Abstract
Purpose:
This study adapted the Structural Family Systems Ratings (SFSR), an observational measure of family interactions, for dementia caregivers. This article presents the development of the SFSR-Dementia Caregiver adaptation (SFSR-DC) and examines relationships between specific family-interaction patterns and caregiver distress.
Design and Methods:
The families of 177 Cuban American and White non-Hispanic American caregivers of dementia patients were assessed at baseline, 6, 12, and 18 months. Structural family theory and clinical experience were used to identify family interaction patterns believed to be related to caregiver emotional functioning. Factor analysis was used to refine subscales and develop a multiscale measure.
Results:
Six reliable subscales were related to caregiver distress and included in the SFSR-DC. There were two second-order factors. The SFSR-DC was provisionally cross-validated and showed invariance across the two ethnic groups.
Implications:
The SFSR-DC provides a method for examining specific and multiple interaction patterns in caregiver families and thus can advance knowledge regarding the role of the family in the stress processes of caregiving. These findings support the relevance of family interactions in caregiver distress and suggest that a treatment approach aimed at supporting family closeness and conflict resolution and reducing negativity might enhance caregiver well-being.
Keywords: Alzheimer's, Measurement, Relations, Cohesion
Family caregivers of dementia patients face elevated stress and experience negative outcomes such as depression (Schulz, Visitainer & Williamson, 1990). anxiety (Schulz & Williamson, 1994), and a sense of burden (Ory, Hoffman, Yee, Tennstedt, & Schulz, 1999). Researchers have sought to identify factors that influence the emotional consequences of caregiving. Such knowledge is useful for designing interventions to prevent and alleviate caregiver distress.
There is mounting evidence that the family plays a role in caregiver distress. Family factors that have been found to be related to the emotional functioning of caregivers include marital cohesion and satisfaction (Rankin, Haut, & Keefover, 2001), cooperative versus competitive communication patterns (Speice, Shields, & Blieszner, 1998), conflict (Semple, 1992), boundary ambiguity (Boss, Caron, Horbal & Mortimer, 1990), and family adaptability (Deimling, Smerglia & Schaefer, 2001; Majerovitz, 1995). Although such studies provide cumulative support for the importance of the family environment, there is no comprehensive theory-based model explaining the mechanisms by which family functioning influences the stress process of caregiving.
The framework that guides the current study is structural family theory (Minuchin, 1974), which views the family as an organism regulated by “structures,” that is, repetitive patterns of interaction. Structures determine the manner in which family members communicate, manage disagreements, distribute leadership roles, form alliances, and negotiate distance or closeness. The family's interaction patterns are relatively stable across different situations, and homeostatic processes make them resistant to change. Whereas healthy families adapt their structures in response to the changing needs of family members, others become rigid or disorganized under stress. In dementia caregiving, which requires a realignment of family interactions (Blieszner & Shifflett, 1990), previously adaptive structures may become obsolete. Although some caregiver families eventually reorganize to fulfill newly required roles, others maintain outdated patterns or come apart.
This structural conceptualization is congruent with the stress-process model (Pearlin, Mullan, Semple & Skaff, 1990) in that family functioning is both a secondary stressor and a resource: Stress can disorganize the family and expose individuals to risk, whereas family adaptation can protect individuals from the untoward affects of stress. There is evidence for the disruptive effects of stress on family functioning (McCubbin & Patterson, 1983; Peterson & Hawley, 1998) as well as the family's stress-buffering role (Patterson, 1988). In caregiving, this concept of the family's dual role in the stress process is supported by the work of Fisher and Lieberman (1996; Lieberman & Fisher, 1999).
At the Miami site of REACH (Resources for Enhancing Alzheimer's Caregiver Health; Eisdorfer et al., 2003), we tested the efficacy of a structural family intervention, Structural Ecosystems Therapy (SET; Mitrani, Szapocznik & Robinson, 2000), for reducing distress in caregivers. Our clinical team aimed to strengthen presumably protective structures such as family support, validation of the caregiver's leadership, and the ability to resolve problems; we also aimed to restructure patterns that we believed contributed to caregiver distress such as emotional detachment, negativity, and angry conflicts. Although our intervention strategies were based on structural theory and clinical experience, empirically derived knowledge of the linkages between specific family interaction patterns and caregiver outcomes is needed to develop family interventions that are precisely aimed at those patterns known to affect caregivers. This paradigm has been instrumental in the development of effective family treatments for delinquency and substance abuse (Szapocznik et al., 1988) but has not been applied to caregivers. Such theory-driven and empirically driven treatment-development efforts are recommended in the caregiving literature (Lebowitz, 2004; Pillemer, Suitor, & Wethington, 2003).
The research agenda outlined here requires a method for examining multiple dimensions of interaction in caregiver families. Family assessment is best achieved by observation-based measures (Lindahl, 2001), because they capture processes that are outside of the awareness of family members and are not subject to the reporter biases inherent in self-report. It is also desirable to have theory-based measures to test theoretical precepts that contribute to a comprehensive model and facilitate the translation of research to practice. The Structural Family Systems Ratings (SFSR; Szapocznik et al., 1991) is the only observational measure of family interaction that specifically focuses on multiple structural constructs at the familywide level (Mitrani & Perez, 2003). However, because the SFSR was designed for families of adolescents with behavior problems, its behavioral indicators may not capture some of the family processes that are most relevant for caregivers.
In the current study we adapted the SFSR to assess interactions in dementia caregiver families by integrating structural family theory, clinical experience, and psychometric findings. Our aim in this article is to introduce the SFSR–Dementia Caregiver adaptation (SFSR-DC) and examine the cross-sectional relationship between specific family-interaction patterns and caregiver distress.
Methods
Participants
The individuals in the sample included the families of 177 caregivers (94 Cuban Americans and 83 non-Hispanic White Americans) who participated at the Miami site of REACH. We assessed families at baseline and at 6, 12, and 18 months. We recruited caregivers through medical providers, social service agencies, and mass media announcements. The inclusion and exclusion criteria for REACH are described elsewhere (Wisniewski et al, 2003). Briefly, caregivers were required to live with the patient and provide care for a minimum of 4 hr per day for at least 6 months. Care recipients had a diagnosis of probable Alzheimer's disease or related dementia or a score below 24 on the Mini-Mental State Exam (MMSE; Folstein, Folstein, & McHugh, 1975). At the Miami site, at least one additional family member had to be available to participate.
