Abstract
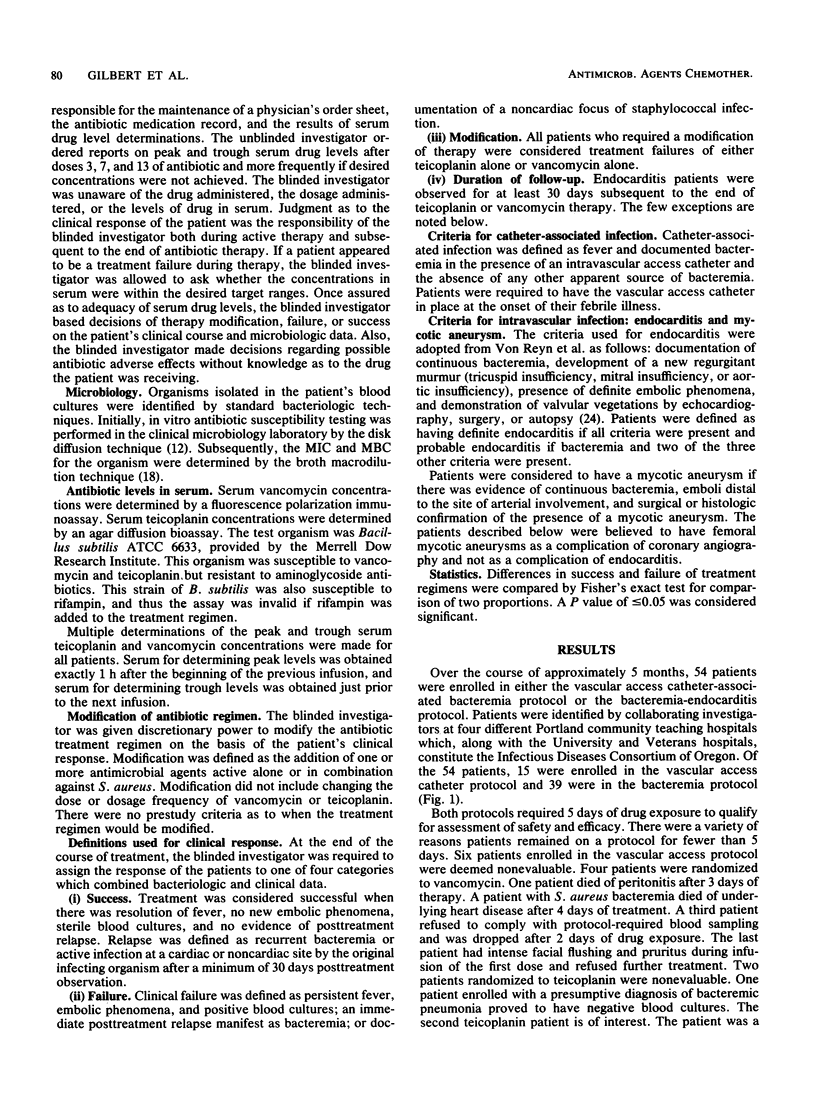
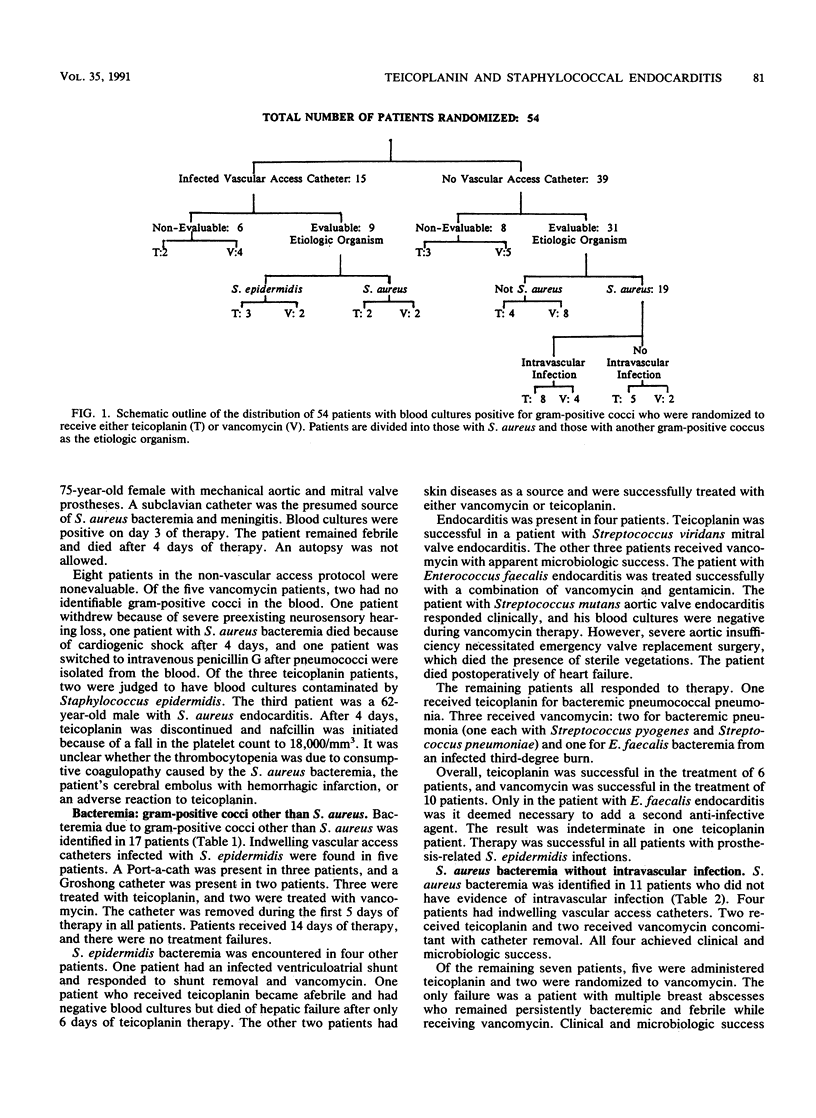
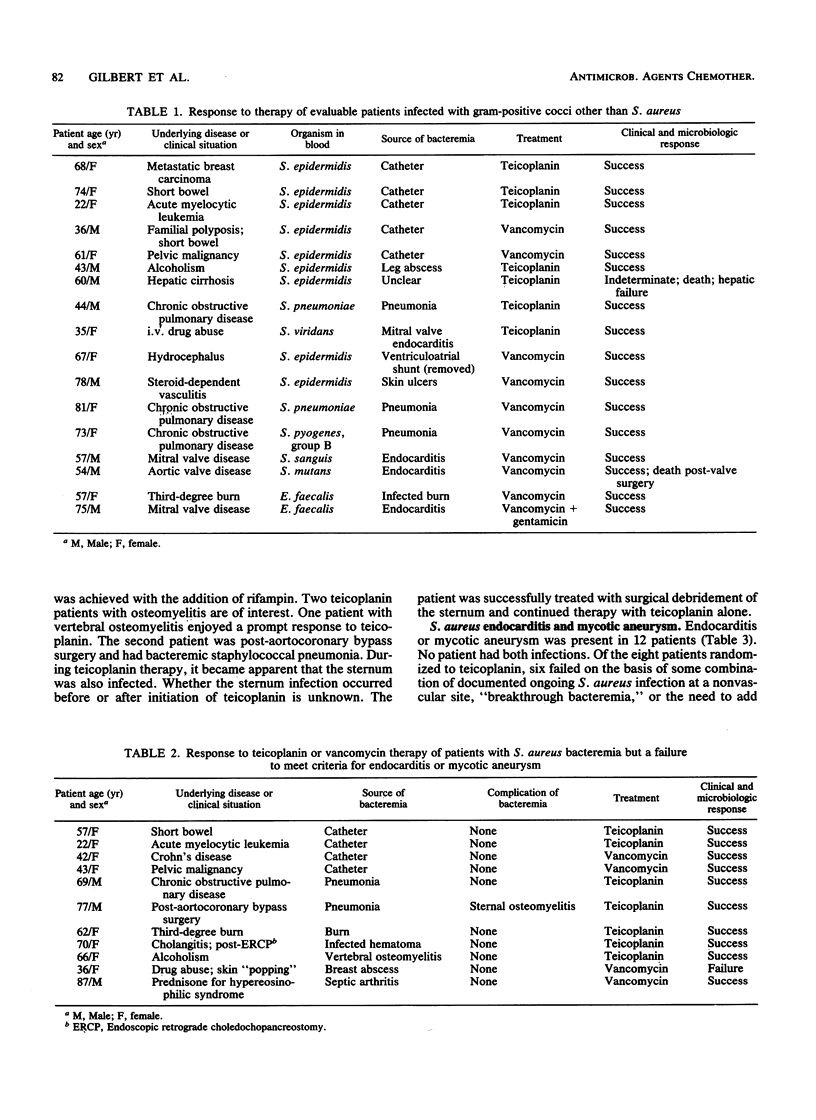
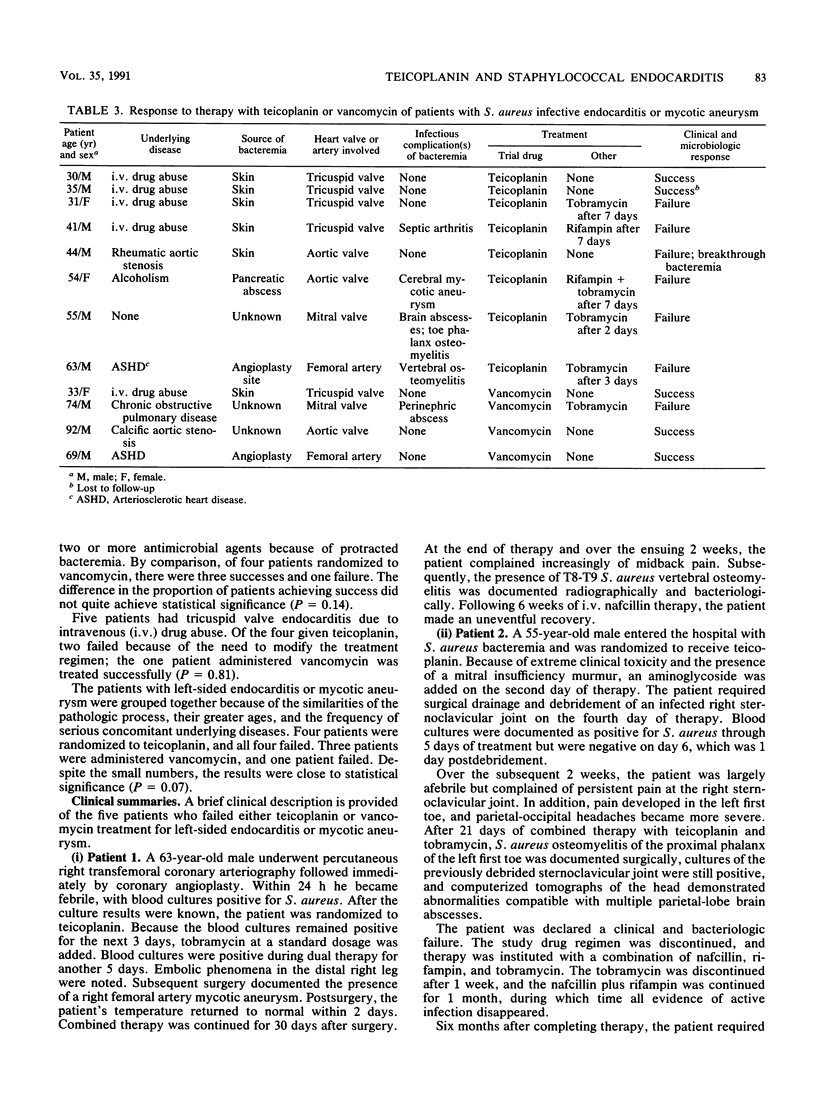
Patients with blood cultures positive for gram-positive cocci were enrolled in a prospective randomized double-blind comparative trial of vancomycin at 15 mg/kg every 12 h versus teicoplanin at 6 mg/kg every 12 h for three doses and then 6 mg/kg every 24 h. A total of 54 patients were randomized, and 40 were evaluable. Of the 40, 9 had infection of indwelling vascular catheters. Four infections were due to Staphylococcus aureus, and five were due to Staphylococcus epidermidis. In concert with catheter removal, all patients were treated successfully, regardless of which drug they were taking. Of 31 patients without an indwelling catheter, 19 were infected with S. aureus, and 12 of the 19 had either endocarditis or mycotic aneurysm. Six of eight patients given teicoplanin failed treatment, as opposed to one of four patients given vancomycin (P = 0.14). Of greater concern, four of four patients with left-sided endocarditis or mycotic aneurysm failed to recover when given teicoplanin, as opposed to one of three patients given vancomycin (P = 0.07). Although not quite statistically significant, the unexpectedly high number of treatment failures with teicoplanin resulted in a decision to discontinue patient enrollment. It is suggested that future trials explore the efficacy of larger doses of teicoplanin.
