Abstract
PR-39 is a porcine antimicrobial peptide that kills bacteria with a mechanism that does not involve cell lysis. Here, we demonstrate that Salmonella enterica serovar Typhimurium can rapidly acquire mutations that reduce susceptibility to PR-39. Resistant mutants appeared at a rate of 0.4 × 10−6 per cell per generation. These mutants were about four times more resistant than the wild type and showed a greatly reduced rate of killing. Genetic analysis revealed mutations in the putative transport protein SbmA as being responsible for the observed resistance. These sbmA mutants were as fit as the wild-type parental strain as measured by growth rates in culture medium and mice and by long-term survival in stationary phase. These results suggest that resistance to certain antimicrobial peptides can rapidly develop without an obvious fitness cost for the bacteria and that resistance development could become a threat to the efficacy of antimicrobial peptides if used in a clinical setting.
The rapid emergence of antibiotic resistance makes development of alternative treatment regimes important. Antimicrobial peptides (AMPs) are essential components of innate immunity that have been identified in organisms ranging from bacteria to humans (9, 54). These peptides are typically less than 100 amino acids in length, positively charged, and amphiphilic but differ greatly in structure and function (54). AMPs often kill quickly and can possess activity against bacteria, fungi, viruses, and protozoa (44). Initial contact between the AMP and the target cell is mediated by electrostatic interactions between the positively charged peptides and the negatively charged bacterial membranes (24). Many peptides then act on the cytoplasmic membrane and subsequently intracellularly, while some are taken into the cell and act mainly on intracellular targets (24). Since AMPs show good efficacy in vitro and there are few reports of resistance, it has been argued that these molecules are suitable for the treatment of bacterial infections (5, 17, 34). The apparent absence of completely resistant bacteria has been suggested to be caused by, for example, the mechanistic difficulties associated with developing resistance to membrane-permeating agents, a high fitness cost of resistance for the bacteria, and the simultaneous exposure to several peptides in a host (26, 54). However, few systematic screening studies of resistance development have been performed, and given the ability of bacteria to adapt to new environments and to develop resistance to existing antibacterial agents, it seems possible that the extensive use of peptides in medicine could also select for novel resistance mechanisms to AMPs. The following observations support this suggestion.
First, bacteria have already evolved several mechanisms to withstand killing by AMPs, and the ability to survive AMP exposure is an important virulence factor of several human pathogens (41). These intrinsic resistance mechanisms include the PhoP-PhoQ two-component signaling pathway in Salmonella that regulates several genes involved in resistance, e.g., the PmrA-PmrB two-component system activating transcription of genes responsible for resistance-enhancing lipopolysaccharide (LPS) modifications that results in a more positively charged membrane that repels positively charged peptides (20, 21). PhoP-PhoQ also activates pagP, which is responsible for incorporating an additional fatty acid into the lipid A portion of LPS, leading to a decreased permeability of the membrane (22). A third PhoP-PhoQ-regulated gene is pgtE, which encodes an outer membrane protease that can cleave α-helical AMPs (19). In Staphylococcus aureus, the dlt operon and mprF confer AMP resistance through modifications that result in a more positively charged cell wall (42, 43). Disruption of these genes renders the bacteria more sensitive to AMP killing and less virulent in mice (31, 42, 43). Other intrinsic resistance mechanisms involve the secretion of molecules that can bind to and neutralize peptides, the suppression of AMP induction in the host, and energy-dependent efflux systems that can transport certain peptides out of the cytoplasm (14, 28, 47).
A second observation is that certain bacteria that are able to cause more severe infections have an increased resistance to AMPs. In a study of clinical Escherichia coli isolates from patients with urinary tract infections, substantial variability in susceptibility to the human cathelicidin LL-37 was observed. E. coli strains isolated from patients with more-severe upper urinary tract infections were more resistant to LL-37 than were strains from individuals with infections of the lower urinary tract, indicating a link between the invasiveness of the E. coli strain and the level of resistance (8). Another example is provided by the analysis of infective endocarditis (IE), where bacterial isolates causing IE were significantly more resistant to platelet microbicidal protein than non-IE-causing isolates, suggesting that resistance is important for the ability to cause IE (51).