The individuals in the sample for the current study at baseline can be described as follows. Caregivers had a mean age of 69.2 years (SD = 11.3) and had been caregiving for an average of 3.7 years (SD = 3.1). The majority of caregivers were female (71.8%); 43.5% were wives, 24.9% were husbands, 23.2% were daughters, and 8.5% were other relatives of the care recipient. The majority, 62.7%, of the caregivers had more than a high school education; 19.8% completed high school only, and 17.5% had less than a high school education. Their mean score on the Center for Epidemiologic Studies–Depression scale (CES-D; Radloff, 1977) was 17.2 (SD = 11.2), with 48% scoring above the clinical cutoff of 16 (Radloff & Teri, 1986). The mean age of the care recipients was 79.7 years (SD = 7.5). About half were female (51.4%). The mean score on the MMSE was 14.3 (SD = 8.0), with a range of 0 to 29.
Measures
The core battery of measures for REACH is described in Wisniewski and colleagues (2003). The SFSR was administered only at Miami. The measures utilized in the present study are presented here.
Caregiver Depression
We measured caregiver depression by using the CES-D, a 20-item self-report of depressive symptoms that asks about the frequency of depressive symptoms within the past week (4-point scale). Cronbach's alpha in this sample at baseline was α = .88.
Caregiver Anxiety
We measured caregiver anxiety by using the State Anxiety Inventory (SAI; Spielberger, 1979), consisting of 10 items comprising the state anxiety subscale of Spielberger's State-Trait Personality Inventory (Spielberger, Gorsuch, Lushene, Vagg, & Jacobs, 1983). Respondents are asked how much they agree with statements such as “I feel nervous” (4-point scale). Cronbach's alpha in the current sample at baseline was α = .85.
Caregiver Subjective Burden
We measured burden with the Revised Memory and Behavior Problems Checklist (RMBPC; Teri et al., 1992). Respondents indicate which of 24 problem behaviors the care recipient exhibited over the past week, and level of upset regarding each reported behavior, by using a 5-point scale. Subjective burden is calculated by finding the average upset score among all behaviors, assigning a zero to behaviors that were not manifested. Cronbach's alpha in the current sample at baseline was α = .83.
Family Interaction Patterns
We assessed family interaction patterns by using the SFSR, which uses a standardized procedure adapted from the Wiltwick Family Task (Minuchin, Rosman, & Baker, 1978) to elicit family interaction on three activities (planning a menu, discussing likes and dislikes about each other, and discussing a recent family argument). The tasks are designed to bring forth family processes that transcend specific presenting problems or content areas but that are nonetheless relevant to the family's management of their problems. Minuchin and colleagues used these tasks in their seminal work to compare the functioning of different diagnostic groups of families.
A trained rater observes videotapes of the family performing these tasks, and the rater codes 63 items on either two or three family tasks to yield a total of 133 indicators. The SFSR yields scores on five subscales: structure, resonance, developmental stage, identified patienthood, and conflict resolution. The range of scores on each subscale is 1 to 5, with higher scores indicating better family functioning. The five subscale scores are summed to determine the total score. Psychometrics with a sample of families of adolescents with behavior problems include alpha reliability of .88 and interrater reliabilities of .89 for total score (Szapocznik et al., 1991).
Procedures
SFSR Rating
A trained rater and V. Mitrani coded 322 videotapes. Mitrani, a developer of the SFSR with 15 years of rating experience, provided the gold standard for rating. The trained rater had more than 5 years of experience rating SFSRs. Rater training for the present study consisted of the two raters' reviewing the coding manual, rating five tapes together, and rating five tapes independently followed by meetings to reconcile discrepancies. Calibration between raters continued throughout the study, and the rating manual was updated to reflect additional instructional details and examples that emerged in these meetings. The raters were blind as to time point and treatment condition.
The average number of participants in the family tasks was 2.80 (SD = 0.75). Although eligibility for the parent study required that a third family member (in addition to the caregiver and care recipient) be available, family tasks were administered even if no others were present. Other family participants included caregivers' daughters (n = 60), sons (n = 44), husbands (n = 32), sisters (n = 17), brothers (n = 14), daughters-in-law (n = 14), sisters-in-law (n = 10), other extended family (n = 46), friends or neighbors (n = 14), and hired aides (n = 6). There were 147 tapes from baseline, 67 from the 6-month assessment, 63 from the 12-month assessment, and 45 from the 18-month assessment. Missing data at the later time points was primarily due to loss to follow-up. However, some family tasks were not administered because of the refusal of the care recipient (n = 8); some were administered but not rated as a result of poor audio or video quality (n = 28) and procedural breaches in family task administration (e.g., when task administrators gave additional instructions or stopped the task too early; n = 16). After the training period, 37 tapes were rated independently by both raters to assess interrater reliability.
We coded all 133 indicators from the SFSR, as well as 60 new indicators (25 items coded on two or more family tasks). A rating form and coding manual are available from V. Mitrani.
Overview of Measure Development Design
Development of the SFSR-DC involved three phases: (a) developing item pools for proposed subscales, (b) refining and conducting a preliminarily cross-validation of the subscales, and (c) developing a multi-dimensional scale. For the sake of clarity, we report the specific methods with the results of each phase.
Results
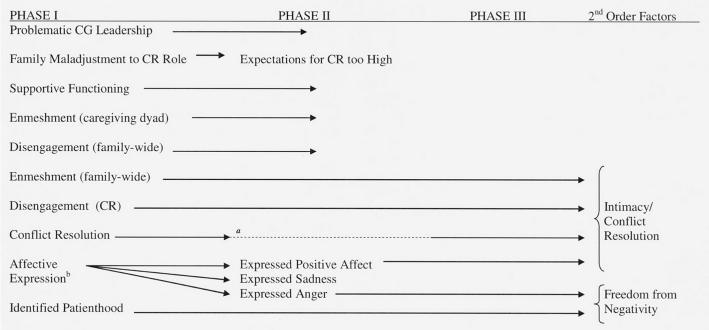
Figure 1 presents the outcome for each proposed subscale throughout the course of measure development.
Figure 1.
