Abstract
An initiative to reduce childhood mortality due to malaria, diarrhoea and vaccine-preventable diseases, called the Africa Child Survival Initiative—Combatting Childhood Communicable Diseases (CCCD) project, was started in 1982 and is now operating in 13 African countries, 12 of which are endemic for malaria. The project's malaria control strategy relies on the use of drugs, mainly chloroquine, to prevent severe illness and death in children less than 5 years of age; chemoprophylaxis for pregnant women is also advised to prevent low birth weight in newborns. The strategy is based on WHO recommendations which focus on improved diagnosis and treatment of cases and chemoprophylaxis for pregnant women.
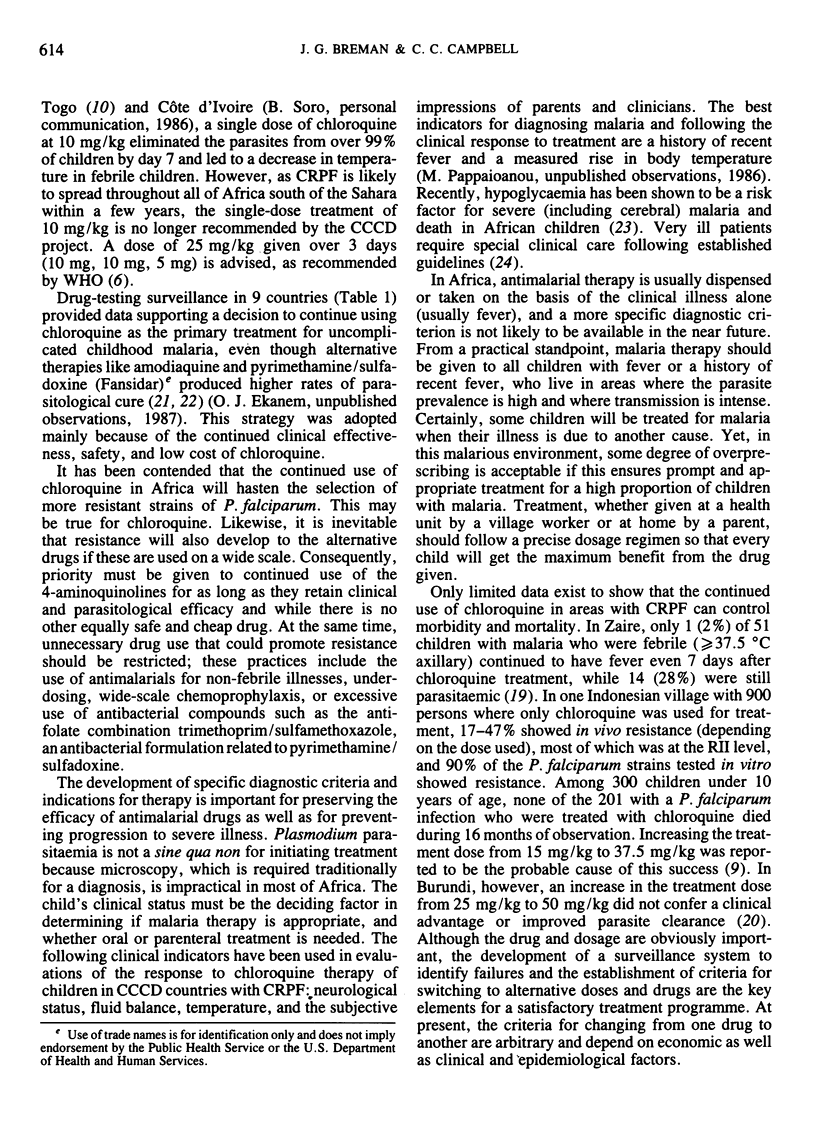
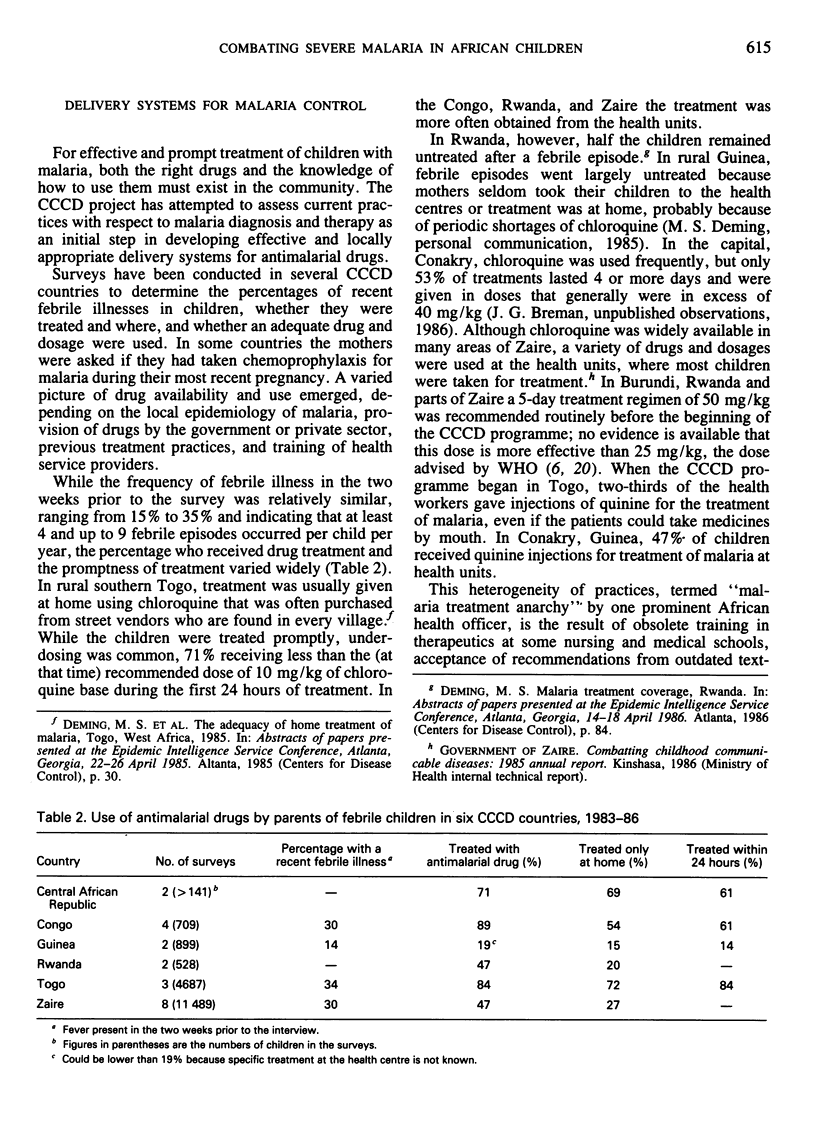
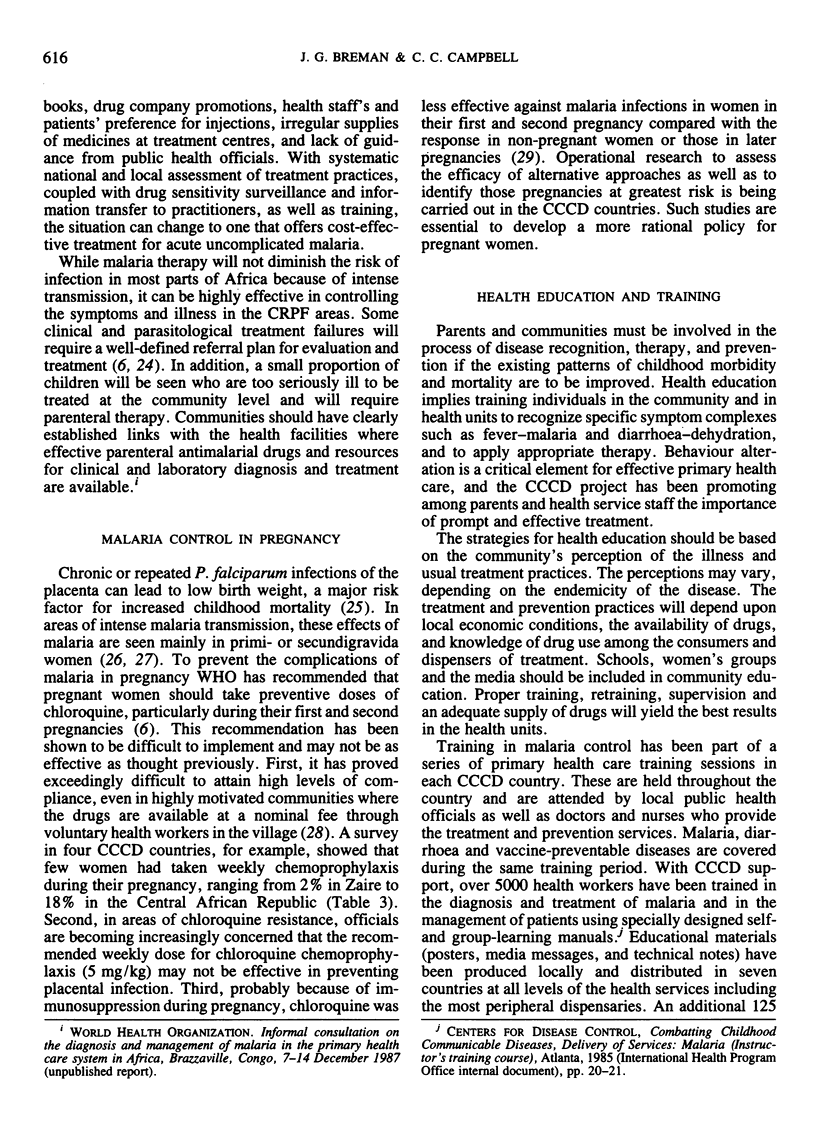
In 9 out of the 13 CCCD countries the sensitivity of Plasmodium falciparum to chloroquine in children was investigated and a drug sensitivity surveillance network was established. In areas with chloroquine-resistant P. falciparum, treatment with chloroquine was found to decrease the temperature in febrile children and to greatly reduce the parasite density, thus preventing severe illness and possible death. Baseline surveys in 6 countries have shown a wide range of treatment practices, e.g., use of chloroquine in various doses without standard guidelines and the