WHEN WE THINK OF THE WORLD Health Organization (WHO), a number of dramatic moments and milestones leap to mind: the launching of the new international health organization in 1948 with the stirring preamble to its constitution; the visionary Alma Ata Declaration of 1978; the announcement in 1980 of the eradication of smallpox, the first disease to be eliminated in human history1; Jonathan Mann’s effective leadership of WHO’s international campaign against HIV/AIDS2; and WHO’s swift responses to severe acute respiratory syndrome (SARS) and avian flu before these could grow into global pandemics.3,4 In this “Images of Health” column, we capture a few other moments in the history of WHO to provide a fuller picture of its activities and achievements over the past 60 years.
When WHO began in the late 1940s, one of its most important functions was to coordinate international epidemiological surveillance activities. These can be traced formally to the turn of the 20th century, when the Office Internationale d’Hygiène Publique (OIHP), created in Paris in 1907, and the League of Nations Health Organization (LNHO), established in Geneva in 1922, gave high priority to epidemiological intelligence, including the collection and timely publication of data from many parts of the world.5–7 In 1926, OIHP and LNHO agreed to cooperate in the maintenance of an Eastern Bureau for International Epidemiological Intelligence in Singapore to serve as a node in an information network reaching across Asia, Australia, and the Pacific.8 During World War II, the United Nations Relief and Rehabilitation Administration took over many of the functions of OIHP, LNHO, and the Eastern Bureau, and in the immediate postwar period arranged to transfer these functions to the newly created WHO.9 Image 1 ▶ shows an early WHO staff worker in Geneva collecting epidemiological information from all over the world.
IMAGE 1—
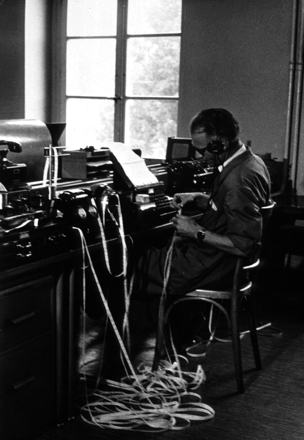
Epidemiological information from around the world being received in the Geneva post office.
Source. Courtesy of the WHO.
By the mid-1950s, malaria had become a major target of WHO’s efforts. The main weapons of the Global Program for Malaria Eradication were new drugs, especially choloroquine, and the spraying of houses with DDT in intense, time-limited campaigns. In image 2 ▶, workers are shown spraying the inside of a house in Thailand with DDT. WHO believed that the developing resistance of the Anopheles mosquito to DDT was caused by insufficient applications of the insecticide, lending additional urgency to the effort. Eradication was then seen as the only way to deal with the worldwide problem of malaria.10
IMAGE 2—

Spraying for mosquitoes inside a Thai household.
Source. Courtesy of the WHO.
Serious problems emerged for eradication in the mid-1960s.11 Among these was a greater than expected level of resistance to insecticides in some Anopheles. In addition, as Rachel Carson’s 1962 book Silent Spring argued, insecticides were toxic and, when misused, produced environmental contamination.12 It would prove impossible to eradicate malaria, and even in areas where the disease had temporarily been brought under control, it soon began to reemerge as a major threat. In 1969, the World Health Assembly concluded that malaria could not be eliminated in the absence of comprehensive rural health services.
In the late 1960s and early 1970s, there was a growing understanding of the need for an underlying infrastructure of health services and health education to support a variety of programs in disease prevention and health promotion. Within this public health framework, specific disease control efforts would not be isolated vertical programs, but would be integrated into a broad range of health and social services. In the 1970s, the example of the barefoot doctors in China captured the public imagination as an example of what relatively untrained health practitioners could do with simple technical tools and strong community support.