Overview of the Structural Family Systems Ratings–Dementia Caregivers Development Procedure (Phase I includes the clinical and theoretical item pool generation, Phase II includes empirical subscale refinement and confirmation, and Phase III includes the empirical multiscale measurement model).
aConflict resolution was unchanged from the existing SFSR; therefore it was not included in Phase II.
bAffective expression was initially proposed as one scale but emerged as three separate factors in Phase II and therefore was treated as three separate subscales.
Phase I
V. Mitrani reviewed dozens of videotaped family therapy sessions in her role as SET supervisor in the Miami REACH trial. The clinical review revealed recurrent family interactions that seemed to affect the well-being of the caregiver. The identified behaviors could be classified into eight constructs, two of which are not captured by the SFSR. We generated an item pool for each construct as a starting point for proposed subscales. Consistent with the SFSR, the same item rated on different family tasks was treated as separate indicators.
There were three sources of items for each item pool: (a) unmodified SFSR items, (b) items adapted from the SFSR with minor modification to fit the population but without changing the construct, and (c) new items. V. Mitrani developed a list of proposed new items and J. Szapocznik reviewed it to determine whether the items were reflective of the proposed construct and, in the case of the two proposed new constructs, whether they represented adequate coverage of the content area. Revisions to the new items were made on the basis of this feedback. Both individuals involved in item development are developers of the SFSR and of SET and are duly qualified to evaluate the appropriateness of the items for the family task method and their representation of the construct. The items, the family task on which they are rated, and their source are listed in Appendix A. The eight proposed subscales are described in the paragraphs that follow.
1. Problematic caregiver leadership is derived primarily from the SFSR's structure subscale and reflects the extent to which the caregiver is not fulfilling a leadership role in the family. This includes deficits in the caregiver's competence, involvement in decision making, alliances, and others' validation of his or her leadership. Problematic caregiver leadership is rated by noting the amount and quality of the caregiver's contribution toward task completion, how it compares with the contributions of other individuals, how others respond to the caregiver's leadership, and the overall resolution of the task.
2. Enmeshment and 3, disengagement, are derived from the SFSR's resonance subscale. Enmeshment refers to boundaries that are highly permeable, thus allowing for a high degree of closeness or intrusion between family members. Enmeshment is rated by noting the number of instances of boundary-intruding behaviors such as speaking for another person, physically controlling another person, and interruptions. Disengagement refers to boundaries that are highly rigid, thus precluding family closeness. Disengagement is rated by noting the absence of engagement (e.g., an individual does not speak or does not relate to others in an affective manner) or the presence of behaviors that reflect alienation (e.g., refusing to participate) during the course of a task.
The SFSR's resonance subscale sums the absolute value of enmeshed and disengaged indicators to yield one score. For the SFSR-DC, we treated enmeshment and disengagement as two separate subscales because our unpublished findings with adolescent families suggest that they are independent dimensions. Another change was the rating of enmeshment and disengagement at two levels. The first level, which is consistent with the SFSR, is to rate familywide resonance behaviors (e.g., the number of times any individual in the family speaks for any other individual in the family; or whether any individual in the family is never spoken to during the course of the task). The second level involved coding five of the enmeshment items (those most relevant to dyadic functioning) specifically within the caregiver–care recipient dyad (e.g., the number of times the caregiver speaks for the care recipient), and coding all of the disengagement items as they applied specifically to the care recipient (e.g., whether the care recipient is never spoken to during the course of the task). Both levels of coding were tested in Phase II.
4. Family maladjustment to the care recipient's roles is derived from the SFSR's developmental stage subscale, and it reflects the family's failure to adapt to the dementia in that the care recipient is assigned roles that are incongruent with his or her level of functioning. Items consist of noting whether family members assign a role to the care recipient that is either too high (e.g., asking an incapacitated care recipient to lead a task) or too low (e.g., the opinions of a capable care recipient are ignored or not solicited).
5. Identified patienthood is an SFSR subscale that assesses the extent or rigidity of family negativity toward and focus on the identified patient. It is rated by noting the number of times family members focus on or express negativity about the care recipient or the caregiving situation. One new item, “catering to the care recipient,” captures one aspect of the family's focus on the care recipient.
6. Conflict resolution is the only SFSR subscale that was unchanged for the SFSR-DC and reflects the manner in which the family manages disagreements and tasks. The resolution of individual differences of opinion and of the overall family task is rated on a 5-point scale. The lowest point on the scale is denial (acting as though a problem does not exist); this is followed by avoidance (the problem emerges but is “swept under the rug”), diffusion (moving on to another problem or conflict without resolving the previous one), and emergence (discussion of the conflict or problem) without reaching a resolution. The highest level is emergence with resolution. We decided not to change this subscale because we observed that caregiver families engaged in all five levels of conflict resolution, and these seemed relevant to caregiver functioning. Further, the scoring of this subscale would not lend itself to factor analysis because items represent mutually exclusive categories and use clinically derived weighting of the different conflict resolution categories.
7. Supportive functioning is a new subscale that, at one end, reflects family support toward the caregiver such as family members' helping with care recipient behavior problems or expressing praise or concern toward the caregiver, and, on the other end, reflects criticism or harsh behavior toward the caregiver. The supportive items were weighted positively and the problematic items were weighted negatively to yield the supportive functioning score. This subscale was proposed in response to our clinical experience as well as research on the relevance for dementia caregivers of family support (Horowitz, 1985; Zarit, Reever, & Bach-Peterson, 1980) and negative exchanges in the social network (Pagel, Erdly, & Becker, 1987).
8. Affective expression reflects the family's overall emotional tone during the family tasks. For each task, the rater assigned a separate score ranging from 0 (not at all) to 4 (extremely) for the extent to which each of four types of affect was expressed by the family: anger or intensity of conflicts, sadness, levity, and positive regard or affection. This subscale was proposed in response to our clinical observation that caregivers in families in which there were expressions of affection or who managed difficulties with a sense of humor seemed to fare better than those in which the overall tone was characterized by sadness or anger.
Phase II
Refining the proposed subscales involved two stages. Stage 1 utilized data collected at the 6-, 12-, and 18-month assessments (n = 175) to reduce the item pools to yield reliable subscales. Stage 2 utilized baseline data (n = 147) to perform a confirmatory factor analysis on the subscales that emerged from Stage 1. Conflict resolution was not included in Phase II because it was being accepted without change for the SFSR-DC.
Phase II, Stage 1
We carried out the following four steps for each proposed subscale.
