Suicide and suicidal behavior is highly familial, and appears to be familially transmitted independently from the familial transmission of psychiatric disorder per se (1). Adoption, twin, and family studies support the view that the etiology of the familial transmission of suicidal behavior is at least in part genetic, and may be mediated by the transmission of intermediate phenotypes, such as impulsive aggression. In addition, there may be environmental causes for familial transmission, including imitation, and the intergenerational transmission of family adversity. In this review, we cover the evidence supporting the familial transmission of suicidal behavior, possible genetic and environmental explanations for this phenomenom, describe putative intermediate phenotypes, and discuss the contributory roles of early child-rearing and concurrent familial environmental stressors to suicidal risk. A better understanding of the mechanisms for the familial transmission of suicidal behavior can help to shed light on etiology, identify individuals at high risk for the development of incident suicidal behavior, and frame targets for intervention and prevention.
Adoption studies (see Table 1)
Table 1.
Schulsinger et al. (1979): Adoption Study: Rates of Suicide in Biological Versus Adoptive Relatives of Adoptees who Committed Suicide and of Live Adoptee Controls*
| Adopted | Index cases | Suicide/biological relatives | Suicide/adopted relatives |
|---|---|---|---|
| Suicide | 57 | 12/269* | 0/148 |
| Controls | 57 | 2/269 | 0/150 |
P < 0.01.
From Schulsinger et al. A family study of suicide. In: Schou M, Stromgren E, eds. Origin, Prevention and Treatment of Affective Disorders. London: Academic Press 1979: 277–287, with permission.
Three adoption studies have been conducted, all using the same Danish adoption registry. Kety et al., in a study designed to examine the genetics of schizophrenia and mood disorders, found a non-significant trend towards higher concordance for suicide in biological, compared to adoptive relatives of adoptees who committed suicide (2). Subsequently, a second study compared the rates of suicide among the biological and adoptive relatives of adoptees who committed suicide vs. biological and adoptive relatives of a matched living adoptee control group in Denmark (3). This study found a six-fold higher rate of suicide in the biological relatives of the suicide vs. those of the control adoptees, and an absence of suicide among the adopted relatives of the suicide vs. control adoptees supporting a genetic rather than environmental etiology (see Table 1). The rate of suicide was higher in the biologic relatives of suicide adoptees regardless of whether the adoptees were psychiatric patients or not. However, it was not possible to determine if the genetic liability to suicide was attributable to the transmission of major psychiatric disorders or to a suicide diathesis per se.
In a third adoption study using this registry, a comparison of biological and adoptive relatives of adult adoptees with mood disorder and matched unaffected adoptees were examined (4), revealed a 15-fold increase in suicide among the biological relatives of the mood-disordered adoptees vs. those of the unaffected adoptees (4). This finding supports the role of mood disorder in the genetics of suicide. However, the greatest increased risk for suicidal behavior was found in the relatives of those probands with “affect reaction,” a diagnosis akin to borderline personality disorder, suggesting that impulsive-aggressive personality traits may play a role in familial aggregation of suicidal behavior (see Table 2).
Table 2.
Incidence of Suicide in Biological Relatives of Depressive and Control Adoptees*
| Diagnosis in adoptee | Incidence of suicide in biological relative (%) | OR | P |
|---|---|---|---|
| Affective reaction | 5/62 (8.1) | 30.3 | < 0.0001 |
| Bipolar depression | 4/71 (5.6) | 20.6 | 0.003 |
| Neurotic depression | 3/122 (2.5) | 8.7 | 0.056 |
| Unipolar depression | 3/132 (2.3) | 8.0 | 0.066 |
| No mental illness | 1/346 (0.3) | - | - |
From Wender et al. Psychiatric disorders in the biological and adoptive families of adopted individuals with affective disorders. Arch Gen Psychiatry 1986;43:923–929, with permission.
Taken together, these studies support a strong role for genetics in explaining the familial concordance of completed suicide. Limitations of these studies include restriction to data gathered through routine medical records, and lack of systematic assessment of suicide attempts as well as completions. Thus, while these studies show there are genetic factors explaining the familial aggregation of suicide, they do not shed a great deal of light on what factors might be involved in familial transmission.
Twin studies (see Tables 3 and 4)
Table 3.
Twins Studies in Which one Twin has Committed Suicide*
| No. of twins (%) concordant for suicide behavior
|
|||
|---|---|---|---|
| Study | MZ | DZ | P |
| Haberlandt [1967] | 14/51 (17.6)a | 0/98 (0) | < 0.001 |
| Juel-Nielsen [1970] | 4/19 (21.1) | 0/58 (0) | < 0.003 |
| Zair [1981] | 1/1 (100) | 0/0 (0) | NS |
| Roy et al. [1991] | 7/62 (11.3) | 2/114 (0) | < 0.01 |
| Roy et al. [1995] | 10/26 (38.5)b | 0/9 (1.7) | < 0.04 |
| Roy and Segal [2001] | 4/13 (30.7)c | 0/15 (0) | < 0.04 |
| Total | 40/172 (23.0) | 2/294 (0.7) | < 0.00001 |
Five pairs, co-twin attempted suicide.
Ten pairs, co-twin attempted suicide.
Three pairs, co-twin attempted suicide.
From Brent and Mann. Family genetic studies, suicide, and suicidal behavior. Am J Psychiatry 2005;133C:13–24, with permission.
Table 4.
Twin Studies of the Genetic Epidemiology of Suicidal Behavior*
| Concordance (%)
|
Concordance (AOR)
|
Heritability (%)
|
||||||
|---|---|---|---|---|---|---|---|---|
| Study | N | Gender | MZ | DZ | MZ | DZ | Ideation | Attempt |
| Statham | 5,995 | Both | 23.1 | 0 | 3.8 | - | 43 | 55 |
| Glowinski | 3,416 | Female | 25 | 12.8 | 5.6 | 4.0 | - | 48 |
| Fu | 7,744 | Male | - | - | 12.1 | 7.4 | 43 | 30 |
| 36 | 17a | |||||||
Adjusted for heritability of other risk factors.
From Brent and Mann. Family genetic studies, suicide, and suicidal behavior. Am J Psychiatry 2005;133C:13–24, with permission.
In their review of twin case reports for suicide, Roy and Segal found an increased concordance for suicide in monogyzotic (MZ) vs. dizygotic twins (DZ) (14.9% vs. 0.7%), consistent with Tsuang’s original observations (5). Roy et al. found an even higher concordance rate for suicide attempt in the surviving monozygotic twin of the co-twin’s suicide in MZ vs. DZ twins (38% vs. 0%), supporting the view that the clinical phenotype for concordance included both completed suicide and suicide attempts (6;7). Because these meta-analyses use reported case series, they are not necessarily representative of all twin pairs affected by suicide. The differential concordance rate for suicide for MZ vs. DZ twins does not appear to be due to greater bereavement reactions in MZ twins (8), since the risk of suicide attempt after the non-suicide death of a co-twin is similar in MZ vs. DZ twins (1.4% vs. 3.3%).
Three twin studies demonstrate familial transmission for suicidal behavior that cannot be explained by the transmission of other psychopathology (9–11). The heritability of suicidal behavior ranging from ideation to attempts ranged between 38% and 55%. While there appears to be overlap between the heritability of suicidal ideation and of actual suicidal behavior, there is a distinct heritable component of suicide attempts demonstrated in two of these studies (9;10). In one study, the heritability of suicidal behavior was demonstrated, even after controlling for the heritability of psychiatric disorders (10). Twin studies generally provide more detailed assessment than adoption studies, and allow for an assessment of environmental and genetic contributors to concordance. However, unless twin studies are combined with adoption studies (i.e., comparison of twins adopted away to different parents), it is difficult to definitively differentiate shared environmental from genetic effects. For example, in a twins-adopted away design, components of maternal behavior previously considered “environment” were explained by genetic concordance of MZ twins eliciting similar maternal responses from unrelated mothers (12). A second limitation is that MZ vs. DZ concordance may be differentially affected by shared or distinct perinatal experiences (13).
Family Studies
Family studies compare the rate of suicide or suicidal behavior in the relatives of a proband with suicidality to the rate of suicide or suicidal behavior in the relatives of probands without suicidality. Studies have varied in outcome (family history of completed suicide, attempted suicide, or both), choice of proband (either completed or attempted suicide), choice of comparison group (community or psychiatric control), and method of assessment of family loading (record review, family history, or direct interview) (14–40). Among the most convincing of these studies have been those based on large population registries, which have shown concordance in death by suicide between parents and children, even after controlling for psychiatric diagnosis and treatment (37;38;41).
Despite variations in methodology, the results are remarkably similar across studies, consistently showing that suicidal behavior aggregates within families. Those studies that adjusted statistically for the familial transmission of psychiatric disorder and other risk factors generally found a familial effect for suicidal behavior that still persisted even after statistical adjustment with effects ranging from a 2- to 12-fold elevation in rates after adjustment (23;24;26;28). These studies support the view that the clinical phenotype of suicidal behavior that is familially transmitted includes both suicide attempt and suicide completion, since the rate of suicide is elevated in the families of attempters, and the rate of attempted suicide is elevated in the families of suicide completers.
Studies of the Risk of Suicide in Probands with Completed Suicide (see Table 5)
Table 5.
