA analysis (Fig. 4A). Three additional genes (MCP-1, RIG-I, and ISG-60), chosen for TLDA analysis based on Ingenuity Pathway analysis of the microarray results, were also highly significantly increased in R312A virus-infected cells compared to WT-infected cells. Direct comparisons of the fold increases in the expression of these 18 genes between the R312A virus-infected cells and the other three conditions (WT, R312A IR, and mock) can be found in Table 1. Because there was an absence of expression of this set of genes in the mock, WT, and irradiated wells, differences in gene expression compared to R312A mutant virus were consistent irrespective of how the groups were compared.
FIG. 4.
Confirmation of microarray results by TLDA and ELISA. (A) IFN and antiviral-related genes that showed a significant increase in expression in cells infected with recEbo-VP35/R312A virus compared to cells infected with recEbo-VP35/WT virus were subjected to TLDA analysis. Three additional genes chosen for analysis include MCP-1 (CCL2), RIG-I, ISG-60. Shown are the fold increases in expression (recEbo-VP35/R312A mutant virus versus recEbo-VP35/WT virus) of the indicated genes for both microarray (▪) and Taqman (░⃞) at 48 hpi. Explanation of gene names and synonyms can be found in Table S3 in the supplemental material. (B) Supernatants collected at 48 hpi were tested for secreted RANTES (CCL5) by ELISA. Secreted RANTES in mock-infected cells and in cells infected with WT, WT IR, or R312A IR viruses were all below the limit of detection of the ELISA (3 pg/ml).
The chemokine RANTES (CCL5) was strongly induced in cells infected with the R312A virus compared to the other conditions. High levels of RANTES protein were detected in supernatants from R312A virus-infected cells by enzyme-linked immunosorbent assay (ELISA) (Fig. 4B). RANTES was undetectable in mock, WT-, WT IR-, or R312A IR virus-infected cells. Therefore, the differences in gene induction at the RNA level resulted in actual measurable differences in protein expression.
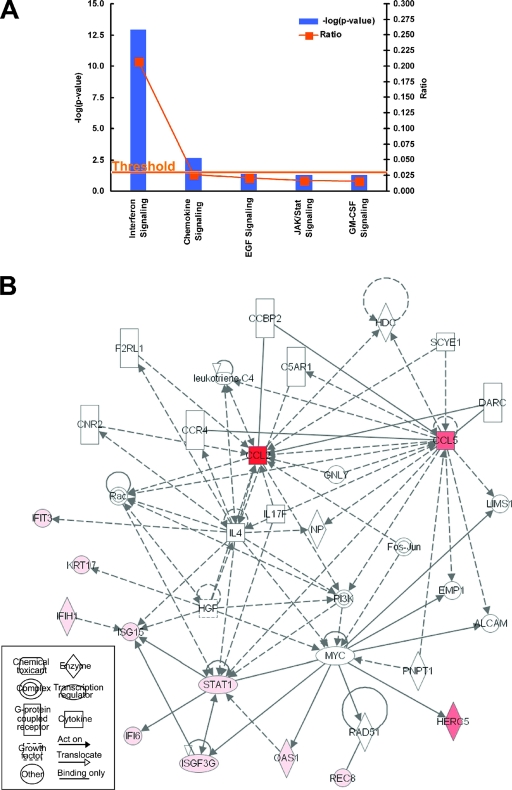
The genes found in Table 1 were analyzed by using Ingenuity Pathway analysis, and the top canonical pathway was still IFN signaling, which had now increased in significance (P = 1.42 × 10−13; ratio 6/29) (Fig. 5A). The chemokine signaling pathway was also significant (P = 3.32 × 10−3; ratio, 2/81). Network analysis revealed known interactions between the identified genes, with STAT1, RANTES, and MCP-1 forming the most central players in the affected network (Fig. 5B).
FIG. 5.
Ingenuity Pathways analysis of differentially regulated genes after infection with recEbo-VP35/R312A virus. (A) The 18 significant genes identified by both microarray and TLDA were used for canonical pathway analysis. Blue bars represent various canonical pathways, and the height of the bar represents the P value. Yellow boxes represent the ratio of genes in the list relative to the total number of genes in the pathway. The yellow line indicates the threshold of significance. (B) Network of genes in both the IFN and chemokine signaling pathways that were found to be differentially expressed in recEbo-VP35/R312A virus-infected cells compared to recEbo-VP35/WT virus-infected cells. The lines in between genes represent known interactions, with solid lines representing direct interactions and dashed lines representing indirect interactions. Red shading indicates an increase in gene expression, and green indicates a decrease in gene expression compared to the controls. The intensity of shading is proportional to the fold difference in gene expression. An explanation of gene names and synonyms can be found in Table S3 in the supplemental material. Network pathway images were created by using Ingenuity Systems software.