1. We entered indicators in the proposed item pool into an exploratory factor analysis (extraction method: principal component analysis; rotation method: varimax with Kaiser normalization). We compared the factor solutions that were suggested by the scree plot (Catell, 1966) and that had eigenvalues greater than 1 (Kaiser, 1958). The factor solution we selected was the one with the smallest number of factors, that offered minimal overlap of indicators between factors, and in which each factor represented a discernible facet of the subscale construct. We removed indicators that did not load at .30 or above on any factor (Comrey & Lee, 1992).
2. For the multifactor solutions from Step 1, we conducted a factor analysis forcing a single-factor solution to determine if the factors could be aggregated into a single subscale. If a single factor was workable, then we removed indicators with a loading of less than .3 on the single factor. If a single factor was not workable, then we moved each factor forward as a separate subscale.
3. For the indicators that remained after Step 2, we calculated internal consistency by using Cronbach's alpha. We removed indicators that substantially lowered alpha by their inclusion.
4. We conducted interrater reliability analyses (from the entire study sample) on indicators that remained after Step 3 by using intraclass correlation. If the interrater reliability was .7 or above (Hruschka et al., 2004; Landis & Koch, 1977), then we accepted the scale as is. If it was lower than .7, then we calculated interrater reliabilities for each indicator and we removed those that substantially reduced the scale's interrater reliability. We used the intraclass correlation coefficient because the ratings did not form a square n × n table (McGraw & Wong, 1996).
The results of Phase I, Stage 1 were that three proposed subscales emerged as single factors: problematic caregiver leadership (10 indicators), identified patienthood (4 indicators), and supportive functioning (11 indicators). Family maladjustment to the care recipient's roles emerged as expectations of the care recipient that are too high (3 indicators). Affective expression emerged as three subscales: expressed positive affect (6 indicators), expressed sadness (2 indicators), and expressed anger (3 indicators). Enmeshment and disengagement, which were tested at two levels of coding, emerged as familywide enmeshment (12 indicators) and care recipient disengagement (9 indicators). In the case of disengagement, both coding levels resulted in the exact same indicators and were capturing the disengagement of the care recipient from the rest of the family.
Phase II, Stage 2
We entered the indicators from each of the nine subscales that emerged from Stage 1 in a single confirmatory factor analysis by using Mplus Version 2.13 (Muthén & Muthén, 2002), to test whether each subscale was explained by its own single common factor. This procedure serves as a cross-validation of the subscales developed in Stage 1. Note however, that this sample does include the same participants as the sample from Stage 1 (but at different time points), so this is not an independent cross-validation.
Of the 60 indicators that emerged from Stage 1, we removed 14 after preliminary analyses. We removed 4 indicators from problematic caregiver leadership, 6 from supportive functioning, and 2 from expectations of the care recipient that are too high because of the low base rate in the new sample (less than 14 in 147). We removed 1 indicator from problematic caregiver leadership because its loading was not significantly different from zero. Because we dropped 2 of the 3 indicators in the expectations of the care recipient that are too high subscale, we also dropped the subscale's final indicator, thus eliminating this subscale.
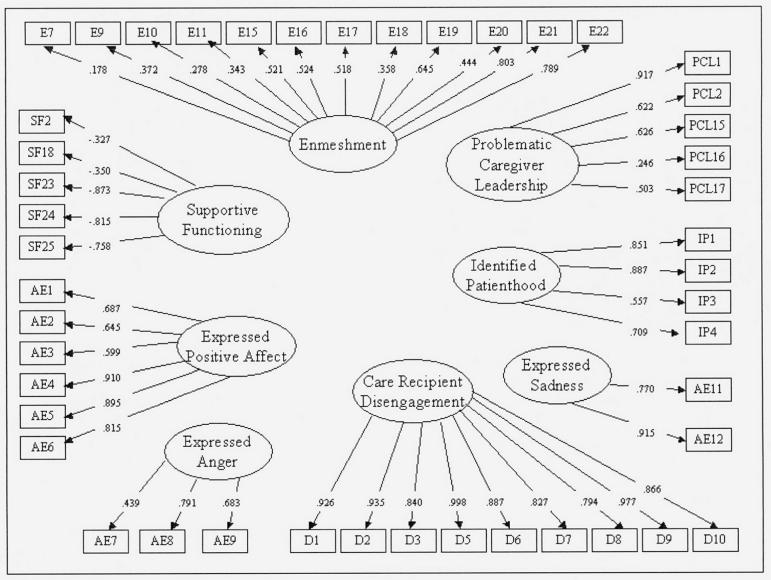
The first-order confirmatory factor analysis tested a model with eight hypothesized common factors (subscales) underlying 46 indicators. This model allowed free correlations between subscales and permitted correlations between error variance terms only for indicators that rated the same items on different tasks. We used two indices of fit, the comparative fit index (CFI) and root mean square error of approximation (RMSEA), to evaluate the model. We did not use the chi-square statistic because significance may be due to sample size despite reasonable fit of the model (Bentler & Bonett, 1980; Byrne 2001). The fit indices (CFI = .922, RMSEA = .076) supported this model (Byrne; Tabachnick & Fidell, 1996). Figure 2 shows the factor loadings for each indicator on their respective subscales. The reader should refer to Appendix A for indicator codes. Table 2 presents the estimated correlations between subscales.
Figure 2.
Factor loadings of indicators on subscales from confirmatory factor analysis (Phase II, Stage 2).
Table 2.
Subscale Reliabilities After Confirmatory Factor Analysis (Phase II, Stage 2)
| Subscale | Composite Reliability |
Interrater Reliability (Intraclass Correlation) |
|---|---|---|
| Problematic caregiver leadership | .735 | .734 |
| Enmeshment | .780 | .838 |
| Care recipient disengagement | .974 | .937 |
| Identified patienthood | .843 | .796 |
| Supportive functioning | .779 | .887 |
| Expressed positive affect | .894 | .814 |
| Expressed sadness | .833 | .819 |
| Expressed anger | .681 | .617 |
| Conflict resolution | — | .800 |
Note: A dash indicates that the composite reliability not calculated because items represent mutually exclusive categories.
We calculated composite reliability (Fornell & Larcker, 1981) for each individual subscale as an index of internal consistency. Table 3 shows each subscale's composite reliability and interrater reliability, using intraclass correlation (n = 37). All subscales except for expressed anger (composite reliability = .68; κ = .62) had composite reliability and interrater reliability above .7.