Lastly, AMP-resistant mutants have been isolated on rare occasions. While most mechanisms conferring resistance have been found by screening for hypersensitivity following gene disruption, some have been found by direct selection for increased resistance to, for example, thrombin-induced platelet microbicidal protein in S. aureus, cathelicidin peptides in Streptococcus pyogenes, and pexiganan in E. coli and in Pseudomonas fluorescens (12, 37, 40). In a recent study, Mattiuzzo et al. mutagenized E. coli cells and selected clones resistant to the proline-rich AMP Bac7 (35). It was shown that inactivation of the gene sbmA, which encodes a putative transporter protein, gave increased resistance to Bac7 due to impaired internalization of the peptide.
Here, we report the ability of Salmonella enterica serovar Typhimurium to develop resistance to the AMP PR-39. PR-39 is a linear, proline- and arginine-rich peptide that was first isolated from porcine small intestine by Agerberth and coworkers in 1991 (1). It is one of the cathelicidin AMPs, which have been identified only in mammals (53). PR-39 is involved in many important immune responses, e.g., as a chemoattractant for neutrophils (27) and by inducing expression of heparan sulfate proteoglycans involved in wound repair (16). PR-39 demonstrates strong activity against several bacteria (1, 48) and has been shown to increase significantly in the sera of pigs with salmonellosis (55). The peptide has not been seen to form pores in bacterial membranes and is thought to have multiple intracellular targets, namely the interruption of DNA and protein synthesis, possibly through induction of proteolytic activity in the bacteria (6).
In our selection system, spontaneous, stable mutants with decreased susceptibility to PR-39 arise at a high rate. We identified a variety of mutations in the gene sbmA that are associated with the resistance phenotype. These mutations did not have a detectable negative effect on the fitness of the resistant bacteria either in vitro or in vivo.
MATERIALS AND METHODS
Bacterial strains, media, and growth conditions.
Strains used in this study were derived from Salmonella enterica serovar Typhimurium LT2 (referred to as Salmonella enterica serovar Typhimurium) and are listed in Table 1. Strain DA6080, carrying a neutral kanamycin marker (cobI24::MudJ Kanr) (36), was used as the reference strain in all competition experiments. Bacteria were grown at 37°C in Iso-Sensitest broth (Oxoid Ltd., Hampshire, England), except where indicated otherwise. SeaKem LE agarose (Cambrex Bio Science Inc., Rockland, ME) was added at a final concentration of 1% for solid media. When appropriate, the following antibiotics were added to the growth medium: kanamycin (50 μg/ml), ampicillin (100 μg/ml), and tetracycline (15 μg/ml) (all from Sigma-Aldrich AB, Stockholm, Sweden). Antibiotic susceptibility was determined with Etest strips as described by the manufacturer (AB Biodisk, Solna, Sweden). MICs to the glycopeptide antibiotic bleomycin (Calbiochem, Nottingham, United Kingdom) and to the peptides protamine sulfate (Sigma-Aldrich AB, Stockholm, Sweden), CNY 100 H-L, LL-37, CRAMP (extended form) (3), and rCRAMP (Innovagen AB, Lund, Sweden) were determined in Mueller-Hinton broth (Becton, Dickinson and Company, Sparks, MD) with various concentrations of peptide and approximately 5 × 105 CFU/ml in a final volume of 50 or 100 μl. Three independent experiments with duplicate samples were performed for each peptide.
TABLE 1.
