Abstract
Periprosthetic osteolysis remains the leading complication of total hip arthroplasty, often resulting in aseptic loosening of the implant, and a requirement for revision surgery. Wear-generated particular debris is the main cause of initiating this destructive process. The purpose of this article is to review recent advances in our understanding of how wear debris causes osteolysis, and emergent strategies for the avoidance and treatment of this disease. The most important cellular target for wear debris is the macrophage, which responds to particle challenge in two distinct ways, both of which contribute to increased bone resorption. First, it is well known that wear debris activates proinflammatory signaling, which leads to increased osteoclast recruitment and activation. More recently, it has been established that wear also inhibits the protective actions of antiosteoclastogenic cytokines such as interferon gamma, thus promoting differentiation of macrophages to bone-resorbing osteoclasts. Osteoblasts, fibroblasts, and possibly lymphocytes may also be involved in responses to wear. At a molecular level, wear particles activate MAP kinase cascades, NFκB and other transcription factors, and induce expression of suppressors of cytokine signaling. Strategies to reduce osteolysis by choosing bearing surface materials with reduced wear properties (such as metal-on-metal) should be balanced by awareness that reducing particle size may increase biological activity. Finally, although therapeutic agents against proinflammatory mediators [such as tumor necrosis factor (TNF)] and osteoclasts (bisphosphonates and molecules blocking RANKL signaling) have shown promise in animal models, no approved treatments are yet available to osteolysis patients. Considerable efforts are underway to develop such therapies, and to identify novel targets for therapeutic intervention.
Key words: aseptic loosening, periprosthetic osteolysis, wear debris
Introduction
The generation of prosthetic implant wear in total joint arthroplasty patients is widely recognized as the major initiating event in development of periprosthetic osteolysis and aseptic loosening, which is the leading complication of this otherwise remarkably successful surgical procedure [1]. Evidence in support of this includes the observations that osteolysis is correlated with higher wear rates [2] and that vast numbers of wear particles are found associated with the periprosthetic interfacial membrane removed during revision surgery [3–5]. Furthermore, experimental systems have demonstrated that particulate debris can induce osteolysis in a variety of animal models [6–12], and inflammatory responses in cultured macrophages [8, 13–17]. Taken together, and notwithstanding evidence for some involvement of other factors—such as fluid pressure [18] and adherent endotoxin [19], which lie beyond the scope of this review—these findings clearly demonstrate that wear debris represents the single most important underlying cause of periprosthetic osteolysis.
Wear debris can be generated in a variety of ways, and may include particles from all the various components of the prosthesis (such as polyethylene, metal, and ceramic) as well as bone cement [20]. Since, as discussed below, cellular responses are highly dependent upon the composition, size, and shape of particles, the type of prosthesis and bearing surface used may have a significant impact on the potential for development of osteolysis. In this review, we discuss the current state of knowledge regarding how wear debris participates in the development of osteolysis, paying particular attention to the various possible cellular targets of particles and the molecular consequences of these cell–particle interactions. In addition, we identify unanswered questions, and possibly fruitful areas for future research into the molecular pathogenesis of osteolysis that may lead to the identification of candidates for therapeutic intervention.
Cellular targets of wear debris particles
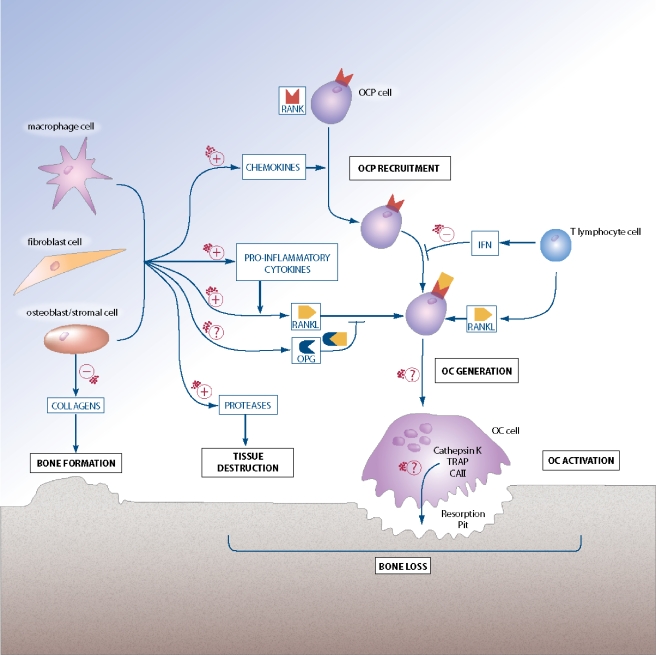
Several different cell types have been implicated in the development of periprosthetic osteolysis in response to wear debris, indicative of a complex network of cellular pathogenesis (see Fig. 1).
Fig. 1.
Cellular and molecular regulation of osteoclastogenesis and the influence of wear debris. Osteoclast precursor cells (OCP) are recruited to the periprosthetic tissues and differentiate into functional osteoclasts (OC), which resorb bone by generation of a resorption pit into which enzymes such as Cathepsin K, tartrate-resistant acid phosphatase (TRAP), and carbonic anhydrase II (CAII) are secreted. Osteoclast maturation and activation is mediated by interaction of RANKL (which can also exist as a cell surface signaling molecule; not shown for clarity) with the OCP receptor RANK. Osteoprotegerin (OPG), a soluble decoy receptor for RANKL, inhibits this pathway, as does the T lymphocyte cytokine, interferon (IFN) gamma. Various other cell types, including macrophages, fibroblasts, and osteoblasts, can modulate this pathway via production of chemokines and proinflammatory cytokines, and can also contribute directly to tissue destruction and/or formation through expression of proteases and collagens. Positive (+) and negative (−) effects of wear particles on key aspects of this complex regulatory system are shown, as are important steps where possible particles involvement has yet to be established (?)
Macrophages and the inflammatory response
There is compelling evidence that the most important cellular target of wear debris is the macrophage. Abundant numbers of macrophages can be identified in the interfacial membrane of patients undergoing revision surgery, and the presence of particles within these cells suggests that they are actively phagocytosing these particles [3]. Phagocytosis of wear particles can be reproduced with cultured macrophage lineage cells and cell lines [13, 14, 21, 22], and this is accompanied by the induction of proinflammatory mediators such as tumor necrosis factor (TNF) alpha, IL-1β, PGE2, and the pleiotropic cytokine IL-6 [8, 13–17]. This suggests that the interfacial membrane macrophages are probably mounting an inflammatory response, and indeed elevated levels of proinflammatory cytokines have been reported in periprosthetic tissues and joint synovial fluid of osteolysis patients [23–26]. However, there is no clear evidence in favor of elevated levels of proinflammatory markers in serum of patients [27–29]. Expression and secretion of matrix metalloproteinases is also elevated in macrophages exposed to wear debris in vitro [30], and elevated levels of these and other proteases have been detected in periprosthetic tissues from osteolysis patients [31, 32], suggesting that elevated extracellular matrix levels of proteases could contribute to tissue destruction in osteolysis patients. Although a variety of different types of wear debris have been shown to induce proinflammatory responses, the specific nature of this response is dependent upon numerous parameters, including composition [33, 34], size [21, 35], shape [36], and volume [37]. In addition, responses to wear particles can be modulated by the presence of adherent endotoxin [19, 38, 39], and also by a variety of physical insults such as application of pressure [40, 41] and stretching [42]. This complexity is further compounded by observations that cells from different donors can respond very differently to particles [21, 33]. Taken together, the extensive body of research on in vitro cellular responses to wear debris suggests that while an inflammatory response by macrophages is central to the development of periprosthetic osteolysis, the detailed nature of this response will vary based upon several parameters, including prosthetic type, patterns of wear, and host factors.
Animal models of osteolysis support a role for an inflammatory response to a variety of types of particulate wear debris. For example, implantation of particulate debris into rabbit tibia induces a foreign body giant cell reaction [43], and tissue surrounding loose rabbit tibial prostheses generates elevated levels of PGE2 compared to the tissue around well-fixated prostheses [44]. Likewise, periprosthetic cells from a canine osteolysis model produce elevated levels of proinflammatory mediators, including PGE2 and IL-1 [45]. Rat models of osteolysis using particulate matter introduced into an air pouch [46, 47] or together with a tibial polyethylene implant [7] have similarly resulted in inflammatory reactions. These early canine, rabbit, and rat in vivo models have, by and large, confirmed the results of in vitro cell culture studies, demonstrating that various particle compositions can induce an inflammatory response (and osteolysis).