excessive use of quinine and chloroquine injections in some health units. As pregnant women are often not taking chemoprophylaxis, research has been started on alternative approaches to drug treatment to prevent the adverse effects of malaria on the fetus.
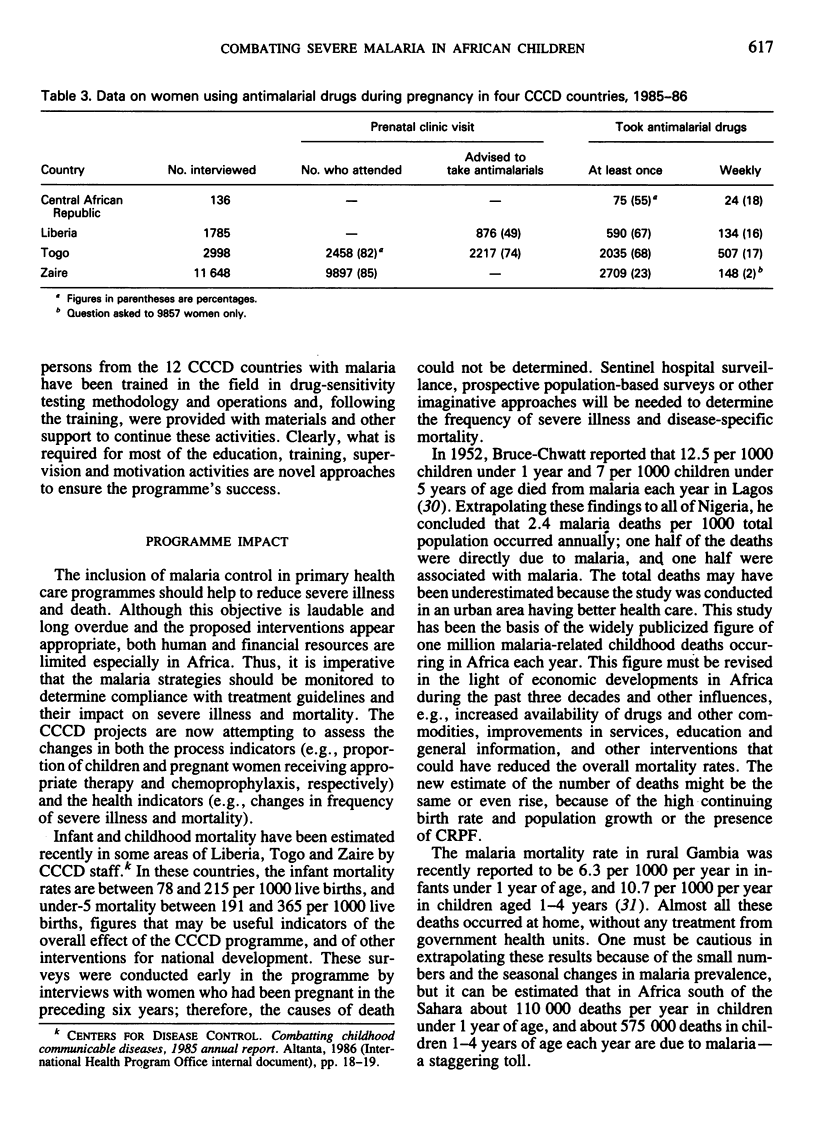
Only 4 of the 12 malarious countries had malaria control units when their CCCD programme began and these were concerned mainly with vector control issues; 11 of 12 countries now have such units and a written CCCD malaria plan. These countries have now integrated malaria control activities into primary health care and have begun to implement standardized treatment and prevention practices that are described in their national CCCD malaria plans.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BRUCE-CHWATT L. J. Malaria in African infants and children in Southern Nigeria. Ann Trop Med Parasitol. 1952 Sep;46(2):173–200. doi: 10.1080/00034983.1952.11685522. [DOI] [PubMed] [Google Scholar]
- Breman J. G., Gayibor A., Roberts J. M., Sexton J. D., Agbo K., Miller K. D., Karsa T., Murphy K. Single-dose chloroquine therapy for Plasmodium falciparum in children in Togo, West Africa. Am J Trop Med Hyg. 1987 May;36(3):469–473. doi: 10.4269/ajtmh.1987.36.469. [DOI] [PubMed] [Google Scholar]