Full text
PDF



Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bayer A. S., Crowell D. J., Yih J., Bradley D. W., Norman D. C. Comparative pharmacokinetics and pharmacodynamics of amikacin and ceftazidime in tricuspid and aortic vegetations in experimental Pseudomonas endocarditis. J Infect Dis. 1988 Aug;158(2):355–359. doi: 10.1093/infdis/158.2.355. [DOI] [PubMed] [Google Scholar]
- Brummitt C. F., Kravitz G. R., Granrud G. A., Herzog C. A. Femoral endarteritis due to Staphylococcus aureus complicating percutaneous transluminal coronary angioplasty. Am J Med. 1989 Jun;86(6 Pt 2):822–824. doi: 10.1016/0002-9343(89)90480-4. [DOI] [PubMed] [Google Scholar]
- Calain P., Krause K. H., Vaudaux P., Auckenthaler R., Lew D., Waldvogel F., Hirschel B. Early termination of a prospective, randomized trial comparing teicoplanin and flucloxacillin for treating severe staphylococcal infections. J Infect Dis. 1987 Feb;155(2):187–191. doi: 10.1093/infdis/155.2.187. [DOI] [PubMed] [Google Scholar]
- Chambers H. F., Kennedy S. Effects of dosage, peak and trough concentrations in serum, protein binding, and bactericidal rate on efficacy of teicoplanin in a rabbit model of endocarditis. Antimicrob Agents Chemother. 1990 Apr;34(4):510–514. doi: 10.1128/aac.34.4.510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chambers H. F., Miller R. T., Newman M. D. Right-sided Staphylococcus aureus endocarditis in intravenous drug abusers: two-week combination therapy. Ann Intern Med. 1988 Oct 15;109(8):619–624. doi: 10.7326/0003-4819-109-8-619. [DOI] [PubMed] [Google Scholar]
- Contrepois A., Joly V., Abel L., Pangon B., Vallois J. M., Carbon C. The pharmacokinetics and extravascular diffusion of teicoplanin in rabbits and comparative efficacy with vancomycin in an experimental endocarditis model. J Antimicrob Chemother. 1988 May;21(5):621–631. doi: 10.1093/jac/21.5.621. [DOI] [PubMed] [Google Scholar]
- Cremieux A. C., Maziere B., Vallois J. M., Ottaviani M., Azancot A., Raffoul H., Bouvet A., Pocidalo J. J., Carbon C. Evaluation of antibiotic diffusion into cardiac vegetations by quantitative autoradiography. J Infect Dis. 1989 May;159(5):938–944. doi: 10.1093/infdis/159.5.938. [DOI] [PubMed] [Google Scholar]
- Del Favero A., Menichetti F., Guerciolini R., Bucaneve G., Baldelli F., Aversa F., Terenzi A., Davis S., Pauluzzi S. Prospective randomized clinical trial of teicoplanin for empiric combined antibiotic therapy in febrile, granulocytopenic acute leukemia patients. Antimicrob Agents Chemother. 1987 Jul;31(7):1126–1129. doi: 10.1128/aac.31.7.1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eggleston M., Ofosu J. Teicoplanin--a new agent for gram-positive bacterial infections. Infect Control Hosp Epidemiol. 1988 May;9(5):209–211. doi: 10.1086/645836. [DOI] [PubMed] [Google Scholar]
- Eng R. H., Bishburg E., Smith S. M., Scadutto P. Staphylococcus aureus bacteremia during therapy. J Infect Dis. 1987 Jun;155(6):1331–1335. doi: 10.1093/infdis/155.6.1331. [DOI] [PubMed] [Google Scholar]
- Galanakis N., Giamarellou H., Vlachogiannis N., Dendrinos C., Daikos G. K. Poor efficacy of teicoplanin in treatment of deep-seated staphylococcal infections. Eur J Clin Microbiol Infect Dis. 1988 Apr;7(2):130–134. doi: 10.1007/BF01963065. [DOI] [PubMed] [Google Scholar]
- Greenwood D., Bidgood K., Turner M. A comparison of the responses of staphylococci and streptococci to teicoplanin and vancomycin. J Antimicrob Chemother. 1987 Aug;20(2):155–164. doi: 10.1093/jac/20.2.155. [DOI] [PubMed] [Google Scholar]