Studies of the Risk of Familial Suicide in the Relatives of Suicide Probands
| Study | Year | Probands | Controls | Sample size proband/control | OR |
|---|---|---|---|---|---|
| Tsuang | 1985 | Patient suicides | Patient non-suicides | 29/491 | 3.8 |
| Egeland | 1985 | Suicides in Amish studies | Comparison pedigree | - | 4.6 |
| Foster | 1999 | Irish suicides | Attendees in same general practice | 118/118 | 3.0(NS)a |
| Powell | 2000 | Inpatient suicides | Inpatient non-suicides | 112/112 | 4.6a |
| Tsai | 2002 | Bipolar suicides | Bipolar controls | 41/41 | 15.1a |
Adjusted OR.
From Brent and Mann. Family genetic studies, suicide, and suicidal behavior. Am J Psychiatry 2005;133C:13–24, with permission.
In studies that examined the familial rates of completed suicide in the relatives of probands who committed suicide, all show an elevated rate of completed suicide in the relatives of completers vs. relatives of a comparison group, regardless of whether that comparison group consists of psychiatric, general medical, and community controls. Also, these findings are consistent, regardless of whether the probands were drawn from large community pedigrees (14), diagnostically heterogenous inpatients (29;42), community samples (27), or bipolar suicides vs. living bipolar controls (36). Two of the studies showed a significant association between family history of suicide and familial suicide after controlling for other risk factors, stressing the unique contribution of the familial transmission of suicidal behavior to suicidal risk.
Population Registry Studies (see Table 6)
Table 6.
Studies of Suicide Based on Registries and Record Linkage*
| Study | Year | Country | Proband | Control | Sample size proband/controls | AOR |
|---|---|---|---|---|---|---|
| Qin | 2002 | Denmark | Suicides, 9–45 | Matched community control | 4,262/80,238 | 2.6a,b |
| Agerbo | 2002 | Denmark | Suicides, 10–21 | Matched community controls | 496/24,800 | 2.3–4.8a,b,c |
| Qin | 2003 | Denmark | Suicides, all ages | Matched community controls | 21,169/423,128 | 2.1a,b |
| Runeson | 2003 | Sweden | Suicides, all ages | Matched non-suicide deaths | 8,396/7,568 | 2.0b |
Adjusted for previous psychiatric admission/care.
Adjusted for relatives previous psychiatric admission.
OR for suicide in father/mother.
From Brent and Mann. Family genetic studies, suicide, and suicidal behavior. Am J Psychiatry 2005;133C:13–24, with permission.
Four studies using Scandinavian registries report a increased risk of suicide conveyed to a first-degree relative, even after controlling for parental and personal history of inpatient psychiatric treatment (35;37;38;41). In one study, family history of suicide was associated with an increased rate of suicide even compared to those who have had a first-degree relative die from either accidents or homicides, supporting the view that the familial transmission of suicidal behavior is not strongly mediated by bereavement (38). One study found an impact of parental suicide on children aged 10–21 for both maternal and paternal suicide, with an increased risk for suicide in offspring even for maternal loss from qother causes; however, the effect of maternal suicide was greater than maternal loss due to other causes (AOR’s 4.8 vs. 2.06). While such studies have the advantage of large, representative databases, they are limited to the information available in medical records, and assessment of psychiatric disorder is limited to those who received treatment. However, in Scandinavian countries, where access to health care has fewer barriers than in the United States, a treated sample is likely to be more representative than it would be in an American study.
Family studies of suicide probands and familial rates of suicidal behavior (See Table 7)
Table 7.
Family Studies of Rates of Suicidal Behavior in Relatives of Suicide Versus Control Probands*
| Study | Year | Proband | Control | N proband/control | AORa,b |
|---|---|---|---|---|---|
| Brent | 1996 | Adolescent suicides | Matched community controls | 58/55 | 4.3 |
| Gould | 1996 | Adolescent suicides | Matched community controls | 120/147 | 5.1 |
| Cheng | 2000 | Adult suicides | Matched community controls | 113/226 | 5.2 |
| Kim | 2005 | Adult male suicides | Matched community controls | 217/171 | 10.6 |
Chart Review.
FH attempt/completion.
Adapted from Brent and Mann. Family genetic studies, suicide, and suicidal behavior. Am J Psychiatry 2005;133C:13–24, with permission.
Four studies have examined rates of attempted and completed suicide in the families of suicide probands vs. the relatives of community controls (23;24;28;40). Two studies focused on adolescents (23;24), and two on adults (28), one of which focused exclusively on males (40). All found an increased rate of suicidal behavior in the relatives of completers compared to relatives of community controls, even after controlling for differences in rates of psychiatric disorder in probands (23;28;40), parent-child discord (24), and rates of psychiatric disorder in family members (23;24;40). Two studies found that the rates of familial suicidal behavior were most significantly increased in the relatives of the probands with increased levels of aggression or Cluster B personality disorder in probands (23;40), supporting a relationship between the familial transmission of aggression and of suicidal behavior. An increased rate of suicide attempts in the relatives of suicide probands supports the definition of a clinical phenotype of suicidal behavior that includes both attempts and completions. In contrast, suicidal ideation was not increased in relatives of completers after adjusting for rates of psychiatric disorder in relatives (23;40), indicating that suicidal ideation is transmitted along with psychiatric disorder, whereas the tendency to translate that ideation into an actual attempt is co-transmitted with impulsivity and aggression.
Family History of Suicidal Behavior in Suicide Attempt Probands (see Table 8)
Table 8.
Family History Studies of Attempted Suicide Probands*
| Study | Year | Proband | Control | N proband/control | OR |
|---|---|---|---|---|---|
| Garfinkela | 1982 | Adol. attempters in ER | ER non-attempters | 505/505 | 5.4 |
| Roya | 1983 | Adult inpt. attempters | Adult inpt. non-attempts | 243/5,602 | 3.4 |
| Linkowski | 1985 | Adult inpt. attempters | Adult inpt. non-attempts | 239/474 | 2.0–3.5 |
| Mitterauer | 1990 | Manic-depressive attempters | Manic depressive non-attempters | 342/80 | 3.3 |
| Sorenson | 1991 | Suicide attempters | Non-attempters | 93/2,211 | 5.8 |
| Malone | 1995 | Depressed attempters | Depressed non-attempters | 100/100 | 7.6 |
| Roy | 2002 | Alcoholic attempters | Alcoholic non-attempters | 124/209 | 2.4/4.0b |
| Roy | 2001 | Cocaine dependent attempters | Cocaine-defendant non-attempters | 84/130 | 4.5/5.9b |
| Roy | 2002 | Opiate-dependent attempters | Opiate-dependant non-attempters | 105/171 | 2.9/6.0b |
| Roy | 2003 | Substance dependent attempters | Substance dependent non-attempters | 175/274 | 3.2/5.9b |
| Mann | 2005 | Mood disordered attempters | Mood-disordered non-attempters | 234/223 | 2.0/2.1b |
| Goodwin | 2004 | Community sample (attempters) | Community sample (non-attempters) | 165/1209 | 4.6 |
Chart review.
Family history of attempters/completions.
Adapted from Brent and Mann. Family genetic studies, suicide, and suicidal behavior. Am J Psychiatry 2005;133C:13–24, with permission.
Table 8 lists 12 studies that have examined the rate of suicidal behavior in the families of suicide attempter probands, using a family history method. The findings are very consistent across studies, finding an increased rate of both completed and attempted suicide in the relatives of suicide attempters compared to the family members of controls. These findings are robust across a wide range of conditions: age of attempters (adolescents and adults), sampling frame (community samples, inpatients, outpatients), and diagnostic category (mixed, depression, bipolar, alcohol abuse, substance abuse). Greater lethality and violence of the attempt was associated with increased family loading in two studies (15;18). Loss of parent in childhood (under age of 11) either due to suicide (43) or due to any cause (22) was associated with an increased risk of attempt. Greater familial loading for suicidal behavior was associated with proband neuroticism, history of abuse or neglect, increased lifetime aggression, and, in those probands with mood disorder, an earlier age of onset of mood disorder (32–34;44;45). Moreover, a history of abuse, increased lifetime aggression, and earlier age of onset of mood disorder were interrelated (44). In one population study, significant relationships between parental and offspring ideation and attempt were reported (46). However, after adjustment for comorbidity, the strongest relationships were between parental and offspring attempt.
Family Studies of Suicide Attempting Probands (see Table 9)
Table 9.
Family Studies of Child or Adolescent Suicide-Attempting Probands*
| Study | Year | Proband | Control | N proband/control | OR |
|---|---|---|---|---|---|
| Pfeffer | 1994 | Prepubertal attempter | Ideator/clinica l control community controls | 25/28/16/54 | 4.3–8.3a |
| Johnson | 1998 | Adol. Inpt. attempters | Adol. Inpatient non-attempters | 62/70 | 2.1b |
| Bridge | 1997 | Community attempters | Community controls | 3/55 | 12.1b |
Attempter/normal control; OR = 8.3, attempter/clinical control.
Adjusted OR.
From Brent and Mann. Family genetic studies, suicide, and suicidal behavior. Am J Psychiatry 2005;133C:13–24, with permission.
Three family studies of child or adolescent suicide attempting probands have been conducted, finding an increased risk of suicide attempt in the relatives of suicide attempting probands (21;25;26). These studies also support a definition of the clinical phenotype that includes suicidal behavior, but does not include suicidal ideation, insofar as Pfeffer and colleagues found that a family history of attempts was increased only in the relatives of proband attempters but not in the relatives of proband ideators (21). A relationship between familial transmission of suicidal behavior and of impulsive aggression was also supported, since a higher rate of assaultive behavior was reported in the relatives of proband suicide attempters (21), and conversely, a higher rate of suicidal behavior in relatives was reported in the relatives of those proband attempters with higher levels of impulsive aggression (26).
