Abstract
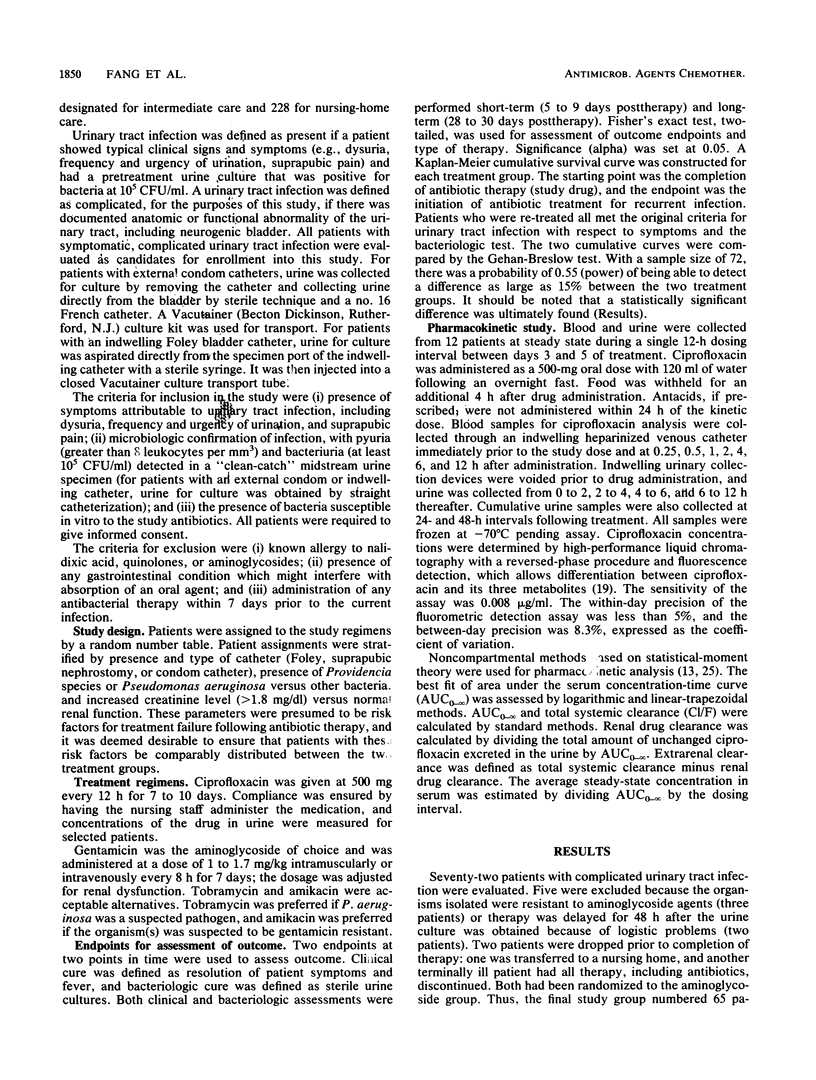
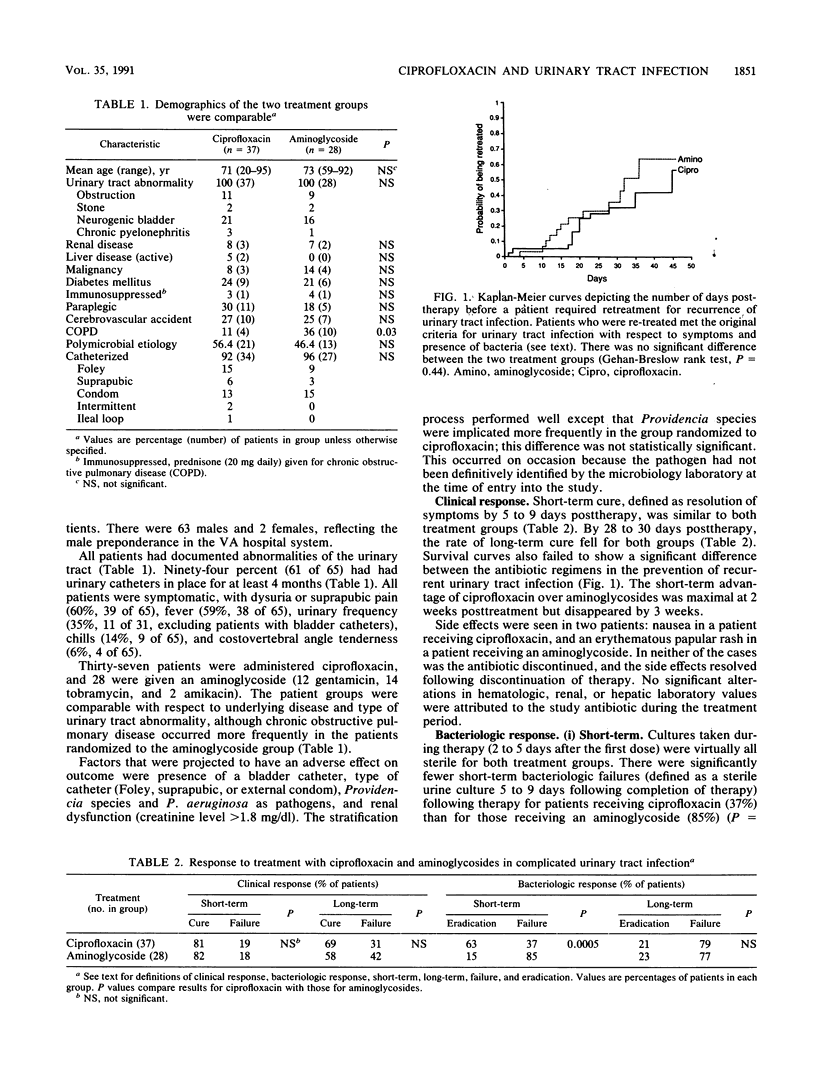
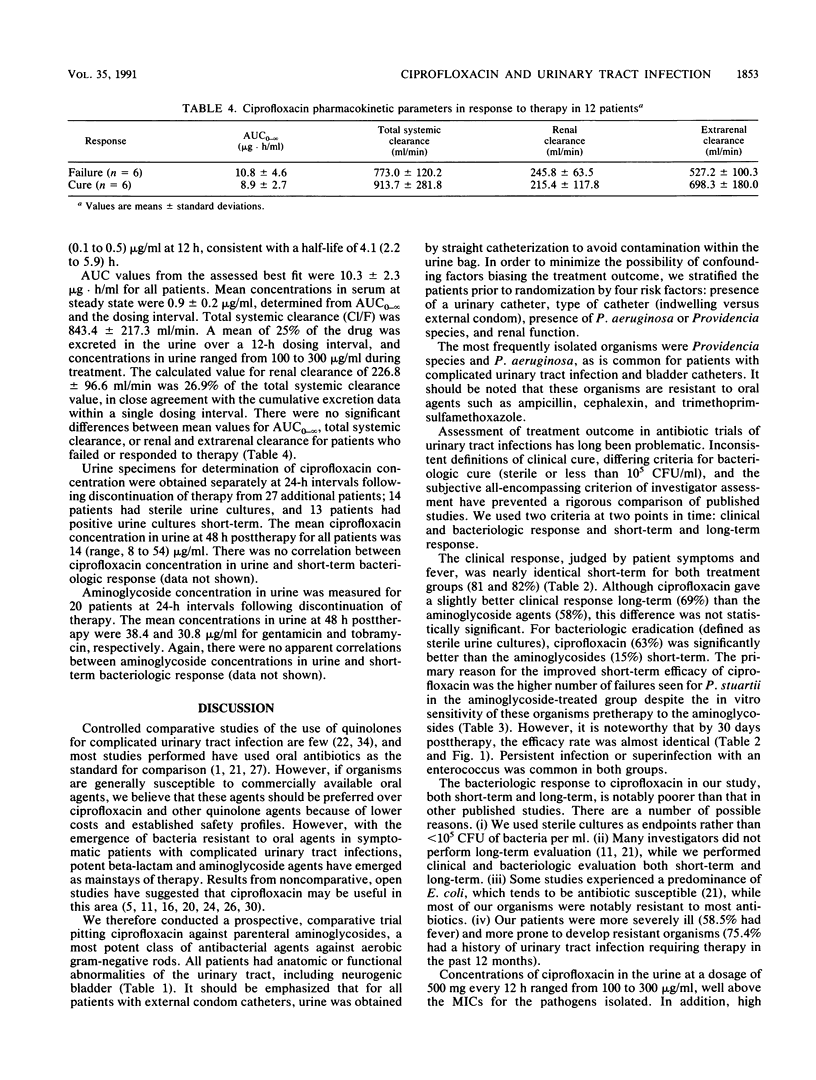
The efficacy of oral ciprofloxacin was compared with that of parenteral aminoglycoside for therapy of complicated urinary tract infection in a prospective randomized trial. The setting was a chronic-care Veterans Administration facility in which long-term bladder catheterization and resistant bacteria were common. Sixty-five consecutive patients were stratified for presence and type of bladder catheter, the presence of Providencia and Pseudomonas aeruginosa organisms versus other urinary pathogens, and renal dysfunction. A pharmacokinetic study of ciprofloxacin concentrations in serum and urine was performed with selected patients. Urinary catheters were present in 94%. All patients were symptomatic, and 58.5% had fever. Ciprofloxacin, 500 mg every 12 h orally, was compared with parenteral aminoglycoside for 7 to 10 days. Clinical response, defined by resolution of symptoms and fever at 5 to 9 days posttherapy (short-term) and 28 to 30 days posttherapy (long-term), was essentially identical for both treatment groups. Bacteriologic response, defined by sterile urine cultures, showed that ciprofloxacin was significantly more efficacious (P = 0.0005) than aminoglycoside at 5 to 9 days posttherapy. However, by 28 to 30 days, the response rate was essentially identical. Emergence of resistance to the study antibiotic was seen in 62 and 70% of those who did not show a bacteriological response and were receiving ciprofloxacin and aminoglycosides, respectively. Concentrations of ciprofloxacin and aminoglycoside in the urine substantially exceeded the MIC for the urinary pathogens isolated, although these concentrations did not correlate with short-term bacteriologic response for either antibiotic. Ciprofloxacin was efficacious in complicated urinary tract infection compared with the current standard of parenteral aminoglycoside among catheterized patients with relatively resistant bacteria.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Allais J. M., Preheim L. C., Cuevas T. A., Roccaforte J. S., Mellencamp M. A., Bittner M. J. Randomized, double-blind comparison of ciprofloxacin and trimethoprim-sulfamethoxazole for complicated urinary tract infections. Antimicrob Agents Chemother. 1988 Sep;32(9):1327–1330. doi: 10.1128/aac.32.9.1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjork D. T., Pelletier L. L., Tight R. R. Urinary tract infections with antibiotic resistant organisms in catheterized nursing home patients. Infect Control. 1984 Apr;5(4):173–176. doi: 10.1017/s0195941700059178. [DOI] [PubMed] [Google Scholar]
