Abstract
Between 1 September and 24 October 1976, 318 cases of acute viral haemorrhagic fever occurred in northern Zaire. The outbreak was centred in the Bumba Zone of the Equateur Region and most of the cases were recorded within a radius of 70 km of Yambuku, although a few patients sought medical attention in Bumba, Abumombazi, and the capital city of Kinshasa, where individual secondary and tertiary cases occurred. There were 280 deaths, and only 38 serologically confirmed survivors.
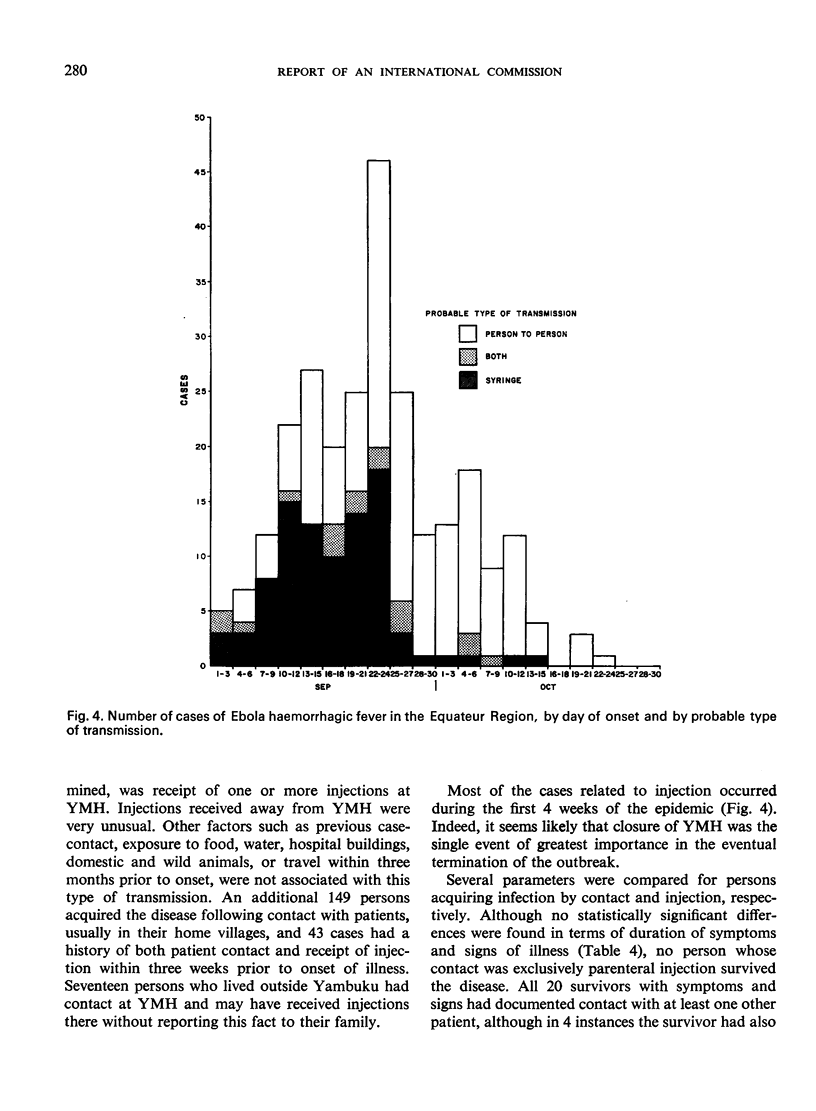
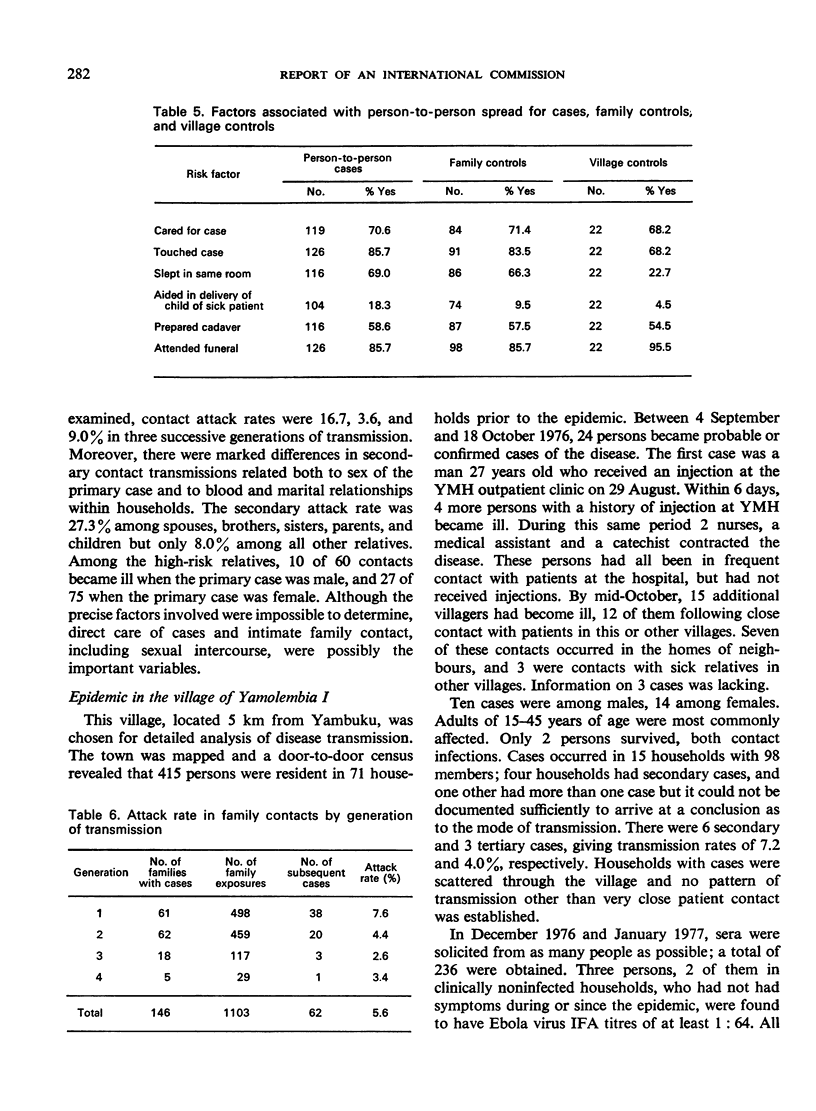
The index case in this outbreak had onset of symptoms on 1 September 1976, five days after receiving an injection of chloroquine for presumptive malaria at the outpatient clinic at Yambuku Mission Hospital (YMH). He had a clinical remission of his malaria symptoms. Within one week several other persons who had received injections at YMH also suffered from Ebola haemorrhagic fever, and almost all subsequent cases had either received injections at the hospital or had had close contact with another case. Most of these occurred during the first four weeks of the epidemic, after which time the hospital was closed, 11 of the 17 staff members having died of the disease. All ages and both sexes were affected, but women 15-29 years of age had the highest incidence of disease, a phenomenon strongly related to attendance at prenatal and outpatient clinics at the hospital where they received injections. The overall secondary attack rate was about 5%, although it ranged to 20% among close relatives such as spouses, parent or child, and brother or sister.
