Abstract
Objective
To identify collaborative instances and hindrances and to produce a model of collaborative practice.
Methods
A 12 month (2005–6) mixed methods clinical case study in a large UK ambulance trust. Collaboration was measured through direct observational ratings of communication skills, teamwork and leadership with 24 multiprofessional emergency care practitioners (ECPs); interviews with 45 ECPs and stakeholders; and an audit of 611 patients.
Results
Quantitative observational ratings indicated that the higher the leadership rating the greater the communication ability (p⩽0.001) and teamwork (p⩽0.001), and the higher grade ECPs were rated more highly on their leadership performance. From the patient audit, influences and outputs of collaborative practice are revealed: mean time on scene was 47 mins; 62% were not conveyed; 38% were referred, mainly to accident and emergency; ECPs claimed to make the referral decision in 87% of cases with a successful referral in 96% of cases; and in 66% of cases ECPs claimed that their intervention prevented an acute trust admission. The qualitative interview findings, final collaborative model and recommendations are reported in another paper.
Conclusions
The collaborative performance of ECPs varies, but the ECPs' role does appear to have an impact on collaborative practices and patient care. Final recommendations are reported with the qualitative results elsewhere.
This paper is the first of a two part report (the second paper presents qualitative and summative findings1) which summarises the findings of a clinical study focusing on interprofessional collaboration in unscheduled out‐of‐hospital emergency care. Pressure is being applied on all those involved in health care to develop treatment and referral pathways for a “seamless service”. For ambulance services a series of reports are calling for change—for example, enhanced collaborative working and the development of emergency care networks2,3,4 with the objective of the “right response first time, in time”.5 Part of these developments has been the development of the emergency care practitioner (ECP) role,6 defined as an “advanced practitioner (paramedic or nurse) capable of assessing, treating and discharging/referring patients at the scene”.5
Work addressing interprofessional collaboration has identified some of the key characteristics of collaborative working7—for example, shared decision making, partnership working, mutual dependency and power sharing.8 Work in the education field drives forward this agenda arguing that interdisciplinary education may reduce medical errors,9 and enhances team working in the community and emergency room.10,11
For the ECP there is a national debate about how the role may develop. However, in relation to collaboration, there is some evidence that they are proactive in building inter‐agency links and developing patient referral processes with general practitioners and other agencies.12 A recent consultation document13 suggests that ECPs should be expert communicators who are comfortable in a multiprofessional environment.
For this study we focused on ECPs (paramedics and nurses) from the Westcountry Ambulance Service NHS Trust (WAST) in the UK, who had completed a 3 month certificate level programme (designed by the Changing Workforce Programme (DH) and University of Coventry) (level 1 ECPs); or Bachelors and Masters level graduates who had completed a BSc in Emergency Care or Masters degree in Advanced Healthcare Practice at the University of Plymouth (UK) (level 3 ECPs); or ECPs who were “in‐training” for an ECP role.
The objectives of the study were to identify instances and hindrances to interprofessional collaboration and to develop a model of collaboration for out‐of‐hospital unscheduled care and other relevant fields. Our research questions included the following: When and with whom do ECPs collaborate (and fail to collaborate)? What are the specific benefits of interprofessional collaboration? What are the key requirements and attributes for interprofessional collaboration?
Interprofessional collaboration was defined as “working in a positive association with more than one professional group”. We took a clinical case study design incorporating quantitative observational approaches, a patient audit, and interviews with ECPs and stakeholders using generic qualitative methods.1 Communication and team work, which included situational leadership roles, emerged from the literature review as fundamental to collaborative working,14,15,16,17 and applicable tools were selected to measure these factors (additional influences on collaborative working are reported in the qualitative findings1). The patient audit identified the influences and outputs of collaborative practice.