Genotypes and MICs of strains used in this study
| Strain | Genotypea | MIC (μM)b | Reference |
|---|---|---|---|
| DA6192 | Wild type (parent) | 2 | Strain collection |
| DA10896 | sbmA (ACG→AAG, T375K) | 6 | This study |
| DA10897 | sbmA (TGG→TAG, W373Stop) | 7 | This study |
| DA10898 | sbmA (del bp 967) | 7 | This study |
| DA10899 | sbmA (CAG→TAG, Q179Stop) | 6 | This study |
| DA10902 | sbmA (del bp 843-844) | 7 | This study |
| DA10905 | sbmA (CTG→CCG, L379P) | 7 | This study |
| DA10907 | sbmA (GAA→AAA, E287K) | 7 | This study |
| DA10912 | sbmA (TAT→TGT, Y326C) | 5 | This study |
| DA10913 | sbmA (TGC→TGA, C67Stop) | 7 | This study |
| DA10914 | sbmA (TCA→TTA, S251L) | 7 | This study |
| DA12088 | ΔsbmA | 6 | This study |
| DA13090 | ΔsbmA/pBAD30::sbmA | 3 | This study |
| DA13088 | wt/pBAD30::sbmA | 1.5 | This study |
| DA14344 | DA10899/pBAD30::sbmA | 3 | This study |
GenBank accession no. for sbmA sequence is NC_003197, region 430359.0.431579. wt, wild type.
Experiments for strains DA13090, DA13088, and DA14344 were performed in the presence of 0.1% arabinose. The MIC of the wild-type strain was 3 μM in these experiments.
PCR and sequencing.
Primers used for PCR and sequencing are shown in Table 2. Template DNA was prepared by dissolving bacterial colonies in 200 μl double-distilled water, boiling them for 5 min, and centrifuging them briefly. In some reactions, samples from bacterial colonies were used as templates. The genes of interest were PCR amplified using the GeneAmp PCR system 9700 and AmpliTaq Gold polymerase (Applied Biosystem, Stockholm, Sweden). Unless indicated as otherwise, the following PCR program was used: denaturation at 95°C for 5 min was followed by 31 cycles of 30 s at 94°C and 30 s at 53°C to 57°C and then elongation at 72°C (1 min/kb). An additional elongation step of 7 min was included after the final cycle. PCR products were purified from solution or a 1% agarose gel using Illustra GFX PCR DNA and a gel band purification kit (GE Healthcare, Buckinghamshire, United Kingdom). Plasmids were isolated with an E.Z.N.A. plasmid minikit (Omega Bio-Tek, Inc., Doraville, GA). All sequencing reactions were carried out at the sequencing facility at MWG Biotech AG, Martinsried, Germany (Sanger sequencing with ABI 3730XL). Sequences were analyzed using CLC Free Workbench software (version 4.5.1).
TABLE 2.
Primers used for PCR and sequencing
| Primer | Sequence (5′-3′)a | Primer binding site(s)b |
|---|---|---|
| yaiU_F | AGCGCCTACACCGATGCTAA | −2344 |
| yaiW_R | TGACTACTACAGCCAGCCAA | 1306 |
| PR_seq2 | TCAGGTACTGGAACTTCGTG | −1804 |
| PR_seq3 | GGTACGTCCATCCCGATGAT | −1251 |
| PR_seq4 | TACCGTTCCCTGATCGAGCA | −644 |
| PR_seq5 | GCGTCACAACGTAGGTCACA | −116 |
| PR_seq6 | GGTGATCGGTGTGCTGAACA | 447 |
| PR_seq7 | GCGCATTCTCTATTTGCAGG | 966 |
| sbmA_1 | CTCGGCATAACGATCAACGA | −466 |
| sbmA_2 | TGGTCGCTGGACTATCTGAT | 176 |
| EcoRIsbmA_F | GTGAATTCGTCACAGCAGCCGTAATAA | −45 |
| XbaIsbmA_R | GCTCTAGACGCCGACATAACGTTTCCTT | 1244 |
| LTsbmA_F | CGTCACAGCAGCCGTAATAAAGATAAGAAGTTA GCAGGAGAGCATGTGTAGGCTGGAGCTGCTTCG | −46 |