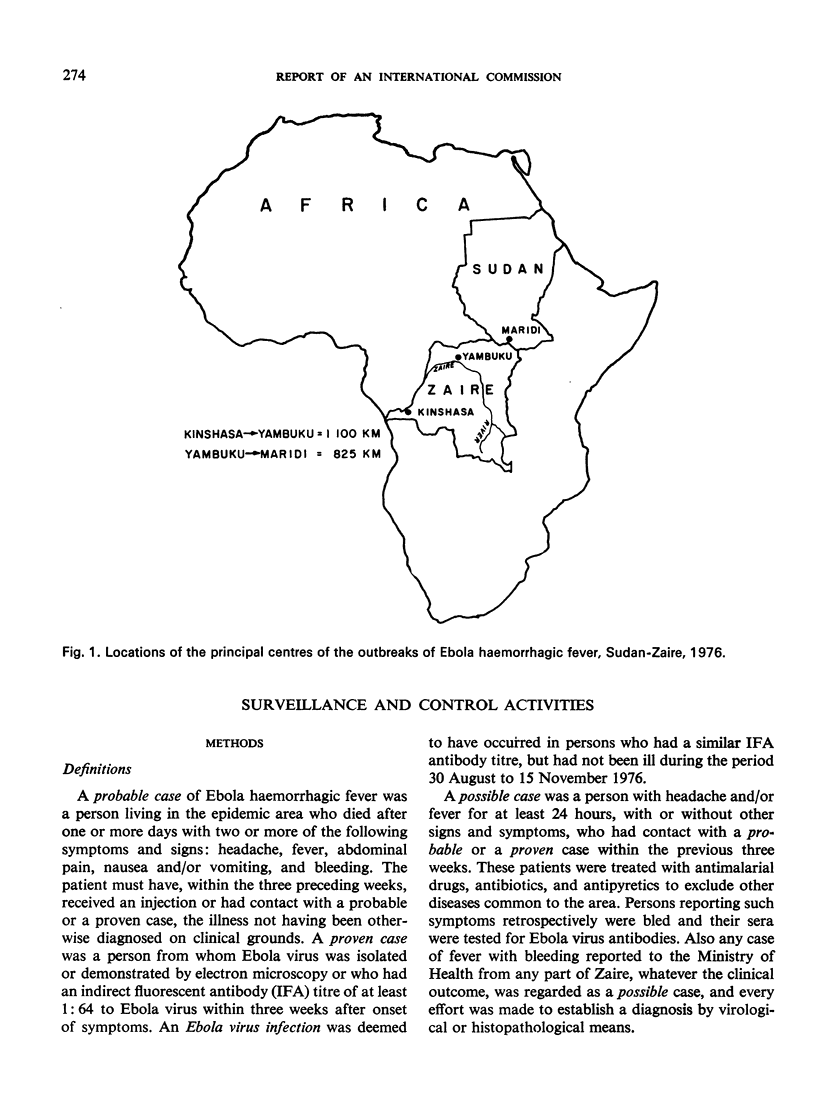
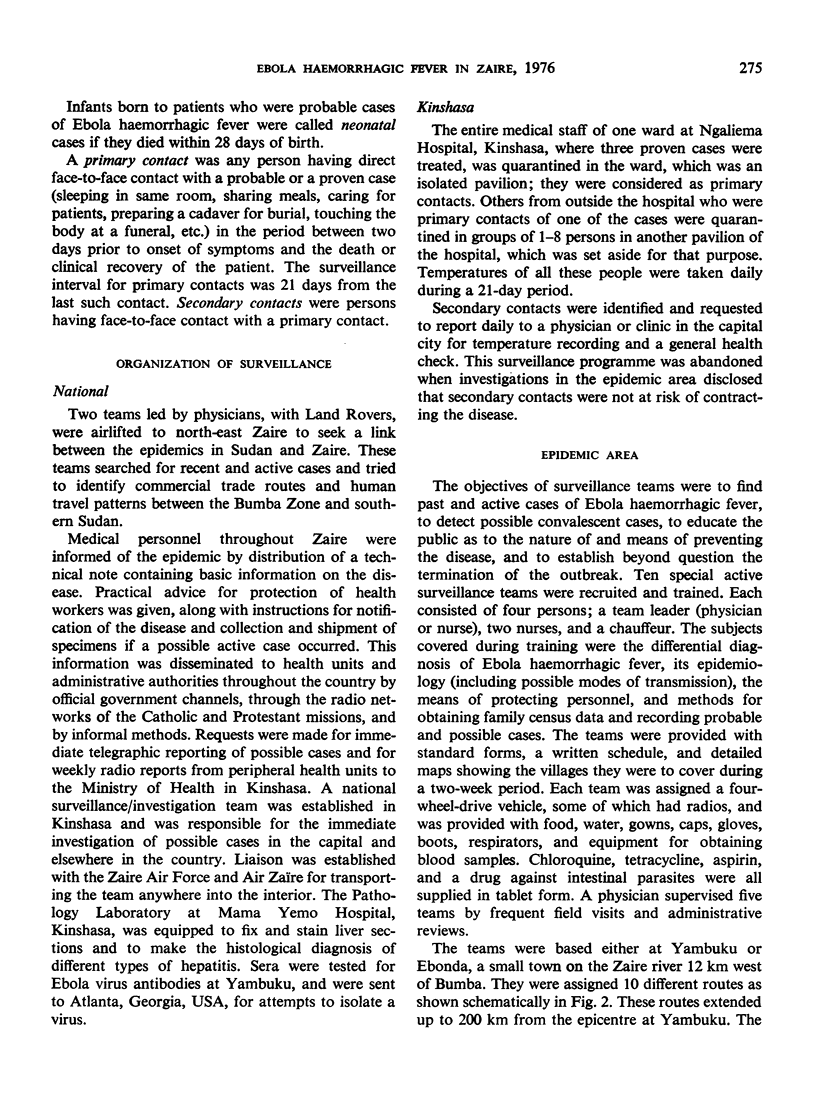
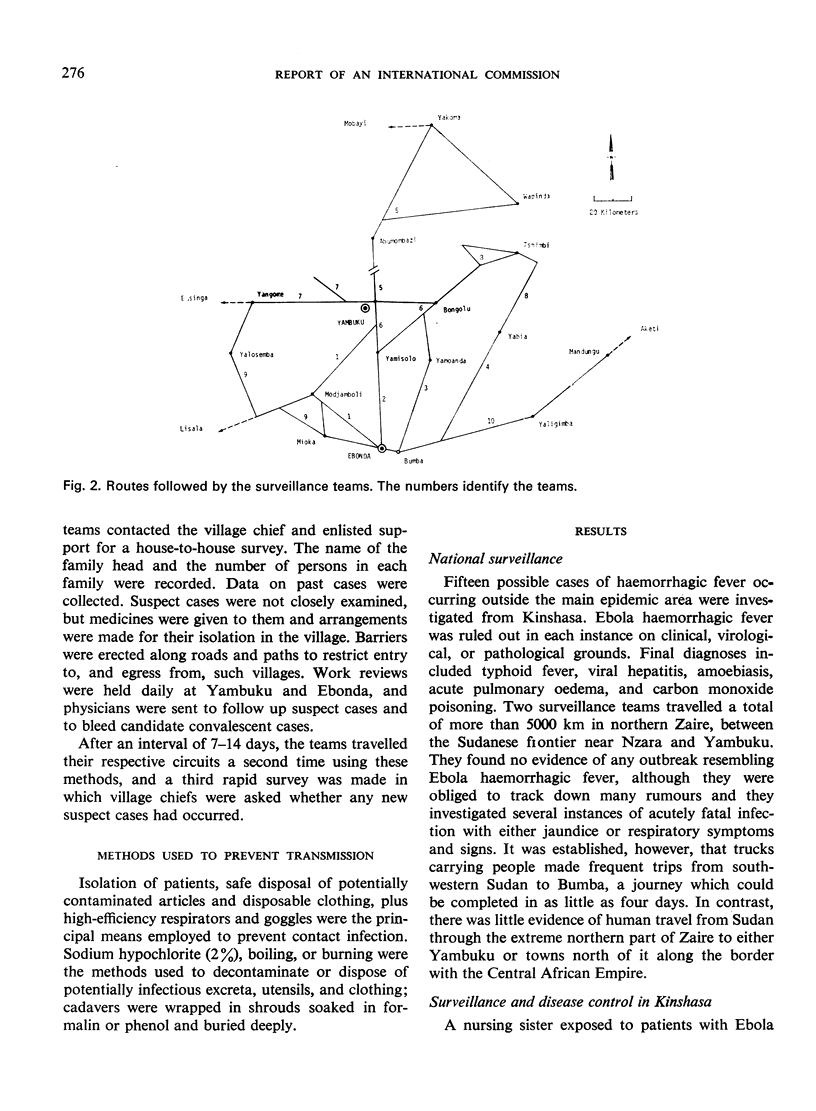
Active surveillance disclosed that cases occurred in 55 of some 550 villages which were examined house-by-house. The disease was hitherto unknown to the people of the affected region. Intensive search for cases in the area of north-eastern Zaire between the Bumba Zone