METHODS
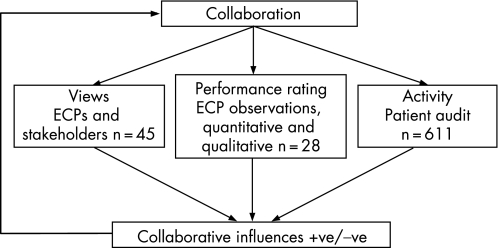
A mixed methods clinical case study (fig 1) based on participants (ECPs and stakeholders) from West Cornwall, West and East Devon. Full National Health Service ethics approval was obtained for observation and interviews of ECPs and stakeholders (patient consent was not a formal requirement of approval) A sample power estimate was calculated for all the quantitative ratings (leadership, team work, communication) from which a purposive sample of ECP participants was selected to include a range of perspectives from applicable personnel. Observational ratings and the patient audit are described below and interviews in the second qualitative report.1
Figure 1 Methods of data collection.
Observational ratings
Three trained observers were used to observe practice, particularly episodes of collaboration. Three tools were selected to measure and rate interactions (appendix 1; to view appendix 1 visit the EMJ website—http://emj.bmj.com/supplemental): the Communication Competence Questionnaire (CCQ)18 for rating communication skills, the “Emergency Team Dynamics” (ETD)19 for team work rating, and an adapted Leadership Behaviour Description Questionnaire (LBDQ)19,20,21 which includes two sub scales—“consideration” denoting the “extent to which leaders show consideration toward members of the team”;20 and “initiating structure” which denotes time bound command and control behaviours. All observed ECPs were rated on their communication ability, but ratings of leadership and team work were only performed in settings where the ECP was working as part of a team (>2 individuals). We hypothesised that there would be an improvement in leadership, communication and team work based on clinical experience and education.
Recruitment
As a purposive sample we aimed to identify a range of ECPs (who were representative of the population), covering gender, profession (nurse/paramedic), and educational qualifications. Potential ECP participants were invited to be involved in the study and arrangements made for a first meeting at which the study was outlined and consent obtained. The process for identifying stakeholders mirrored that of ECPs.1
Patient audit
All ECPs in the employ of WAST were asked to complete an audit form on all patients over two 3 week periods in February 2006 and April/May 2006. The form was adapted from the current (2006) ECP National Audit (appendix 2; to view appendix 2 visit the EMJ website—http://emj.bmj.com/supplemental) and included demographic, treatment and referral details/rates and questions relating to collaborative and referral practice.
Data analysis
Parametric and non‐parametric statistical analysis was selected dependant on the data distribution. Descriptive statistics for demographic data and Student's t tests (t) for interval data, Mann‐Whitney (z) for ordinal and χ2 tests (with Yates correction) for nominal data, and Pearson's correlation (r) and Spearman's (ρ) as the non‐paramedic equivalent. Approximate 95% confidence intervals (CI) for mean and proportion differences was estimated by confidence interval analysis software.22 Numerical data were analysed with SPSS version 11.5 software. All tests for statistical significance were two‐tailed, unless indicated, with the level of significance at p = 0.05.
Results
Validity and reliability of the rating scales
LBDQ and CCQ have been previously identified as having a high validity and reliability.18,19,20,21 In this study all three scales (including ETD) demonstrated good face and content validity, assessed by the research team and two external experts. The internal reliability/consistency (Cronbach's α) for all the scales was good (>82%).
Observational ratings
Between November 2005 and May 2006 a sample of 24 ECPs (a 44% sample from 55 ECPs) were observed on 28 occasions by three trained observers for periods of 5–12 h. Where repeat visits were made it was to a second area of work (a general practice or out‐of‐hours doctors service). ECPs were observed during day and night shifts in a range of settings (for example, patients' homes, road traffic accidents and general practice) with a focus on their collaborative practice, which included communication, team work and leadership ratings. The researchers took a non‐participatory observational role to remain as unobtrusive as possible. The researcher withdrew where the ECP was undertaking intimate or personal patient care.