More recently, three murine models of wear debris-induced osteolysis have been developed, allowing the power of murine knockout and transgenic technologies to be applied to the study of osteolysis in vivo. In the first of these three murine models, implantation of metal, polyethylene, and PMMA bone cement particulate debris into subcutaneously generated air pouches all induce macrophage infiltration and production of proinflammatory cytokines [10]. Gene therapy with the anti-inflammatory cytokines IL-1Ra or viral IL-10 protects mice from the inflammatory response to particles [48] and, importantly, also ameliorates wear debris-induced osteolysis of bone fragments introduced into the air pouch [12], suggesting that the inflammatory response to particles contributes to the eventual bone loss characteristic of osteolysis. The second mouse model to gain prominence involves direct application of particulate matter to the exposed calvarium [6, 8]. This calvarial model was extensively used to study the involvement of the key proinflammatory cytokine, TNF-alpha, in particle-induced inflammation and osteolysis. Interestingly, inhibiting TNF alpha action by deletion of the genes encoding TNF receptors [8, 49], or by treatment with Etanercept, a TNF antagonist consisting of the extracellular region of human p75 TNF-alpha receptor fused to the Fc portion of human IgG1 [50], diminishes particle-induced inflammation and osteolysis, providing more evidence for inflammation/TNF-alpha production as essential precursors of bone erosion in osteolysis. The calvarial model was also used to show that the anti-inflammatory cytokine viral IL10 can suppress wear debris-induced osteolysis [51], and to identify a role for COX2 in osteolysis. COX2-deficient mice were significantly protected from calvarial osteolysis induced by titanium particles, whereas Celecoxib, a selective COX2 inhibitor, inhibited PGE2 production, inflammation, and osteolysis in response to particles in wild-type mice [52]. No involvement of COX1 was identified.
The calvarial and air-pouch murine models have proved extremely valuable in the search for key molecules implicated in osteolysis. However, they suffer from a number of features that distinguish them from the analogous situation experienced by osteolysis patients, the most significant being the absence of a loaded implant, and the use of implanted bone slices (air-pouch model) or flat bones (calvarial model) as opposed to long bones with the periosteum removed. In response to these concerns about the appropriateness of these models for some aspects of the human disease, work in the Goodman laboratory [11, 53] and in our own laboratory, has begun on the development of a third class of mouse osteolysis model, in which load-bearing implant are introduced to the long bones, and the effects of particles around the prosthesis are studied. Early results from these models are promising and have confirmed that particles around the implants induce a proinflammatory response in the periprosthetic tissue [11], and that the proinflammatory cytokine IL-1 [53] and the pleiotropic cytokine IL6 (our unpublished data) are involved in this response.
Osteoclast lineage cells
The final cellular consequence of particle action is an excess of osteoclast activity, which results in unchecked bone erosion. How do particles cause this? Osteoclasts (OCs), the only cell type capable of bone resorption, are derived from circulating hematopoietic cells of the monocyte/macrophage lineage. We shall thus consider two ways in which particles might increase OC activity: generation of functional OCs from osteoclast precursor cells (OCPs) within the periprosthetic space and recruitment of OCPs from the blood.
OC generation and activation
As mentioned above, inhibition of the inflammatory response to wear debris alleviates osteolysis in mouse models, suggesting that one important bone loss pathway is secondary to the inflammatory response. This is consistent with known bone proresorptive actions of cytokines such as TNF alpha and IL1, which act—at least in part—directly on osteoclast precursors (OCPs). In addition to their direct actions on osteoclasts and their precursors, proinflammatory cytokines may indirectly promote OC activity, through induction of expression of receptor activator of NFκB ligand (RANKL), the key cytokine regulator of osteoclast generation and activation. RANKL binds to receptor activator of NFκB (RANK) expressed on the surface of OCs and OCPs [54], and is necessary and sufficient for the differentiation of OCPs to mature, functional OCs in the presence of the survival factor MCSF [55, 56]. Osteoprotegerin (OPG), a naturally occurring decoy receptor for RANKL functions to down-regulate osteoclastogenesis by binding RANKL and thus preventing its interaction with RANK [57]. Thus, the RANKL/OPG ratio has emerged as a critical parameter in the regulation of bone resorption, and has been correlated with a variety of bone disorders [58]. Although RANKL/OPG ratios have yet to be correlated with osteolysis, there are compelling reasons to suspect that bone loss in these individuals is mediated by elevated RANKL/OPG. First, RANKL blockade with OPG [59, 60] or RANK:Fc (a RANKL antagonist consisting of the extracellular region of RANK fused to the Fc portion of human IgG1) [61], or by using mice genetically deficient in RANK [61] prevents wear debris-induced osteolysis in the murine calvarial model. Second, wear debris can increase the RANKL/OPG ratio in murine calvarial tissues [62]. Third, several reports have identified elevated RANKL expression in the interfacial membranes from osteolysis patients [63–66]. Our own data also indicate that very low levels of OPG in osteolysis patients may underlie dramatic increases in periprosthetic RANKL/OPG ratios (Koulouvaris and Purdue, unpublished observations). The cellular basis for elevated RANKL expression is complicated by the fact that several different cell types within the periprosthetic tissue are capable of RANKL expression, including osteoblasts, fibroblasts, and T lymphocytes, each of which are considered in the following sections. Remarkably, macrophages and giant cells in the interfacial membranes of osteolysis patients have also been reported to express RANKL [63–66], despite the fact that macrophage lineage cells are generally thought not to express RANKL under normal conditions. The molecular basis of increased RANKL in osteolysis is likely downstream of proinflammatory cytokines such as TNF alpha and IL1, which are known to increase RANKL expression in several cell types [58].
Taken together, these observations indicate that one likely mechanism whereby particulate debris may induce osteoclast generation and activation is an indirect one, mediated through the actions of proinflammatory mediators that can act on osteoclast precursors and, most importantly, modulate the RANKL/OPG ratio through actions on cells within the periprosthetic tissue. But is this the only way in which wear debris may act upon OCPs? Recent studies in our laboratory question whether, in addition to stimulating inflammatory RANKL expression within periprosthetic tissues, wear debris might also act directly upon OCPs, to modulate signaling pathways and responses to cytokines within these cells, and hence impact their differentiation and/or activation [68].
For example, several cytokines have demonstrated antiosteoclastogenic activities, which inhibit the differentiation of OCPs to fully fledged, active osteoclasts. Perhaps the best characterized of these is interferon gamma, which potently down-regulates RANKL-induced osteoclastogenesis [67]. We have shown that antiosteoclastogenic interferon gamma signaling in OCPs (as characterized by activation of the STAT1 signaling molecule) is potently inhibited by titanium wear debris [68]. Similar findings show that signaling by IL6, which can also suppress differentiation of OCPs, is also suppressed by titanium and by PMMA bone cement (which has no effect on interferon gamma signaling) [68]. Thus, wear debris may simultaneously act in two ways to promote bone loss: activation of proinflammatory signaling in macrophages, and inhibition of the protective effects of antiosteoclastogenic cytokines in OCPs.
Osteoclast precursor recruitment
Excess osteoclast activity in osteolysis may involve not just generation and activation of OCs in the periprosthetic vicinity, but also recruitment of increased numbers of OCPs to these sites. The existence of increased levels of OCPs in the pseudomembrane of osteolysis patients is implied by the observation that macrophage lineage cells isolated from these tissues display a greatly increased propensity to differentiate to OCs (relative to analogous cell populations from osteoarthritis patients) [69]. The principal mediators of hematopoietic cell recruitment to tissues are chemokines, a large family of chemotactic cytokines, which interact with specific chemokine receptors expressed upon the cell surface of target cells. Expression of the chemokines including MCP-1 and MIP-1-alpha in cultured macrophages is increased by exposure to wear particles [70], and these same proteins are expressed in the periprosthetic tissues of osteolysis patients [70, 71]. MIP-1-alpha is of particular interest here, because it is reported to increase OC motility, and its receptor, CCR1, is expressed in OCs and their precursors [72]. Another chemokine, IL8, has also been implicated in aseptic loosening [73–75].
Bone formation cells
While most effort has been concentrated on understanding excessive bone resorption in osteolysis patients, less attention has been paid to the possible involvement of defective bone formation. Under normal conditions, resorption and formation balance each other to allow bone remodeling and homeostasis. It is therefore important to consider whether, in addition to promoting osteoclast activity, wear debris might also contribute to osteolysis by inhibiting bone formation. Wear debris particles have been shown to decrease expression of collagen types I and III by osteoblasts (OBs), the cell type responsible for bone formation [76–78]. In addition, titanium has been reported to reduce OB viability by inducing apoptosis [79], and PMMA bone cement reduces OB proliferation [80]. There is also evidence that differentiation of OBs from mesenchymal stem cells is down-regulated by titanium particles [81], and that titanium and zirconium oxide induce mesenchymal stem cell apoptosis [82], suggesting that wear debris might inhibit both OB formation and function.
In addition to modulating bone formation by OBs, particles may also disrupt the contribution of OBs to OC generation and/or recruitment. For instance, expression of RANKL and MCSF by cultured OBs can be induced by low concentrations of wear debris [83], as can expression of proinflammatory mediators such as TNF-alpha, IL6 and PGE2 [76, 80], which—as discussed above—can subsequently lead to osteoclast activation. In addition, OBs can produce chemokines involved in OCP recruitment, such as MIP-1-alpha, and this is elevated by proinflammatory cytokines such as TNF-alpha and IL-1-alpha [72].