| LTsbmA_R | CGGGACGCCGCCGACATAACGTTTCCTTCTGTT AGCTAAAAGAGTGCATATGAATATCCTCCTTAG | 1252 |
| Arb1 | GGCCACGCGTCGACTAGTACNNNNNNNNNNGATAT | Arbitrary |
| Arb6 | GGCCACGCGTCGACTAGTACNNNNNNNNNNACGCC | Arbitrary |
| Arb2 | GGCCACGCGTCGACTAGTAC | Arb1 and Arb6 |
| TL | TCCATTGCTGTTGACAAAGGGAAT | Mini Tn10 (Tetr) |
| TR | ACCTTTGGTCACCAACGCTTTTCC | Mini Tn10 (Tetr) |
| Universal | GACAAGATGTGTATCCACCTTAAC | Mini Tn10 (Tetr) |
| pBAD_F | TTAGCGGATCCTACCTGACG | pBAD30 |
| pBAD_F2 | CGCTTCAGCCATACTTTTCA | pBAD30 |
| pBAD_R | ACGGCGTTTCACTTCTGAGT | pBAD30 |
Restriction enzyme cleavage sites are underlined.
For the first 14 primers, the primer binding site is indicated as the position of the 5′ nucleotide in relation to the first nucleotide in the start codon of sbmA. A minus indicates nucleotides upstream of the start codon.
AMPs and isolation of mutants.
PR-39 was synthesized by EZBiolab Inc., Westfield, IN, and by Innovagen AB, Lund, Sweden. The peptide was dissolved in double-distilled water. Ten-microliter drops with ∼4 × 106 bacteria from independent 1-ml cultures were spotted onto medium supplemented with 3 μM PR-39, and plates were incubated at 37°C overnight. Twenty-one independent survivors were isolated and tested for growth by applying drops of 106 bacteria onto media containing 3 μM PR-39.
Mutation rate determination.
Approximately 106 CFU from each of 27 independent cultures were spotted on plates containing 3 μM PR-39, and the number of colonies in each spot was scored the next day. The mutation rate to PR-39 resistance was calculated from the median number of colonies and the number of applied cells (32). To determine the amount of background growth, spots with no visible colonies after incubation were cut out with a scalpel and transferred to a microcentrifuge tube containing 200 μl phosphate-buffered saline (PBS). After the mixture was vortexed three times for 10 s each time, different dilutions were spread onto Luria-Bertani agar (LA) plates to determine the number of viable cells.
PR-39 susceptibility assays.
MIC assays were performed with 96-microwell plates (round bottom; Nunc A/S, Roskilde, Denmark). Bacteria were grown to mid-exponential phase and diluted to approximately 105 CFU/ml, and 90 μl of the diluted bacteria were mixed with various concentrations of PR-39 to a final volume of 100 μl. The microwell plates were incubated at 37°C with continuous shaking (200 rpm). The MIC was defined as the lowest concentration of PR-39 yielding no visible growth. All experiments were done with duplicate samples on at least two separate occasions. Killing over time was determined in 96-microwell plates in a total volume of 100 μl. Approximately 5 × 106 CFU/ml were subjected to 0, 2, 4, 8, and 16 μM PR-39. Samples were removed and plated before the start of the experiment and after 0.5, 1, 4, and 24 h to determine the number of viable cells. Percent survival was calculated for each time point by dividing the number of viable cells after peptide treatment with the total number of viable cells and multiplying the quotient by 100.
Fitness measurements. (i) Growth rate measurements.