A global assessment of leadership, team work and communication, in a wide range of situations (urgent and non‐urgent) was made at the end of each observation, using the afore mentioned scales. Twenty‐one male ECPs were observed and three females, all over 31 years of age. Three had primary qualifications as nurses and 21 were paramedics, two had dual qualifications. Fifteen were qualified at certificate level (level 1), seven at bachelor's level, and two at master's level (both identified as level 3 practitioners). Thirteen worked in secondary roles to the ambulance service—for example, minor injury units and out‐of‐hours doctor services. Number of years working as a health care professional averaged 19 years (range 10–33 years) while the mean time as an ECP was 1.8 years (range 1–3 years).
There was a significant correlation between all the rating scales: LBDQ and CCQ (r = 0.764, p = 0.01); LBDQ and ETD (r = 0.836, p = 0.01); ETD and CCQ (r = 0.815, p = 0.01). This implies that the better leaders were also better communicators leading dynamic teams.
The average ECP score on the rating scales was high, CCQ 83% (65 points on a scale of 0–78), ETD 79% (22 points on a scale of 0–28), and LBDQ 79% (63 points on a scale of 0–80). However, the ranges are notable: 51–100% on communication skills, 36–100% on team work, and 29–100% on leadership ratings (see appendix 1 for rating scales).
Analysis of level 1 and level 3 ECP performance in relation to leadership, communication and team work revealed that level 3 practitioners performed at a higher mean rating in communication and leadership and the teams that they led were more dynamic. This reached borderline significance in the two leadership sub scales LBDQ (consideration) (t = 1.76, p = 0.05, one‐tailed) and in LBDQ (initiating structure) (z = −1.86, p = 0.032, one‐tailed). Years working as a healthcare professional was also correlated with ECPs ability to structure a team (r = 0.473, p = 0.023).
Results of patient audit
We undertook an audit of patients seen by ECPs over two 3 week periods in February 2006 and April/May 2006 (findings that are likely to have been related to collaborative practice are reported here, other results will be reported at a later date). Twenty‐five ECPs from across the region completed a total of 611 patient audit forms. The return rate varied between practitioners but, considering the random nature of patient calls and their allocation to ECPs, the sample would appear to be reasonably representative of the population. The objective was to identify likely influences and outputs of collaborative practice.
The mean time on scene was 46.5 min, ranging from <1 min to 4.5 h. From the ECP interview data,1 the longer times on scene were often blamed on the failure in referral systems and/or transport delays. There was no significant difference in the on scene time between levels of ECP with time set at < or >30 min (χ2 = 0.413, p = 0.53).
ECPs non‐conveyance rate was 62% (336/539) (95% CI 58% to 66%). Reports from the same period (K Wenman, presentation at the Peninsula Practitioner Conference, Plymouth UK, 11 September 2006) indicate that the total Trust's non‐conveyance rate was 32%. These rates compare well with previously reported rates of 50% for ECPs and 36% for paramedics from the same Trust.12
Between ECP levels (level 1, level 3 and training ECPs) there was a significant difference in patient transport rates (z = −2.05, p = 0.04). Training ECPs conveyed 58% (19/33) (95% CI 41% to 73%) of cases compared to 35% (165/474) (95% CI 31% to 39%) of level 1 ECPs and 38% (19/50) (95% CI 26% to 52%) of level 3 ECPs.
Forty‐eight per cent of patients (285/595) (95% CI 44% to 52%) were seen, treated and discharged by an ECP and 38% of patients were referred. The remaining patients were seen and treated with general practitioners or other professionals. However, between ECP levels (level 1, level 3 and training ECPs) there was a significant difference in patient outcome (χ2 = 41.85, p⩽0.001). Training ECPs treated and released fewer of their patients (36% (12/33) (95% CI 22% to 53%)) than level 1 ECPs (49% (246/506) (95% CI 44% to 53%)) and level 3 ECPs (48% (27/56) (95% CI 35% to 61%)).