Fibroblasts
Fibroblasts are abundant within the interfacial membrane of osteolysis patients, and express RANKL [66, 84]. Expression of RANKL by fibroblasts can be up-regulated by incubation with titanium particles or by the inflammatory mediator PGE2, and these stimulated cells can support differentiation of OCPs to OCs in the presence of MCSF [85]. Likewise, fibroblasts isolated from arthroplasty membranes of osteolysis patients (which had presumably been exposed to wear debris in vivo) were able to support generation of OCs from human monocytes [86]. These observations suggest that periprosthetic fibroblasts exposed to wear and/or proinflammatory mediators may be a major source of the RANKL required to drive osteoclastogenesis in osteolysis patients. Particles can also induce production in cultured fibroblasts of proinflammatory mediators, collagenase and stromelysin [87, 88], which could contribute to the development of osteolysis, and chemokines, which could contribute to the recruitment of increased numbers of OCPs to periprosthetic tissues [89].
Lymphocytes
Involvement of lymphocytes in osteolysis is an attractive hypothesis, but remains controversial. T lymphocytes are emerging as key regulators of bone homeostasis because of their ability to generate both proosteoclastogenic (i.e., RANKL) and antiosteoclastogenic (i.e., interferon gamma) cytokines upon activation, and are critically involved in the RANKL-dependent bone loss observed in inflammatory bone erosion diseases such as rheumatoid arthritis [90–92]. However, although some studies of the cellularity of periprosthetic tissues retrieved from osteolysis patients during revision surgery suggest the presence of significant numbers of activated T cells [93, 94], others discount this possibility, finding only unactivated T cells present in significant [95] or low [96] amounts. At a molecular level, some studies report the presence of Th1 and Th2 cytokines in the periprosthetic tissues [94], while other researchers find none [95, 96]. In animal studies, mice with deficiencies in lymphocytes retain the ability to form granulomas [97, 98] and develop osteolysis [99] in response to wear debris, suggesting that lymphocytes are not causally involved in these processes. On the other hand, mice with deficiencies in lymphocytes fail to mount an inflammatory response to polyethylene particles injected into the knee [100], and titanium particles induce larger sutures in athymic mice than wild-type controls when applied to exposed calvaria [101]. Perhaps the strongest evidence for the involvement of lymphocytes in aseptic loosening are two recent reports correlating a metal-specific lymphocyte response to poor implant performance [102] and characterizing lymphocytic infiltration around metal-on-metal arthroplasties [103]. More research will be necessary to determine whether lymphocytes are substantially involved in osteolysis or not.
Molecular targets of wear debris
As discussed above, a good deal is known about the eventual modulation of expression of numerous proteins, including cytokines, chemokines, and proteases, by wear debris. In contrast, considerably less is understood about the molecular events upstream of the transcription of the genes encoding these proteins initiated by particles.
Macrophage cell surface receptors
Remarkably little is known about the molecular basis of wear debris interaction with the surfaces of cells. Even for macrophages, the best-characterized cellular target for particle action, the identity of the cell surface receptors responsible for recognition of the particles, and the full repertoire of signaling cascades initiated or modified by particle binding, remain poorly understood. One important consideration in determining the involvement of specific macrophage surface receptors is the extent to which different particles become opsonized with host serum proteins prior to phagocytosis. There is evidence that polyethylene activates complement [104], and this would argue in favor of a role for complement receptors, such as CR3, in particle uptake. Indeed, CR3 expressing phagocytes have been detected in granulomatous lesions associated with hip replacement [105]. By contrast, research on alveolar macrophage response to environmental particulate matter has implicated scavenger receptors, such as MARCO, in opsonin-independent uptake of titanium particles [106], suggesting that different particles may use different surface receptors. This would provide an intriguing explanation of the abilities of different types of wear debris to elicit particle type-specific responses in cultured macrophages. Consistent with this, opsonization was shown to be not essential (although it may be involved) in responses of human monocytes and macrophage cell lines to titanium [107, 108]. The concept that opsonization may differentially regulate uptake of different compositions of wear debris is also supported by observations that the spectra of adherent human serum proteins demonstrates a level of particle specificity [109]. To further explore this important line of inquiry, our laboratory has developed a flow cytometry assay to monitor particle uptake by macrophages, and confirmed that scavenger receptor inhibition specifically reduces titanium particle phagocytosis. Interestingly, PMMA bone cement uptake was inhibited by blocking the CR3 complement receptor, but not affected by scavenger receptor inhibition (Rakshit et al., unpublished data). An involvement of CR3 in particle action is also supported by observations that antibodies against CR3 reduces particle uptake [14], and that activation of this receptor mimics several aspects of downstream signaling by particles (discussed in more detail below), in that MAP kinases [110] and the transcription factors NFκB, NF-IL6, and AP-1 are activated [14, 111], and production of proinflammatory cytokines [14] and chemokines [111] are elevated.
Intracellular signaling molecules
MAP kinases
Data from our laboratory and others have shown that wear debris of various compositions can induce rapid activation of MAP kinase family members [14, 68, 112]. For instance, PMMA bone cement and titanium can each, within 15–30 min, induce activation by phosphorylation of all three of the major MAP kinase subgroups, namely, p38, ERK, and JNK [68]. These three pathways are involved in numerous cellular activities, and all three are required for osteoclast generation and activation [113]. Inhibition of MAP kinase activation reduces the ability of wear debris to induce proinflammatory cytokine induction in cultured OCPs [68], suggesting that MAP kinases are critical transducers of the signals emanating from particle–cell interaction to the nucleus. There appears to be considerable redundancy among the different MAP kinase families in this respect, because inhibition of multiple MAP kinase subgroups is far more effective in down-regulating particle action than inhibition of any single subgroup alone. Our laboratory has recently reported a second, distinct role for MAP kinases in wear particle action, relating to the ability of PMMA and titanium to inhibit antiosteoclastogenic IL-6 signaling. Use of inhibitors for specific MAP kinases has revealed that p38 MAP kinase (but neither ERK nor JNK MAP kinases) activity is essential for wear-mediated down-regulation of IL-6 signaling [68]. CR3 engagement also stimulates MAP kinase activation, consistent with a role for this receptor in wear debris recognition [14, 110].
Transcription factors
Perhaps the most notable transcription factor implicated in wear debris action is NFκB. This protein complex, long known as a key regulator of inflammatory gene expression, is also emerging as an important player during osteoclastogenesis. Mice lacking NFκB, in addition to having defective macrophages, are also osteopetrotic, resulting from an inability to generate functional osteoclasts [114, 115]. Wear debris can activate NFκB in cultured macrophages [14], OCPs [116], and the J774 murine macrophage cell line [49]. Supporting evidence for a role of NFκB in osteolysis comes from observations that deficiency of NFκB1 in mice protects against titanium-induced calvarial osteolysis [49], and that inhibition of NFκB blocks wear debris induction of osteoclastogenesis in vitro [116, 117]. Other transcription factors, such as NF-IL6 [14] and AP-1 [118], have also been shown to become activated following wear debris treatment of macrophages. However, the relevance of these factors in osteolysis remains unclear.
Suppressors of cytokine signaling (SOCS) proteins
As discussed above, we have demonstrated that wear debris can inhibit signaling by antiosteoclastogenic cytokines, such as interferon gamma and IL-6. These cytokines signal via the JAK-Stat pathway, with interferon gamma principally activating Stat1, and IL6 chiefly activating Stat3 [119]. How might the wear particles down-regulate JAK-Stat signaling? At least two mechanisms for inhibition of JAK-Stat signaling are known: MAP kinase activation [120, 121] and induction of a family of proteins known as suppressors of cytokine signaling (SOCS) [122]. Specifically, SOCS1 inhibits interferon gamma activation of Stat1 and SOCS3 inhibits IL-6 activation of STAT3. As noted above, p38 MAP kinase mediates inhibition of IL-6 signaling. However, this does not appear to be the only mechanism whereby wear debris inhibits IL6, since results from our laboratory also show that PMMA and titanium strongly induce expression of SOCS3 [68]. Thus particles trigger multiple pathways (MAP kinase activation and SOCS3 induction) that collaborate to effectively shut down IL-6 signaling.
Current options for implant design
Biologic response to wear particles, corrosion products, or both has been shown to be the primary source of morbidity and early implant failure. Wear rates in excess of 0.2 mm/year have been reported to cause 100% failure of total hip replacement. In the same study, wear rates greater than 0.15 mm/year were shown to put the hip at risk for aseptic loosening [123]. In well functioning THR, wear rate has been measured to be 0.05 mm/year [124]. One of the biggest challenges in implant design research today is to develop better wear-resistant materials to reduce the generation of particles. Bearing surface choices include a metal (cobalt–chrome, CrCo) head and polyethylene (PE) socket, ceramic-on-polyethylene, ceramic-on-ceramic, and metal-on-metal.