Halfdan T. Mahler, a charismatic Danish physician, became director-general of WHO in this time of considerable international change and ferment. Under Mahler’s leadership, the promise of basic health services was transmuted into a broader conception of community-based, development-related primary health care, as crystallized during the conference at Alma Ata, in what is now Kazakhstan, in 1978 and announced in the famous declaration of “Health for All.” In this conception of primary health care, health work is understood to be part of socioeconomic development; it was based on broad community participation and included village health workers, traditional healers, and grass-roots social mobilization. Image 3 ▶ shows village health workers attending a course on primary health care in Torodi, Niger, in West Africa.
IMAGE 3—
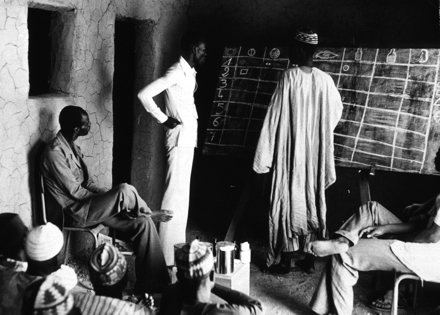
Village health workers attending a course on primary health care in Torodi, Niger.
Source. Courtesy of the WHO.
Closely related to efforts in primary care was WHO’s activity in the field of maternal and child health. Beginning in the 1950s and 1960s, WHO worked to reduce high maternal mortality and infant death rates in developing nations by setting up maternal and child health services and programs for the training of midwives and traditional birth attendants, encouraging prenatal care for pregnant women, referring women with high-risk pregnancies to hospital care, and working to improve general health and nutrition levels.13
In the 1970s, WHO worked increasingly with other agencies—most notably, UNICEF—on collaborative programs. Pursuing the ideal of multisectoral health improvement and development, agencies found creative ways to pool their resources and work side by side on child health and nutrition, clean water, and access to health services and family planning. Image 4 ▶, from a joint WHO–UNICEF campaign, shows the result of such collaboration: a healthy mother and child.
IMAGE 4—
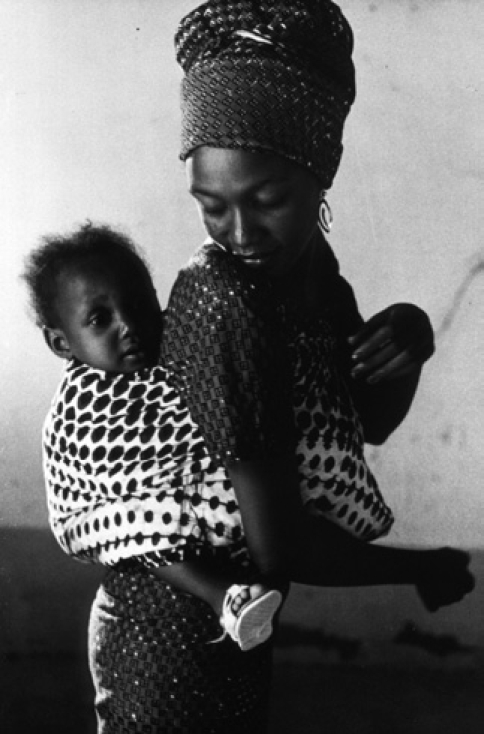
A healthy mother and child. WHO photograph by M. Jacot.
Note. Courtesy of the WHO.
Relations between WHO and UNICEF were, in reality, marked by alternating periods of cooperation and tension. James Grant, the executive director of UNICEF appointed after the Alma Ata Conference, considered WHO’s broad and visionary approach to primary health care to be too idealistic. Instead, he subscribed to an “interim” strategy of selective primary health care.14 This consisted of simple, inexpensive interventions, such as the control of infant diarrheal diseases with salt-and-sugar packets that could be mixed with water to make oral rehydration solution (Image 5 ▶). These sorts of interventions—cost-effective and easy to monitor and evaluate—attracted the support of many donors and bilateral agencies.
IMAGE 5—
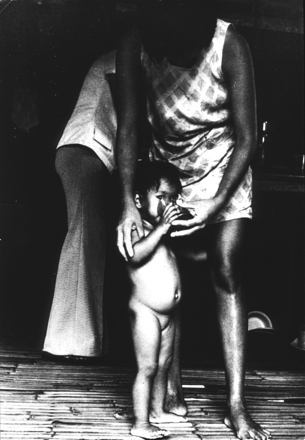
Child drinking oral rehydration solution.