DISCUSSION
Microarray technology has the advantage of allowing simultaneous analysis of the expression of thousands of genes in a sample. The breadth and sensitivity of the analysis allows identification of pathways affected and cascades of gene expression alterations that would be impossible to achieve by other methods. However, data generated by such approaches can be subject to misinterpretation unless rigorous experimental design and statistical analysis are applied. Here, our experimental design involved three replicate samples at each time point for each infection condition, including inactivated virus controls. This level of sampling allowed rigorous statistical analysis and array normalization such that genes not confidently detected in at least two samples were excluded from further analysis. In addition to stringent statistical cutoffs, we aimed to further maximize signal to noise by examining gene expression differences induced by infection with two recombinant Ebola viruses differing by only a single amino acid within VP35. Both viruses were generated by reverse genetics, and therefore their sequence is precisely defined and identical to each other with the exception of the single nucleotide change. This design allowed us to eliminate extrinsic variables and precisely assess the effect of the single amino acid change.
Despite this rigorous experimental design and statistical analysis, our initial experiments yielded data that did not accurately reflect gene expression differences related to virus infection. We found that when we utilized infected cell supernatant as the virus inoculum, the gene expression pattern observed did not result from virus infection but presumably was in response to chemokines and cytokines present in the conditioned supernatant. This initial comparison of WT-infected cells with mock-infected cells yielded results similar to those from an earlier study (also initiated with virus-infected cell supernatant), which demonstrated that WT Ebola virus infection appeared to downregulate numerous cellular genes (20). However, we failed to observe reproducible clear-cut gene expression differences between infectious viruses and identically prepared IR noninfectious control viruses or between our WT Ebola virus and the R312A mutant virus. Removal of extraneous material from the virus inoculum by purification of virus by ultracentrifugation gave strikingly different gene expression responses.
When using purified virus preparations, we found that WT Ebola virus was remarkably efficient at inhibiting the expression of IFN, antiviral, and chemokine genes. There were few differences seen between gene expression patterns for cells infected with infectious WT virus, inactivated WT virus, or inactivated mutant virus or for mock-infected cells. However, in sharp contrast, the single amino acid change of R312A within the IRF-3 inhibitory domain of VP35 resulted in infectious virus that induced a robust innate antiviral immune response. These results illustrate the importance of purifying virus prior to infecting cells for the analysis of cellular responses to infection by sensitive methods such as microarray analysis. Other investigators have recently followed similar protocols for virus purification prior to microarray analysis (24).
Gene expression differences observed only in cells infected with the R312A mutant virus alone gave insight into the genes controlled by the IRF-3 inhibitory domain of VP35. Based on our previous findings (17), we hypothesized that the R312A mutant virus would be unable to control IRF-3-responsive gene expression. Our recent work highlighted the importance of this single amino acid change for viral pathogenicity because infection of mice with a mouse-adapted version of this virus resulted in complete attenuation (16).
Both microarray and TaqMan analysis confirmed our hypothesis and revealed that a number of genes within the IRF-3 and IFN pathways are upregulated by infection with the R312A virus compared to the WT. Cells infected with the R312A virus, unlike cells infected with the WT virus, showed increased expression of genes known to be directly transactivated by IRF-3, including MDA-5, RANTES (CCL5), ISG-15, ISG-54, ISG-56, ISG-60, and OAS (12, 34). The finding that both RANTES and ISG-56 are activated in cells infected with R312A virus compared to the WT virus supports the use of both genes as markers for IRF-3 activation (17, 18). In addition, there was significantly more secreted RANTES protein in cell culture supernatants from recEbo-VP35/R312A virus-infected samples compared to WT and controls. This serves as a critical verification that the differences in gene expression at the RNA level translate to measurable differences in protein expression levels.