- Carme B., Benthein F., Moudzeo H., Bitsi A., Madzou G. Chimio-résistance de Plasmodium falciparum au Congo. I. Etude in vivo après 10 et 25 mg/kg de chloroquine (235 tests). Bull Soc Pathol Exot Filiales. 1986;79(4):490–502. [PubMed] [Google Scholar]
- Coosemans M. H., Hendrix L., Barutwanayo M., Butoyi G., Onori E. Pharmacorésistance de Plasmodium falciparum au Burundi. Bull World Health Organ. 1985;63(2):331–338. [PMC free article] [PubMed] [Google Scholar]
- Deloron P., Sexton J. D., Bugilimfura L., Sezibera C. Amodiaquine and sulfadoxine-pyrimethamine as treatment for chloroquine-resistant Plasmodium falciparum in Rwanda. Am J Trop Med Hyg. 1988 Mar;38(2):244–248. doi: 10.4269/ajtmh.1988.38.244. [DOI] [PubMed] [Google Scholar]
- Heymann D. L., Khoromana C. O., Wirima J. J., Campbell C. C. Comparative efficacy of alternative primary therapies for Plasmodium falciparum infections in Malawi. Trans R Soc Trop Med Hyg. 1987;81(5):722–724. doi: 10.1016/0035-9203(87)90005-8. [DOI] [PubMed] [Google Scholar]
- Hoffman S. L., Masbar S., Hussein P. R., Soewarta A., Harun S., Marwoto H. A., Campbell J. R., Smrkovski L., Purnomo, Wiady I. Absence of malaria mortality in villagers with chloroquine-resistant Plasmodium falciparum treated with chloroquine. Trans R Soc Trop Med Hyg. 1984;78(2):175–178. doi: 10.1016/0035-9203(84)90271-2. [DOI] [PubMed] [Google Scholar]
