Abstract
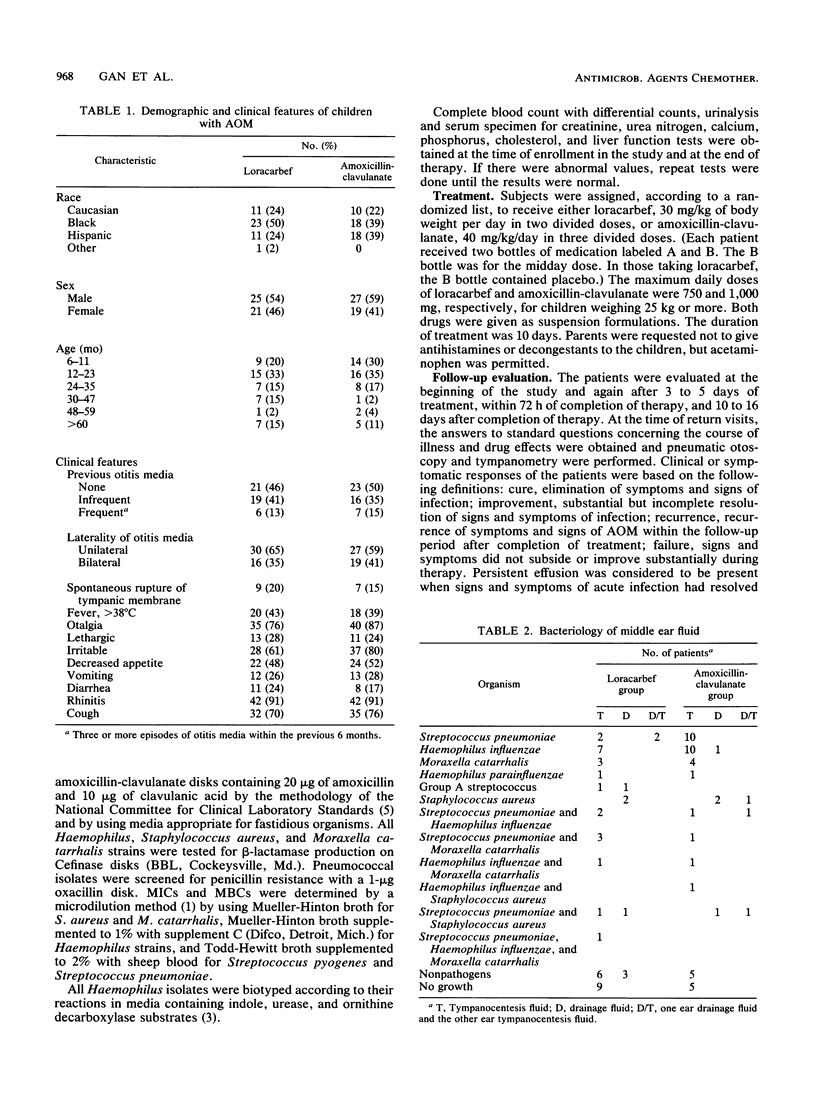
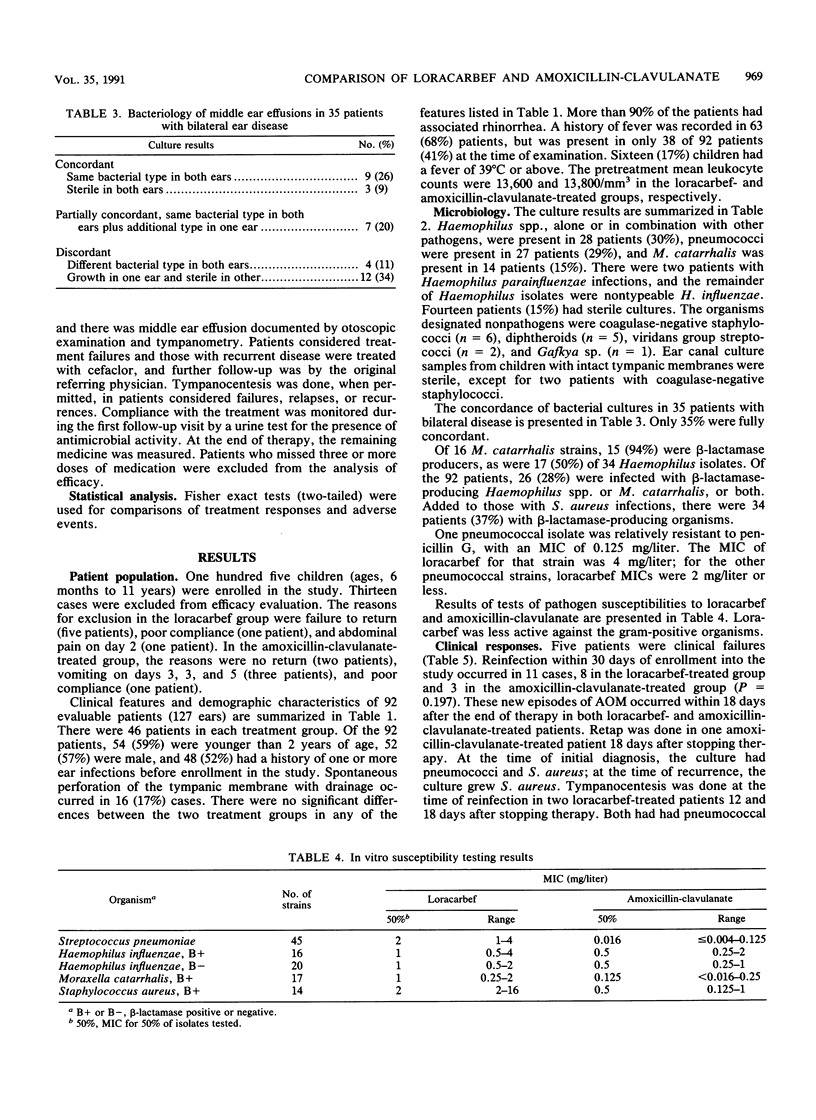
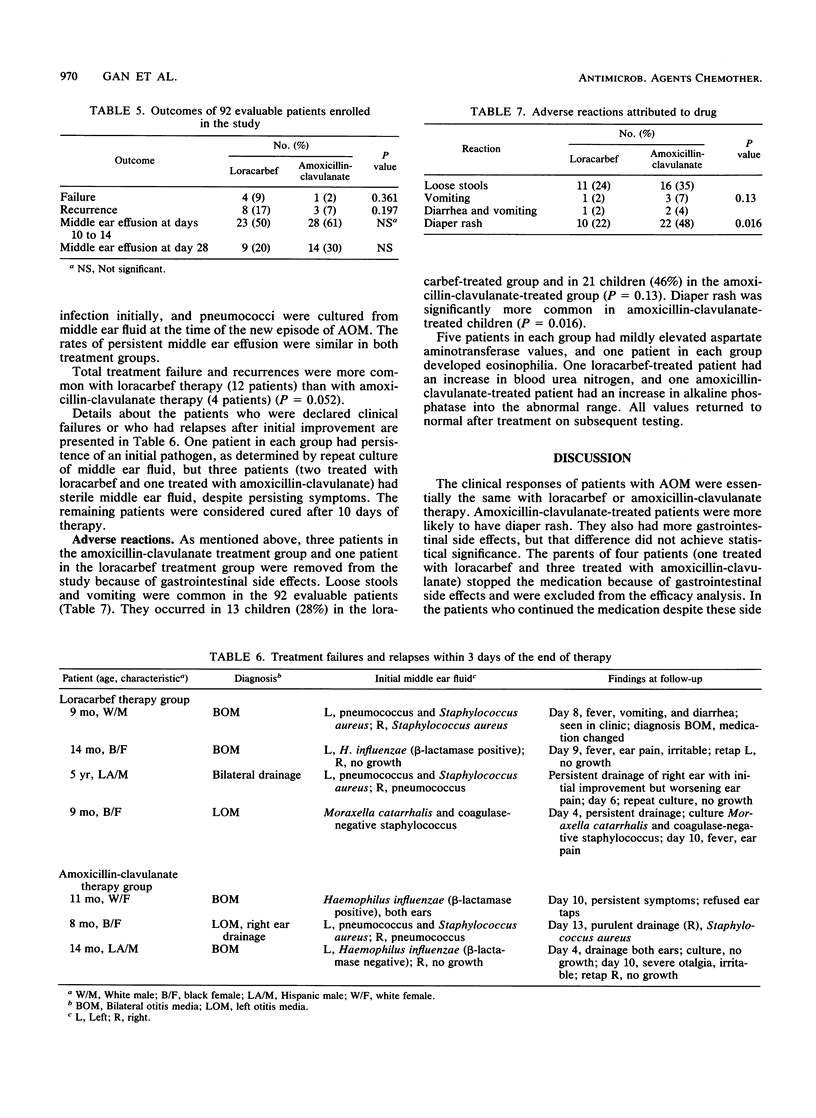
One hundred five infants and children with acute otitis media were randomized to therapy with loracarbef, an experimental carbacephem antibiotic, or amoxicillin-clavulanate (Augmentin), an approved drug for this disease. Ninety-two were evaluable (46 in each group). Middle ear fluid samples obtained for culture before therapy grew Haemophilus spp. in 30% of cases, pneumococci in 29% of cases, and Moraxella catarrhalis in 15% of cases. beta-Lactamase-producing bacteria were found in 37% of patients. Clinical failure occurred in four loracarbef-treated patients and one amoxicillin-clavulanate-treated patient (P = 0.361). Recurrence of acute otitis media was more common in the 2 to 3 weeks after loracarbef treatment (eight patients) than it was after amoxicillin-clavulanate therapy (three patients), but not significantly so (P = 0.197). Thus, combined failure and recurrence occurred in 12 loracarbef-treated patients and four amoxicillin-clavulanate-treated patients (P = 0.052). Gastrointestinal side effects occurred in 13 loracarbef-treated and 21 amoxicillin-clavulanate-treated patients (P = 0.13). Diaper rash was more common with amoxicillin-clavulanate (22 patients) than with loracarbef (10 patients; P = 0.016). Satisfactory results were achieved with both antibiotics, and adverse effects, although common, were minor.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Hendrickse W. A., Kusmiesz H., Shelton S., Nelson J. D. Five vs. ten days of therapy for acute otitis media. Pediatr Infect Dis J. 1988 Jan;7(1):14–23. doi: 10.1097/00006454-198801000-00005. [DOI] [PubMed] [Google Scholar]
- Kovatch A. L., Wald E. R., Michaels R. H. beta-Lactamase-producing Branhamella catarrhalis causing otitis media in children. J Pediatr. 1983 Feb;102(2):261–264. doi: 10.1016/s0022-3476(83)80537-x. [DOI] [PubMed] [Google Scholar]
- Nelson J. D., Shelton S., Kusmiesz H. Pharmacokinetics of LY163892 in infants and children. Antimicrob Agents Chemother. 1988 Nov;32(11):1738–1739. doi: 10.1128/aac.32.11.1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shelton S., Nelson J. D. In vitro susceptibilities of common pediatric pathogens to LY163892. Antimicrob Agents Chemother. 1988 Feb;32(2):268–270. doi: 10.1128/aac.32.2.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shurin P. A., Marchant C. D., Kim C. H., Van Hare G. F., Johnson C. E., Tutihasi M. A., Knapp L. J. Emergence of beta-lactamase-producing strains of Branhamella catarrhalis as important agents of acute otitis media. Pediatr Infect Dis. 1983 Jan-Feb;2(1):34–38. doi: 10.1097/00006454-198301000-00009. [DOI] [PubMed] [Google Scholar]


