Abstract
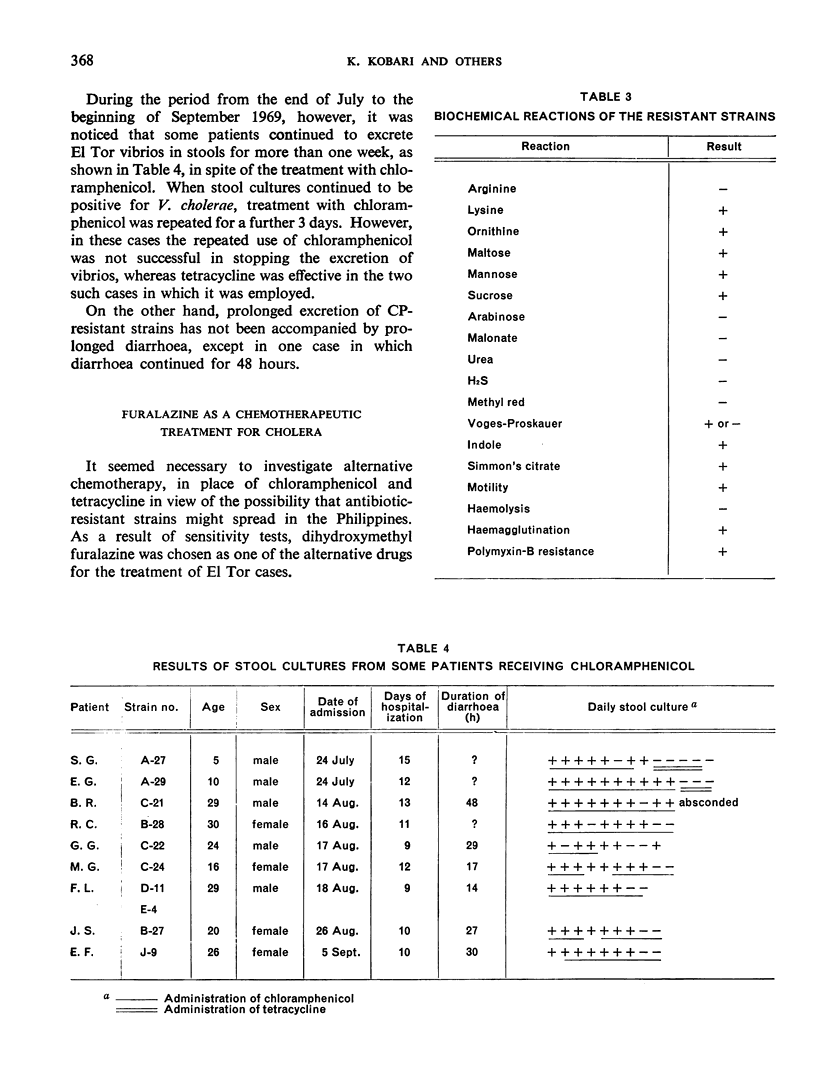
Among 1109 patients with bacteriologically confirmed El Tor cholera admitted to the San Lazaro Hospital, Manila, in 1969, 11 patients continued to excrete vibrios of the same biotype and serotype in stools for more than 1 week in spite of antibiotic treatment.