The growth rates of 10 of the resistant mutants were determined using a Bioscreen C analyzer (Oy Growth Curves Ab Ltd., Helsinki, Finland). Approximately 106 cells were inoculated into 400 μl Iso-Sensitest broth in a bioscreen plate and incubated at 37°C with continuous shaking. Absorbance was measured at 600 nm at regular intervals. Each strain was assayed in four independent cultures in at least three separate experiments. The susceptible wild-type strain was included as a reference, and relative growth rates were calculated as the growth rate of the mutants divided by the growth rate of the reference strain.
(ii) Competition experiments in laboratory media.
Fitness was also determined by competition experiments between five of the mutants and the genetically tagged wild-type strain DA6080 at a 1:1 ratio in Luria-Bertani broth (LB) and M9 medium with glycerol. A total of 106 cells of each mutant was mixed with 106 wild-type cells in 1-ml cultures. Each day, 106 bacteria were passaged to fresh medium. Samples were spread in duplicate on LA plates after every other cycle. After 8 h of incubation, the samples were printed onto medium with and without kanamycin. The competition index (CI) was calculated as the ratio of the PR-39-resistant mutant cells to the cells of the reference strain and was plotted against the number of generations of growth. A selection coefficient, s, a measure of the population growth rates averaged over the entire experiment, was calculated from each competition as the slope of the following regression model (13): s = [lnR(t)/R(0)]/[t × ln(2)]. In this model, R is the ratio of the number of mutant bacteria to the number of wild-type bacteria, t is the number of generations, and the unit of s is the number of generations−1. The fitness of the wild type was set to 1, and the relative fitness of the mutants was calculated as 1 + smutant.
(iii) Competition experiments with mice.
The fitness of four PR-39-resistant strains was measured by performing competition experiments with mice. The mouse experiments were carried out at the animal facility at the Microbiology and Tumor Biology Centre, Karolinska Institute (Stockholm, Sweden), in compliance with national and institutional guidelines (ethical permit N107/06). Each bacterial strain was grown to logarithmic growth phase and diluted and mixed with strain DA6080 at a 1:1 ratio in PBS. For each competition experiment, four 7-week-old female BALB/c mice were infected with ∼2 × 105 cells in a 100-μl volume of PBS by intraperitoneal injection. The mice were sacrificed after 3 days, and the livers and spleens were removed and homogenized in PBS. The ratio of the number of mutant bacteria to the number of reference strain bacteria was determined by plating different dilutions of the homogenates on LA plates and LA plates supplemented with kanamycin. The CI was calculated as the ratio of the mutant population to the wild-type population after one cycle of growth in mice (∼10 generations). From this value and the number of generations of growth in mice, the selection coefficient (s) was calculated using the following equation (36): s = ln(CI)/[10 × ln(2)].
Genetic techniques. (i) Isolation of mini-Tn10 transposons linked to PR-39 resistance mutations.
P22 phage was grown in a pool of random mini-Tn10 Δ16Δ17 (Tetr) insertions in a wild-type genetic background and used to infect one PR-39-resistant strain. Transductants were selected on Iso-Sensitest plates with tetracycline. Loss of PR-39 resistance was screened for by streaking colonies on medium with and without 3 μM PR-39. Tetracycline-resistant and PR-39-susceptible clones were identified and backcrossed to the original mutant strain to determine linkage of the tetracycline marker to PR-39 resistance. An isogenic pair of tetracycline-resistant, PR-39-susceptible strains and of tetracycline-resistant, PR-39-resistant strains were saved by freezing them in 10% dimethyl sulfoxide at −70°C. Linkage to the same Tetr marker was also determined for the additional 20 mutants.
(ii) Identification of insertion points.