High risk studies
A variant of the family study, the high risk study, has been used to prospectively examine the risks and processes associated with the familial transmission of suicidal behavior. In three studies that have taken this strategy, results are consistent—offspring of adult mood disordered suicide attempters have a much higher risk of suicide attempt than offspring of mood disordered probands who have never made a suicide attempt (see Figure 1). Greater familial loading for suicidal behavior is associated with a higher risk and earlier age of onset of suicidal behavior in offspring (see Figure 2), as well as higher levels of impulsive aggression in both parent and offspring (46–50). In one study, it was demonstrated that the familial transmission of suicidal behavior was in part mediated by the familial transmission of impulsive aggression (48). Furthermore, in prospective follow-up of high risk offspring, high levels of impulsive aggression, along with early-onset depression, predicted earlier onset and higher risk of suicidal behavior (49).
Figure 1. Risk of Suicide Attempt in the Offspring of Attempters Compared to Offspring of Non-Attempters.*.
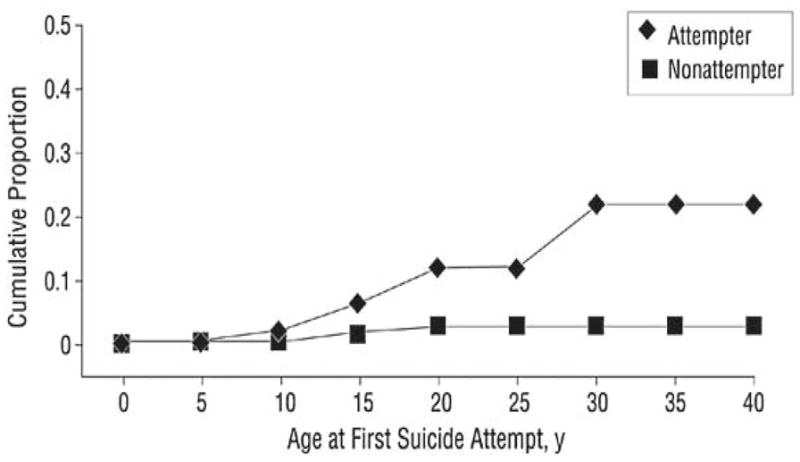
Diamond = Attempter
Square = Nonattempter
*From Brent et al. Familial pathways to early-onset suicide attempt: Risk for suicidal behavior in offspring of mood-disordered suicide attempters. Arch Gen Psychiatry 2002; 59:801–807, with permission.
Figure 2. Suicide Attempts Over Time Among Offspring of Mood Disorder Probands From Sibling Pairs Concordant or Discordant for Suicidal Behavior*.
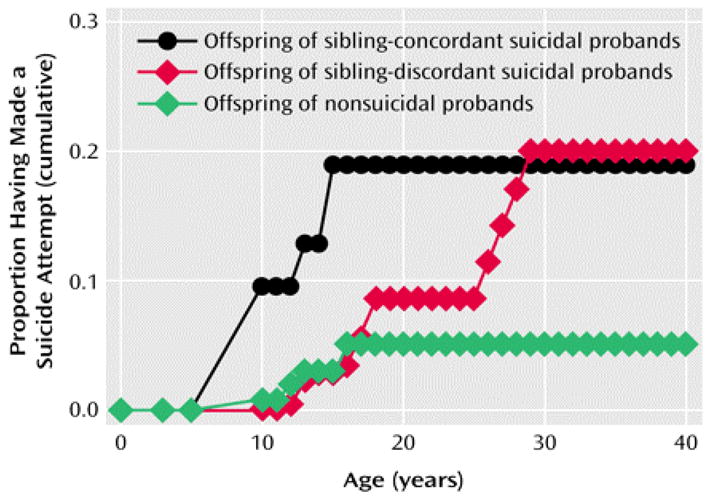
Black Circle = Offspring of sibling-concordant suicidal probands
Red Diamond = Offspring of sibling-discordant suicidal probands
Green Diamond = Offspring of nonsuicidal probands
*From Brent et al. Peripubertal suicide attempts in offspring of suicide attempters with siblings concordant for suicidal behavior. Am J Psychiatry 2003; 160:1486–1493, with permission.
High risk, family-genetic studies may also shed some light on some family-environmental factors that may contribute to the familial transmission of suicidal behavior. Most notably, the risk of suicide attempt in offspring of adult suicide attempters was greatly heightened if the parent themselves had a reported history of sexual abuse (47;49). Using a high-risk design (top-down), this relationship between parental sexual abuse and offspring attempt appears to be mediated through two pathways: (1) parental history of abuse that leads to an increased risk of offspring abuse, which in turn increases the risk for mood and anxiety disorder and suicide attempt; and (2) parental history of abuse that is associated with higher offspring impulsive aggression, which in turn increases the risk for early onset mood disorder and suicide attempt (51;52). Similar inter-relationships among parental history of abuse, offspring early-onset mood disorder and impulsive aggression, and suicide attempt were found in a “bottom-up” family history study (44). Taken together, these studies suggest that early abuse in childhood could account for some, but not all of the familial clustering of suicidal behavior because of the familial transmission of liability to abuse.
Possible mechanisms by which familial transmission of suicidal behavior may occur
Some possible intermediate phenotypes have emerged from family genetic studies. An intermediate phenotype according to Gottesman and Gould (53), must be related to the clinical phenotype, must be heritable, must predict the onset of the condition in offspring, and show evidence of mediation when controlling for the relationship between parent and offspring transmission of the overall clinical phenotype. The intermediate phenotype with the most convergent evidence is impulsive aggression, i.e., the propensity to react with aggression or hostility to frustration or provocation. This construct has been shown to be related to risk for suicide attempt (54), to predict onset of suicide attempt (49), to be heritable (55), and to mediate the transmission of suicidal behavior (48). Other possible intermediate phenotypes include neuroticism, which is heritable, and is related both to onset of attempt, and to family loading for suicidal behavior (56). Impaired working memory and executive function, which may form the neurocognitive substrate for impulsive aggression and for poor interpersonal problem-solving, has been shown to be altered in adult attempters, offspring of adult attempters, and to be heritable (57;58).
In addition to genetic transmission, familial transmission of suicidal behavior could be explained in a number of other ways, such as familial transmission of adverse family environment, imitation, or bereavement.
Intergenerational transmission of adverse family rearing environments
As noted above, the familial transmission of suicidal behavior is confounded by the familial transmission of abuse. The inter-relationship between the transmission of abuse and of suicidal behavior is complex, in part because parents who abuse their children are also at higher risk for psychiatric conditions that predispose to suicidal behavior, including depression, substance abuse, and suicidal behavior (59;60). Furthermore, impulsive aggression in a parent may predispose that parent to be abusive, but also may be transmitted to that child as a heritable trait. In fact, the relationship between parental abuse and offspring suicidal behavior is mediated in part by the transmission of impulsivity and aggression (51;52). Further complicating an understanding of this interrelationship between the child abuse and impulsive aggression are the longstanding neurobiological changes that have been reported in maltreated children that may account for increased impulsivity and aggression (61).
Imitation
The familial transmission of suicidal behavior could in theory be explained by imitation. This is plausible given evidence that youth suicide occurs in time-space clusters, and that exposure to print and electronic media publicity about suicidal behavior has been consistently been shown to be associated with an increase in suicidal behavior (62). However, in youth exposed to a sibling’s or a friend’s suicide, there is no evidence of imitation (63;64). In both high risk and twin studies that have examined the temporal relationship between attempts in relatives, no relationship consistent with imitation could be found (9;47). While imitation is difficult to disprove, these prospective case-control studies, taken with those of adoption studies, suggest that imitation is not a clinically significant contributor to the familial transmission of suicidal behavior.
Interestingly, exposure to a friend’s suicide attempt, but not to a friend’s completed suicide, appears to be associated with an increased risk for suicidal behavior (64;65). Knowing a person who has attempted suicide, whether a relative or not, has also been reported to be a risk factor for suicidal behavior in mid-life (66). It is possible, though, that exposure to suicidal behavior is the result of “assortative friendships,” insofar as friends of individuals with psychological difficulties are more likely to have mental disorder themselves. Peers with health risk behaviors, including suicidal behavior, are much more likely to have friends with increased rates of these behaviors (67). Moreover, the concordance among peers’ health risk behaviors is much higher in the face of family dysfunction (67). Conversely, the deleterious impact of an adverse rearing environment can be buffered by a pro-social peer group (68).
Parental bereavement
Retrospective, record linkage and prospective longitudinal studies have found that bereavement conveys an increased risk for depression and suicide.(69–73). There seems to be a more deleterious effect of parental bereavement when the child who has lost a parent is younger than the age of 12 (33;65;74). Record linkage studies indicate that parental loss by suicide is most strongly associated with suicide risk in offspring, but that so is maternal loss from any cause (41). The relationship between early parental loss and suicidal behavior may be mediated by an increased risk for depression (71;72). Other factors that may contribute further to suicidal risk are pre-morbid parental psychopathology (49), traumatic exposure predisposing to post-traumatic stress disorder (PTSD), and the development of complicated grief (prolonged negative affect and rumination about the loss), which in turn has been shown to predispose to suicidal ideation in young adults (75). However, empirical data does not support a specific relationship between parent loss due to suicide and suicidal behavior in the child, compared to parent loss due to other causes (76–79). Moreover, the association between child completed suicide and parental attempted suicide suggests that, while bereavement and loss may play a small role in the overall effect of familial transmission, the majority of the familial effect is due to some other mechanism.