(a) Metal (CrCo) head-on-polyethylene has been in use for 30 years. Although the conventional polyethylene (PE) has shown excellent energy absorption, good wettability, and low coefficient of friction, it has been associated with higher wear characteristics (0.075–0.4 mm/year [123]). Highly cross-linked PE has been introduced in total joint replacement to reduce the wear debris. Hip simulator studies have shown that highly cross-linked PE had better wear resistance, higher resistance to delamination, and less wear against rough femoral balls than conventional PE [125]. Moreover, cross-linking has been correlated with superior wear behavior in vitro with large femoral heads [126]. Clinical studies have shown short term results with superior wear resistance [127–129]. The need for longer follow-up has been recognized. Due to lack of long-term follow-up data of in vivo use of cross-linked PE, some authors have reported the continued use of standard PE sterilized with gamma radiation in an air environment with a shelf life of less than 3 years [130].
(b) Ceramics (aluminum or zirconium oxide) have a long history as implant articulating surfaces [131]. The incidence of high fracture rates has been reduced with the third generation of ceramics [132]. Wear rates for ceramic-on-polyethylene bearings ranged from 0 to 150 μm/year and 10% to 50% less wear than with a standard metal femoral head [133]. Moreover, in hip simulator testing, alumina-on-alumina produced wear rates of 1 μm/year compared with 200 μm/year for a standard cobalt chromium-on-polyethylene [132]. However, in a multicenter, prospective, and randomized study an alumina-on-alumina bearing had no significant difference in clinical performance with a CrCo-on-polyethylene bearing [132]. Another alternative with ceramics is oxinium, an oxidized zirconium metal, which showed lower wear rates and more resistance to scratching when articulated with cross-linked polyethylene [134]. Although ceramics have demonstrated very good results in both clinical and laboratory experiments, there are some concerns that need to be addressed. Microseparation, a unique pattern of stripe wear during gait, has been described in zirconium femoral heads [131]. The incidence of fracture, although low, continues to be an issue. Revision can be very challenging because of the inability to use a ceramic head for the second time and the loss of head and liner options intraoperatively. Moreover, fracture of the ceramic head produces particles that are retained and may compromise the results of revision. Another issue is chipping of liner that may occur with component impingement. Ceramic liner chipping may also occur during insertion, when the liner is locked in a nonconcentric manner and introduces wear debris from a second modular interface [131]. Finally, another concern is the cost of ceramics, which is 20% higher than metal-on-polyethylene [130].
(c) Metal-on-metal THR has the longest clinical history of any of the currently used articular couples. Retrieval analysis of metal-on-metal THR demonstrated wear between 1 and 5 μm/year in comparison with 100–200 μm/year associated with metal–polyethylene wear [135, 136]. Although the metal particles are smaller in size, the numbers are much higher. However, the immune response is mild and no multinucleated giant cells have been found in retrieved metal-on-metal bearings [135], although lymphocytic reactions have been observed [103]. There continues to be an issue concerning elevated serum metal ions that have been documented in several reports [135]. Despite the variabilities in techniques of measuring the metal ions, no evidence of necrosis or pathologic abnormalities has been reported [136]. Another concern is the possibility of carcinogenesis due to the metal ions. This has been reported in animal studies; however, in human studies this was not statistically greater than the conventional metal-on-polyethylene [135]. Currently, there are limited data to show a causal link between the elevated ions and the development of carcinogenesis. The short-term clinical results of metal-on-metal THR are equal or better than those of conventional articular couples. Additional advantages of metal-on-metal are the ability to use larger-diameter femoral heads for enhanced stability and the absence of possible fracture of the articular components.
Therapeutic possibilities, now and in the future
Identification of osteolysis as an inflammatory bone erosion disease has culminated in the consideration of two main approaches to treatment: anti-inflammatory agents and suppressors of bone resorption. Anti-inflammatory agents, such as cox-2 inhibitors and TNF antagonists, have yielded encouraging results in animal models of osteolysis. For instance, Etanercept [50] and pentoxifylline [6], TNF antagonists that operate as a decoy receptor and an inhibitor of secretion, respectively, have been independently shown to diminish particle-induced osteolysis in the murine calvarial model, along with COX2 inhibitor Celecoxib [52]. However, despite these encouraging animal studies, it is not yet known how well these anti-inflammatory agents may perform in the prevention or treatment of human osteolysis. Orally administered pentoxifylline reduces the inflammatory response of isolated monocytes to wear debris in healthy subjects [137], but has not been tested in osteolysis patients, and a small trial of Etanercept [138] in osteolysis patients proved inconclusive.
Given that excessive osteoclast activity represents the cellular endpoint of osteolysis, it is not surprising that the bisphosphonate class of osteoclast inhibitors have come in for much discussion as possible therapeutic agents for this disease. Again, however, despite promising results in animal models, there is no clinical evidence supporting the effectiveness of these drugs in the treatment of osteolysis patients. Alendronate inhibits wear debris-induced osteolysis in the rat loaded tibial implant model of osteolysis [7] and in a similar canine model [9], and is also effective in preventing osteolysis in the murine calvarial model [6]. A single dose of zoledronic acid administered directly after surgery also suppressed particle-induced osteolysis in mouse calvaria [139]. Bisphosphonates inhibit OC formation by blocking the mevalonate pathway of isoprenoid biosynthesis. Because statins, as HMGCoA reductase inhibitors, also target the mevalonate pathway, they have been considered as possible drugs for osteolysis. Indeed, simvastatin has been shown to prevent wear debris-induced osteolysis in the murine calvarial model [140]. The central role of RANKL in osteoclastogenesis makes this cytokine an attractive target for possible therapies. OPG (a naturally occurring RANKL antagonist) and RANK-Fc, which reduce RANKL levels, have been successfully used to prevent osteolysis in animal models [59–61]. It remains to be seen whether these approaches will be effective in the treatment of osteolysis patients. Clinical trials with a monoclonal antibody against RANKL (AMG-162) have demonstrated safety and antiresorptive activity [141, 142], but this new agent has yet to be assessed in osteolysis patients. Such treatments would be expected to decrease bone loss, but not reduce inflammation (as seen in OPG treatment of rat adjuvant arthritis [92]), which may be a concern, as elevated TNF and IL1 levels are capable of promoting osteoclastogenesis in the presence of only very low levels of RANKL, suggesting that without reducing inflammation, blockade of RANKL would have to be essentially complete to be effective. An alternative approach would be combined therapy with antagonists against both RANKL and proinflammatory mediators. Such an approach proved successful in an arthritis model [143]. Because RANK signaling is transduced via NFκB, antagonists against this transcription factor may represent effective treatments for osteolysis. In this regard, it is intriguing to note that direct inhibition of NFκB with the NEMO-binding domain (NBD) peptide is reported to prevent bone loss in inflammatory bone erosion patients [144]. However, since persistent inhibition of NFκB could result in immune deficiency or cell death, such treatments should be approached with caution.
Inhibitors of mature OC function represent another possible class of therapeutic agents yet to be evaluated in osteolysis patients. As more become known of the molecular details of osteoclast biology and particle action, it is hoped that additional targets for drug design will become available. For instance, inhibitors of cathepsin K (an OC-specific protease) [145, 146], the osteoclast ATPase proton pump [147], vitronectin receptor [148], and src tyrosine kinase [149], all of which are required for resorption, have been developed.
Perhaps the biggest impediment to the development of therapeutic strategies for osteolysis is the lack of an accepted outcome measure. In response to this, we are developing modified magnetic resonance imaging approaches toward the evaluation of periprosthetic osteolysis [150]; three-dimensional computed tomography is also being applied to this problem [151, 152].
Conclusion
Much progress has recently been made in understanding how, at the molecular and cellular levels, prosthetic wear debris can ultimately cause osteolysis and aseptic loosening. The established scenario of particle-induced proinflammatory signaling has been embellished with an understanding of how wear can also promote maturation of osteoclasts from macrophages, by inhibiting protective, antiosteoclastogenic cytokines such as interferon gamma. We are starting to unravel the complexities of interactions between wear particles and macrophage cell surface receptors, and to describe the intracellular signaling pathways activated by such interactions. Such progress emphasizes the reality that development of therapeutic approaches to the treatment of osteolysis is long overdue.