Table 3.
Correlations (Spearman's ρ) Between Subscales and Caregiver Outcomes
| Subscale | Depression | Anxiety | Subjective Burden |
|---|---|---|---|
| Problematic caregiver leadership | −.079 | −.130 | −.092 |
| Enmeshment | −.097 | −.271** | −.073 |
| Care recipient disengagement | .310** | .307** | .087 |
| Identified patienthood | .128 | .132 | .253** |
| Supportive functioning | −.088 | −.057 | −.004 |
| Expressed positive affect | −.176* | −.218* | .094 |
| Expressed sadness | .144 | .141 | .124 |
| Expressed anger | .038 | .029 | .201* |
| Conflict resolution | −.262** | −.327** | −.030 |
Note: Bolded data indicate significant correlations.
p ≤ .05
p ≤ .01.
Phase III
In Phase III we were interested in combining the subscales to yield an overall measure related to caregiver distress. This involved four stages, which are explained in the following paragraphs.
Phase III, Stage 1
We examined the correlations between each subscale and caregiver depression, anxiety, and subjective burden. We used baseline data to provide the largest independent sample of family tasks tapes. These correlations are shown in Table 4. We retained those scales that had a significant (p < .05) correlation with at least one distress measure.
Phase III, Stage 2
We converted the subscale scores from a continuous measure to a 5-point category scale. We based this conversion on quintile cutoffs of each subscale's distribution, utilizing data from all time points so as to provide as large a standardization sample of scores as possible. We reverse scored the subscales that were positively associated with unfavorable outcomes. We summed the converted scores for the six subscales to yield an SFSR-DC total score, which was related to depression (ρ = −.328, p < .001), anxiety (ρ = −.419, p < .001), and subjective burden (ρ = −.268, p < .001). In comparison, the total score from the SFSR was only related to depression (ρ = −.196, p < .019).
Phase III, Stage 3
We tested the factor structure of the SFSR-DC by entering baseline data for each subscale as an indicator loading on a single latent variable in a confirmatory factor analysis using Mplus. The model met criterion for goodness of fit on the CFI index (.918) but not RMSEA (.092). Although these fit indices were somewhat acceptable, an examination of the six scale loadings revealed that identified patienthood and expressed anger had low negative loadings on the latent family-functioning variable, suggesting that a two-factor model might fit the data better. We tested the two-factor model by using confirmatory factor analysis. Fit indices were CFI = .981 and RMSEA = .048, indicating good fit. Factor 1, which we named intimacy–conflict resolution, consisted of enmeshment, care recipient disengagement, conflict resolution, and expressed positive affect. This factor was correlated with depression (ρ = −.301, p < .001) and anxiety (ρ = −.409, p < .001). Factor 2, freedom from negativity, consisted of identified patienthood and expressed anger (recall that high scores reflect low negativity). This factor was correlated with subjective burden (ρ = −.301, p < .001).
Phase III, Stage 4
We tested whether the overall factor pattern in the two-factor measurement model was the same for both ethnic groups (White non-Hispanic American and Cuban American) by using multigroup confirmatory factor analysis. This procedure compares the relative fit of a model that constrains the two ethnic groups to be the same to an alternative model where the two groups are allowed to be different. There was not a statistically significantly difference in fit [χ2(df = 3) = 2.03, p < .567] between the two models, suggesting invariance.
Discussion
Although the family is the most proximal and influential interpersonal context throughout the life span, and therefore clearly influences caregiver emotional functioning, there is currently no model elucidating the family mechanisms of caregiver distress. Scientific progress is dependent on the measurement of key variables (Nunnally & Bernstein, 1994). The SFSR-DC provides a theoretically grounded observational method for examining multiple dimensions of family interaction that are related to emotional distress in caregivers. In this way, the SFSR-DC can promote understanding of the role of the family in the stress process of caregiving; that is, how the family is affected by having a member with dementia, how family adaptation can protect caregivers from the effects of stress, and, conversely, how the family's failure to adapt exposes the caregiver to risk. Such research could ultimately contribute to the development of precisely focused family interventions to prevent and alleviate caregiver distress.
In addition to measure development, this study provided support for the relevance of family interactions in caregiver distress, and it expanded our knowledge regarding some specific facets of this relationship. First, the use of non-caregiving-related tasks demonstrated that family interactions do not have to be about caregiving to be relevant for caregiver distress. Second, enmeshment, which is typically considered to be problematic (Minuchin, 1974), appears to play a protective function. It is likely that we tapped a moderate level of enmeshment reflecting cohesiveness rather than gross boundary violations, and perhaps it would be more accurate to rename the subscale enmeshment–cohesion. Another finding was that care recipient disengagement was related to caregiver distress. This warranted further analysis because of the possibility that the patient's impairment was driving this relationship. Controlling for MMSE, we found that partial correlations of care recipient disengagement with depression (r = .215, p < .011) and anxiety (r = .228, p < .007) suggest that, regardless of the patient's level of impairment, caregivers are at risk for distress when care recipients are uninvolved in family activities. Finally, we found that it is the manner in which families manage conflicts, rather than the amount of conflict (which we examined in a follow-up analysis) that is related to distress in caregivers.
Limitations
Limitations in this study warrant caution in interpreting results. First, the family members who participated were those who chose to attend after being invited by the caregiver. Therefore, the sample may be overrepresented by family members who were attached to the family. Second, the different phases of measures development did not use independent samples. A further limitation related to sampling is that the pattern of missing data after baseline is likely to represent a bias in the follow-up sample, on which we based our Stage 1 measurement strategy. However, the confirmatory stage and the correlations with caregiver distress were performed with the baseline sample, which had good representation.
Directions for Future Research
Further efforts are needed to cross-validate and examine the SFSR-DC's relationship with other family measures. Although it has been argued that any family activity can be used to assess interpersonal processes (Florsheim & Benjamin, 2001), the choice of family tasks has an impact on the behaviors that are elicited and may have implications for the SFSR-DC's ecological validity. Accordingly, a question that deserves study is whether using family tasks that are directly related to caregiving (e.g., discussing how the family should address some aspect of the patient's care) can tap family processes that are more central to caregiver distress.