Other cytokine and ISGs were found to be significantly upregulated in cells infected with R312A virus and include RIG-I, MCP-1 (CCL2), STAT1, IRF-9, and Mx1. Although these genes are not known to be directly regulated by IRF-3, it is likely that activation of IRF-3 in these cells leads to increased expression of these other cytokines and antiviral-related genes due to the overlapping nature and autocrine/paracrine amplification of the antiviral system. The results presented here are remarkable in that the tight control of gene expression exhibited by the WT virus is dramatically reversed by the single amino acid change in VP35.
Pathway analysis using Ingenuity Systems software indicated that both the IFN and cytokine pathways were significantly activated in cells infected with R312A virus compared to WT virus, with the IFN pathway being particularly highly statistically significant. The most central players according to the Ingenuity Pathways network diagram are STAT1, RANTES (CCL5), and MCP-1 (CCL2), in that these three proteins have the most known interactions with each other and the other proteins within the pathway. STAT1 is a critical transcription factor involved in signaling from the IFN receptors. RANTES (CCL5) and MCP-1 (CCL2) are important chemokines that recruit and activate leukocytes that are critical in the development of adaptive immunity. The fact that the WT virus can effectively inhibit expression of these three genes implies that authentic WT Ebola virus inhibits not only IFN and antiviral gene expression but also the recruitment and activation of critical immune cells required for mounting effective antibody responses. Indeed, fatal cases of Ebola virus infection are associated with a lack of virus-specific humoral responses (1, 22, 23, 31).
Both MDA-5 and RIG-1, the two RNA helicases that act as cytosolic sensor molecules, were significantly induced by infection with R312A virus compared to the WT virus. Both molecules are constitutively expressed and act as sentinels in the cytosol that signal through IPS-1/MAVS/VISA/Cardif and lead to activation of IRF-3 and other transcription factors (19). Expression of MDA-5 and RIG-1 is then amplified in response to viral infection in a positive feedback loop. MDA-5 has been shown to be directly upregulated by IRF-3, whereas RIG-1 upregulation requires IFN-α/β signaling (34). Based on the data presented here, WT Ebola virus effectively prevents increased expression of these two important sensor molecules, which likely averts further amplification of the IFN system and activation of innate immunity.
Interestingly, both IRF-9 and STAT1 were upregulated in cells infected with R312A virus compared to WT virus. IRF-9 and STAT1 are members of the transcriptional activator ISGF3, which plays a critical role in IFN signaling and amplification of the antiviral response through the induction of IRF-7 (19). That these two genes are expressed at high levels in R312A virus-infected cells provides supporting evidence that the virus is unable to suppress the innate antiviral pathway in these cells. Conversely, the WT virus efficiently prevents expression of both of these genes and hence prevents amplification of the antiviral response.
Insight into how Ebola virus affects general cellular gene expression can be gleaned from the set of genes that are regulated after infection by both the WT and the R312A mutant Ebola viruses. Since this set of genes was significant in both WT and mutant virus-infected cells, confidence that these gene expression alterations are real is high. Analysis indicated that this set of genes includes those involved in death receptor signaling, RNA posttranscriptional modification, and hematological system development and function. The death receptor signaling genes (TANK and caspase-6) may contribute to the significant amount of cell apoptosis that is seen in Ebola virus-infected humans and animal models (1, 9, 10, 13) and suggest that hepatocytes themselves may undergo apoptosis as a direct or indirect consequence of infection. The fact that both viruses induce expression of a number of genes related to RNA processing and modification suggests that the virus modifies the host RNA machinery to promote efficient viral transcription and replication. Finally, both viruses affect genes related to hematological system development and function, suggesting that virus manipulation of these genes may contribute to the lymphopenia, thrombocytopenia, and neutrophilia seen during Ebola virus infection (5, 26, 29). These three networks may form the bridge between viral replication and consequent host damage and disease. These results provide a roadmap for further investigation into the effects of Ebola infection on host cell processes.
Other studies have been done to look at gene expression by microarray after Ebola virus infection. Rubins et al. analyzed temporal gene expression in the peripheral blood of nonhuman primates infected with Ebola virus (27). Very little IFN and antiviral gene expression is seen for the first 2 to 3 days postinfection. This is consistent with our results and suggests innate antiviral immunity is suppressed during the critical time that the virus is seeding many organs, including the liver and spleen (10). From 4 days postinfection onward, virus titers in blood and organs are extremely high (10), and expression of antiviral genes is seen (27) but is likely ineffective due to the overwhelming amount of viral replication. Unlike our present study, however, Rubins et al. analyzed a mixed population of cells (peripheral blood mononuclear cells), and thus direct comparisons between the two studies are difficult to interpret.