Other family-environmental factors that may interact with genetic risk factors for suicidal behavior
Parental divorce and separation
There is a large literature documenting a higher risk for suicidal behavior and suicide in children from non-intact families. However, divorce per se is unlikely to lead to suicidal behavior (41;80;81). For example, marital disruption is more common in parents with psychiatric disorder. In studies that have examined the three-way relationships between divorce, parental and child psychiatric disorder, and child suicidal behavior, the relationship between divorce and child suicidal behavior is markedly attenuated after controlling for higher rates of parental psychiatric disorder (82–84). Young maternal age is another correlate of divorce that also predicts onset of suicidal behavior in adolescents (65). It is likely that the processes that ensue subsequent to the divorce that predict child adjustment. For example, Tousignant showed a dose response relationship between the number of parental figures (and subsequent disruptions) and the risk for adolescent suicidal behavior (85). A cascade of processes and predisposing factors mediate the relationship between divorce and eventual suicidal behavior (86). The relationship between parental divorce and child mental health disorders is mediated by the quality of the child’s relationship with the caretaking parent, the caretaking parent’s mental health, and the degree to which the child engages in active and problem-based coping.
Marital break-up and conjugal bereavement in adult life
Marital break-up is a frequent precipitant for suicide attempts and completed suicide, particularly in those with alcohol and substance abuse problems (87). There is evidence that the relationship rupture in alcoholics often follows domestic violence (88). In midlife and older individuals, particular males, conjugal bereavement is a risk factor for suicidal ideation and behavior, especially in concert with other psychiatric risk factors (89;90) Among women, having a child was protective against conjugal bereavement’s impact on suicide risk (91). Complicated grief has been shows to increase the risk for suicidal ideation above and beyond psychiatric disorder (75). Conversely, suicide, particularly in the geriatric age group is less likely to occur in those with a strong support network, e.g., confiding friendships, children nearby, or living with children (92;93).
Quality of family relationships
Family discord, including high expressed emotion have consistently been shown to be both correlates and predictors of adolescent suicidal behavior (94), although the relationship between discord and suicide attempt is somewhat attenuated after controlling for parental and child psychiatric disorder (84). Parent-child discord is the single most common precipitant for completed suicide in adolescents under the age of 16 (95). Other characteristics of parent-child relationships that have characterized suicidal adolescents have been lack of perceived support, and poor communication, particularly between children and fathers (24;85;96). In older individuals, marital conflict is often associated with depression and substance abuse, although it is difficult to disentangle the extent to which the psychiatric illness is a source of the discord, or a consequence. Nevertheless, marital therapy aimed at reducing discord and increasing support has been shown to relieve depression when discord is a prominent part of the presentation (97–100). Moral objections to suicide have also been shown to protect against suicidal behavior, and such attitudes can also be familially transmitted (101;102).
Family protective factors
High parent-child warmth, parental monitoring, consistent parental discipline, and family cohesion have been shown to be protective against youthful suicidal behavior (103). High levels of protective factors lower the risk for suicide attempt in adolescents even in the presence of other high risk behaviors and predisposing factors (67;103)
Adult suicide attempters, in general, report lower perceived family support, and concern about the impact on family is one of the most common reasons given by depressed individuals for not engaging in suicidal behavior (104;105). A much lower proportion of adults who commit suicide are in a stable relationship compared to living controls (76), suggesting that the continuation of a strong pair-bond is protective. As noted above, other factors protective against suicide in older individuals are a strong network of support, including living with children (if the individual is female) or having them nearby.
Childhood experience of abuse
Physical and sexual abuse, particularly sexual abuse that involves genital or anal penetration, are strongly associated with suicide attempts and completions. According to some epidemiological studies, sexual abuse has a population attributable risk of nearly 20%, meaning that the rate of suicidal behavior in adolescents could be decreased by 20% if sexual abuse could be eliminated (106–108). The mechanism by which abuse increases risk for suicidal behavior is complex, as child maltreatment usually takes place against a background of family discord, parental psychopathology, including a parental history of suicidal behavior, all of which can also increase the risk for suicidal behavior in children (59;60). However, while it is clear that abuse increases the risk for a wide array of psychiatric disorders, some studies show that even after controlling for the increased risk of psychiatric disorder, abuse increases the risk and decreases the age of onset for suicidal behavior (109;110).
Sexual abuse in parent and child appear to increase the risk for transmission of suicidal behavior through several possible mechanisms. As noted above, sexual abuse in a parent increases the likelihood of sexual abuse in the child, which in turn increases the likelihood for a mood or anxiety disorder, and for suicide attempt (33;48;51;111). Second, parents who abuse their children are more likely to also attempt suicide as well as have mood and substance disorders, so that the liability for suicide attempt in the child may come from both genetic and environmental manifestations of a common diathesis (59;60). Third, sexual abuse may increase the likelihood of expression of traits related to suicidal risk, like neuroticism, anxiety, depression, and impulsive aggression (32;47;51;110;112–114). Also, abuse and other adverse circumstances could be familially transmitted by shared environmental rather than by genetic mechanisms. Fu et al. found that shared environment explained as much of the variance in suicide attempts as did heritability (10). Dinwiddie et al., in an analysis of the Australian twin registry reported in Statham et al. (9), found that the negative impact of sexual abuse on mental health outcomes was explained by shared environment, rather than genetic factors (115).
There is growing evidence of long-lasting neurobiological changes as a result of neglectful or abusive rearing environments. In mice, pups who are exposed to low levels of maternal grooming show changes in cortisol response to stress, cognitive impairment, and lower persistence in the face of frustrating tasks than those exposed to high levels of grooming (116–118). Moreover, the specific maternal behavior (grooming) appears to be familially transmitted from mother to daughter. However, this transmission is not due to genetic factors because cross-fostering experiments show that it is exposure to grooming rather than the grooming style of the biological mother that determines grooming behavior in the offspring (116). Neuroendocrine studies of children with a history of maltreatment show alternations in the hypothalamic pituitary adrenal axis (HPA), although some studies have reported lower than expected response to stress, and some, higher than expected response (119). Neuroimaging studies in children exposed to maltreatment also show changes in corpus collusum and hippocampus volume that may account for some of the cognitive findings associated with a history of maltreatment (61). Abuse and adverse rearing environments result in a decrease in central serotonergic function, a biological system that has been linked to impulsive aggression and suicidal behavior (120–124).
Interactions between genes and environment
In the debate between about the relative contributions of nature and nurture, there is a “nature to nurture,” (125) meaning that adverse family environments do not occur at random, and may arise due to parental or child genetic contributors to these adverse environments. Parental psychiatric illness is a risk factor for premature parental death, which in turn puts their offspring at higher risk for psychiatric disorder (49). Parents who abuse their children are more likely to have psychiatric disorders such as depression, substance abuse, and a history of suicidal behavior, so that their children are at risk because of their genetic diathesis as well as because of the exposure to abuse (60;126). Children who are risk for depression may follow a stochastic pathway: (1) genes that predispose to anxiety also predispose to the occurrence of certain depressogenic life events, that, in the face of a genetic diathesis to anxiety, lead to depression (127). Finally, studies of twins reared apart show that dimensions of maternal behavior such as parental warmth are actually heritable, being induced by the behavior of the twin offspring (12).
Second, it is important to recognize that environmental factors are most likely to affect those with a genetic diathesis. This was most elegantly demonstrated by Caspi and colleagues, who showed that the likelihood of depression and suicidal behavior was greatest when there was a history of stressful life events (including abuse) and a less function allelic form of the serotonin transporter promoter gene (112). This finding has been replicated several times (71;128–130). Kaufman et al. found that the risk for depression was greatest in abused children who also had a family history of depression (124).
Third, these different family-environmental stressors rarely occur in isolation. For example, it is more common for a child with a background of maltreatment to have been also exposed to multiple parental figures, parental criminality and psychiatric disorder, witnessing domestic violence, and economic instability (96;131;132). Nevertheless, there is evidence that there are factors that are protective against suicidal behavior even in the face of substantial other risk factors (103).
Summary
It is well-recognized that suicidal behavior runs in families. Adoption and twin studies together make a compelling case that familial transmission of suicidal behavior is in part attributable to genetic factors. There is some evidence that the transmission of suicidal behavior is mediated by the transmission of impulsive aggression. Other, less thoroughly investigated possible mediators include neuroticism and neurocognitive deficits. However, given that at best, around 50% of the variance is explained by genes, there is a significant role for environmental factors as well. The most plausible explanations for non-genetic familial transmission are the intergenerational transmission of abuse and of adverse familial environments. Bereavement and relationship disruption may make a specific contribution to suicidal risk via the development of complicated grief although the long-term effects are likely to be mediated by complex chain of inter-related events. Imitation may also make a contribution to suicidal risk, at least with regard to attempted suicide. However, so-called family environmental factors often are related to risk factors that are heritable. Conversely, and most genetic factors exert their impact on depression and suicidal behavior via an interaction with a stressful environment.