ECPs considered outcomes to be unsatisfactory in only 5% (29/582) (95% CI 4% to 7%) of cases—for example, no appropriate patient group directive. ECPs worked with general practitioners, paramedics, technicians, first responders, etc, and claimed to make the referral decision in 87% of cases (136/156) (95% CI 81% to 92%) with a successful referral in 96% of cases (238/249) (95% CI 92% to 98%).
Most patients were referred to accident and emergency (46% (139/302) (95% CI 41% to 52%)), but a significant number of other resources were made use of, including general practitioners (13%), minor injuries units (7%), district nurses (2%), and Falls groups (1%). ECPs were also asked: “Did you perform an ECP‐specific intervention, which avoided Acute Trust admission?” Sixty‐six per cent (396/600) (95% CI 62% to 70%) responded in the affirmative.
Discussion
The rating scales appear to be valid and reliable, demonstrating a consistency >82% (Cronbach's α). Intuitively one would expect there to be a correlation between communication, team work and leadership and from our ratings this was the case; better leaders were better communicators and led higher performing teams. What was notable, however, was the poor leadership and communication ability of some of the ECPs, and consequently the poor performance of their teams.
The findings indicated a borderline trend towards better leadership from the level 3 practitioners implying that the management and leadership programmes attended by this level of ECP may have been beneficial. Length of experience as a healthcare professional was also correlated with ECPs ability to structure a team (LBDQ initiating structure p = 0.023), implying that staff should be experienced before an ECP appointment.
At a time when the Trusts' conveyance rate was 68% the ECPs conveyance rate of 38% (that is, a non‐conveyance rate of 62%) is impressive and suggests a risk taking confidence in care and a collaborative and supportive network. It is also an improvement from previously reported conveyance rates of 50%.12 However, the number of returns to patients are unknown, which would paint a fuller picture of the safety issues. Nevertheless it is likely that many inappropriate admissions were avoided.
ECPs did claim that outcomes were satisfactory in 95% of cases, and that when working with other health professionals they made the referral decision in the majority of cases, implying a good level of collaboration and expertise. The majority of patients were referred to emergency departments but there was a wide range—if infrequent use—of other treatment centres, the implication being that there is a broad collaborative network that could be used more frequently.
The small number of ECPs meant that the study had relatively low power to detect outcome changes. For example, our power estimates suggest that the study was adequately powered to detect differences of 25% between level 1 and level 3 ECPs on the leadership, communication and team work ratings. In addition, as some of our data were collected in observational settings, there may have been a change of behaviour related to “observer effects”, a Hawthorne effect.23 However this was hopefully balanced by the variety of methods and sources of data to produce an accurate consensus overview.1
In conclusion, ECPs collaborative performance varies, but experienced ECPs do appear to have an impact on collaborative practice, as measured by leadership, communication ability, team work, referral decisions and rates and conveyance rates.
In our second report,1 we identify the range of professionals in ECPs network and the influences on collaborative development—for example, cultural effects on working practices; a desire for up‐skilling in applicable work areas (such as minor injury units); and a drive for enhanced teamwork and greater fluency in patient care. However, we also identify reasons for collaborative failures such as level of education, communication and language failings, leadership and team work ability, lack of clinical supervision, and cultural limitations. These results are drawn together in a model of collaboration to match the studies' objectives and to produce a final set of recommendations.1
To view appendices 1 and 2 visit the EMJ website—http://emj.bmj.com/supplemental
Supplementary Material
Acknowledgements
The authors would like to offer their sincere thanks to the ambulance service and all those who participated in the study.