Source. WHO photograph by B. Cvjetanovic, courtesy of the WHO.
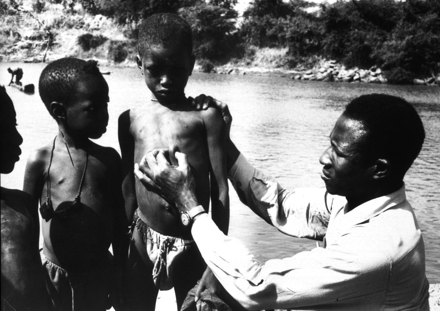
Immunization against the diseases of childhood was another simple and effective intervention as part of selective primary health care. In the new political context of the 1980s, with conservative regimes, the emergence of neoliberalism, and the consequent reduction of health budgets, immunization proved a popular and successful initiative. A WHO Expanded Program on Immunization (EPI; Image 6 ▶) was initially designed in the 1970s but drew increased support in the 1980s after WHO announced the successful worldwide eradication of smallpox. EPI contributed to the technology of vaccines and the social organization of vaccination campaigns through such mechanisms as national vaccination days.
IMAGE 6—
Prevention is essential to protect life; there is no substitute for vaccination and immunization.
Source. WHO/UNICEF photograph, courtesy of the WHO.
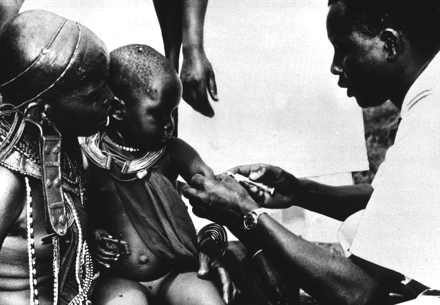
WHO’s post–Alma Ata achievements were not limited to immunization programs. In the late 1980s, onchocerciasis, also known as river blindness, was brought under control in West and Central Africa.15 In the mid-1970s when WHO first initiated the Onchocerciasis Control Program (OCP), over 1 million people suffered from the disease. Partnering with OCP were the World Bank and a recently created WHO Special Program for Research and Training in Tropical Diseases. The charismatic Gambian physician Ebrahim M. Samba led the program to success.16 The OCP implemented a 10-year strategy, trained specialists from and for Africa, and relied on trained village health workers organized in mobile teams to destroy populations of black flies. New filaricides and insecticides helped with vector control. Merck & Co. provided the drug, ivermectin, free of charge to those needing treatment. In image 7 ▶, we see a physician examining a nodule on the chest of a young boy—a characteristic of onchocerciasis.
IMAGE 7—
Nodules, or lumps in the skin, produced by parasitic worms are one of the early signs of onchocerciasis.
Source. WHO photograph by P. A. Pittet, courtesy of the WHO.
In the 1990s, WHO entered a new phase of its history, as a leader of “global health.” This concept emerged in the latter part of the 20th century as a replacement for the earlier notion of “international health,” which had emphasized intergovernmental cooperation and a particular structure of organizations and agencies.17 “Global health” emphasized a new institutional fluidity in response to the increasing economic, political, and social interdependence of the modern world and the resulting common dangers and opportunities in the form of diseases, products, and ideas that readily crossed borders.
Much of the impetus for global health came from the World Bank, which carved out a major new role for itself in the late 1980s and early 1990s, when WHO was mired in particularly difficult economic and organizational problems. In 1990, the Bank’s loans for health surpassed WHO’s total budget. But WHO struggled to regain standing as the arbiter and organizer of global health (Image 8 ▶). It was relatively successful under the leadership of Gro Harlem Brundtland, director-general from 1998 to 2003. As the former prime minister of Norway and a physician and public health official, Brundtland brought a formidable reputation and expertise to her position. She was familiar with the global thinking of the environmental movement as former chair of the UN World Commission on Environment and Development, which produced the Brundtland Report that led to the Earth Summit of 1992. By general agreement, Brundtland succeeded in repositioning WHO as a respected leader in the field of global health.