Acknowledgments
This work was supported by NIMH grants MH 43366, 55123, 6612, 56390, 66371and 62185. The expert assistance of Beverly Sughrue in preparation of the manuscript is appreciated.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference List
- 1.Brent DA, Mann JJ. Family genetic studies of suicide and suicidal behavior. Am J Med Genetics. 2005;133C:13–24. doi: 10.1002/ajmg.c.30042. [DOI] [PubMed] [Google Scholar]
- 2.Kety SS, Rosenthal D, Wender PH, Schulsinger F. The types and prevalence of mental illness in the biological and adoptive families of adopted schizophrenia. J Psychiat Res. 1968;6:345–362. [Google Scholar]
- 3.Schulsinger F, Kety SS, Rosenthal D, Wender PH. A family study of suicide. In: Schou M, Stromgren E, editors. Origin, Prevention and Treatment of Affective Disorders. London: Academic Press; 1979. pp. 277–287. [Google Scholar]
- 4.Wender PH, Kety SS, Rosenthal D, Schulsinger F, Ortmann J, Lunde I. Psychiatric disorders in the biological and adoptive families of adopted individuals with affective disorders. Archives of General Psychiatry. 1986;43:923–929. doi: 10.1001/archpsyc.1986.01800100013003. [DOI] [PubMed] [Google Scholar]
- 5.Tsuang MT. Genetic factors in suicide. Dis Nerv Syst. 1977;38:498–501. [PubMed] [Google Scholar]
- 6.Roy A, Segal NL. Suicidal behavior in twins: A replication. J Affect Disord. 2001;66:71–74. doi: 10.1016/s0165-0327(00)00275-5. [DOI] [PubMed] [Google Scholar]
- 7.Roy A, Segal NL, Sarchiapone M. Attempted suicide among living co-twins of twin suicide victims. Am J Psychiatry. 1995;152:1075–1076. doi: 10.1176/ajp.152.7.1075. [DOI] [PubMed] [Google Scholar]
- 8.Segal NL, Roy A. Suicidal attempts and ideation in twins whose co-twins’ deaths were non-suicides: Replication and elaboration. Pers Individ Differences. 2001;31:445–452. [Google Scholar]
- 9.Statham DJ, Heath AC, Madden PAF, Bucholz KK, Bierut L, Dinwiddie SH, Slutske WS, Dunne MP, Martin NG. Suicidal behaviour: An epidemiological and genetic study. Psychol Med. 1998;28:839–855. doi: 10.1017/s0033291798006916. [DOI] [PubMed] [Google Scholar]
- 10.Fu Q, Heath AC, Bucholz KK, Nelson EC, Glowinski AL, Goldberg J, Lyons MJ, Tsuang MT, Jacob T, True MR, Eisen SA. A twin study of genetic and environmental influences on suicidality in men. Psychol Med. 2002;32:11–24. doi: 10.1017/s0033291701004846. [DOI] [PubMed] [Google Scholar]
- 11.Glowinski A, Bucholz KK, Nelson EC, Fu Q, Madden P, Reich W, Heath AC. Suicide attempts in an adolescent female twin sample. J Am Acad Child Adolesc Psychiatry. 2001;40:1300–1307. doi: 10.1097/00004583-200111000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Plomin R, Reiss D, Hetherington EM, Howe GW. Nature and nurture: Genetic contributions to measures of the family environment. Dev Psychol. 1994;30(1):32–43. [Google Scholar]
- 13.Devlin B, Daniels M, Roeder K. The heritability of IQ. Nature. 1997;388:468–471. doi: 10.1038/41319. [DOI] [PubMed] [Google Scholar]
- 14.Egeland JA, Sussex JN. Suicide and family loading for affective disorders. J Am Med Assoc. 1985;254:915–918. [PubMed] [Google Scholar]
- 15.Garfinkel BD, Froese A, Hood J. Suicide attempts in children and adolescents. Am J Psychiatry. 1982;139:1257–1261. doi: 10.1176/ajp.139.10.1257. [DOI] [PubMed] [Google Scholar]
- 16.Roy A. Family history of suicide. Archives of General Psychiatry. 1983;40:971–974. doi: 10.1001/archpsyc.1983.01790080053007. [DOI] [PubMed] [Google Scholar]
- 17.Tsuang MT. Risk of suicide in the relatives of schizophrenics, manics, depressives, and controls. J Clin Psychiatry. 1983;44:396–400. [PubMed] [Google Scholar]
- 18.Linkowski P, de Maertelaer V, Mendlewicz J. Suicidal behaviour in major depressive illness. Acta Psychiatrica Scandinavica. 1985;72:233–238. doi: 10.1111/j.1600-0447.1985.tb02600.x. [DOI] [PubMed] [Google Scholar]
- 19.Mitterauer B. A contribution to the discussion of the role of the genetic factor in suicide, based on five studies in an epidemiologically defined area (Province of Salzburg, Austria) Compr Psychiatry. 1990;31:557–565. doi: 10.1016/0010-440x(90)90070-9. [DOI] [PubMed] [Google Scholar]
- 20.Sorenson SB, Rutter CM. Transgenerational patterns of suicide attempt. J Consult Clin Psychol. 1991;59:861–866. doi: 10.1037//0022-006x.59.6.861. [DOI] [PubMed] [Google Scholar]
- 21.Pfeffer CR, Normandin L, Tatsuyuki K. Suicidal children grow up: Suicidal behavior and psychiatric disorders among relatives. J Am Acad Child Psychiatry. 1994;33:1087–1097. doi: 10.1097/00004583-199410000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Malone KM, Haas GL, Sweeney JA, Mann JJ. Major depression and the risk of attempted suicide. J Affect Disord. 1995;34:173–185. doi: 10.1016/0165-0327(95)00015-f. [DOI] [PubMed] [Google Scholar]
- 23.Brent DA, Bridge J, Johnson BA, Connolly J. Suicidal behavior runs in families: A controlled family study of adolescent suicide victims. Archives of General Psychiatry. 1996;53:1145–1152. doi: 10.1001/archpsyc.1996.01830120085015. [DOI] [PubMed] [Google Scholar]
- 24.Gould MS, Fisher P, Parides M, Flory M, Shaffer D. Psychosocial risk factors of child and adolescent completed suicide. Archives of General Psychiatry. 1996;53:1155–1162. doi: 10.1001/archpsyc.1996.01830120095016. [DOI] [PubMed] [Google Scholar]
- 25.Bridge JA, Brent DA, Johnson B, Connolly J. Familial aggregation of psychiatric disorders in a community sample of adolescents. J Am Acad Child Adolesc Psychiatry. 1997;36:628–636. doi: 10.1097/00004583-199705000-00013. [DOI] [PubMed] [Google Scholar]
- 26.Johnson BA, Brent DA, Bridge J, Connolly J, Matta J, Constantine D, Rather C, White T. The familial aggregation of adolescent suicide attempts. Acta Psychiatrica Scandinavica. 1998;97:18–24. doi: 10.1111/j.1600-0447.1998.tb09957.x. [DOI] [PubMed] [Google Scholar]
- 27.Foster T, Gillespie K, McClelland R, Patterson C. Risk factors for suicide independent of DSM-III-R Axis I disorder: Case control psychological autopsy study in Northern Ireland. Br J Psychiatry. 1999;175:175–179. doi: 10.1192/bjp.175.2.175. [DOI] [PubMed] [Google Scholar]
- 28.Cheng AT, Chen THH, Chen CC, Jenkins R. Psychosocial and psychiatric risk factors for suicide: Case-control psychological autopsy study. Br J Psychiatry. 2000;177:360–365. doi: 10.1192/bjp.177.4.360. [DOI] [PubMed] [Google Scholar]
- 29.Powell J, Geddes J, Deeks J, Goldacre M, Hawton K. Suicide in psychiatric hospital in-patients: Risk factors and their predictive powers. Br J Psychiatry. 2000;176:266–272. doi: 10.1192/bjp.176.3.266. [DOI] [PubMed] [Google Scholar]
- 30.Roy A. Relation of family history of suicide to suicide attempts in alcoholics. Am J Psychiatry. 2000;157:2050–2051. doi: 10.1176/appi.ajp.157.12.2050. [DOI] [PubMed] [Google Scholar]
- 31.Roy A. Characteristics of cocaine-dependent patients who attempt suicide. Am J Psychiatry. 2001;158:1215–1219. doi: 10.1176/appi.ajp.158.8.1215. [DOI] [PubMed] [Google Scholar]
- 32.Roy A. Family history of suicide and neuroticism: A preliminary study. Psychiatry Res. 2002;110:87–90. doi: 10.1016/s0165-1781(02)00011-2. [DOI] [PubMed] [Google Scholar]
- 33.Roy A. Childhood trauma and neuroticism as an adult: Possible implication for the development of the common psychiatric disorders and suicidal behaviour. Psychol Med. 2002;32:1471–1474. doi: 10.1017/s0033291702006566. [DOI] [PubMed] [Google Scholar]
- 34.Roy A. Characteristics of opiate dependent patients who attempt suicide. J Clin Psychiatry. 2002;63:403–407. doi: 10.4088/jcp.v63n0505. [DOI] [PubMed] [Google Scholar]
- 35.Qin P, Agerbo E, Mortensen PB. Suicide risk in relation to family history of completed suicide and psychiatric disorders: A nested case-control study based on longitudinal registers. The Lancet. 2002;360:1126–1130. doi: 10.1016/S0140-6736(02)11197-4. [DOI] [PubMed] [Google Scholar]
- 36.Tsai SY, Kuo C, Chen CC, Lee H. Risk factors for completed suicide in bipolar disorder. J Clin Psychiatry. 2002;63:469–476. doi: 10.4088/jcp.v63n0602. [DOI] [PubMed] [Google Scholar]