- Greenwood D. Microbiological properties of teicoplanin. J Antimicrob Chemother. 1988 Jan;21 (Suppl A):1–13. doi: 10.1093/jac/21.suppl_a.1. [DOI] [PubMed] [Google Scholar]
- Korzeniowski O., Sande M. A. Combination antimicrobial therapy for Staphylococcus aureus endocarditis in patients addicted to parenteral drugs and in nonaddicts: A prospective study. Ann Intern Med. 1982 Oct;97(4):496–503. doi: 10.7326/0003-4819-97-4-496. [DOI] [PubMed] [Google Scholar]
- Leport C., Perronne C., Massip P., Canton P., Leclercq P., Bernard E., Lutun P., Garaud J. J., Vilde J. L. Evaluation of teicoplanin for treatment of endocarditis caused by gram-positive cocci in 20 patients. Antimicrob Agents Chemother. 1989 Jun;33(6):871–876. doi: 10.1128/aac.33.6.871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levine D. P., Cushing R. D., Jui J., Brown W. J. Community-acquired methicillin-resistant Staphylococcus aureus endocarditis in the Detroit Medical Center. Ann Intern Med. 1982 Sep;97(3):330–338. doi: 10.7326/0003-4819-97-3-330. [DOI] [PubMed] [Google Scholar]
- Pallanza R., Berti M., Goldstein B. P., Mapelli E., Randisi E., Scotti R., Arioli V. Teichomycin: in-vitro and in-vivo evaluation in comparison with other antibiotics. J Antimicrob Chemother. 1983 May;11(5):419–425. doi: 10.1093/jac/11.5.419. [DOI] [PubMed] [Google Scholar]
- Pohlod D. J., Saravolatz L. D., Somerville M. M. In-vitro susceptibility of gram-positive cocci to LY146032 teicoplanin, sodium fusidate, vancomycin, and rifampicin. J Antimicrob Chemother. 1987 Aug;20(2):197–202. doi: 10.1093/jac/20.2.197. [DOI] [PubMed] [Google Scholar]
- Small P. M., Chambers H. F. Vancomycin for Staphylococcus aureus endocarditis in intravenous drug users. Antimicrob Agents Chemother. 1990 Jun;34(6):1227–1231. doi: 10.1128/aac.34.6.1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuazon C. U., Washburn D. Teicoplanin and rifampicin singly and in combination in the treatment of experimental Staphylococcus epidermidis endocarditis in the rabbit model. J Antimicrob Chemother. 1987 Aug;20(2):233–237. doi: 10.1093/jac/20.2.233. [DOI] [PubMed] [Google Scholar]
- Verbist L., Tjandramaga B., Hendrickx B., Van Hecken A., Van Melle P., Verbesselt R., Verhaegen J., De Schepper P. J. In vitro activity and human pharmacokinetics of teicoplanin. Antimicrob Agents Chemother. 1984 Dec;26(6):881–886. doi: 10.1128/aac.26.6.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Von Reyn C. F., Levy B. S., Arbeit R. D., Friedland G., Crumpacker C. S. Infective endocarditis: an analysis based on strict case definitions. Ann Intern Med. 1981 Apr;94(4 Pt 1):505–518. doi: 10.7326/0003-4819-94-4-505. [DOI] [PubMed] [Google Scholar]
- Williams A. H., Grüneberg R. N. Teicoplanin revisited. J Antimicrob Chemother. 1988 Oct;22(4):397–401. doi: 10.1093/jac/22.4.397. [DOI] [PubMed] [Google Scholar]
- Wise R., Donovan I. A., McNulty C. A., Waldron R., Andrews J. M. Teicoplanin, its pharmacokinetics, blister and peritoneal fluid penetration. J Hosp Infect. 1986 Mar;7 (Suppl A):47–55. doi: 10.1016/0195-6701(86)90007-1. [DOI] [PubMed] [Google Scholar]
- de Lalla F., Santoro D., Rinaldi E., Suter F., Cruciani M., Guaglianone M. H., Rizzardini G., Pellegata G. Teicoplanin in the treatment of infections by staphylococci, Clostridium difficile and other gram-positive bacteria. J Antimicrob Chemother. 1989 Jan;23(1):131–142. doi: 10.1093/jac/23.1.131. [DOI] [PubMed] [Google Scholar]