Because Ebola virus has multiple immune subversion mechanisms, the relative contribution of each mechanism to pathogenesis is difficult to assess. However, reverse genetics allows assessment of individual amino acid changes in the context of live virus infection. Here, we demonstrated that the single R312A mutation in VP35 leads to the activation of IFN, antiviral, and cytokine signaling pathways. In this context, amino acid R312 of VP35 appears to be critical for controlling this powerful host response. Based on these findings, as well as our previous results (16, 17), inhibition of IRF-3 phosphorylation is most likely the predominant mechanism contributing to these results. However, given that the R312A mutation in VP35 also disrupts RNA-silencing suppressor function (14) and RNA binding (6), we cannot rule out the additive effect of both mechanisms on these results. Single point mutations such as this can reveal precise host control mechanisms of the virus. The results from the present study provide detailed evidence that VP35 plays a significant role in the inhibition of innate antiviral gene expression by Zaire ebolavirus. The present study also provides an explanation underlying our recent finding that a mouse-adapted version of the recEbo-VP35/R312A mutant virus is completely attenuated in mice (16). Taken together, VP35 from Ebola virus appears to be a major viral virulence factor and contributor to the rapid disease progression seen in Ebola virus-infected patients.
Supplementary Material
Acknowledgments
We acknowledge Tara Sealy (Special Pathogens Branch, CDC) for technical assistance and Tom Ksiazek (Special Pathogens Branch, CDC) for support.
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the funding agency.
Footnotes
Published ahead of print on 19 March 2008.
Supplemental material for this article may be found at http://jvi.asm.org/.
REFERENCES
- 1.Baize, S., E. M. Leroy, M. C. Georges-Courbot, M. Capron, J. Lansoud-Soukate, P. Debre, S. P. Fisher-Hoch, J. B. McCormick, and A. J. Georges. 1999. Defective humoral responses and extensive intravascular apoptosis are associated with fatal outcome in Ebola virus-infected patients. Nat. Med. 5:423-426. [DOI] [PubMed] [Google Scholar]
- 2.Basler, C. F., A. Mikulasova, L. Martinez-Sobrido, J. Paragas, E. Muhlberger, M. Bray, H. D. Klenk, P. Palese, and A. Garcia-Sastre. 2003. The Ebola virus VP35 protein inhibits activation of interferon regulatory factor 3. J. Virol. 77:7945-7956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Basler, C. F., X. Wang, E. Muhlberger, V. Volchkov, J. Paragas, H. D. Klenk, A. Garcia-Sastre, and P. Palese. 2000. The Ebola virus VP35 protein functions as a type I IFN antagonist. Proc. Natl. Acad. Sci. USA 97:12289-12294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bray, M., K. Davis, T. Geisbert, C. Schmaljohn, and J. Huggins. 1998. A mouse model for evaluation of prophylaxis and therapy of Ebola hemorrhagic fever. J. Infect. Dis. 178:651-661. [DOI] [PubMed] [Google Scholar]
- 5.Bray, M., S. Hatfill, L. Hensley, and J. W. Huggins. 2001. Hematological, biochemical, and coagulation changes in mice, guinea-pigs and monkeys infected with a mouse-adapted variant of Ebola Zaire virus. J. Comp. Pathol. 125:243-253. [DOI] [PubMed] [Google Scholar]
- 6.Cardenas, W. B., Y. M. Loo, M. Gale, Jr., A. L. Hartman, C. R. Kimberlin, L. Martinez-Sobrido, E. O. Saphire, and C. F. Basler. 2006. Ebola virus VP35 protein binds double-stranded RNA and inhibits alpha/beta interferon production induced by RIG-I signaling. J. Virol. 80:5168-5178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Feng, Z., M. Cerveny, Z. Yan, and B. He. 2007. The VP35 protein of Ebola virus inhibits the antiviral effect mediated by double-stranded RNA-dependent protein kinase PKR. J. Virol. 81:182-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garcia-Sastre, A., and C. A. Biron. 2006. Type 1 interferons and the virus-host relationship: a lesson in detente. Science 312:879-882. [DOI] [PubMed] [Google Scholar]