- 37.Qin P, Agerbo E, Mortensen PB. Suicide risk in relation to socioeconomic, demographic, psychiatric, and familial factors: A national register-based study of all suicides in Denmark, 1981–1997. Am J Psychiatry. 2003;160:765–772. doi: 10.1176/appi.ajp.160.4.765. [DOI] [PubMed] [Google Scholar]
- 38.Runeson B, Asberg M. Family history of suicide among suicide victims. Am J Psychiatry. 2003;160:1525–1526. doi: 10.1176/appi.ajp.160.8.1525. [DOI] [PubMed] [Google Scholar]
- 39.Roy A. Characteristics of drug addicts who attempt suicide. Psychiatry Res. 2003;121:99–103. doi: 10.1016/s0165-1781(03)00206-3. [DOI] [PubMed] [Google Scholar]
- 40.Kim CD, Seguin M, Therrien N, Riopel G, Chawky N, Lesage AD, Turecki G. Familial aggregation of suicidal behavior: A family study of male suicide completers from the general population. Am J Psychiatry. 2005;162:1017–1019. doi: 10.1176/appi.ajp.162.5.1017. [DOI] [PubMed] [Google Scholar]
- 41.Agerbo E, Nordentoft M, Mortensen PB. Familial, psychiatric, and socioeconomic risk factors for suicide in young people: Nested case-controlled study. Br Med J. 2002;325 doi: 10.1136/bmj.325.7355.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tsuang MT, Simpson JC. Mortality studies in psychiatry: Should they stop or proceed? Archives of General Psychiatry. 1985;42:98–103. doi: 10.1001/archpsyc.1985.01790240100012. [DOI] [PubMed] [Google Scholar]
- 43.Roy A. Early parental death and adult depression. Psychol Med. 1983;13:861–865. doi: 10.1017/s0033291700051588. [DOI] [PubMed] [Google Scholar]
- 44.Mann JJ, Bortinger J, Oquendo MA, Currier D, Li S, Brent DA. Family history of suicidal behavior and mood disorders in probands with mood disorders. Am J Psychiatry. 2005;162:1672–1679. doi: 10.1176/appi.ajp.162.9.1672. [DOI] [PubMed] [Google Scholar]
- 45.Hawton K, Haw C, Houston K, Townsend E. Family history of suicidal behaviour: Prevalence and significance in deliberate self-harm patients. Acta Psychiatrica Scandinavica. 2002;106:387–393. doi: 10.1034/j.1600-0447.2002.02003.x. [DOI] [PubMed] [Google Scholar]
- 46.Goodwin RD, Beautrais AL, Fergusson DM. Familial transmission of suicidal ideation and suicide attempts: evidence from a general population sample. Psychiatry Res. 2004;126:159–165. doi: 10.1016/j.psychres.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 47.Brent DA, Oquendo M, Birmaher B, Greenhill L, Kolko D, Stanley B, Zelazny J, Brodsky B, Bridge J, Ellis S, Salazar O, Mann JJ. Familial pathways to early-onset suicide attempt: Risk for suicidal behavior in offspring of mood-disordered suicide attempters. Archives of General Psychiatry. 2002;59:801–807. doi: 10.1001/archpsyc.59.9.801. [DOI] [PubMed] [Google Scholar]
- 48.Brent DA, Oquendo MA, Birmaher B, Greenhill L, Kolko D, Stanley B, Zelazny J, Brodsky B, Firinciogullari S, Ellis SP, Mann JJ. Peripubertal suicide attempts in offspring of suicide attempters with siblings concordant for suicidal behavior. Am J Psychiatry. 2003;160:1486–1493. doi: 10.1176/appi.ajp.160.8.1486. [DOI] [PubMed] [Google Scholar]
- 49.Melhem NM, Brent DA, Ziegler M, Iyengar S, Kolko DJ, Oquendo M, Birmaher B, Burke A, Zelazny J, Stanley B, Mann JJ. Familial pathways to early-onset suicidal behavior: Familial and individual antecedents of suicidal behavior. Am J Psychiatry. 2007;164:1364–1370. doi: 10.1176/appi.ajp.2007.06091522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lieb R, Bronisch T, Hofler M, Schreier A, Wittchen H-U. Maternal suicidality and risk of suicidality in offspring: Findings from a community study. Am J Psychiatry. 2005;162:1665–1671. doi: 10.1176/appi.ajp.162.9.1665. [DOI] [PubMed] [Google Scholar]
- 51.Brodsky BS, Mann JJ, Stanley B, Tin A, Oquendo M, Birmaher B, Greenhill L, Kolko D, Zelazny J, Burke A, Melhem N, Brent D. Familial transmission of suicidal behavior: Factors mediating the relationship between abuse and offspring suicide attempts. Journal of Clinical Psychiatry. doi: 10.4088/jcp.v69n0410. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Brent DA, Oquendo MA, Birmaher B, Greenhill L, Kolko D, Stanley B, Zelazny J, Brodsky B, Melhem NM, Ellis SP, Mann JJ. Familial transmission of mood disorders: Convergence and divergence with transmission of suicidal behavior. J Am Acad Child Adolesc Psychiatry. 2004;43:1259–1266. doi: 10.1097/01.chi.0000135619.38392.78. [DOI] [PubMed] [Google Scholar]
- 53.Gottesman II, Gould TD. The endophenotype concept in psychiatry: Etymology and strategic intentions. Am J Psychiatry. 2003;160:636–645. doi: 10.1176/appi.ajp.160.4.636. [DOI] [PubMed] [Google Scholar]
- 54.Mann JJ, Waternaux C, Haas GL, Malone KM. Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry. 1999;156:181–189. doi: 10.1176/ajp.156.2.181. [DOI] [PubMed] [Google Scholar]
- 55.Coccaro E, Bergeman CS, Kavoussi RJ, Seroczynski AD. Heritability of aggression and irritability: A twin study of the Buss-Durkee aggression scales in adult male subjects. Biol Psychiatry. 1997;41:273–284. doi: 10.1016/s0006-3223(96)00257-0. [DOI] [PubMed] [Google Scholar]
- 56.Beautrais A, Joyce PR, Mulder RT. Personality traits and cognitive styles as risk factors for serious suicide attempts among young people. Suicide Life Threat Behav. 1999;29:37–47. [PubMed] [Google Scholar]
- 57.Beers SR, Keilp JG, Melhem NM, Wiles C, Ozawa H, Birmaher B, Mann JJ, Brent DA. Familial transmission of suicidal behavior: Neuropsychological dysfunction in offspring of suicide attempters. Psychological Medicine. Submitted. [Google Scholar]
- 58.Jeglic EL, Sharp IR, Chapman JE, Brown GK, Beck AT. History of family suicide behaviors and negative problem solving in multiple suicide attempters. Archives of Suicide Research. 2005;9:135–146. doi: 10.1080/13811110590903981. [DOI] [PubMed] [Google Scholar]
- 59.Roberts J, Hawton K. Child abuse and attempted suicide. Br J Psychiatry. 1980;137:319–323. doi: 10.1192/bjp.137.4.319. [DOI] [PubMed] [Google Scholar]
- 60.Chaffin M, Kelleher KJ, Hollenberg J. Onset of physical abuse and neglect: Psychiatric, substance abuse and social risk factors from prospective community data. Child Abuse and Neglect. 1996;20:191–203. doi: 10.1016/s0145-2134(95)00144-1. [DOI] [PubMed] [Google Scholar]
- 61.DeBellis MD, Thomas LA. Biologic findings of post-traumatic stress disorder and child maltreatment. Current Psychiatry Reports. 2003;5:108–117. doi: 10.1007/s11920-003-0027-z. [DOI] [PubMed] [Google Scholar]
- 62.Gould MS. Suicide and the media. Ann N y Acad Sci. 2001;932:200–224. doi: 10.1111/j.1749-6632.2001.tb05807.x. [DOI] [PubMed] [Google Scholar]
- 63.Brent DA, Moritz G, Bridge J, Perper J, Canobbio R. The impact of adolescent suicide on siblings and parents: A longitudinal follow-up. Suicide Life Threat Behav. 1996;26:253–259. [PubMed] [Google Scholar]
- 64.Brent DA, Moritz G, Bridge J, Perper J, Canobbio R. Long-term impact of exposure to suicide: A three-year controlled follow-up. J Am Acad Child Adolesc Psychiatry. 1996;35(5):646–653. doi: 10.1097/00004583-199605000-00020. [DOI] [PubMed] [Google Scholar]
- 65.Lewinsohn PM, Rohde P, Seeley JR. Adolescent suicidal ideation and attempts: Prevalence, risk factors, and clinical implications. Clin Psychol Sci Prac. 1996;3:25–46. [Google Scholar]
- 66.Conner KR, Duberstein PR. Predisposing and precipitating factors for suicide among alcoholics: empirical review and conceptual integration. Alcoholism: Clinical & Experimental Research. 2004;28:65–17S. doi: 10.1097/01.alc.0000127410.84505.2a. [DOI] [PubMed] [Google Scholar]
- 67.Prinstein MJ, Boergers J, Spirito A. Adolescents’ and their friends’ health-risk behavior: Factors that alter or add to peer influence. J Pediatr Psychol. 2001;26:287–298. doi: 10.1093/jpepsy/26.5.287. [DOI] [PubMed] [Google Scholar]
- 68.Lynskey MT, Fergusson DM. Factors protecting against the development of adjustment difficulties in young adults exposed to childhood sexual abuse. Child Abuse and Neglect. 1997;21:1177–1190. doi: 10.1016/s0145-2134(97)00093-8. [DOI] [PubMed] [Google Scholar]