References
- 1.Harris WH (2001) Wear and periprosthetic osteolysis: the problem. Clin Orthop Relat Res 66–70 [DOI] [PubMed]
- 2.Dumbleton JH, Manley MT, Edidin AA (2002) A literature review of the association between wear rate and osteolysis in total hip arthroplasty. J Arthroplasty 17:649–661 [DOI] [PubMed]
- 3.Schmalzried TP, Jasty M, Harris WH (1992) Periprosthetic bone loss in total hip arthroplasty. Polyethylene wear debris and the concept of the effective joint space. J Bone Jt Surg Am 74:849–863 [PubMed]
- 4.Hirakawa K, Bauer TW, Stulberg BN et al. (1996) Comparison and quantitation of wear debris of failed total hip and total knee arthroplasty. J Biomed Mater Res 31:257–263 [DOI] [PubMed]
- 5.Margevicius KJ, Bauer TW, McMahon JT et al. (1994) Isolation and characterization of debris in membranes around total joint prostheses. J Bone Jt Surg Am 76:1664–1675 [DOI] [PubMed]
- 6.Schwarz EM, Benz EB, Lu AP et al. (2000) Quantitative small-animal surrogate to evaluate drug efficacy in preventing wear debris-induced osteolysis. J Orthop Res 18:849–855 [DOI] [PubMed]
- 7.Millett PJ, Allen MJ, Bostrom MP (2002) Effects of alendronate on particle-induced osteolysis in a rat model. J Bone Jt Surg Am 84-A:236–249 [DOI] [PubMed]
- 8.Merkel KD, Erdmann JM, McHugh KP et al. (1999) Tumor necrosis factor-alpha mediates orthopedic implant osteolysis. Am J Pathol 154:203–210 [DOI] [PMC free article] [PubMed]
- 9.Shanbhag AS, Hasselman CT, Rubash HE (1997) The John Charnley Award. Inhibition of wear debris mediated osteolysis in a canine total hip arthroplasty model. Clin Orthop Relat Res:33–43 [PubMed]
- 10.Wooley PH, Morren R, Andary J et al. (2002) Inflammatory responses to orthopaedic biomaterials in the murine air pouch. Biomaterials 23:517–526 [DOI] [PubMed]
- 11.Warme BA, Epstein NJ, Trindade MC et al. (2004) Proinflammatory mediator expression in a novel murine model of titanium-particle-induced intramedullary inflammation. J Biomed Mater Res B Appl Biomater 71:360–366 [DOI] [PubMed]
- 12.Yang SY, Wu B, Mayton L et al. (2004) Protective effects of IL-1Ra or vIL-10 gene transfer on a murine model of wear debris-induced osteolysis. Gene Ther 11:483–491 [DOI] [PubMed]
- 13.Blaine TA, Rosier RN, Puzas JE et al. (1996) Increased levels of tumor necrosis factor-alpha and interleukin-6 protein and messenger RNA in human peripheral blood monocytes due to titanium particles. J Bone Jt Surg Am 78:1181–1192 [DOI] [PubMed]
- 14.Nakashima Y, Sun DH, Trindade MC et al. (1999) Signaling pathways for tumor necrosis factor-alpha and interleukin-6 expression in human macrophages exposed to titanium–alloy particulate debris in vitro. J Bone Jt Surg Am 81:603–615 [DOI] [PubMed]
- 15.Wimhurst JA, Brooks RA, Rushton N (2001) Inflammatory responses of human primary macrophages to particulate bone cements in vitro. J Bone Jt Surg Br 83:278–282 [DOI] [PubMed]
- 16.Ingham E, Green TR, Stone MH et al. (2000) Production of TNF-alpha and bone resorbing activity by macrophages in response to different types of bone cement particles. Biomaterials 21:1005–1013 [DOI] [PubMed]
- 17.Maloney WJ, James RE, Smith RL (1996) Human macrophage response to retrieved titanium alloy particles in vitro. Clin Orthop Relat Res :268–278 [PubMed]
- 18.Skripitz R, Aspenberg P (2000) Pressure-induced periprosthetic osteolysis: a rat model. J Orthop Res 18:481–484 [DOI] [PubMed]
- 19.Greenfield EM, Bi Y, Ragab AA et al. (2005) Does endotoxin contribute to aseptic loosening of orthopedic implants? J Biomed Mater Res B Appl Biomater 72:179–185 [DOI] [PubMed]
- 20.Saleh KJ, Thongtrangan I, Schwarz EM (2004) Osteolysis: medical and surgical approaches. Clin Orthop Relat Res:138–147 [PubMed]
- 21.Yagil-Kelmer E, Kazmier P, Rahaman MN et al. (2004) Comparison of the response of primary human blood monocytes and the U937 human monocytic cell line to two different sizes of alumina ceramic particles. J Orthop Res 22:832–838 [DOI] [PubMed]
- 22.Xing S, Waddell JE, Boynton EL (2002) Changes in macrophage morphology and prolonged cell viability following exposure to polyethylene particulate in vitro. Microsc Res Tech 57:523–529 [DOI] [PubMed]
- 23.Chiba J, Rubash HE, Kim KJ et al (1994) The characterization of cytokines in the interface tissue obtained from failed cementless total hip arthroplasty with and without femoral osteolysis. Clin Orthop Relat Res:304–312 [PubMed]
- 24.Stea S, Visentin M, Granchi D et al (2000) Cytokines and osteolysis around total hip prostheses. Cytokine 12:1575–1579 [DOI] [PubMed]
- 25.Goodman SB, Huie P, Song Y et al. (1998) Cellular profile and cytokine production at prosthetic interfaces. Study of tissues retrieved from revised hip and knee replacements. J Bone Jt Surg Br 80:531–539 [DOI] [PubMed]
- 26.Sabokbar A, Rushton N (1995) Role of inflammatory mediators and adhesion molecules in the pathogenesis of aseptic loosening in total hip arthroplasties. J Arthroplasty 10:810–816 [DOI] [PubMed]
- 27.Fiorito S, Magrini L, Goalard C (2003) Pro-inflammatory and anti-inflammatory circulating cytokines and periprosthetic osteolysis. J Bone Jt Surg Br 85:1202–1206 [DOI] [PubMed]
- 28.Granchi D, Verri E, Ciapetti G et al (1998) Bone-resorbing cytokines in serum of patients with aseptic loosening of hip prostheses. J Bone Jt Surg Br 80:912–917 [DOI] [PubMed]
- 29.Hernigou P, Intrator L, Bahrami T et al (1999) Interleukin-6 in the blood of patients with total hip arthroplasty without loosening. Clin Orthop Relat Res:147–154 [DOI] [PubMed]
- 30.Nakashima Y, Sun DH, Maloney WJ et al (1998) Induction of matrix metalloproteinase expression in human macrophages by orthopaedic particulate debris in vitro. J Bone Jt Surg Br 80:694–700 [DOI] [PubMed]
- 31.Kido A, Pap G, Nagler DK et al (2004) Protease expression in interface tissues around loose arthroplasties. Clin Orthop Relat Res:230–236 [DOI] [PubMed]
- 32.Takei I, Takagi M, Santavirta S et al (2000) Messenger ribonucleic acid expression of 16 matrix metalloproteinases in bone–implant interface tissues of loose artificial hip joints. J Biomed Mater Res 52:613–620 [DOI] [PubMed]
- 33.Sethi RK, Neavyn MJ, Rubash HE et al (2003) Macrophage response to cross-linked and conventional UHMWPE. Biomaterials 24:2561–2573 [DOI] [PubMed]
- 34.Haynes DR, Boyle SJ, Rogers SD et al (1998) Variation in cytokines induced by particles from different prosthetic materials. Clin Orthop Relat Res:223–230 [PubMed]
- 35.Green TR, Fisher J, Stone M et al (1998) Polyethylene particles of a ‘critical size’ are necessary for the induction of cytokines by macrophages in vitro. Biomaterials 19:2297–2302 [DOI] [PubMed]
- 36.Yang SY, Ren W, Park Y et al (2002) Diverse cellular and apoptotic responses to variant shapes of UHMWPE particles in a murine model of inflammation. Biomaterials 23:3535–3543 [DOI] [PubMed]
- 37.Shanbhag AS, Jacobs JJ, Black J et al (1994) Macrophage/particle interactions: effect of size, composition and surface area. J Biomed Mater Res 28:81–90 [DOI] [PubMed]
- 38.Brooks RA, Wimhurst JA, Rushton N (2002) Endotoxin contamination of particles produces misleading inflammatory cytokine responses from macrophages in vitro. J Bone Jt Surg Br 84:295–299 [DOI] [PubMed]
- 39.Bi Y, Van De Motter RR, Ragab AA et al (2001) Titanium particles stimulate bone resorption by inducing differentiation of murine osteoclasts. J Bone Jt Surg Am 83-A:501–508 [DOI] [PubMed]
