Abstract
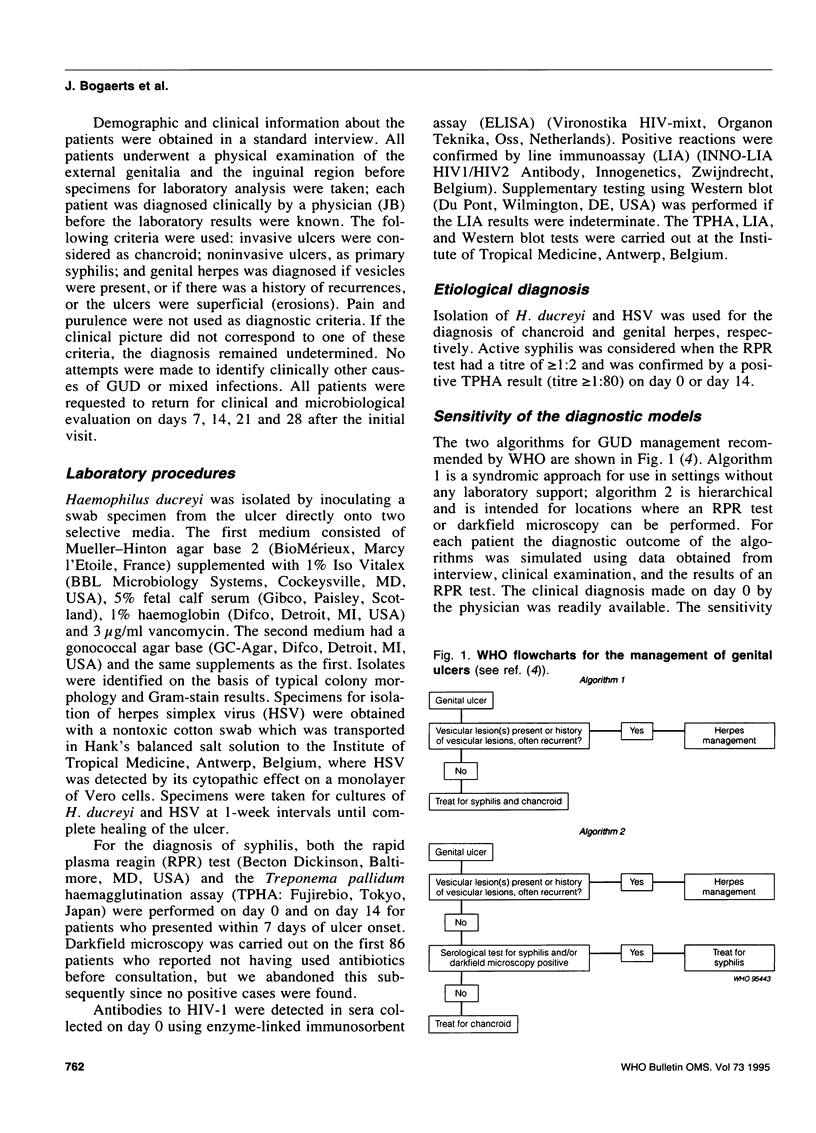
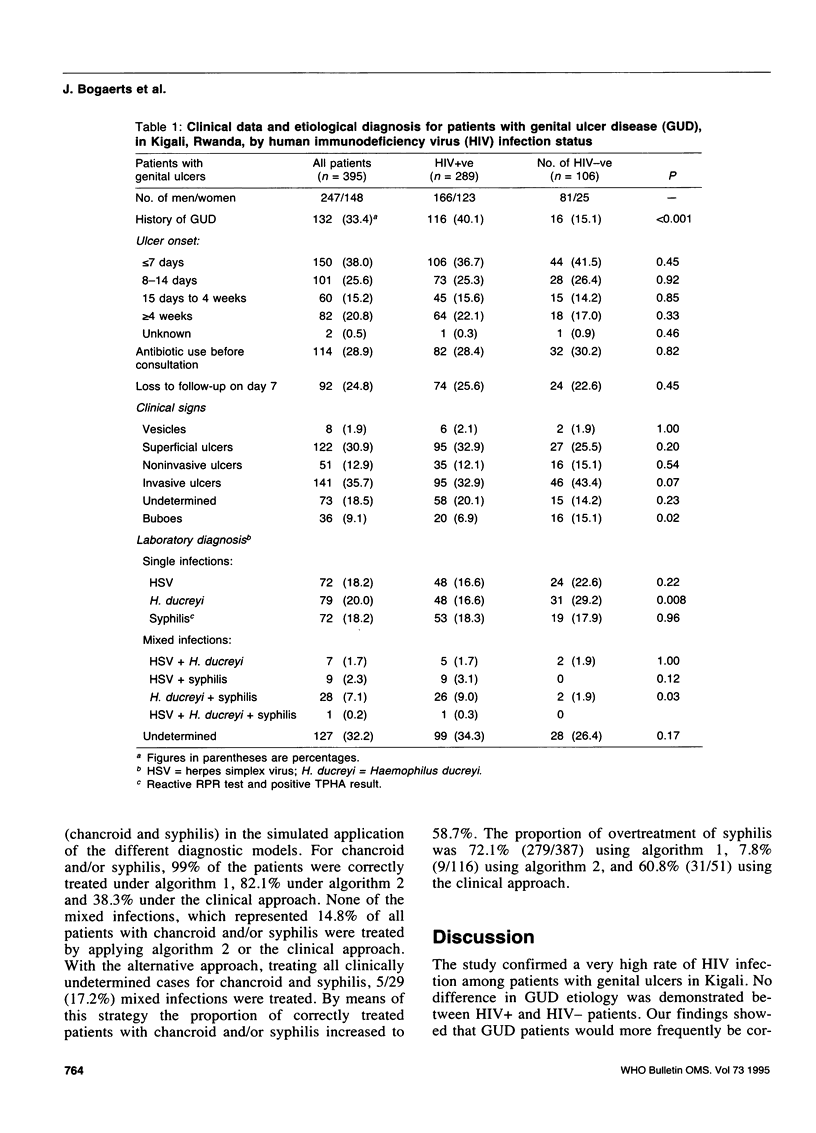
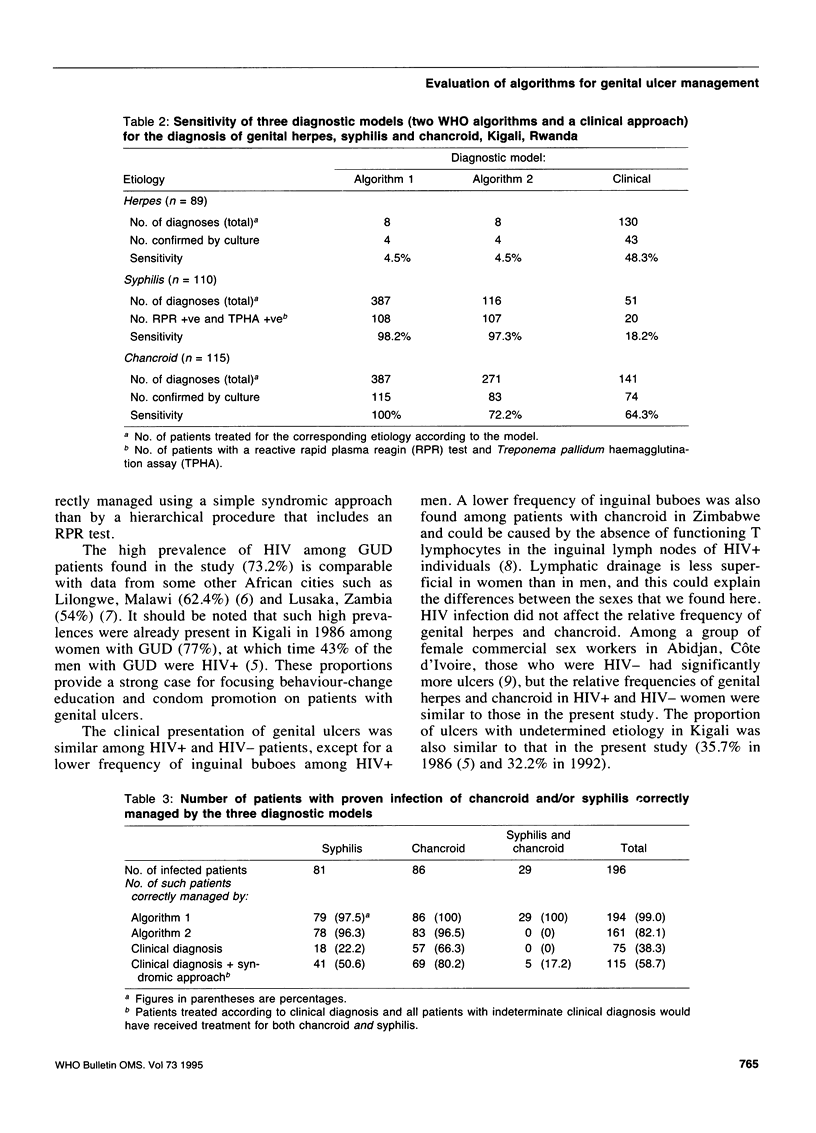
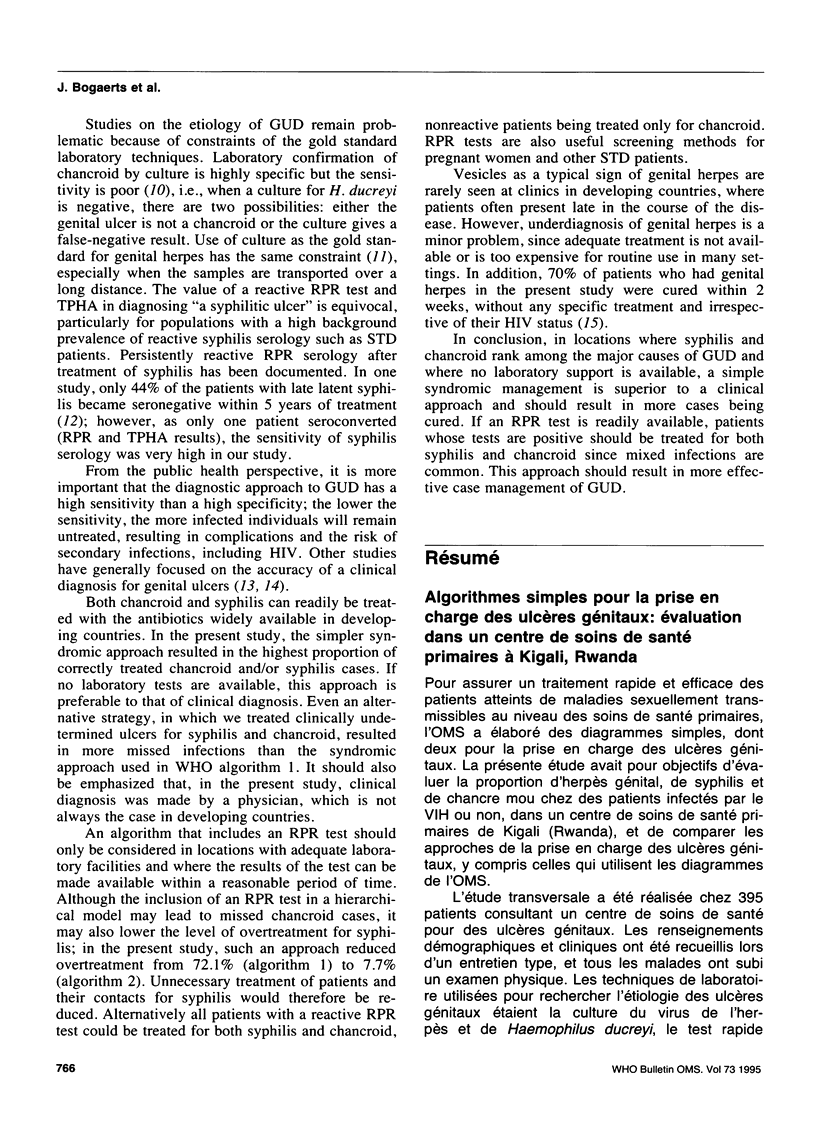
A cross-sectional study was conducted among 395 patients presenting with genital ulcers at a primary health care centre in Kigali, Rwanda. Using clinical data and the results of a rapid plasma reagin (RPR) test, we simulated the diagnostic outcome of two simple WHO flowcharts for the management of genital ulcers. These outcomes and a clinical diagnosis were then compared with the laboratory diagnosis based on culture for genital herpes and Haemophilus ducreyi and serology for syphilis. The prevalence of HIV infection was high (73%) but there was no difference between HIV-positive and HIV-negative patients in the clinical presentation and etiology of genital ulcer disease. The proportion of correctly managed chancroid