Transposon insertion points were identified using arbitrarily primed PCRs in two steps. In the first reaction, transposon-specific primers were mixed with arbitrary primers consisting of a defined part and a variable part. An initial denaturation step of 5 min at 95°C was followed by five cycles of 30 s at 95°C, 30 s at 30°C, and 1 min at 72°C and then by another 30 cycles of 30 s at 95°C, 30 s at 55°C, and 1 min at 72°C. The last elongation step was prolonged to 6 min. A second nested PCR was performed using 1 μl of the first reaction mixture as a template. After 5 min of denaturation at 95°C, 29 cycles of 30 s at 95°C, 30 s at 54°C, and 1 min at 72°C were run, with the last elongation extended to 6 min. The resulting PCR fragments were purified and sequenced using a primer with homology to the transposon (universal primer) (Table 2). To identify the resistance mutations, genes in the vicinity of the transposon insertion were PCR amplified and sequenced with primers that were designed based on publicly available genome sequences of S. enterica serovar Typhimurium.
Construction of an sbmA deletion mutant.
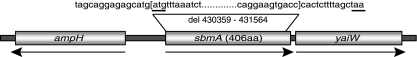
The chromosomal sbmA gene was inactivated using linear transformation as described previously (10). In brief, a kanamycin resistance cassette was amplified by PCR from plasmid pKD4 by using primers with homology to both the cassette and the sbmA gene. The deletion was constructed in a strain carrying plasmid pKD46, which encodes the phage lambda Red recombination system, and was subsequently moved to a wild-type background by transduction. To avoid polar effects on downstream genes, the kanamycin cassette was removed using pCP20-encoded Flp targeting Flp recombination sites within the cassette, leaving an 85-nucleotide scar (7, 10). The deletion was confirmed by colony PCR and sequencing. For exact deletion start and end points, see Fig. 1.
FIG. 1.
Schematic representation of the sbmA region. Transcription directions are indicated by arrows. The sequence deleted in strain DA12088 is indicated above the gene. Start and stop codons are underlined. The region is not drawn to scale. aa, amino acids.
Cloning and complementation of sbmA.
The wild-type sbmA gene (bp 430314 to 431602) was PCR amplified using a forward primer carrying an EcoRI restriction enzyme site and a reverse primer containing an XbaI site. The PCR fragment was restriction digested and cloned into plasmid pBAD30 (Ampr) under the control of an arabinose-inducible promoter (23). The plasmid was transformed into chemically competent E. coli TOP10 cells (Invitrogen, Stockholm, Sweden), and transformants were selected on LA plates supplemented with ampicillin. The plasmid was purified, sequenced, and electroporated into DA6192 (wild type), DA12088 (ΔsbmA), and DA10899 (sbmA Q179Stop). The strains were grown to logarithmic phase in the presence of 0.1% arabinose (Sigma-Aldrich AB, Stockholm, Sweden) to induce the SbmA-expressing plasmid. MIC measurements were performed as described above, with the exception that arabinose was included in the medium. The wild-type parental strain and the original mutant strains were assayed in parallel as controls.
Survival in stationary phase.
The ability of the sbmA deletion strain to survive in stationary phase was determined by incubating five independent lineages of DA12088 in LB over an extended period of time without changing the medium. Each lineage was started by inoculating 1.5 ml LB with 105 bacterial cells. The tubes were incubated at 37°C for 32 days, and samples were removed and plated on LA at regular intervals. The percent rate of survival and the number of CFU after an overnight incubation were calculated and compared for each sampling time point. The wild-type strain was assayed in parallel for comparison.
RESULTS
Isolation and characterization of PR-39-resistant mutants.