Abbreviations
CCQ - Communication Competence Questionnaire
ETD - Emergency Team Dynamics
ECP - emergency care practitioner
LBDQ - Leadership Behaviour Description Questionnaire
WAST - Westcountry Ambulance Service NHS Trust
Footnotes
Funding: Burdett Trust for Nursing
Competing interests: None
To view appendices 1 and 2 visit the EMJ website—http://emj.bmj.com/supplemental
References
- 1.Cooper S, O'Carroll J, Jenkin A.et al Collaborative practices in unscheduled emergency care: role and impact of the emergency care practitioner—qualitative and summative findings. Emerg Med J 200724625–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Department of Health Life in the fast lane. London: Department of Health, 1997
- 3.Department of Health Reforming emergency care. London: Department of Health Publications, 2000
- 4.Department of Health Improving emergency care. London: Department of Health Publications, 2004
- 5.Department of Health Taking healthcare to the patient: transforming NHS ambulance services. London: Department of Health Publications, 200564
- 6.Joint Royal Colleges Ambulance Liaison Committee The future role and education of paramedic ambulance service personnel (emerging concepts). London: Joint Royal Colleges Ambulance Liaison Committee, 2000
- 7.Leathard A. Models of inter‐professional collaboration. In: Leathard A, ed. Inter‐profesional collaboration from policy to practice in health and social care. Hove: Brunner‐Routledge, 200393–117.
- 8.D'Armour D, Ferrada‐Videla M, Rodrigiez M.et al The conceptual basis for inter‐professional collaboration; core concepts and theoretical frameworks. Journal of Inter‐professional Care 200519(Suppl 1)116–131. [DOI] [PubMed] [Google Scholar]
- 9.Risser D, Rice M, Salisbury M.et al The potential for improved teamwork to reduce medical errors in the emergency department. Ann Emerg Med 199934373–383. [DOI] [PubMed] [Google Scholar]
- 10.Poulton B C, West M A. Effective multidisciplinary teamwork in primary health care. Journal of Advanced Nursing 199318918–925. [DOI] [PubMed] [Google Scholar]
- 11.Ummenhofer W, Amsler F, Sutter P W.et al Team performance in the emergency room: assessment of inter‐disciplinary attitudes. Resuscitation 20014939–46. [DOI] [PubMed] [Google Scholar]
- 12.Cooper S, Barrett B, Black S.et al The emerging role of the emergency care practitioner. Emerg Med J 200421614–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Department of Health The competence and curriculum framework for the emergency care practitioner. A document for discussion. London: Department of Health, 200564
- 14.Department of Health Right skill, right time, right place. The ECP report. London: Modernisation Agency, Department of Health Publications, 2004
- 15.Leathard A.Inter‐professional collaboration; from policy to practice in health and social care. Hove: Brunner‐Routledge, 2003
- 16.Miller C, Freeman M. Clinical teamwork: the impact of policy on collaborative practice. In: Leathard A, ed. Inter‐professional collaboration: from policy to practice in health and social care Hove: Brunner–Routledge, 2003
- 17.Engel C, Gursky E. Management and inter‐professional collaboration. In: Leathard A, ed. Inter‐professional collaboration: from policy to practice in health and social care Hove: Brunner–Routledge, 200344–55.
- 18.Monge P R, Bachman S G, Dillard J P.et al Communicator competence in the workplace: model testing and scale development. In: Burgoon M, rd. Communication Yearbook 5. New Brunswick: NJ Transaction Books, 1981505–527.
- 19.Cooper S, Wakelam A. Leadership of resuscitation teams: ‘lighthouse leadership'. Resuscitation 19994227–45. [DOI] [PubMed] [Google Scholar]
- 20.Stogdill R M.Handbook of leadership: a survey of theory and research. New York: Free Press, 1974
- 21.Cooper S. Developing leaders for advanced life support; an evaluation of a training programme. Resuscitation 20014933–38. [DOI] [PubMed] [Google Scholar]
- 22.SISA Simple Interactive Statistical Analysis, 2006 http;//home.clara.net/sisa/omhlp. htm 25/1/07
- 23.Campbell J, Maxey V, Watson W. Hawthorne effect; implications for pre‐hospital research. Ann Emerg Med 199526590–594. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.