- Boelaert J., Valcke Y., Schurgers M., Daneels R., Rosseneu M., Rosseel M. T., Bogaert M. G. The pharmacokinetics of ciprofloxacin in patients with impaired renal function. J Antimicrob Chemother. 1985 Jul;16(1):87–93. doi: 10.1093/jac/16.1.87. [DOI] [PubMed] [Google Scholar]
- Boerema J., Boll B., Muytjens H., Branolte J. Efficacy and safety of ciprofloxacin (Bay 0 9867) in the treatment of patients with complicated urinary tract infections. J Antimicrob Chemother. 1985 Aug;16(2):211–217. doi: 10.1093/jac/16.2.211. [DOI] [PubMed] [Google Scholar]
- Chin N. X., Neu H. C. Ciprofloxacin, a quinolone carboxylic acid compound active against aerobic and anaerobic bacteria. Antimicrob Agents Chemother. 1984 Mar;25(3):319–326. doi: 10.1128/aac.25.3.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chinn R. H., Maskell R., Mead J. A., Polak A. Renal stones and urinary infection: a study of antibiotic treatment. Br Med J. 1976 Dec 11;2(6049):1411–1413. doi: 10.1136/bmj.2.6049.1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crump B., Wise R., Dent J. Pharmacokinetics and tissue penetration of ciprofloxacin. Antimicrob Agents Chemother. 1983 Nov;24(5):784–786. doi: 10.1128/aac.24.5.784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fihn S. D., Stamm W. E. Interpretation and comparison of treatment studies for uncomplicated urinary tract infections in women. Rev Infect Dis. 1985 Jul-Aug;7(4):468–478. doi: 10.1093/clinids/7.4.468. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick L. A., Bilezikian J. P. Acute primary hyperparathyroidism. Am J Med. 1987 Feb;82(2):275–282. doi: 10.1016/0002-9343(87)90068-4. [DOI] [PubMed] [Google Scholar]
- Freeman R. B., Smith W. M., Richardson J. A., Hennelly P. J., Thurm R. H., Urner C., Vaillancourt J. A., Griep R. J., Bromer L. Long-term therapy for chronic bacteriuria in men. U.S. Public Health Service cooperative study. Ann Intern Med. 1975 Aug;83(2):133–147. doi: 10.7326/0003-4819-83-2-133. [DOI] [PubMed] [Google Scholar]