- 40.Skoglund B, Aspenberg P (2003) PMMA particles and pressure—a study of the osteolytic properties of two agents proposed to cause prosthetic loosening. J Orthop Res 21:196–201 [DOI] [PubMed]
- 41.McEvoy A, Jeyam M, Ferrier G et al (2002) Synergistic effect of particles and cyclic pressure on cytokine production in human monocyte/macrophages: proposed role in periprosthetic osteolysis. Bone 30:171–177 [DOI] [PubMed]
- 42.Fujishiro T, Nishikawa T, Shibanuma N et al (2004) Effect of cyclic mechanical stretch and titanium particles on prostaglandin E2 production by human macrophages in vitro. J Biomed Mater Res A 68:531–536 [DOI] [PubMed]
- 43.Goodman SB, Fornasier VL, Lee J et al (1990) The histological effects of the implantation of different sizes of polyethylene particles in the rabbit tibia. J Biomed Mater Res 24:517–524 [DOI] [PubMed]
- 44.Goodman SB, Chin RC, Magee FP (1992) Prostaglandin E2 production by the membrane surrounding loose and fixated cemented tibial hemiarthroplasties in the rabbit knee. Clin Orthop Relat Res:283–287 [PubMed]
- 45.Spector M, Shortkroff S, Hsu HP et al (1990) Tissue changes around loose prostheses. A canine model to investigate the effects of an antiinflammatory agent. Clin Orthop Relat Res:140–152 [PubMed]
- 46.Gelb H, Schumacher HR, Cuckler J et al (1994) In vivo inflammatory response to polymethylmethacrylate particulate debris: effect of size, morphology, and surface area. J Orthop Res 12:83–92 [DOI] [PubMed]
- 47.Nagase M, Udagawa E, Schumacher HR et al (1990) Prolonged inflammatory reactions induced by ceramic powders in the rat air pouch model. Nippon Seikeigeka Gakkai Zasshi 64:602–611 [PubMed]
- 48.Yang S, Wu B, Mayton L et al (2002) IL-1Ra and vIL-10 gene transfer using retroviral vectors ameliorates particle-associated inflammation in the murine air pouch model. Inflamm Res 51:342–350 [DOI] [PubMed]
- 49.Schwarz EM, Lu AP, Goater JJ et al (2000) Tumor necrosis factor-alpha/nuclear transcription factor-kappaB signaling in periprosthetic osteolysis. J Orthop Res 18:472–480 [DOI] [PubMed]
- 50.Childs LM, Goater JJ, O'Keefe RJ et al (2001) Efficacy of etanercept for wear debris-induced osteolysis. J Bone Miner Res 16:338–347 [DOI] [PubMed]
- 51.Carmody EE, Schwarz EM, Puzas JE et al (2002) Viral interleukin-10 gene inhibition of inflammation, osteoclastogenesis, and bone resorption in response to titanium particles. Arthritis Rheum 46:1298–1308 [DOI] [PubMed]
- 52.Zhang X, Morham SG, Langenbach R et al (2001) Evidence for a direct role of cyclo-oxygenase 2 in implant wear debris-induced osteolysis. J Bone Miner Res 16:660–670 [DOI] [PubMed]
- 53.Epstein NJ, Warme BA, Spanogle J et al (2005) Interleukin-1 modulates periprosthetic tissue formation in an intramedullary model of particle-induced inflammation. J Orthop Res 23:501–510 [DOI] [PubMed]
- 54.Hsu H, Lacey DL, Dunstan CR et al (1999) Tumor necrosis factor receptor family member RANK mediates osteoclast differentiation and activation induced by osteoprotegerin ligand. Proc Natl Acad Sci USA 96:3540–3545 [DOI] [PMC free article] [PubMed]
- 55.Nicholson GC, Malakellis M, Collier FM et al (2000) Induction of osteoclasts from CD14-positive human peripheral blood mononuclear cells by receptor activator of nuclear factor kappaB ligand (RANKL). Clin Sci (Lond) 99:133–140 [PubMed]
- 56.Quinn JM, Elliott J, Gillespie MT et al (1998) A combination of osteoclast differentiation factor and macrophage-colony stimulating factor is sufficient for both human and mouse osteoclast formation in vitro. Endocrinology 139:4424–4427 [DOI] [PubMed]
- 57.Simonet WS, Lacey DL, Dunstan CR et al (1997) Osteoprotegerin: a novel secreted protein involved in the regulation of bone density. Cell 89:309–319 [DOI] [PubMed]
- 58.Hofbauer LC, Schoppet M (2004) Clinical implications of the osteoprotegerin/RANKL/RANK system for bone and vascular diseases. JAMA 292:490–495 [DOI] [PubMed]
- 59.Ulrich-Vinther M, Carmody EE, Goater JJ et al (2002) Recombinant adeno-associated virus-mediated osteoprotegerin gene therapy inhibits wear debris-induced osteolysis. J Bone Jt Surg Am 84-A:1405–1412 [DOI] [PubMed]
- 60.Goater JJ, O'Keefe RJ, Rosier RN et al (2002) Efficacy of ex vivo OPG gene therapy in preventing wear debris induced osteolysis. J Orthop Res 20:169–173 [DOI] [PubMed]
- 61.Childs LM, Paschalis EP, Xing L et al (2002) In vivo RANK signaling blockade using the receptor activator of NF-kappaB:Fc effectively prevents and ameliorates wear debris-induced osteolysis via osteoclast depletion without inhibiting osteogenesis. J Bone Miner Res 17:192–199 [DOI] [PubMed]
- 62.Masui T, Sakano S, Hasegawa Y et al (2005) Expression of inflammatory cytokines, RANKL and OPG induced by titanium, cobalt–chromium and polyethylene particles. Biomaterials 26:1695–1702 [DOI] [PubMed]
- 63.Mandelin J, Li TF, Liljestrom M et al (2003) Imbalance of RANKL/RANK/OPG system in interface tissue in loosening of total hip replacement. J Bone Jt Surg Br 85:1196–1201 [DOI] [PubMed]
- 64.Gehrke T, Sers C, Morawietz L et al. (2003) Receptor activator of nuclear factor kappaB ligand is expressed in resident and inflammatory cells in aseptic and septic prosthesis loosening. Scand J Rheumatol 32:287–294 [DOI] [PubMed]
- 65.Haynes DR, Crotti TN, Potter AE et al (2001) The osteoclastogenic molecules RANKL and RANK are associated with periprosthetic osteolysis. J Bone Jt Surg Br 83:902–911 [DOI] [PubMed]
- 66.Horiki M, Nakase T, Myoui A et al (2004) Localization of RANKL in osteolytic tissue around a loosened joint prosthesis. J Bone Miner Metab 22:346–351 [DOI] [PubMed]
- 67.Takayanagi H, Ogasawara K, Hida S et al (2000) T-cell-mediated regulation of osteoclastogenesis by signalling cross-talk between RANKL and IFN-gamma. Nature 408:600–605 [DOI] [PubMed]
- 68.Rakshit DS, Ly K, Sengupta TK et al (2006) Wear debris inhibition of anti-osteoclastogenic signaling By IL6 and IFN-gamma: mechanistic insights and implications for periprosthetic osteolysis. J Bone Jt Surg Am 88:788-799 [DOI] [PubMed]
- 69.Sabokbar A, Fujikawa Y, Neale S et al (1997) Human arthroplasty derived macrophages differentiate into osteoclastic bone resorbing cells. Ann Rheum Dis 56:414–420 [DOI] [PMC free article] [PubMed]
- 70.Nakashima Y, Sun DH, Trindade MC et al (1999) Induction of macrophage C–C chemokine expression by titanium alloy and bone cement particles. J Bone Jt Surg Br 81:155–162 [DOI] [PubMed]
- 71.Haynes DR, Crotti TN, Zreiqat H (2004) Regulation of osteoclast activity in peri-implant tissues. Biomaterials 25:4877–4885 [DOI] [PubMed]
- 72.Yu X, Huang Y, Collin-Osdoby P et al (2004) CCR1 chemokines promote the chemotactic recruitment, RANKL development, and motility of osteoclasts and are induced by inflammatory cytokines in osteoblasts. J Bone Miner Res 19:2065–2077 [DOI] [PubMed]
- 73.Ishiguro N, Kojima T, Ito T et al (1997) Macrophage activation and migration in interface tissue around loosening total hip arthroplasty components. J Biomed Mater Res 35:399–406 [DOI] [PubMed]
- 74.Lassus J, Waris V, Xu JW et al (2000) Increased interleukin-8 (IL-8) expression is related to aseptic loosening of total hip replacement. Arch Orthop Trauma Surg 120:328–332 [DOI] [PubMed]
- 75.Shanbhag AS, Jacobs JJ, Black J et al (1995) Cellular mediators secreted by interfacial membranes obtained at revision total hip arthroplasty. J Arthroplasty 10:498–506 [DOI] [PubMed]
- 76.Vermes C, Chandrasekaran R, Jacobs JJ et al (2001) The effects of particulate wear debris, cytokines, and growth factors on the functions of MG-63 osteoblasts. J Bone Jt Surg Am 83-A:201–211 [DOI] [PubMed]