- Khoromana C. O., Campbell C. C., Wirima J. J., Heymann D. L. In vivo efficacy of chloroquine treatment for Plasmodium falciparum in Malawian children under five years of age. Am J Trop Med Hyg. 1986 May;35(3):465–471. doi: 10.4269/ajtmh.1986.35.465. [DOI] [PubMed] [Google Scholar]
- McCormick M. C. The contribution of low birth weight to infant mortality and childhood morbidity. N Engl J Med. 1985 Jan 10;312(2):82–90. doi: 10.1056/NEJM198501103120204. [DOI] [PubMed] [Google Scholar]
- McGregor I. A., Wilson M. E., Billewicz W. Z. Malaria infection of the placenta in The Gambia, West Africa; its incidence and relationship to stillbirth, birthweight and placental weight. Trans R Soc Trop Med Hyg. 1983;77(2):232–244. doi: 10.1016/0035-9203(83)90081-0. [DOI] [PubMed] [Google Scholar]
- Moran J. S., Bernard K. W., Greenberg A. E., Patchen L., Waterman S., Bennet H. S. Failure of chloroquine treatment to prevent malaria in Americans in West Africa. JAMA. 1987 Nov 6;258(17):2376–2377. [PubMed] [Google Scholar]
- Ruebush T. K., 2nd, Breman J. G., Kaiser R. L., Warren M. Selective primary health care. XXIV. Malaria. Rev Infect Dis. 1986 May-Jun;8(3):454–466. doi: 10.1093/clinids/8.3.454. [DOI] [PubMed] [Google Scholar]
- Salako L. A., Fadeke Aderounmu A. In-vitro chloroquine and mefloquine-resistant Plasmodium falciparum in Nigeria. Lancet. 1987 Mar 7;1(8532):572–573. doi: 10.1016/s0140-6736(87)90221-2. [DOI] [PubMed] [Google Scholar]