Our findings suggest that family closeness and conflict resolution can help protect caregivers from distress, and that family negativity is a risk factor. Longitudinal studies are needed to understand how these and other family structures are changed in response to changes in the stress associated with having a family member with dementia. There are questions about the interaction of family composition and family functioning. Therefore, the use of this measure in a longitudinal design requires documentation of changes in family participation and whether these changes reflect changes in family composition. Clinical follow-up studies also are needed to ascertain whether family structures can be transformed through family therapy and whether such changes in family functioning predict changes in caregiver distress.
Table 1.
Estimated Correlations between Subscales
| Problematic Caregiver Leadership |
Supportive Functioning |
Enmeshment | Care Recipient Disengagement |
Identified Patienthood |
Expressed Positive Affect |
Expressed Sadness |
Expressed Anger |
|
|---|---|---|---|---|---|---|---|---|
| Problematic caregiver leadership | — | |||||||
| Supportive functioning | .545 | — | ||||||
| Enmeshment | .210 | .329 | — | |||||
| Care recipient disengagement | .305 | .001 | −.022 | — | ||||
| Identified patienthood | −.040 | .133 | −.012 | −.113 | — | |||
| Expressed positive affect | −.112 | .083 | .922***a | −.331* | −.087 | — | ||
| Expressed sadnes | .245 | .302 | −.129 | .009 | .592*** | −.261** | — | |
| Expressed anger | .433 | .192 | .088 | .084 | .298** | −.243* | .324** | — |
p < .05
p < .01
p < .001.
Statistical significance was calculated in Mplus by dividing the estimate of the covariance by the standard error of the estimate (a t test). Note that using the Fisher Z test, any correlation that is greater than .164 in absolute value is significantly different than zero at the .05 level.
Acknowledgments
This study was supported by a mentored scientist development grant from the National Institute on Aging (Grant K01AG00977) to V. Mitrani, and a grant from the National Institute on Aging and National Institute on Nursing Research (Grant VO1AG13292) to C. Eisdorfer. We express our gratitude to Carl Eisdorfer, Richard Schulz, Monica Zarate, Frank Dillon, and the families who participated in this study.
Appendix A
Item Pool for Each Proposed Subscale
| Item Description | Task (Indicator Code) | Source |
|---|---|---|
| Problematic Caregiver Leadership | ||
| Othera gives at least two more task opinions than CG | I (PCL1), III (PCL2) | Structure-Modified |
| CR gives at least two more task opinions than CG | I (PCL3), III (PCL4) | Structure-Modified |
| CR surpasses CG in number of task opinions | I (PCL5), III (PCL6) | Structure-Modified |
| CG gives no guidance | I (PCL7), III (PCL8) | Structure-Modified |
| CG misinterprets task causing miscompletion | I (PCL9), III (PCL10) | Structure-Modified |
| Other misinterprets task causing miscompletion | I (PCL11), III (PCL12) | Structure-Modified |
| CG not part of leadership subsystem | I (PCL13), III (PCL14) | Structure-Modified |
| CG functioning below expectations | I (PCL15), II (PCL16), III (PCL17) | Developmental Stage-Modified |
| CG treated like a child | I (PCL18), II (PCL19), III (PCL20) | Developmental Stage-Modified |
| Other usurps CG's authority | I (PCL21), II (PCL22), III (PCL23) | Developmental Stage-Modified |
| Task resolution lower than “emergence without resolution” | I (PCL24), II (PCL25), III (PCL26) | Conflict Resolution-Modified |
| Enmeshment | ||
| Semi- or undifferentiated responses | I (E1), II (E2) | Resonance |
| Differentiated responses | I (E3), II (E4) | Resonance |
| Mind readingsb | I (E5), II (E6) | Resonance |
| Mediated responses (one person speaks for another person) | I (E7), II (E8) | Resonance |
| Continuations (of another person's speech) | I (E9), II (E10) | Resonance |
| Personal control (one person speaks authoritatively about another person) | I (E11), II (E12) | Resonance |
| Engagement reaction | I (E13), II (E14) | Resonance |
| Simultaneous speeches | I (E15), II (E16) | Resonance |
| Interruptions | I (E17), II (E18) | Resonance |
| Losses of distance (use of physical control) | I (E19), II (E20) | Resonance |
| Joint affective reactions | I (E21), II (E22) | Resonance |
| Disengagementc | ||
| A participant is not spoken to | I (D1), II (D2) | Resonance |
| A participant is not spoken about | I (D3), II (D4) | Resonance |
| A participant does not speak | I (D5), II (D6) | Resonance |
| A participant is not related to affectively | I (D7), II (D8) | Resonance |
| A participant does not relate affectively | I (D9), II (D10) | Resonance |
| A participant is not allied with anyone | I (D11), II (D12) | Resonance |
| A participant refuses a request to participate | I (D13), II (D14) | Resonance |
| A participant ignores a request to participate | I (D15), II (D16) | Resonance |
| A participant asks to be excluded from the task | I (D17), II (D18) | Resonance |
| A participant asks to be excluded from a family activity | I (D19), II (D20) | Resonance |
| A participant expresses a wish to be away from the family | I (D21), II (D22) | Resonance |
| Family Maladjustment to CR Role | ||
| Expectations of CR too high | I (FA1), II (FA2), III (FA3) | Developmental Stage-Modified |
| Expectations of CR too low | I (FA4), II (FA5), III (FA6) | Developmental Stage-Modified |
| Expectations of CR both too high and too low | I (FA7), II (FA8), III (FA9) | New |
| Identified Patienthood | ||
| Negativity about CR or caregiving | II (IP1), III (IP2) | Identified Patienthood |
| CR or caregiving centrality | II (IP3), III (IP4) | Identified Patienthood |
| Overprotection or nurturance of IPhood (CR dysfunction is reinforced) | II (IP5), III (IP6) | Identified Patienthood-Modified |
| Denial of other problems | II (IP7), III (IP8) | Identified Patienthood |
| Other Identified Patienthood | II (IP9), III (IP10) | Identified Patienthood |
| Catering to the CR | I (IP11), II (IP12) | New |
| Conflict Resolution | ||
| No. of “denials” | I (CR1), III (CR2) | Conflict Resolution |
| No. of “avoidances” | I (CR3), III (CR4) | Conflict Resolution |
| No. of “diffusions” | I (CR5), III (CR6) | Conflict Resolution |
| No. of “emergence without resolutions” | I (CR7), III (CR8) | Conflict Resolution |
| No. of “emergence with resolutions” | I (CR9), III (CR10) | Conflict Resolution |
| Level of resolution achieved on overall task | I (CR11), II (CR12), III (CR13) | Conflict Resolution |
| Supportive Functioning | ||
| CR or others give guidance | I (SF1), III (SF2) | New |
| CR gives comfort to CG | I (SF3), III (SF4) | New |
| Other gives comfort to CG | I (SF5), III (SF6) | New |
| CR expresses concern for CG | I (SF7), III (SF8) | New |
| Other expresses concern for CGI | I (SF9), III (SF10) | New |
| CR praises CG | I (SF11), III (SF12) | New |
| Other praises CG | I (SF13), III (SF14) | New |
| CR criticizes CG | I (SF15), III (SF16) | New |
| Other criticizes CG | I (SF17), III (SF18) | New |
| CR is harsh towards CG | I (SF19), III (SF20) | New |
| Other is harsh towards CG | I (SF21), III (SF22) | New |
| Support rating regarding CR behavior problems | I (SF23), II (SF24), III (SF25) | New |
| CG has no allies | I (SF26), III (SF27) | Structure-Modified |
| Others not part of leadership subsystem | I (SF28), III (SF29) | Structure-Modified |
| CG's spouse not supportive | I (SF30), III (SF31) | Structure-Modified |
| Affective Expression | ||
| Affection or positive regard rating | I (AE1), II (AE2), III (AE3) | New |
| Levity rating | I (AE4), II (AE5), III (AE6) | New |
| Anger rating | I (AE7), II (AE8), III (AE9) | New |
| Sadness rating | I (AE10), II (AE11), III (AE12) | New |
Notes: CG = caregiver; CR = care recipient. Bolded indicators were included in the Phase II, Stage 2 model.