- 9.Geisbert, T. W., L. E. Hensley, T. R. Gibb, K. E. Steele, N. K. Jaax, and P. B. Jahrling. 2000. Apoptosis induced in vitro and in vivo during infection by Ebola and Marburg viruses. Lab. Investig. 80:171-186. [DOI] [PubMed] [Google Scholar]
- 10.Geisbert, T. W., L. E. Hensley, T. Larsen, H. A. Young, D. S. Reed, J. B. Geisbert, D. P. Scott, E. Kagan, P. B. Jahrling, and K. J. Davis. 2003. Pathogenesis of Ebola hemorrhagic fever in cynomolgus macaques: evidence that dendritic cells are early and sustained targets of infection. Am. J. Pathol. 163:2347-2370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gibb, T. R., M. Bray, T. W. Geisbert, K. E. Steele, W. M. Kell, K. J. Davis, and N. K. Jaax. 2001. Pathogenesis of experimental Ebola Zaire virus infection in BALB/c mice. J. Comp. Pathol. 125:233-242. [DOI] [PubMed] [Google Scholar]
- 12.Grandvaux, N., M. J. Servant, B. tenOever, G. C. Sen, S. Balachandran, G. N. Barber, R. Lin, and J. Hiscott. 2002. Transcriptional profiling of interferon regulatory factor 3 target genes: direct involvement in the regulation of interferon-stimulated genes. J. Virol. 76:5532-5539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gupta, M., C. Spiropoulou, and P. E. Rollin. 2007. Ebola virus infection of human PBMC causes massive death of macrophages, CD4 and CD8 T-cell sub-populations in vitro. Virology 364:45-54. [DOI] [PubMed] [Google Scholar]
- 14.Haasnoot, J., W. de Vries, E. J. Geutjes, M. Prins, P. de Haan, and B. Berkhout. 2007. The Ebola virus VP35 protein is a suppressor of RNA silencing. PLoS Pathog. 3:e86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haller, O., G. Kochs, and F. Weber. 2006. The interferon response circuit: induction and suppression by pathogenic viruses. Virology 344:119-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hartman, A. L., B. H. Bird, J. S. Towner, Z. Antoniadou, S. R. Zaki, and S. T. Nichol. 2008. Inhibition of IRF-3 activation by VP35 is critical for the high virulence of Ebola virus. J. Virol. 82:2699-2704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hartman, A. L., J. E. Dover, J. S. Towner, and S. T. Nichol. 2006. Reverse genetic generation of recombinant Zaire Ebola viruses containing disrupted IRF-3 inhibitory domains results in attenuated virus growth in vitro and higher levels of IRF-3 activation without inhibiting viral transcription or replication. J. Virol. 80:6430-6440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hartman, A. L., J. S. Towner, and S. T. Nichol. 2004. A C-terminal basic amino acid motif of Zaire ebolavirus VP35 is essential for type I interferon antagonism and displays high identity with the RNA-binding domain of another interferon antagonist, the NS1 protein of influenza A virus. Virology 328:177-184. [DOI] [PubMed] [Google Scholar]
- 19.Honda, K., and T. Taniguchi. 2006. IRFs: master regulators of signalling by Toll-like receptors and cytosolic pattern-recognition receptors. Nat. Rev. Immunol. 6:644-658. [DOI] [PubMed] [Google Scholar]
- 20.Kash, J. C., E. Muhlberger, V. Carter, M. Grosch, O. Perwitasari, S. C. Proll, M. J. Thomas, F. Weber, H. D. Klenk, and M. G. Katze. 2006. Global suppression of the host antiviral response by Ebola- and Marburgviruses: increased antagonism of the type I interferon response is associated with enhanced virulence. J. Virol. 80:3009-3020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khan, A. S., F. K. Tshioko, D. L. Heymann, B. Le Guenno, P. Nabeth, B. Kerstiens, Y. Fleerackers, P. H. Kilmarx, G. R. Rodier, O. Nkuku, P. E. Rollin, A. Sanchez, S. R. Zaki, R. Swanepoel, O. Tomori, S. T. Nichol, C. J. Peters, J. J. Muyembe-Tamfum, and T. G. Ksiazek. 1999. The reemergence of Ebola hemorrhagic fever, Democratic Republic of the Congo, 1995. Commission de Lutte contre les Epidemies a Kikwit. J. Infect. Dis. 179(Suppl. 1):S76-S86. [DOI] [PubMed] [Google Scholar]