- 69.Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ. Childhood parental loss and adult psychopathology in women: A twin study perspective. Archives of General Psychiatry. 1992;49:109–116. doi: 10.1001/archpsyc.1992.01820020029004. [DOI] [PubMed] [Google Scholar]
- 70.Kendler KS, Gardner CO, Prescott CA. Toward a comprehensive development model for major depression in men. Am J Psychiatry. 2006;163:115–124. doi: 10.1176/appi.ajp.163.1.115. [DOI] [PubMed] [Google Scholar]
- 71.Kendler KS, Sheth K, Gardner CO, Prescott CA. Childhood parental loss and risk for first-onset of major depression and alcohol dependence: The time-decay of risk and sex differences. Psychol Med. 2002;32:1187–1194. doi: 10.1017/s0033291702006219. [DOI] [PubMed] [Google Scholar]
- 72.Reinherz HZ, Giaconia RM, Carmola Hauf AM, Wasserman MS, Silverman AB. Major depression in the transition to adulthood: Risks and impairments. J Abnorm Psychol. 1999;108:500–510. doi: 10.1037//0021-843x.108.3.500. [DOI] [PubMed] [Google Scholar]
- 73.Tremblay GC, Israel AC. Children’s adjustment to parental death. Clin Psychol Sci Prac. 1998;5:424–438. [Google Scholar]
- 74.Roy A. Childhood trauma and attempted suicide in alcoholics. The Journal of Nervous and Mental Disease. 2001;189:120–121. doi: 10.1097/00005053-200102000-00008. [DOI] [PubMed] [Google Scholar]
- 75.Latham AE, Prigerson HG. Suicidality and bereavement: Complicated grief as a psychiatric disorder presenting greatest risk for suicidality. Suicide Life Threat Behav. 2004;34:350–362. doi: 10.1521/suli.34.4.350.53737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Melhem N, Walker M, Moritz G, Brent DA. Antecedents and sequelae of sudden parental death in children and surviving caregivers. Archives of Pediatric and Adolescent Medicine. doi: 10.1001/archpedi.162.5.403. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Jordan JR. Is suicide bereavement different? A reassessment of the literature. Suicide Life Threat Behav. 2001;31:91–102. doi: 10.1521/suli.31.1.91.21310. [DOI] [PubMed] [Google Scholar]
- 78.Cerel J, Fristad M, Verducci J, Weller RA, Weller EB. Childhood bereavement: Psychopathology in the 2 years postparental death. J Am Acad Child Adolesc Psychiatry. 2006;45:681–690. doi: 10.1097/01.chi.0000215327.58799.05. [DOI] [PubMed] [Google Scholar]
- 79.Cerel J, Fristad MA, Weller EB, Weller RA. Suicide-bereaved children and adolescents: A controlled longitudinal examination. J Am Acad Child Adolesc Psychiatry. 1999;38:672–679. doi: 10.1097/00004583-199906000-00013. [DOI] [PubMed] [Google Scholar]
- 80.Goldney RD. Parental loss and reported childhood stress in young women who attempt suicide. Acta Psychiatrica Scandinavica. 1981;64:34–59. doi: 10.1111/j.1600-0447.1981.tb00759.x. [DOI] [PubMed] [Google Scholar]
- 81.Adam KS, Bouckoms A, Streiner DL. Parental loss and family stability in attempted suicide. Archives of General Psychiatry. 1982;39:1081–1085. doi: 10.1001/archpsyc.1982.04290090065013. [DOI] [PubMed] [Google Scholar]
- 82.Gould MS, Shaffer D, Fisher P, Garfinkel R. Separation/divorce and child and adolescent completed suicide. J Am Acad Child Adolesc Psychiatry. 1998;37:155–162. doi: 10.1097/00004583-199802000-00007. [DOI] [PubMed] [Google Scholar]
- 83.Gould MS, Greenberg T, Velting DM, Shaffer D. Youth suicide risk and preventative interventions: A review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 2003;42:386–405. doi: 10.1097/01.CHI.0000046821.95464.CF. [DOI] [PubMed] [Google Scholar]
- 84.Brent DA, Perper JA, Moritz G, Liotus L, Schweers J, Balach L, Roth C. Familial risk factors for adolescent suicide: A case-control study. Acta Psychiatrica Scandinavica. 1994;89:52–58. doi: 10.1111/j.1600-0447.1994.tb01485.x. [DOI] [PubMed] [Google Scholar]
- 85.Tousignant M, Bastien MF, Hamel S. Suicidal attempts and ideations among adolescents and young adults: The contribution of the father’s and mother’s care and of parental separation. Soc Psychiatry Psychiatr Epidemiol. 1993;28:256–261. doi: 10.1007/BF00788746. [DOI] [PubMed] [Google Scholar]
- 86.Sandler IN, Tein JY, Mehta P, Wolchik S, Ayers T. Coping efficacy and psychological problems of children of divorce. Child Development. 2000;71:1099–1118. doi: 10.1111/1467-8624.00212. [DOI] [PubMed] [Google Scholar]
- 87.Murphy GE, Wetzel RD, Robins E, McEvoy L. Multiple risk factors predict suicide in alcoholism. Archives of General Psychiatry. 1992;49:459–463. doi: 10.1001/archpsyc.1992.01820060039006. [DOI] [PubMed] [Google Scholar]
- 88.Conner KR, Duberstein P, Conwell Y. Domestic violence, separation, and suicide in young men with early onset alcoholism: Reanalyses of Murphy’s data. Suicide and Life Threatening Behavior. 2000;30:354–359. [PubMed] [Google Scholar]
- 89.Kposowa AJ. Marital status and suicide in the National Longitudinal Mortality Study. J Epidemiol Community Health. 2000;54:254–261. doi: 10.1136/jech.54.4.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Li G. The interaction effect of bereavement and sex on the risk of suicide in the elderly: An historical cohort study. Soc Sci Med. 1995;40:825–828. doi: 10.1016/0277-9536(94)00135-g. [DOI] [PubMed] [Google Scholar]
- 91.Agerbo E. Midlife suicide risk, partner’s psychiatric illness, spouse and child bereavement by suicide or other modes of death: A gender specific study. J Epidemiol Community Health. 2005;59:407–412. doi: 10.1136/jech.2004.024950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Rowe JL, Conwell Y, Schulberg H, Bruce ML. Social support and suicidal ideation in order adults using home healthcare services. American Journal of Geriatric Psychiatry. 2006;14:758–766. doi: 10.1097/01.JGP.0000218324.78202.25. [DOI] [PubMed] [Google Scholar]
- 93.Rowe JL, Bruce ML, Conwell Y. Correlates of suicide among home health care utilizers who died by suicide and community controls. Suicide and Life Threatening Behavior. 2006;36:65–75. doi: 10.1521/suli.2006.36.1.65. [DOI] [PubMed] [Google Scholar]
- 94.Wagner BM. Family risk factors for child and adolescent suicidal behavior. Psychol Bull. 1997;121:246–298. doi: 10.1037/0033-2909.121.2.246. [DOI] [PubMed] [Google Scholar]
- 95.Brent DA, Baugher M, Bridge J, Chen J, Beery L. Age and sex-related risk factors for adolescent suicide. J Am Acad Child Adolesc Psychiatry. 1999;38:1497–1505. doi: 10.1097/00004583-199912000-00010. [DOI] [PubMed] [Google Scholar]
- 96.Fergusson DM, Lynskey MT. Childhood circumstances, adolescent adjustment, and suicide attempts in a New Zealand birth cohort. J Am Acad Child Adolesc Psychiatry. 1995;34:612–622. doi: 10.1097/00004583-199505000-00013. [DOI] [PubMed] [Google Scholar]
- 97.Jacobson NS, Dobson KS, Truax PA, Addis ME, Koerner K, Gollan JK, Gortner E, Prince SE. A component analysis of cognitive-behavioral treatment for depression. J Consult Clin Psychol. 1996;64(2):295–304. doi: 10.1037//0022-006x.64.2.295. [DOI] [PubMed] [Google Scholar]
- 98.Jacobson NS, Schamaling KB, Holtzworth-Munroe A. Component analysis of behavioral marital therapy: 2-year follow-up and prediction of relapse. J Mar Fam Ther. 1987;13:187–195. doi: 10.1016/0005-7967(85)90102-0. [DOI] [PubMed] [Google Scholar]
- 99.Jacobson NS, Holtzworth-Munroe A, Schmaling KB. Marital therapy and spouse involvement in the treatment of depression, agoraphobia and alcoholism. J Consult Clin Psychol. 1989;57:5–10. doi: 10.1037//0022-006x.57.1.5. [DOI] [PubMed] [Google Scholar]
- 100.Jacobson NS, Dobson K, Frizzetti AE, Schmaling KB, Salusky S. Marital therapy as a treatment for depression. J Consult Clin Psychol. 1991;59:547–557. doi: 10.1037//0022-006x.59.4.547. [DOI] [PubMed] [Google Scholar]
- 101.Dervic K, Oquendo MA, Currier D, Grunebaum MF, Burke AK, Mann JJ. Moral objections to suicide: Can they counteract suidiality in patients with cluster B psychopathology? J Clin Psychiatry. 2006;67:620–625. [PubMed] [Google Scholar]
- 102.Gur M, Miller L, Warner V, Wickramaratne P, Weissman M. Maternal depression and the intergenerational transmission of religion. J Nerv Ment Dis. 2005;193:338–345. doi: 10.1097/01.nmd.0000161701.05878.8a. [DOI] [PubMed] [Google Scholar]