- Sexton J. D., Deloron P., Bugilimfura L., Ntilivamunda A., Neill M. Parasitologic and clinical efficacy of 25 and 50 mg/kg of chloroquine for treatment of Plasmodium falciparum malaria in Rwandan children. Am J Trop Med Hyg. 1988 Mar;38(2):237–243. doi: 10.4269/ajtmh.1988.38.237. [DOI] [PubMed] [Google Scholar]
- Spencer H. C., Kaseje D. C., Sempebwa E. K., Huong A. Y., Roberts J. M. Malaria chemoprophylaxis to pregnant women provided by community health workers in Saradidi, Kenya. II. Effect on parasitaemia and haemoglobin levels. Ann Trop Med Parasitol. 1987 Apr;81 (Suppl 1):83–89. doi: 10.1080/00034983.1987.11812192. [DOI] [PubMed] [Google Scholar]
- Steketee R. W., Brandling-Bennett A. D., Kaseje D. C., Schwartz I. K., Churchill F. C. In vivo response of Plasmodium falciparum to chloroquine in pregnant and non-pregnant women in Siaya District, Kenya. Bull World Health Organ. 1987;65(6):885–890. [PMC free article] [PubMed] [Google Scholar]
- Steketee R. W., Breman J. G., Paluku K. M., Moore M., Roy J., Ma-Disu M. Malaria infection in pregnant women in Zaire: the effects and the potential for intervention. Ann Trop Med Parasitol. 1988 Apr;82(2):113–120. doi: 10.1080/00034983.1988.11812217. [DOI] [PubMed] [Google Scholar]
- White N. J., Miller K. D., Marsh K., Berry C. D., Turner R. C., Williamson D. H., Brown J. Hypoglycaemia in African children with severe malaria. Lancet. 1987 Mar 28;1(8535):708–711. doi: 10.1016/s0140-6736(87)90354-0. [DOI] [PubMed] [Google Scholar]