and the Sudan frontier near Nzara and Maridi failed to detect definite evidence of a link between an epidemic of the disease in that country and the outbreak near Bumba. Nevertheless it was established that people can and do make the trip between Nzara and Bumba in not more than four days: thus it was regarded as quite possible that an infected person had travelled from Sudan to Yambuku and transferred the virus to a needle of the hospital while receiving an injection at the outpatient clinic.
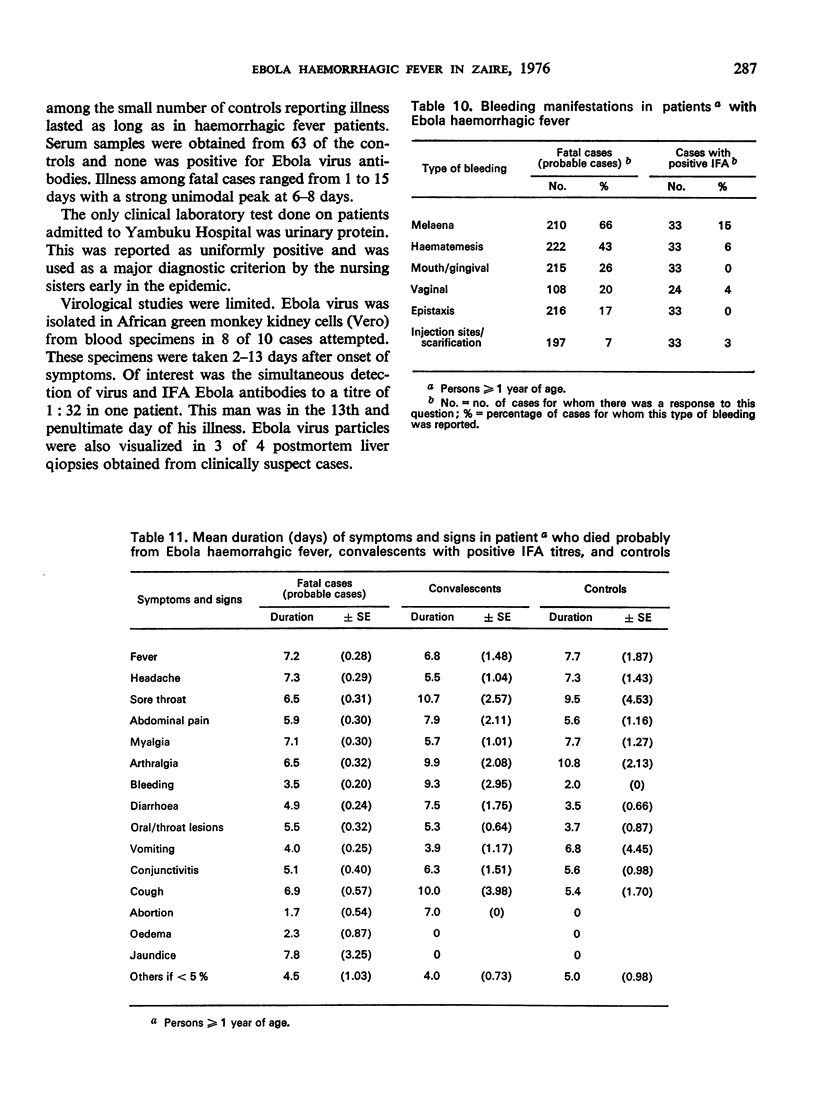
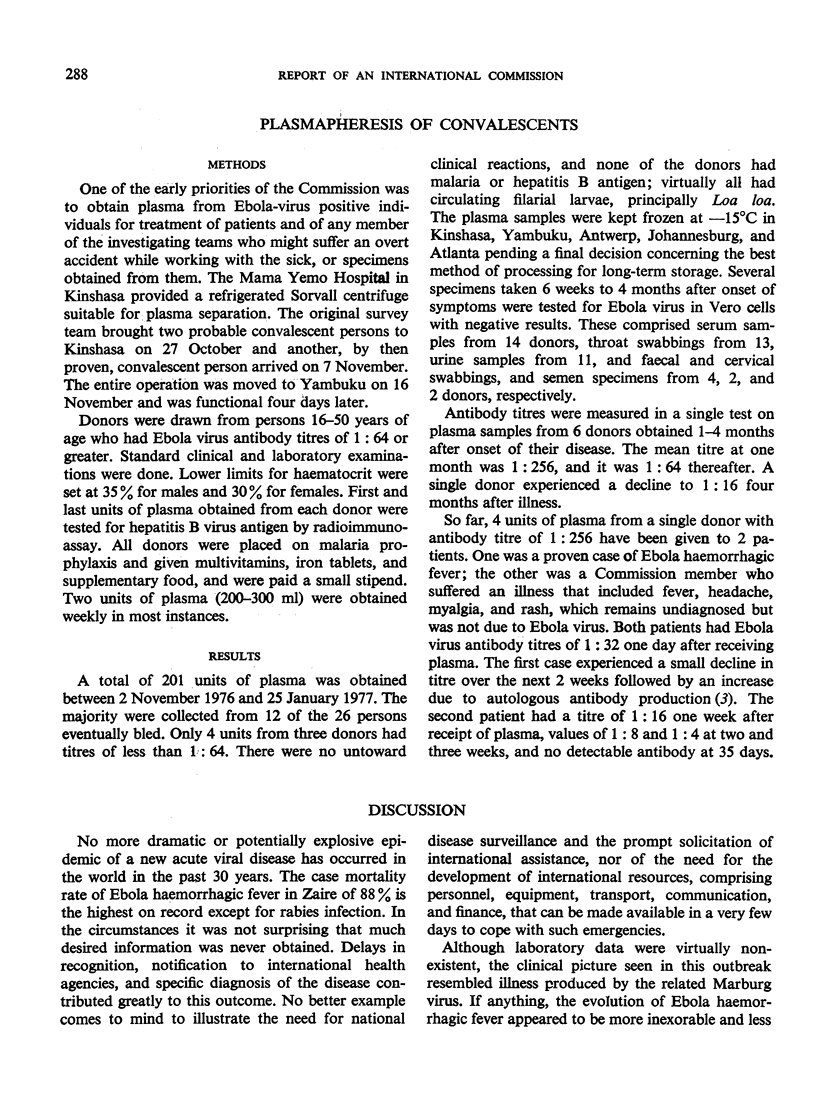
Both the incubation period, and the duration of the clinical disease averaged about one week. After 3-4 days of non-specific symptoms and signs, patients typically experienced progressively severe sore throat, developed a maculopapular rash, had intractable abdominal pain, and began to bleed from multiple sites, principally the gastrointestinal tract. Although laboratory determinations were limited and not conclusive, it was concluded that pathogenesis of the disease included non-icteric hepatitis and possibly acute pancreatitis as well as disseminated intravascular coagulation.