- 103.Borowsky IW, Ireland M, Resnick MD. Adolescent suicide attempts: Risks and protectors. Pediatrics. 2001;107:485–493. doi: 10.1542/peds.107.3.485. [DOI] [PubMed] [Google Scholar]
- 104.Oquendo MA, Dragatsi D, Harkavy-Friedman J, Dervic K, Currier D, Burke AK, Grunebaum MF, Mann JJ. Protective factors against suicidal behavior in Latinos. J Nerv Ment Dis. 2005;193:438–443. doi: 10.1097/01.nmd.0000168262.06163.31. [DOI] [PubMed] [Google Scholar]
- 105.Malone KM, Oquendo MA, Haas GL, Ellis SP, Li S, Mann JJ. Protective factors against suicidal acts in major depression: Reasons for living. Am J Psychiatry. 2000;157:1084–1088. doi: 10.1176/appi.ajp.157.7.1084. [DOI] [PubMed] [Google Scholar]
- 106.Fergusson DM, Horwood L, Lynskey MT. Childhood sexual abuse and psychiatric disorder in young adulthood: II. Psychiatric outcomes of childhood sexual abuse. J Am Acad Child Adolesc Psychiatry. 1996;35:1365–1374. doi: 10.1097/00004583-199610000-00024. [DOI] [PubMed] [Google Scholar]
- 107.Fergusson DM, Lynskey MT, Horwood LJ. Childhood sexual abuse and psychiatric disorder in young adulthood: I. Prevalence of sexual abuse and factors associated with sexual abuse. J Am Acad Child Adolesc Psychiatry. 1996;35:1355–1364. doi: 10.1097/00004583-199610000-00023. [DOI] [PubMed] [Google Scholar]
- 108.Brown J, Cohen P, Johnson JG, Smailes EM. Childhood abuse and neglect: Specificity of effects on adolescent and young adult depression and suicidality. J Am Acad Child Adolesc Psychiatry. 1999;38:1490–1496. doi: 10.1097/00004583-199912000-00009. [DOI] [PubMed] [Google Scholar]
- 109.Borowsky IW, Resnick MD, Ireland M, Blum RW. Suicide attempts among American Indian and Alaska native youth: Risk and protective factors. Archives of Pediatrics and Adolescent Medicine. 1999;153:573–580. doi: 10.1001/archpedi.153.6.573. [DOI] [PubMed] [Google Scholar]
- 110.Molnar BE, Buka SL, Kessler RC. Child sexual abuse and subsequent psychopathology: Results from the National Comorbidity Survey. Am J Public Health. 2001;91:753–760. doi: 10.2105/ajph.91.5.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Herrenkohl EC, Herrenkohl RC, Toedter LJ. Perspectives on the intergenerational transmission of abuse in The Dark Side of Families. In: Finkelhor D, Gelles RJ, Hotaling GT, Straus MA, editors. Current Family Violence Research. Beverly Hills, CA: Sage; 1983. pp. 305–316. [Google Scholar]
- 112.Caspi A, McClay J, Moffitt TE, Mill J, Martin J, Craig IW, Taylor A, Poulton R. Role of genotype in the cycle of violence in maltreated children. Science. 2002;297:851–854. doi: 10.1126/science.1072290. [DOI] [PubMed] [Google Scholar]
- 113.Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington H, McClay J, Mill J, Martin J, Braithwaite A, Poulton R. Influence of life stress on depression: Moderation by a polymorphism in the 5-HT gene. Science. 2003;301:386–389. doi: 10.1126/science.1083968. [DOI] [PubMed] [Google Scholar]
- 114.Molnar BE, Berkman LF, Buka SL. Psychopathology, childhood sexual abuse and other childhood adversities: Relative links to subsequent suicidal behavior in the U.S. Psychol Med. 2001;31:965–977. doi: 10.1017/s0033291701004329. [DOI] [PubMed] [Google Scholar]
- 115.Dinwiddie S, Heath AC, Dunne MP, Bucholz KK, Madden PAF, Slutske WS, Bierut L, Statham DB, Martin NG. Early sexual abuse and lifetime psychopathology: A co-twin-control study. Psychol Med. 2000;30:41–52. doi: 10.1017/s0033291799001373. [DOI] [PubMed] [Google Scholar]
- 116.Francis D, Diorio J, Liu D, Meaney M. Nongenomic transmission across generations of maternal behavior and stress responses in the rat. Science. 1999;286:1155–1158. doi: 10.1126/science.286.5442.1155. [DOI] [PubMed] [Google Scholar]
- 117.Liu D, Diorio J, Day JC, Francis D, Meaney M. Maternal care, hippocampal synaptogenesis and cognitive development in rats. Nature Neuroscience. 2000;3:799–806. doi: 10.1038/77702. [DOI] [PubMed] [Google Scholar]
- 118.Anisman H, Zaharia M, Meaney M, Merali Z. Do early-life events permanently alter behavioral and hormonal responses to stressors? International Journal of Developmental Neuroscience. 1998;16:149–164. doi: 10.1016/s0736-5748(98)00025-2. [DOI] [PubMed] [Google Scholar]
- 119.DeBellis MD. Developmental traumatology: The psychobiological development of maltreated children and its implications for research, treatment, and policy. Development and Psychopathology. 2001;13:539–564. doi: 10.1017/s0954579401003078. [DOI] [PubMed] [Google Scholar]
- 120.Manuck SB, Flory JD, McCaffery JM, Matthews KA, Mann JJ, Muldoon MF. Aggression, impulsivity, and central nervous system serotonergic responsivity in a nonpatient sample. Neuropsychopharmacology. 1998;19:287–299. doi: 10.1016/S0893-133X(98)00015-3. [DOI] [PubMed] [Google Scholar]
- 121.Mann JJ. Neurobiology of suicidal behavior. Nature Reviews Neuroscience. 2003;4:819–828. doi: 10.1038/nrn1220. [DOI] [PubMed] [Google Scholar]
- 122.Champoux M, Bennett A, Shannon C, Higley JD, Lesch KP, Suomi S. Serotonin transporter gene polymorphism, differential early rearing, and behavior in rhesus monkey neonates. Mol Psychiatry. 2002;7:1058–1063. doi: 10.1038/sj.mp.4001157. [DOI] [PubMed] [Google Scholar]
- 123.Pine DS, Coplan J, Wasserman GA, Miller LS, Fried JE, Davies M, Cooper TB, Greenhill L, Shaffer D, Parsons B. Neuroendocrine response to fenfluramine challenge in boys. Associations with aggressive behavior and adverse rearing. Archives of General Psychiatry. 1997;54:839–846. doi: 10.1001/archpsyc.1997.01830210083010. [DOI] [PubMed] [Google Scholar]
- 124.Kaufman J, Birmaher B, Perel J, Dahl R, Stull S, Brent D, Trubnick LA-SM, Ryan N. Serotonergic functioning in depressed abused children: Clinical and familial correlates. Biol Psychiatry. 1998;44:973–981. doi: 10.1016/s0006-3223(98)00203-0. [DOI] [PubMed] [Google Scholar]
- 125.Rutter M, Dunn J, Plomin R, Simonoff E, Pickles A, Maughan B, Ormel J, Meyer J, Eaves L. Integrating nature and nurture: Implications of person-environment correlations and interactions for developmental psychopathology. Development & Psychopathology. 1997;9:335–364. doi: 10.1017/s0954579497002083. [DOI] [PubMed] [Google Scholar]
- 126.Kelleher K, Chaffin M, Hollenberg J, Fischer E. Alcohol and drug disorders among physically abusive and neglectful parents in a community-based sample. Am J Public Health. 1994;84:1586–1590. doi: 10.2105/ajph.84.10.1586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Eaves L, Silberg J, Erkanli A. Resolving multiple epigenetic pathways to adolescent depression. J Child Psychol Psychiatry. 2003;44:1006–1014. doi: 10.1111/1469-7610.00185. [DOI] [PubMed] [Google Scholar]
- 128.Kaufman J, Yang BZ, Douglas-Palumberi H, Grasso D, Lipschitz D, Houshyar S, Krystal JH, Gelernter J. Brain-derived neurotrophic factor-5-HTTLPR gene interactions and environmental modifiers of depression in children. Biol Psychiatry. 2006;59:673–680. doi: 10.1016/j.biopsych.2005.10.026. [DOI] [PubMed] [Google Scholar]
- 129.Zalsman G, Huang Y-Y, Oquendo MA, Burke AK, Hu X-Z, Brent DA, Ellis SP, Goldman D, Mann JJ. Association of a triallelic serotonin transporter gene promoter polymorphism region (5-HTTLPR), with stressful life events and severity of depression. Am J Psychiatry. 2006;163:1588–1593. doi: 10.1176/ajp.2006.163.9.1588. [DOI] [PubMed] [Google Scholar]
- 130.Kaufman J, Yang BZ, Douglas-Palumberi H, Houshyar S, Lischitz D, Krystal JH, Gelernter J. Social supports and serotonin transporter gene moderate depression in maltreated children. Proc Natl Acad Sci USA. 2004;101:17316–17321. doi: 10.1073/pnas.0404376101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Fergusson DM, Lynskey MT. Adolescent resiliency to family adversity. J Child Psychol Psychiatry. 1996;37:281–292. doi: 10.1111/j.1469-7610.1996.tb01405.x. [DOI] [PubMed] [Google Scholar]
- 132.Fergusson DM, Woodward LJ, Horwood LJ. Risk factors and life processes associated with the onset of suicidal behaviour during adolescence and early adulthood. Psychol Med. 2000;30:23–39. doi: 10.1017/s003329179900135x. [DOI] [PubMed] [Google Scholar]