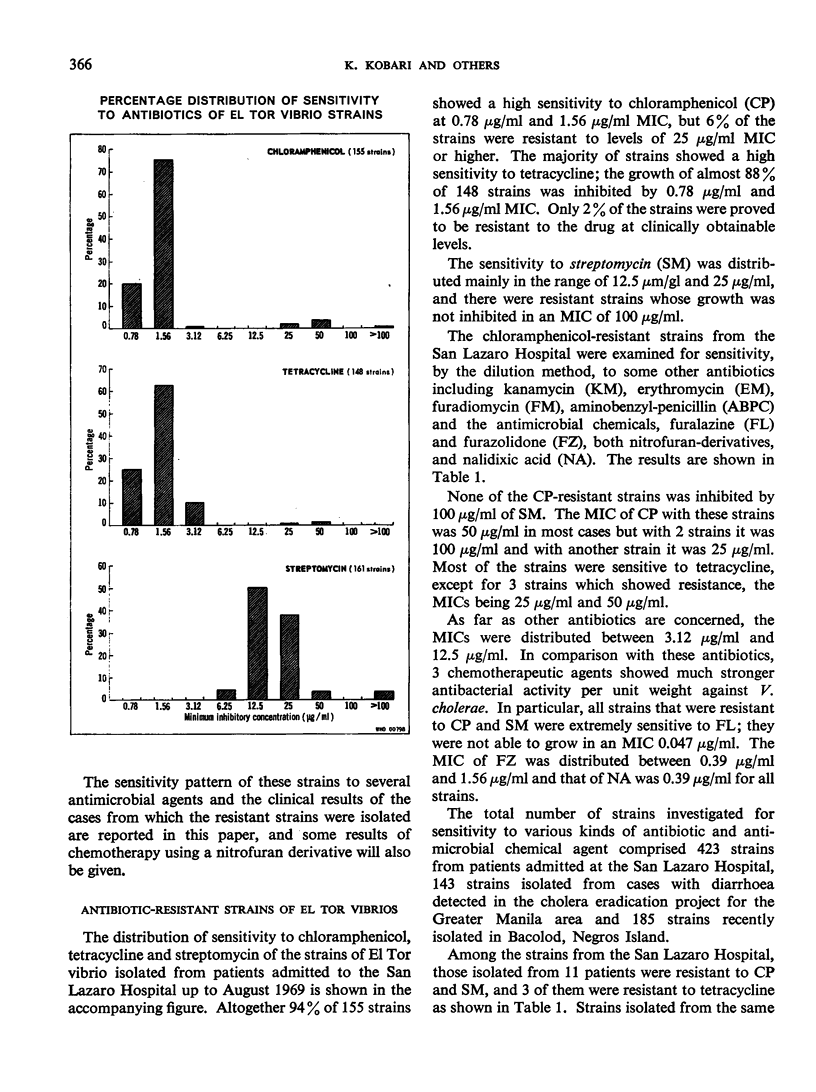
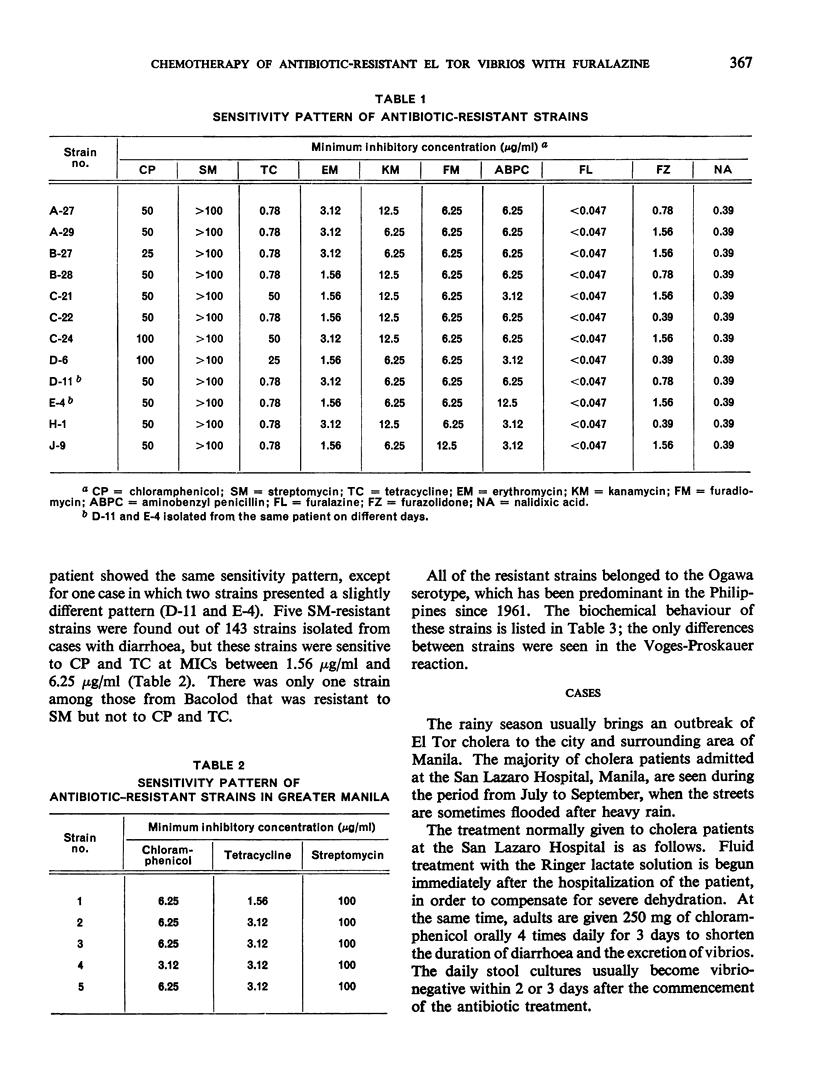
The strains isolated from these patients all belonged to the Ogawa serotype and were all highly resistant to streptomycin and chloramphenicol, and a few of them were resistant also to tetracycline. Other streptomycin-resistant strains of El Tor vibrio were detected, 5 in the Greater Manila area and 1 in Bacolod.