- Gasser T. C., Ebert S. C., Graversen P. H., Madsen P. O. Ciprofloxacin pharmacokinetics in patients with normal and impaired renal function. Antimicrob Agents Chemother. 1987 May;31(5):709–712. doi: 10.1128/aac.31.5.709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gleckman R. A. Treatment duration for urinary tract infections in adults. Antimicrob Agents Chemother. 1987 Jan;31(1):1–5. doi: 10.1128/aac.31.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez M. A., Uribe F., Moisen S. D., Fuster A. P., Selen A., Welling P. G., Painter B. Multiple-dose pharmacokinetics and safety of ciprofloxacin in normal volunteers. Antimicrob Agents Chemother. 1984 Nov;26(5):741–744. doi: 10.1128/aac.26.5.741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kresken M., Wiedemann B. Development of resistance to nalidixic acid and the fluoroquinolones after the introduction of norfloxacin and ofloxacin. Antimicrob Agents Chemother. 1988 Aug;32(8):1285–1288. doi: 10.1128/aac.32.8.1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger J. N., Kaiser D. L., Wenzel R. P. Nosocomial urinary tract infections: secular trends, treatment and economics in a university hospital. J Urol. 1983 Jul;130(1):102–106. doi: 10.1016/s0022-5347(17)50980-5. [DOI] [PubMed] [Google Scholar]
- Leigh D. A., Emmanuel F. X., Petch V. J. Ciprofloxacin therapy in complicated urinary tract infections caused by Pseudomonas aeruginosa and other resistant bacteria. J Antimicrob Chemother. 1986 Nov;18 (Suppl 500):117–121. doi: 10.1093/jac/18.supplement_d.117. [DOI] [PubMed] [Google Scholar]
- Leigh D. A., Smith E. C., Marriner J. Comparative study using norfloxacin and amoxycillin in the treatment of complicated urinary tract infections in geriatric patients. J Antimicrob Chemother. 1984 May;13 (Suppl B):79–83. doi: 10.1093/jac/13.suppl_b.79. [DOI] [PubMed] [Google Scholar]
- Malinverni R., Glauser M. P. Comparative studies of fluoroquinolones in the treatment of urinary tract infections. Rev Infect Dis. 1988 Jan-Feb;10 (Suppl 1):S153–S163. doi: 10.1093/clinids/10.supplement_1.s153. [DOI] [PubMed] [Google Scholar]
- Neu H. C. Ciprofloxacin: an overview and prospective appraisal. Am J Med. 1987 Apr 27;82(4A):395–404. [PubMed] [Google Scholar]
- Preheim L. C., Cuevas T. A., Roccaforte J. S., Mellencamp M. A., Bittner M. J. Oral ciprofloxacin in the treatment of elderly patients with complicated urinary tract infections due to trimethoprim/sulfamethoxazole-resistant bacteria. Am J Med. 1987 Apr 27;82(4A):295–300. [PubMed] [Google Scholar]