- 77.Yao J, Cs-Szabo G, Jacobs JJ et al (1997) Suppression of osteoblast function by titanium particles. J Bone Jt Surg Am 79:107–112 [DOI] [PubMed]
- 78.Vermes C, Roebuck KA, Chandrasekaran R et al (2000) Particulate wear debris activates protein tyrosine kinases and nuclear factor kappaB, which down-regulates type I collagen synthesis in human osteoblasts. J Bone Miner Res 15:1756–1765 [DOI] [PubMed]
- 79.Pioletti DP, Leoni L, Genini D et al (2002) Gene expression analysis of osteoblastic cells contacted by orthopedic implant particles. J Biomed Mater Res 61:408–420 [DOI] [PubMed]
- 80.Zambonin G, Colucci S, Cantatore F et al (1998) Response of human osteoblasts to polymethylmetacrylate in vitro. Calcif Tissue Int 62:362–365 [DOI] [PubMed]
- 81.Wang ML, Nesti LJ, Tuli R et al (2002) Titanium particles suppress expression of osteoblastic phenotype in human mesenchymal stem cells. J Orthop Res 20:1175–1184 [DOI] [PubMed]
- 82.Wang ML, Tuli R, Manner PA et al (2003) Direct and indirect induction of apoptosis in human mesenchymal stem cells in response to titanium particles. J Orthop Res 21:697–707 [DOI] [PubMed]
- 83.Pioletti DP, Kottelat A (2004) The influence of wear particles in the expression of osteoclastogenesis factors by osteoblasts. Biomaterials 25:5803–5808 [DOI] [PubMed]
- 84.Quinn JM, Horwood NJ, Elliott J et al (2000) Fibroblastic stromal cells express receptor activator of NF-kappa B ligand and support osteoclast differentiation. J Bone Miner Res 15:1459–1466 [DOI] [PubMed]
- 85.Wei X, Zhang X, Zuscik MJ et al (2005) Fibroblasts express RANKL and support osteoclastogenesis in a COX-2-dependent manner after stimulation with titanium particles. J Bone Miner Res 20:1136–1148 [DOI] [PubMed]
- 86.Sabokbar A, Itonaga I, Sun SG et al (2005) Arthroplasty membrane-derived fibroblasts directly induce osteoclast formation and osteolysis in aseptic loosening. J Orthop Res 23:511–519 [DOI] [PubMed]
- 87.Yao J, Glant TT, Lark MW et al (1995) The potential role of fibroblasts in periprosthetic osteolysis: fibroblast response to titanium particles. J Bone Miner Res 10:1417–1427 [DOI] [PubMed]
- 88.Manlapaz M, Maloney WJ, Smith RL (1996) In vitro activation of human fibroblasts by retrieved titanium alloy wear debris. J Orthop Res 14:465–472 [DOI] [PubMed]
- 89.Yaszay B, Trindade MC, Lind M et al (2001) Fibroblast expression of C–C chemokines in response to orthopaedic biomaterial particle challenge in vitro. J Orthop Res 19:970–976 [DOI] [PubMed]
- 90.Kotake S, Udagawa N, Hakoda M et al (2001) Activated human T cells directly induce osteoclastogenesis from human monocytes: possible role of T cells in bone destruction in rheumatoid arthritis patients. Arthritis Rheum 44:1003–1012 [DOI] [PubMed]
- 91.Gravallese EM, Manning C, Tsay A et al (2000) Synovial tissue in rheumatoid arthritis is a source of osteoclast differentiation factor. Arthritis Rheum 43:250–258 [DOI] [PubMed]
- 92.Kong YY, Feige U, Sarosi I et al (1999) Activated T cells regulate bone loss and joint destruction in adjuvant arthritis through osteoprotegerin ligand. Nature 402:304–309 [DOI] [PubMed]
- 93.Farber A, Chin R, Song Y et al (2001) Chronic antigen-specific immune-system activation may potentially be involved in the loosening of cemented acetabular components. J Biomed Mater Res 55:433–441 [DOI] [PubMed]
- 94.Arora A, Song Y, Chun L et al (2003) The role of the TH1 and TH2 immune responses in loosening and osteolysis of cemented total hip replacements. J Biomed Mater Res A 64:693–697 [DOI] [PubMed]
- 95.Baldwin L, Flanagan BF, McLaughlin PJ et al (2002) A study of tissue interface membranes from revision accord knee arthroplasty: the role of T lymphocytes. Biomaterials 23:3007–3014 [DOI] [PubMed]
- 96.Li TF, Santavirta S, Waris V et al (2001) No lymphokines in T-cells around loosened hip prostheses. Acta Orthop Scand 72:241–247 [DOI] [PubMed]
- 97.Jiranek W, Jasty M, Wang JT et al (1995) Tissue response to particulate polymethylmethacrylate in mice with various immune deficiencies. J Bone Jt Surg Am 77:1650–1661 [DOI] [PubMed]
- 98.Goodman S, Wang JS, Regula D et al (1994) T-lymphocytes are not necessary for particulate polyethylene-induced macrophage recruitment. Histologic studies of the rat tibia. Acta Orthop Scand 65:157–160 [DOI] [PubMed]
- 99.Taki N, Tatro JM, Nalepka JL et al (2005) Polyethylene and titanium particles induce osteolysis by similar, lymphocyte-independent, mechanisms. J Orthop Res 23:376–383 [DOI] [PubMed]
- 100.Sandhu J, Waddell JE, Henry M et al. (1998) The role of T cells in polyethylene particulate induced inflammation. J Rheumatol 25:1794–1799 [PubMed]
- 101.Childs LM, Goater JJ, O'Keefe RJ et al (2001) Effect of anti-tumor necrosis factor-alpha gene therapy on wear debris-induced osteolysis. J Bone Jt Surg Am 83-A:1789–1797 [DOI] [PubMed]
- 102.Hallab NJ, Anderson S, Stafford T et al (2005) Lymphocyte responses in patients with total hip arthroplasty. J Orthop Res 23:384–391 [DOI] [PubMed]
- 103.Davies AP, Willert HG, Campbell PA et al (2005) An unusual lymphocytic perivascular infiltration in tissues around contemporary metal-on-metal joint replacements. J Bone Jt Surg Am 87:18–27 [DOI] [PubMed]
- 104.DeHeer DH, Engels JA, DeVries AS et al (2001) In situ complement activation by polyethylene wear debris. J Biomed Mater Res 54:12–19 [DOI] [PubMed]
- 105.Santavirta S, Hoikka V, Eskola A et al (1990) Aggressive granulomatous lesions in cementless total hip arthroplasty. J Bone Jt Surg Br 72:980–984 [DOI] [PubMed]
- 106.Palecanda A, Paulauskis J, Al-Mutairi E et al (1999) Role of the scavenger receptor MARCO in alveolar macrophage binding of unopsonized environmental particles. J Exp Med 189:1497–1506 [DOI] [PMC free article] [PubMed]
- 107.Palmbos PL, Sytsma MJ, DeHeer DH et al (2002) Macrophage exposure to particulate titanium induces phosphorylation of the protein tyrosine kinase lyn and the phospholipases Cgamma-1 and Cgamma-2. J Orthop Res 20:483–489 [DOI] [PubMed]
- 108.Maloney WJ, Sun DH, Nakashima Y et al (1998) Effects of serum protein opsonization on cytokine release by titanium–alloy particles. J Biomed Mater Res 41:371–376 [DOI] [PubMed]
- 109.Sun DH, Trindade MC, Nakashima Y et al (2003) Human serum opsonization of orthopedic biomaterial particles: protein-binding and monocyte/macrophage activation in vitro. J Biomed Mater Res A 65:290–298 [DOI] [PubMed]
- 110.Rezzonico R, Chicheportiche R, Imbert V et al (2000) Engagement of CD11b and CD11c beta2 integrin by antibodies or soluble CD23 induces IL-1beta production on primary human monocytes through mitogen-activated protein kinase-dependent pathways. Blood 95:3868–3877 [PubMed]
- 111.Rezzonico R, Imbert V, Chicheportiche R et al (2001) Ligation of CD11b and CD11c beta(2) integrins by antibodies or soluble CD23 induces macrophage inflammatory protein 1 alpha (MIP-1 alpha) and MIP-1 beta production in primary human monocytes through a pathway dependent on nuclear factor-kappaB. Blood 97:2932–2940 [DOI] [PubMed]
- 112.Abbas S, Clohisy JC, Abu-Amer Y (2003) Mitogen-activated protein (MAP) kinases mediate PMMA-induction of osteoclasts. J Orthop Res 21:1041–1048 [DOI] [PubMed]
- 113.Boyle WJ, Simonet WS, Lacey DL (2003) Osteoclast differentiation and activation. Nature 423:337–342 [DOI] [PubMed]
- 114.Iotsova V, Caamano J, Loy J et al (1997) Osteopetrosis in mice lacking NF-kappaB1 and NF-kappaB2. Nat Med 3:1285–1289 [DOI] [PubMed]