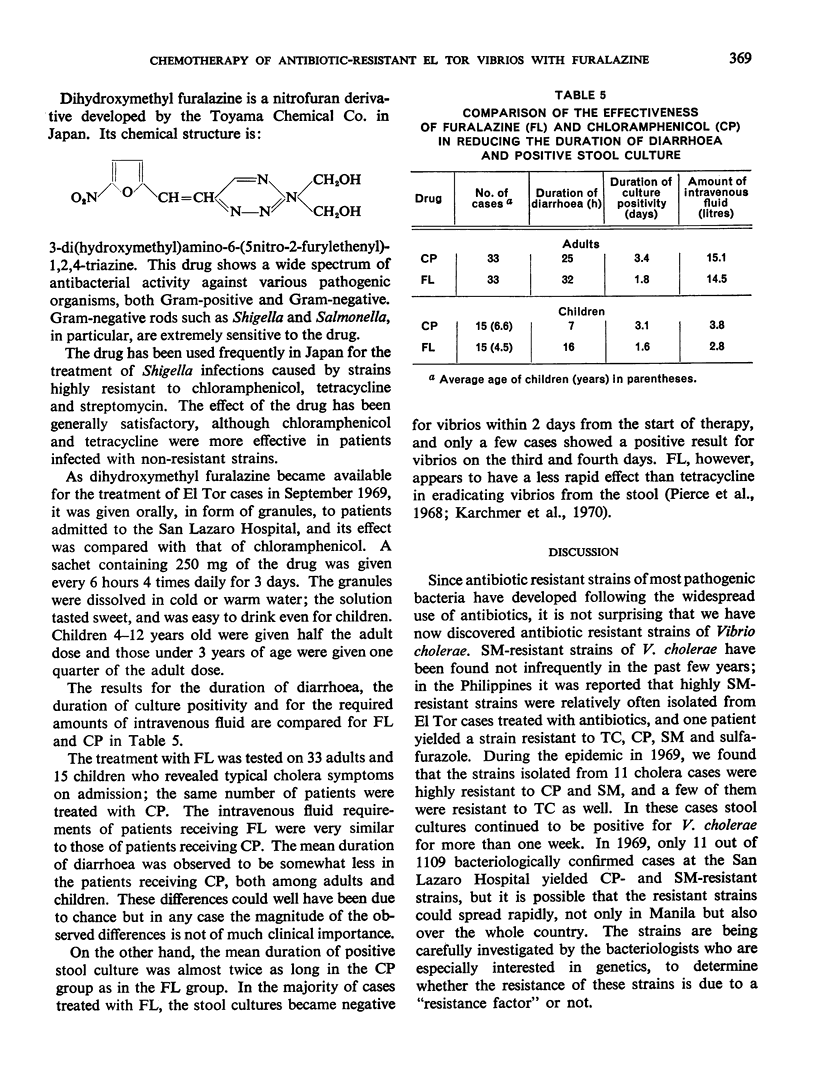
The antibiotic-resistant strains showed a high sensitivity to 3 kinds of antimicrobial chemicals, particularly dihydroxymethyl furalazine.