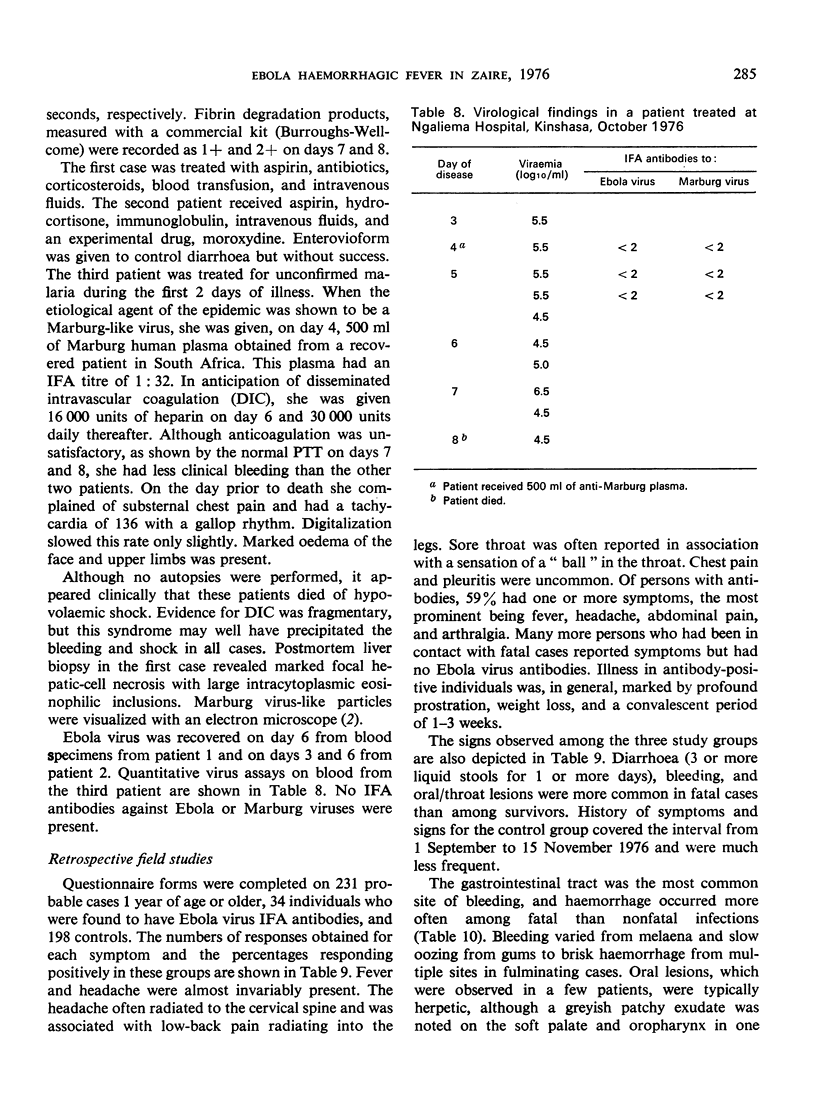
This syndrome was caused by a virus morphologically similar to Marburg virus, but immunologically distinct. It was named Ebola virus. The agent was isolated from the blood of 8 of 10 suspected cases using Vero cell cultures. Titrations of serial specimens obtained from one patient disclosed persistent viraemia of 106.5-104.5 infectious units from the third day of illness until death on the eighth day. Ebola virus particles were found in formalin-
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Emond R. T., Evans B., Bowen E. T., Lloyd G. A case of Ebola virus infection. Br Med J. 1977 Aug 27;2(6086):541–544. doi: 10.1136/bmj.2.6086.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson K. M., Lange J. V., Webb P. A., Murphy F. A. Isolation and partial characterisation of a new virus causing acute haemorrhagic fever in Zaire. Lancet. 1977 Mar 12;1(8011):569–571. doi: 10.1016/s0140-6736(77)92000-1. [DOI] [PubMed] [Google Scholar]
- Wulff H., Lange J. V. Indirect immunofluorescence for the diagnosis of Lassa fever infection. Bull World Health Organ. 1975;52(4-6):429–436. [PMC free article] [PubMed] [Google Scholar]