- Rocci M. L., Jr, Jusko W. J. LAGRAN program for area and moments in pharmacokinetic analysis. Comput Programs Biomed. 1983 Jun;16(3):203–216. doi: 10.1016/0010-468x(83)90082-x. [DOI] [PubMed] [Google Scholar]
- Ryan J. L., Berenson C. S., Greco T. P., Mangi R. J., Sims M., Thornton G. F., Andriole V. T. Oral ciprofloxacin in resistant urinary tract infections. Am J Med. 1987 Apr 27;82(4A):303–306. [PubMed] [Google Scholar]
- Sabbaj J., Hoagland V. L., Cook T. Norfloxacin versus co-trimoxazole in the treatment of recurring urinary tract infections in men. Scand J Infect Dis Suppl. 1986;48:48–53. [PubMed] [Google Scholar]
- Sanders W. E., Jr Efficacy, safety, and potential economic benefits of oral ciprofloxacin in the treatment of infections. Rev Infect Dis. 1988 May-Jun;10(3):528–543. doi: 10.1093/clinids/10.3.528. [DOI] [PubMed] [Google Scholar]
- Stark R. P., Maki D. G. Bacteriuria in the catheterized patient. What quantitative level of bacteriuria is relevant? N Engl J Med. 1984 Aug 30;311(9):560–564. doi: 10.1056/NEJM198408303110903. [DOI] [PubMed] [Google Scholar]
- Van Poppel H., Wegge M., Dammekens H., Chysky V. Ciprofloxacin in the treatment of urinary tract infection in patients with multiple sclerosis. Eur J Clin Microbiol. 1986 Apr;5(2):251–253. doi: 10.1007/BF02014002. [DOI] [PubMed] [Google Scholar]
- Warren J. W., Muncie H. L., Jr, Hall-Craggs M. Acute pyelonephritis associated with bacteriuria during long-term catheterization: a prospective clinicopathological study. J Infect Dis. 1988 Dec;158(6):1341–1346. doi: 10.1093/infdis/158.6.1341. [DOI] [PubMed] [Google Scholar]
- Wise R., Andrews J. M., Edwards L. J. In vitro activity of Bay 09867, a new quinoline derivative, compared with those of other antimicrobial agents. Antimicrob Agents Chemother. 1983 Apr;23(4):559–564. doi: 10.1128/aac.23.4.559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfson J. S., Hooper D. C. Treatment of genitourinary tract infections with fluoroquinolones: activity in vitro, pharmacokinetics, and clinical efficacy in urinary tract infections and prostatitis. Antimicrob Agents Chemother. 1989 Oct;33(10):1655–1661. doi: 10.1128/aac.33.10.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]