IMAGE 8—
Our Planet, our health: think globally, act locally.
Source. WHO Health Day poster, 1990, courtesy of the WHO.
In his brief tenure as director-general before his sudden and untimely death, J. W. Lee continued the strategy, with emphasis on such initiatives as “3 × 5”—the effort to use antiretrovirals to treat 3 million HIV-infected people by 2005. Margaret Chan, fresh from the successful campaign to control avian influenza and SARS, became the new director-general in November 2006. Building on the success of programs to contain communicable diseases, she is strengthening international surveillance systems and emphasizing the need to build up a strong infrastructure of public health and health services in all of the member countries. She is also bringing WHO into a new position of leadership in dealing with the likely health effects of global warming.18
Contributors All authors contributed equally to the research and writing of this article.
References
- 1.Fenner F, Henderson DA, Arita I, Je zek Z, Ladnyi ID. Smallpox and Its Eradication. Geneva, Switzerland: World Health Organization; 1988.
- 2.Tarantola D, Gruskin S, Brown TM, Fee E. Jonathan Mann: founder of the health and human rights movement. Am J Public Health. 2006;96:1942–1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abraham T. Twenty-First Century Plague: The Story of SARS. Baltimore, MD: Johns Hopkins University Press; 2005.
- 4.Tambyah P, Leung P-C. Eds. Bird Flu: A Rising Pandemic in Asia and Beyond? Singapore: World Scientific; 2006.
- 5.Goodman N. International Health Organizations and Their Work. London, England: J. & A. Churchill; 1952.
- 6.Durbin M. The League of Nations Health Organization. In: Weindling P, ed. International Health Organizations and Movements, 1918–1939. Cambridge, England: Cambridge University Press; 1995:56–80.
- 7.Borowy I. World health in a book—the international health yearbooks. In: Borowy I, Gruner WD, eds. Facing Illness in Troubled Times, 1918–1939. Frankfurt am Main, Germany: Peter Lang; 2005:85–128.
- 8.Manderson L. Wireless wars in the eastern arena: epidemiological surveillance, disease prevention and the work of the Eastern Bureau of the League of Nations Health Organization, 1925–1942. In: International Health Organizations and Movements, 1919–1939. New York, NY: Cambridge University Press; 1995:109–133.
- 9.Sawyer W. Achievements of UNRRA as an international health organization. Am J Public Health. 1947;37:41–58. [PMC free article] [PubMed] [Google Scholar]
- 10.Packard RM. “No other logical choice”: global malaria eradication and the politics of international health in the post-war era. Parassitologia. 1998;40:217–229. [PubMed] [Google Scholar]
- 11.Vargas L. The phenomenon of resistance to insecticides in Anopheles transmitters of malaria [in Spanish]. Salud Publica Mex. 1973;12:21–27. [PubMed] [Google Scholar]
- 12.Carson R. Silent Spring. Cambridge, MA: Riverside Press; 1962.
- 13.Barton E. Maternal and child health in the 1950s and 1960s. World Health Forum. 1998;19:436–440. [PubMed] [Google Scholar]
- 14.Cueto M. The origins of primary health care and selective primary health care. Am J Public Health. 2004;94:1864–1874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization. The prevention of blindness. WHO Chron. 1976;30:391–397. [PubMed] [Google Scholar]
- 16.Godlee F. The World Health Organization in Africa. Brit Med J. 1994; 309:553–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brown T, Cueto M, Fee E. The World Health Organization and the transition from “international” to “global” public health. Am J Public Health. 2006;96:62–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chan M. Climate change and health. Presented at: 2007 David E. Barmes Global Health Lecture, National Institutes of Health, December 10, 2007; Bethesda, MD.