Other refers to a participant other than the caregiver or the care recipient.
Item coded at both the family-wide and caregiving dyad level.
All disengagement items were coded at both the family-wide and care recipient level.
References
- Bentler PM, Bonnet DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychological Bulletin. 1980;88:588–606. [Google Scholar]
- Blieszner R, Shifflett PA. The effects of Alzheimer's disease on close relationships between patients and caregivers. Family Relations. 1990;39:57–62. [Google Scholar]
- Boss P, Caron W, Horbal J, Mortimer J. Predictors of depression in caregivers of dementia patients: Boundary ambiguity and mastery. Family Process. 1990;29:245–254. doi: 10.1111/j.1545-5300.1990.00245.x. [DOI] [PubMed] [Google Scholar]
- Byrne BM. Structural equation modeling with AMOS: Basic concepts, applications, and programming. Lawrence Erlbaum Associates; Mahwah, NJ: 2001. [Google Scholar]
- Catell RB. The scree test for the number of factors. Multivariate Behavioral Research. 1966;1:245–276. doi: 10.1207/s15327906mbr0102_10. [DOI] [PubMed] [Google Scholar]
- Comrey AL, Lee HB. A first course in factor analysis. 2nd ed. Erlbaum; Hillsdale, NJ: 1992. [Google Scholar]
- Deimling GT, Smerglia VL, Schaefer ML. The impact of family environment and decision-making satisfaction and caregiver depression: A path analytic model. Journal of Aging and Health. 2001;13(1):47–71. doi: 10.1177/089826430101300103. [DOI] [PubMed] [Google Scholar]
- Eisdorfer C, Czaja SJ, Loewenstein DA, Rubert MP, Arguelles S, Mitrani VB, et al. The effect of a family therapy and technology-based intervention on caregiver depression. The Gerontologist. 2003;43:521–531. doi: 10.1093/geront/43.4.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher L, Lieberman MA. The effects of family context on adult offspring of patients with Alzheimer's disease: A longitudinal study. Journal of Family Psychology. 1996;10:180–191. [Google Scholar]
- Florsheim P, Benjamin LS. The structural analysis of social behavior. In: Kerig PK, Lindahl LM, editors. Family observational coding systems: Resources for systemic research. Erlbaum; Mahwah, NJ: 2001. pp. 127–150. [Google Scholar]
- Folstein MF, Folstein SF, McHugh PR. Mini-Mental State: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Fornell C, Larcker DF. Evaluating structural equation models with unobservable variables and measurement error. Journal of Marketing Research. 1981;48(1):39–50. [Google Scholar]
- Horowitz A. Sons and daughters as caregivers to older parents: Differences in role performance and consequences. The Gerontologist. 1985;25:612–617. doi: 10.1093/geront/25.6.612. [DOI] [PubMed] [Google Scholar]
- Hruschka DJ, Schwartz D, Cobb St. John D, Picone-Decaro E, Jenkins RA, Carey JW. Reliability in coding open-ended data: Lessons learned from HIV behavioral research. Field Methods. 2004;16:307–331. [Google Scholar]
- Kaiser HF. The varimax criterion for analytic rotation in factor analysis. Psychometrika. 1958;23:187–200. [Google Scholar]
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- Lebowitz BD. Clinical trials in late life: New science in old paradigms. The Gerontologist. 2004;44:452–458. doi: 10.1093/geront/44.4.452. [DOI] [PubMed] [Google Scholar]
- Lieberman MA, Fisher L. The effects of family conflict resolution and decision making on the provision of help for an elder with Alzheimer's disease. The Gerontologist. 1999;39:159–166. doi: 10.1093/geront/39.2.159. [DOI] [PubMed] [Google Scholar]
- Lindahl KM. Methodological issues in family observational research. In: Kerig PK, Lindahl KM, editors. Family observational coding systems: Resources for systemic research. Erlbaum; Mahwah, NJ: 2001. pp. 23–32. [Google Scholar]
- Majerovitz SD. Role of family adaptability in the psychological adjustment of spouse caregivers to patients with dementia. Psychology and Aging. 1995;10:447–457. doi: 10.1037//0882-7974.10.3.447. [DOI] [PubMed] [Google Scholar]
- McCubbin HI, Patterson JM. The family stress process: The double ABCX model of adjustment and adaptation. In: McCubbin HI, Sussman M, Patterson J, editors. Social stress and the family: Advances and developments in family stress theory and research. Haworth Press; New York: 1983. pp. 7–37. [Google Scholar]
- McGraw KO, Wong SP. Forming inferences about some intraclass correlation coefficients. Psychological Methods. 1996;1:30–46. [Google Scholar]
- Minuchin S. Families and family therapy. Harvard University Press; Cambridge, MA: 1974. [Google Scholar]
- Minuchin S, Rosman BL, Baker L. Psychosomatic families: Anorexia nervosa in context. Harvard University Press; Cambridge, MA: 1978. [Google Scholar]
- Mitrani VB, Perez M. Structural/strategic family therapy. In: Sexton TL, Weeks G, Robbins MS, editors. Handbook of family therapy. Brunner Routledge; New York: 2003. pp. 177–200. [Google Scholar]