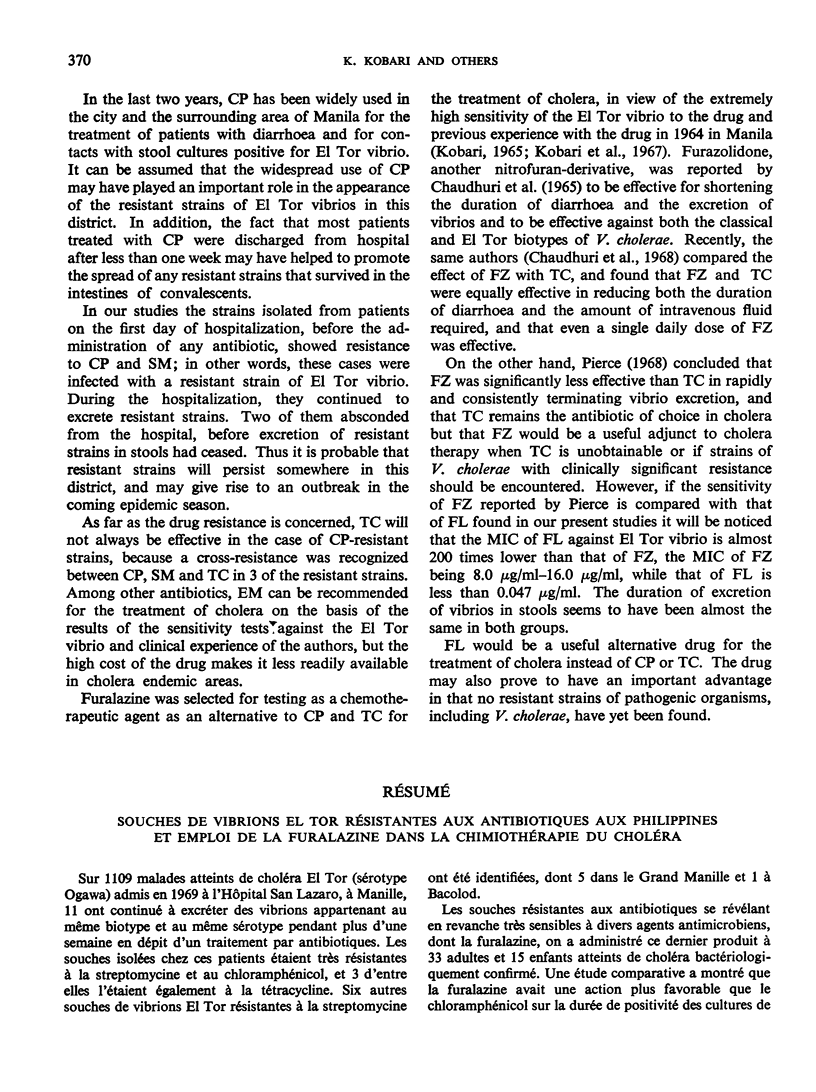
Furalazine was given to 33 adults and 15 children with bacteriologically confirmed cholera, and its effect in reducing the duration of diarrhoea and excretion of vibrios was investigated in comparison with the same number of cases treated with chloramphenicol. Furalazine was more effective in reducing the duration of positive stool culture than chloramphenicol, and the two antimicrobial agents were equally effective in decreasing intravenous fluid requirements.
Since furalazine was satisfactory in reducing the duration of diarrhoea and excretion of vibrios in stools, and since no resistant strains were found, the drug could be recommended as an alternative to chloramphenicol and tetracycline in the treatment of cholera.