- 115.Franzoso G, Carlson L, Xing L et al (1997) Requirement for NF-kappaB in osteoclast and B-cell development. Genes Dev 11:3482–3496 [DOI] [PMC free article] [PubMed]
- 116.Clohisy JC, Hirayama T, Frazier E et al (2004) NF-kB signaling blockade abolishes implant particle-induced osteoclastogenesis. J Orthop Res 22:13–20 [DOI] [PubMed]
- 117.Ren W, Li XH, Chen BD et al (2004) Erythromycin inhibits wear debris-induced osteoclastogenesis by modulation of murine macrophage NF-kappaB activity. J Orthop Res 22:21–29 [DOI] [PubMed]
- 118.Miyanishi K, Trindade MC, Ma T et al (2003) Periprosthetic osteolysis: induction of vascular endothelial growth factor from human monocyte/macrophages by orthopaedic biomaterial particles. J Bone Miner Res 18:1573–1583 [DOI] [PubMed]
- 119.Shuai K, Liu B (2003) Regulation of JAK-STAT signalling in the immune system. Nat Rev Immunol 3:900–911 [DOI] [PubMed]
- 120.Sengupta TK, Talbot ES, Scherle PA et al (1998) Rapid inhibition of interleukin-6 signaling and Stat3 activation mediated by mitogen-activated protein kinases. Proc Natl Acad Sci USA 95:11107–11112 [DOI] [PMC free article] [PubMed]
- 121.Ahmed ST, Ivashkiv LB (2000) Inhibition of IL-6 and IL-10 signaling and Stat activation by inflammatory and stress pathways. J Immunol 165:5227–5237 [DOI] [PubMed]
- 122.Kubo M, Hanada T, Yoshimura A (2003) Suppressors of cytokine signaling and immunity. Nat Immunol 4:1169–1176 [DOI] [PubMed]
- 123.Sochart DH (1999) Relationship of acetabular wear to osteolysis and loosening in total hip arthroplasty. Clin Orthop Relat Res:135–150 [PubMed]
- 124.Ilchmann T, Markovic L, Joshi A et al (1998) Migration and wear of long-term successful Charnley total hip replacements. J Bone Jt Surg Br 80:377–381 [DOI] [PubMed]
- 125.Muratoglu OK, Bragdon CR, O'Connor DO et al (2001) A novel method of cross-linking ultra-high-molecular-weight polyethylene to improve wear, reduce oxidation, and retain mechanical properties. Recipient of the 1999 HAP Paul Award. J Arthroplasty 16:149–160 [DOI] [PubMed]
- 126.Muratoglu OK, Bragdon CR, O'Connor D et al (2001) Larger diameter femoral heads used in conjunction with a highly cross-linked ultra-high molecular weight polyethylene: a new concept. J Arthroplasty 16:24–30 [DOI] [PubMed]
- 127.Heisel C, Silva M, dela Rosa MA et al (2004) Short-term in vivo wear of cross-linked polyethylene. J Bone Jt Surg Am 86-A:748–751 [DOI] [PubMed]
- 128.Digas G, Karrholm J, Thanner J et al (2003) Highly cross-linked polyethylene in cemented THA: randomized study of 61 hips. Clin Orthop Relat Res:126–138 [DOI] [PubMed]
- 129.D'Antonio JA, Manley MT, Capello WN et al (2005) Five-year experience with Crossfire highly cross-linked polyethylene. Clin Orthop Relat Res 441:143–150 [DOI] [PubMed]
- 130.Engh CA, Sychterz CJ, Engh CA Jr (2005) Conventional ultra-high molecular weight polyethylene: a gold standard of sorts. Instr Course Lect 54:183–187 [PubMed]
- 131.Barrack RL, Burak C, Skinner HB (2004) Concerns about ceramics in THA. Clin Orthop Relat Res:73–79 [DOI] [PubMed]
- 132.Capello WN, Dantonio JA, Feinberg JR et al (2005) Alternative bearing surfaces: alumina ceramic bearings for total hip arthroplasty. Instr Course Lect 54:171–176 [PubMed]
- 133.Jazrawi LM, Kummer FJ, DiCesare PE (1998) Alternative bearing surfaces for total joint arthroplasty. J Am Acad Orthop Surg 6:198–203 [DOI] [PubMed]
- 134.Bourne RB, Barrack R, Rorabeck CH et al (2005) Arthroplasty options for the young patient: Oxinium on cross-linked polyethylene. Clin Orthop Relat Res 441:159–167 [DOI] [PubMed]
- 135.MacDonald SJ (2004) Metal-on-metal total hip arthroplasty: the concerns. Clin Orthop Relat Res:86–93 [DOI] [PubMed]
- 136.Cuckler JM (2005) The rationale for metal-on-metal total hip arthroplasty. Clin Orthop Relat Res 441:132–136 [DOI] [PubMed]
- 137.Pollice PF, Rosier RN, Looney RJ et al (2001) Oral pentoxifylline inhibits release of tumor necrosis factor-alpha from human peripheral blood monocytes: a potential treatment for aseptic loosening of total joint components. J Bone Jt Surg Am 83-A:1057–1061 [DOI] [PubMed]
- 138.Schwarz EM, Campbell D, Totterman S et al (2003) Use of volumetric computerized tomography as a primary outcome measure to evaluate drug efficacy in the prevention of peri-prosthetic osteolysis: a 1-year clinical pilot of etanercept vs. placebo. J Orthop Res 21:1049–1055 [DOI] [PubMed]
- 139.von Knoch M, Wedemeyer C, Pingsmann A et al (2005) The decrease of particle-induced osteolysis after a single dose of bisphosphonate. Biomaterials 26:1803–1808 [DOI] [PubMed]
- 140.von Knoch F, Heckelei A, Wedemeyer C et al (2005) The effect of simvastatin on polyethylene particle-induced osteolysis. Biomaterials 26:3549–3555 [DOI] [PubMed]
- 141.Bekker PJ, Holloway DL, Rasmussen AS et al (2005) A single-dose placebo-controlled study of AMG 162, a fully human monoclonal antibody to RANKL, in postmenopausal women. 2004. J Bone Miner Res 20:2275–2282 [DOI] [PubMed]
- 142.Takahashi N, Ozawa H (2005) A new treatment for osteoporosis using fully human monoclonal antibody to RANKL, AMG 162. Clin Calcium 15:43–48 [PubMed]
- 143.Zwerina J, Hayer S, Tohidast-Akrad M et al (2004) Single and combined inhibition of tumor necrosis factor, interleukin-1, and RANKL pathways in tumor necrosis factor-induced arthritis: effects on synovial inflammation, bone erosion, and cartilage destruction. Arthritis Rheum 50:277–290 [DOI] [PubMed]
- 144.Dai S, Hirayama T, Abbas S et al (2004) The IkappaB kinase (IKK) inhibitor, NEMO-binding domain peptide, blocks osteoclastogenesis and bone erosion in inflammatory arthritis. J Biol Chem 279:37219–37222 [DOI] [PubMed]
- 145.Bossard MJ, Tomaszek TA, Levy MA et al (1999) Mechanism of inhibition of cathepsin K by potent, selective 1,5-diacylcarbohydrazides: a new class of mechanism-based inhibitors of thiol proteases. Biochemistry 38:15893–15902 [DOI] [PubMed]
- 146.Lark MW, Stroup GB, James IE et al (2002) A potent small molecule, nonpeptide inhibitor of cathepsin K (SB 331750) prevents bone matrix resorption in the ovariectomized rat. Bone 30:746–753 [DOI] [PubMed]
- 147.Visentin L, Dodds RA, Valente M et al (2000) A selective inhibitor of the osteoclastic V-H(+)-ATPase prevents bone loss in both thyroparathyroidectomized and ovariectomized rats. J Clin Invest 106:309–318 [DOI] [PMC free article] [PubMed]
- 148.Lark MW, Stroup GB, Dodds RA et al (2001) Antagonism of the osteoclast vitronectin receptor with an orally active nonpeptide inhibitor prevents cancellous bone loss in the ovariectomized rat. J Bone Miner Res 16:319–327 [DOI] [PubMed]
- 149.Shakespeare WC, Metcalf CA, 3rd, Wang Y et al (2003) Novel bone-targeted Src tyrosine kinase inhibitor drug discovery. Curr Opin Drug Discov Dev 6:729–741 [PubMed]
- 150.Potter HG, Nestor BJ, Sofka CM et al (2004) Magnetic resonance imaging after total hip arthroplasty: evaluation of periprosthetic soft tissue. J Bone Jt Surg Am 86-A:1947–1954 [DOI] [PubMed]
- 151.Looney RJ, Boyd A, Totterman S et al (2002) Volumetric computerized tomography as a measurement of periprosthetic acetabular osteolysis and its correlation with wear. Arthritis Res 4:59–63 [DOI] [PMC free article] [PubMed]
- 152.Puri L, Wixson RL, Stern SH et al (2002) Use of helical computed tomography for the assessment of acetabular osteolysis after total hip arthroplasty. J Bone Jt Surg Am 84-A:609–614 [DOI] [PubMed]