- Mitrani VB, Szapocznik J, Robinson C. Structural ecosystems therapy with seropositive African American mothers. In: Pequegnat W, Szapocznik J, editors. Inside families: The role of families in preventing and adapting to HIVIAIDS. National Institute of Mental Health; Rockville, MD: 2000. pp. 243–280. [Google Scholar]
- Muthén LK, Muthén BO. How to use a Monte Carlo study to decide on sample size and determine power. Structural Equation Modeling. 2002;9:599–620. [Google Scholar]
- Nunnally J, Bernstein I. Psychometric theory. 3rd ed. McGraw-Hill; New York: 1994. [Google Scholar]
- Ory MG, Hoffman RR, Yee JL, Tennstedt S, Schulz R. Prevalence and impact of caregiving: A detailed comparison between dementia and mondementia caregivers. The Gerontologist. 1999;39:177–185. doi: 10.1093/geront/39.2.177. [DOI] [PubMed] [Google Scholar]
- Pagel MD, Erdly WW, Becker J. Social networks: We get by with (and in spite of) a little help from our friends. Journal of Personality and Social Psychology. 1987;53:793–804. doi: 10.1037//0022-3514.53.4.793. [DOI] [PubMed] [Google Scholar]
- Patterson J. Families experiencing stress: I. The Family Adjustment and Adaptation Response Model; II. Applying the FAAR Model to health-related issues for intervention and research. Family Systems Medicine. 1988;6:202–237. [Google Scholar]
- Pearlin L, Mullan J, Semple S, Skaff M. Caregiving and the stress process: An overview of concepts and their measurements. The Gerontologist. 1990;30:583–594. doi: 10.1093/geront/30.5.583. [DOI] [PubMed] [Google Scholar]
- Peterson J, Hawley DR. Effects of stressors on parenting attitudes and family functioning in a primary prevention program. Family Relations. 1998;47:221–227. [Google Scholar]
- Pillemer K, Suitor JJ, Wethington E. Integrating theory, basic research, and intervention: Two case studies from caregiving research. The Gerontologist. 2003;43:19–28. doi: 10.1093/geront/43.suppl_1.19. [DOI] [PubMed] [Google Scholar]
- Radloff L. The Center for Epidemiological Studies Depression Scale: A self-report depression scale for research in the general population. Applied Psychological Measurements. 1977;3:385–401. [Google Scholar]
- Radloff LS, Teri L. Use of the Center for Epidemiological Studies–Depression Scale with older adults. Clinical Gerontologist. 1986;5(1–2):119–136. [Google Scholar]
- Rankin ED, Haut MW, Keefover RW. Current marital functioning as a mediating factor in depression among spouse caregivers in dementia. Clinical Gerontologist. 2001;23(34):27–44. [Google Scholar]
- Schulz R, Visitainer P, Williamson GM. Psychiatric and physical morbidity effects of caregiving. Journal of Gerontology. 1990;45:181–191. doi: 10.1093/geronj/45.5.p181. [DOI] [PubMed] [Google Scholar]
- Schulz R, Williamson GM. Health effects of caregiving: Prevalence of mental and physical illness in Alzheimer's caregivers. In: Light E, Niederehe G, Lebowitz BD, editors. Stress effects on family caregivers of Alzheimer's patients: Research and interventions. Sprague; New York: 1994. pp. 38–63. [Google Scholar]
- Semple SJ. Conflict in Alzheimer's caregiving families: Its dimensions and consequences. The Gerontologist. 1992;32:648–655. doi: 10.1093/geront/32.5.648. [DOI] [PubMed] [Google Scholar]
- Speice J, Shields CG, Blieszner R. The effects of family communication patterns during middle-phase Alzheimer's disease. Families, Systems & Health: The Journal of Collaborative Family Health Care. 1998;16:233–248. [Google Scholar]
- Spielberger CD. Preliminary manual for the State-Trait Personality Inventory (STPI) University of South Florida; Tampa: 1979. [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene PR, Vagg PR, Jacobs GA. State Trait Anxiety Inventory for Adults (STAIS-AD) Manual. Consulting Psychologists Press; Palo Alto, CA: 1983. [Google Scholar]
- Szapocznik J, Perez-Vidal A, Brickman A, Foote FH, Santisteban D, Hervis OE, et al. Engaging adolescent drug abusers and their families into treatment: A strategic structural systems approach. Journal of Consulting & Clinical Psychology. 1988;56:552–557. doi: 10.1037//0022-006x.56.4.552. [DOI] [PubMed] [Google Scholar]
- Szapocznik J, Rio AT, Hervis OE, Mitrani VB, Kurtines WM, Faraci AM. Assessing change in family functioning as a result of treatment: The Structural Family Systems Rating Scale (SFSR) Journal of Marital and Family Therapy. 1991;17:295–310. [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. 3rd ed. HarperCollins; New York: 1996. [Google Scholar]
- Teri L, Truax P, Logsdon R, Uomoto J, Zarit S, Vitaliano PP. Assessment of behavioral problems in dementia: The Revised Memory and Behavior Problems Checklist. Psychology and Aging. 1992;31:76–83. doi: 10.1037//0882-7974.7.4.622. [DOI] [PubMed] [Google Scholar]
- Wisniewski S, Belle S, Coon D, Marcus S, Ory M, Burgio L, et al. The Resources for Enhancing Alzheimer's Caregiver Health (REACH): Project design and baseline characteristics. Psychology and Aging. 2003;18:375–384. doi: 10.1037/0882-7974.18.3.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: Correlates of feelings of burden. The Gerontologist. 1980;20:649–654. doi: 10.1093/geront/20.6.649. [DOI] [PubMed] [Google Scholar]