and/or syphilis cases was 99% using a syndromic approach, 82.1% using a hierarchical algorithm including an RPR test, and 38.3% with a clinical diagnosis. In situations where no laboratory support is available, a simple syndromic approach is preferable to the clinical approach for the management of genital ulcer. If an RPR test can be included in the diagnostic strategy, patients with a reactive RPR test should be treated for both syphilis and chancroid infection.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bogaerts J., Ricart C. A., Van Dyck E., Piot P. The etiology of genital ulceration in Rwanda. Sex Transm Dis. 1989 Jul-Sep;16(3):123–126. doi: 10.1097/00007435-198907000-00001. [DOI] [PubMed] [Google Scholar]
- Chapel T. A., Brown W. J., Jeffres C., Stewart J. A. How reliable is the morphological diagnosis of penile ulcerations? Sex Transm Dis. 1977 Oct-Dec;4(4):150–152. doi: 10.1097/00007435-197710000-00008. [DOI] [PubMed] [Google Scholar]
- Dangor Y., Ballard R. C., da L Exposto F., Fehler G., Miller S. D., Koornhof H. J. Accuracy of clinical diagnosis of genital ulcer disease. Sex Transm Dis. 1990 Oct-Dec;17(4):184–189. doi: 10.1097/00007435-199010000-00007. [DOI] [PubMed] [Google Scholar]
- Fiumara N. J. Serologic responses to treatment of 128 patients with late latent syphilis. Sex Transm Dis. 1979 Oct-Dec;6(4):243–246. doi: 10.1097/00007435-197910000-00003. [DOI] [PubMed] [Google Scholar]
- Koutsky L. A., Stevens C. E., Holmes K. K., Ashley R. L., Kiviat N. B., Critchlow C. W., Corey L. Underdiagnosis of genital herpes by current clinical and viral-isolation procedures. N Engl J Med. 1992 Jun 4;326(23):1533–1539. doi: 10.1056/NEJM199206043262305. [DOI] [PubMed] [Google Scholar]
- Kristensen J. K. The prevalence of symptomatic sexually transmitted diseases and human immunodeficiency virus infection in outpatients in Lilongwe, Malawi. Genitourin Med. 1990 Aug;66(4):244–246. doi: 10.1136/sti.66.4.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latif A. S. Sexually transmitted diseases in Africa. Genitourin Med. 1990 Aug;66(4):235–237. doi: 10.1136/sti.66.4.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Farrell N., Hoosen A. A., Coetzee K. D., van den Ende J. Genital ulcer disease: accuracy of clinical diagnosis and strategies to improve control in Durban, South Africa. Genitourin Med. 1994 Feb;70(1):7–11. doi: 10.1136/sti.70.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Dyck E., Piot P. Laboratory techniques in the investigation of chancroid, lymphogranuloma venereum and donovanosis. Genitourin Med. 1992 Apr;68(2):130–133. doi: 10.1136/sti.68.2.130. [DOI] [PMC free article] [PubMed] [Google Scholar]