- 22.Ksiazek, T. G., P. E. Rollin, A. J. Williams, D. S. Bressler, M. L. Martin, R. Swanepoel, F. J. Burt, P. A. Leman, A. S. Khan, A. K. Rowe, R. Mukunu, A. Sanchez, and C. J. Peters. 1999. Clinical virology of Ebola hemorrhagic fever (EHF): virus, virus antigen, and IgG and IgM antibody findings among EHF patients in Kikwit, Democratic Republic of the Congo, 1995. J. Infect. Dis. 179(Suppl. 1):S177-S187. [DOI] [PubMed] [Google Scholar]
- 23.Ksiazek, T. G., C. P. West, P. E. Rollin, P. B. Jahrling, and C. J. Peters. 1999. ELISA for the detection of antibodies to Ebola viruses. J. Infect. Dis. 179(Suppl. 1):S192-S198. [DOI] [PubMed] [Google Scholar]
- 24.Loo, Y. M., J. Fornek, N. Crochet, G. Bajwa, O. Perwitasari, L. Martinez-Sobrido, S. Akira, M. A. Gill, A. Garcia-Sastre, M. G. Katze, and M. Gale, Jr. 2008. Distinct RIG-I and MDA5 signaling by RNA viruses in innate immunity. J. Virol. 82:335-345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Muhlberger, E., M. Weik, V. E. Volchkov, H. D. Klenk, and S. Becker. 1999. Comparison of the transcription and replication strategies of marburg virus and Ebola virus by using artificial replication systems. J. Virol. 73:2333-2342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Reed, D. S., L. E. Hensley, J. B. Geisbert, P. B. Jahrling, and T. W. Geisbert. 2004. Depletion of peripheral blood T lymphocytes and NK cells during the course of Ebola hemorrhagic fever in cynomolgus macaques. Viral Immunol. 17:390-400. [DOI] [PubMed] [Google Scholar]
- 27.Rubins, K. H., L. E. Hensley, V. Wahl-Jensen, K. M. Daddario Dicaprio, H. A. Young, D. S. Reed, P. B. Jahrling, P. O. Brown, D. A. Relman, and T. W. Geisbert. 2007. The temporal program of peripheral blood gene expression in the response of nonhuman primates to Ebola hemorrhagic fever. Genome Biol. 8:R174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sanchez, A., T. W. Geisbert, and H. Feldmann. 2006. Filoviridae: Marburg and Ebola viruses, p. 1409-1448. In B. M. Knipe, P. M. Howley, D. E. Griffen, R. A. Lamb, and M. A. Martin (ed.), Fields virology, 5th ed. Lippincott-Raven, Philadelphia, PA.
- 29.Sanchez, A., M. Lukwiya, D. Bausch, S. Mahanty, A. J. Sanchez, K. D. Wagoner, and P. E. Rollin. 2004. Analysis of human peripheral blood samples from fatal and nonfatal cases of Ebola (Sudan) hemorrhagic fever: cellular responses, virus load, and nitric oxide levels. J. Virol. 78:10370-10377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Towner, J. S., J. Paragas, J. E. Dover, M. Gupta, C. S. Goldsmith, J. W. Huggins, and S. T. Nichol. 2005. Generation of eGFP expressing recombinant Zaire ebolavirus for analysis of early pathogenesis events and high-throughput antiviral drug screening. Virology 332:20-27. [DOI] [PubMed] [Google Scholar]
- 31.Towner, J. S., P. E. Rollin, D. G. Bausch, A. Sanchez, S. M. Crary, M. Vincent, W. F. Lee, C. F. Spiropoulou, T. G. Ksiazek, M. Lukwiya, F. Kaducu, R. Downing, and S. T. Nichol. 2004. Rapid diagnosis of Ebola hemorrhagic fever by reverse transcription-PCR in an outbreak setting and assessment of patient viral load as a predictor of outcome. J. Virol. 78:4330-4341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Towner, J. S., T. K. Sealy, T. G. Ksiazek, and S. T. Nichol. 2007. High-throughput molecular detection of hemorrhagic fever virus threats with applications for outbreak settings. J. Infect. Dis. 196(Suppl. 2):S205-S212. [DOI] [PubMed] [Google Scholar]
- 33.Tusher, V. G., R. Tibshirani, and G. Chu. 2001. Significance analysis of microarrays applied to the ionizing radiation response. Proc. Natl. Acad. Sci. USA 98:5116-5121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yount, J. S., T. M. Moran, and C. B. Lopez. 2007. Cytokine-independent upregulation of MDA5 in viral infection. J. Virol. 81:7316-7319. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.