Full text
PDF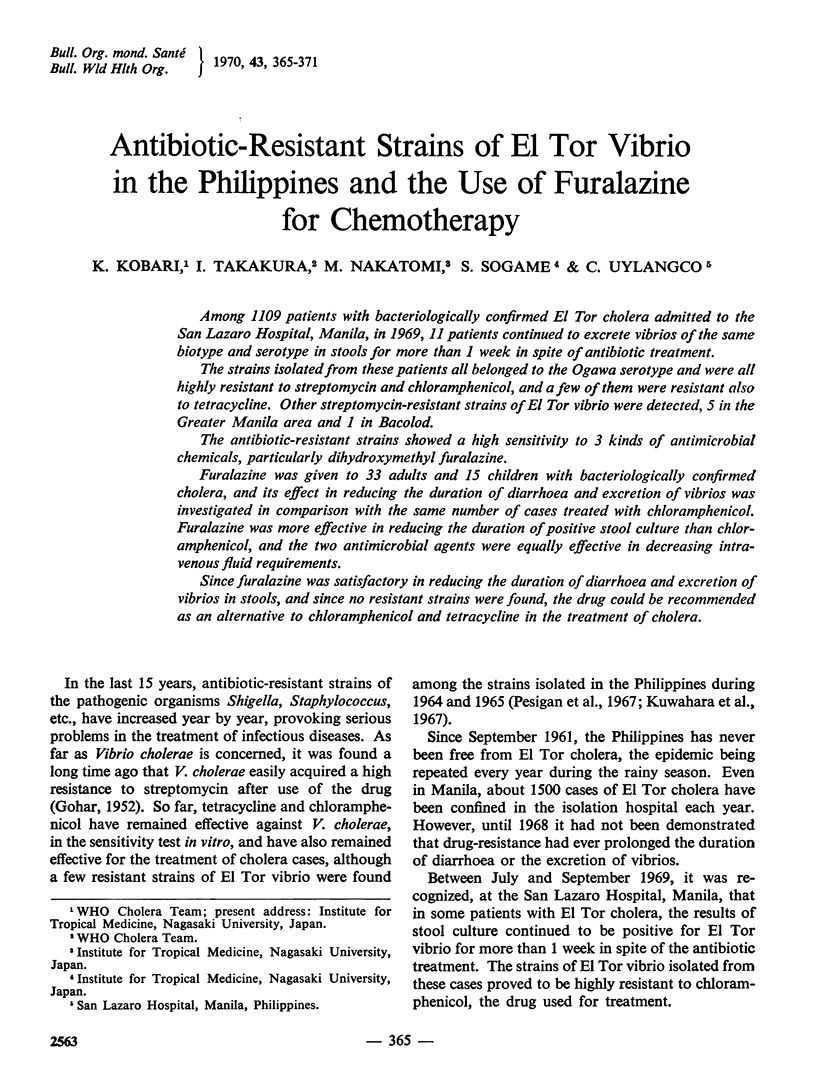
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Chaudhuri R. N., Neogy K. N., Sanyal S. N., Gupta R. K., Manji P. Furazolidone in the treatment of cholera. Lancet. 1968 Feb 17;1(7538):332–333. doi: 10.1016/s0140-6736(68)90796-4. [DOI] [PubMed] [Google Scholar]
- GOHAR M. A., EL-MOFTY A., EISSA A. A., MOUSA A. H., SOROUR A., DOSS H., GOMA T., ABOU EL-WAFA M., EL-AZHARI A., MITRI S. Some observations on the carrier state in cholera. J Trop Med Hyg. 1952 Nov;55(11):241–245. [PubMed] [Google Scholar]
- Karchmer A. W., Curlin G. T., Huq M. I., Hirschhorn N. Furazolidone in paediatric cholera. Bull World Health Organ. 1970;43(3):373–378. [PMC free article] [PubMed] [Google Scholar]
- Kobari K., Uylangco C., Vasco J., Takahira Y., Shimizu N. Observations on cholera treated orally and intravenously with antibiotics. With particular reference to the number of vibrios excreted in the stool. Bull World Health Organ. 1967;37(5):751–762. [PMC free article] [PubMed] [Google Scholar]
- Kuwahara S., Goto S., Kimura M., Abe H. Drug-sensitivity of El Tor vibrio strains isolated in the Philippines in 1964 and 1965. Bull World Health Organ. 1967;37(5):763–771. [PMC free article] [PubMed] [Google Scholar]
- Pesigan T. P., Gomez C. Z., Barua D. The drug-sensitivity of isolates from cholera El Tor patients in San Lazaro Hospital, Manila. Bull World Health Organ. 1967;37(5):814–815. [PMC free article] [PubMed] [Google Scholar]
- Roberts H. J. Amphetamine. Lancet. 1965 Oct 30;2(7418):909–910. doi: 10.1016/s0140-6736(65)92549-3. [DOI] [PubMed] [Google Scholar]