To isolate PR-39-resistant mutants, several independent cultures of DA6192 were grown to stationary phase, and 10-μl drops with 106 CFU from each culture were spotted onto solid medium agar plates containing 3 μM PR-39. On average, 2 colonies appeared in each spot after an overnight incubation at 37°C, and 21 independent (i.e., from 21 independent cultures) colonies were purified and saved. These 21 mutants grew well on medium supplemented with 3 μM PR-39. To identify the mutation(s) responsible for PR-39 resistance, one of the mutants was infected with a P22 phage lysate grown on a mini-Tn10 pool prepared from wild-type bacteria. Tetracycline-resistant transductants were picked and screened for the loss of PR-39 resistance. A phage lysate of one tetracycline-resistant and PR-39-susceptible clone was backcrossed to the original mutant strain and to the other 20 PR-39-resistant mutants to determine the linkage of the Tetr marker to the PR-39 resistance-conferring mutation. The Tetr marker showed approximately 70% linkage to the PR-39 resistance in all strains, indicating that their mutations were located in the same area of the chromosome. By performing an arbitrarily primed PCR out from the transposon, followed by DNA sequencing of the amplified area, the transposon insertion point was identified to the gene yaiV. DNA sequencing of the genes in the vicinity of the transposon insertion revealed a mutation in the gene sbmA (GenBank accession no. NC_003197, region 430359.0.431579). The 1,221-bp sbmA gene of S. enterica serovar Typhimurium shows high sequence similarity to the E. coli sbmA gene, and orthologues have also been identified in several other gram-negative bacteria. SbmA is predicted to be a part of a transporter belonging to the ATP-binding-cassette superfamily of transport proteins (35, 46). When the sbmA gene from an additional nine mutants was sequenced, a set of different mutations was identified (Table 1). Five mutations were single nucleotide changes leading to an amino acid substitution (T375K, L379P, E287K, Y326C, and S251L), three were nonsense mutations (W373Stop, Q179Stop, and C67Stop), and two were short deletions (del bp 843 to 844, del bp 967).
Determination of the in vitro mutation rate to achieve resistance.
The rate of mutation to achieve PR-39 resistance was measured by using the median method of Lea and Coulson (32). Bacteria (106 CFU) were applied in 10-μl drops from 27 independent cultures of DA6192 on PR-39-supplemented agar plates. The number of colonies was scored the next day, and from the median number of colonies appearing in each spot (two) and the average number of bacterial cells applied (3.8 × 106 CFU), we calculated the mutation rate to be 0.4 × 10−6 per cell per generation. The amount of background growth in the spots was measured to verify that the mutations appeared in the overnight cultures and not after application of the cells to the selective plates. Areas of defined size with no visible colonies were removed and vortexed in PBS, and samples were plated for viable counts. The background growth after 24 h was significantly lower than the number of bacteria that had been applied in each spot (data not shown), indicating that no growth had occurred on the selection plates and that the resistant mutants preexisted in the original cultures.
Quantification of PR-39 resistance in the sbmA mutants.
The susceptibility to PR-39 was assayed by measuring MICs and by examining killing over time at different concentrations of PR-39. We observed a three- to fourfold increase in MIC values for the mutants compared to those for the wild type (Table 1). Apart from the increase in MIC, the mutants also had a much greater capacity to survive even higher concentrations of peptide (8 and 16 μM) and were able to recover to a much greater extent than the wild-type strain. In Fig. 2, we have plotted the time-kill kinetics (change in percentage of viable bacteria over time) of bacteria at different concentrations of PR-39 relative to those of a control without peptide. In the controls, the bacteria increased about 8-fold in 4 h and 10-fold in 24 h (from 5 × 106 CFU/ml at the start of the experiment to 1.2 × 109 and 5 × 109 CFU/ml at 4 and 24 h, respectively). As can be seen, at the higher concentrations of peptide (4, 8, and 16 μM) after 24 h of incubation, the sbmA mutants showed 4- to 8-log-higher rates of survival than the wild-type parental strain.
FIG. 2.
Killing curves for PR-39-resistant mutants at the following concentrations of PR-39: 2 μM (A), 4 μM (B), 8 μM (C), and 16 μM (D). Bacteria were subjected to the peptide, and the numbers of viable cells were measured at different time points. The curves represent the change in percentage of viable bacteria over time relative to that of a control without peptide. Filled diamonds, wild type; open circles, DA10899 (Q179Stop); open triangles, DA12088 (ΔsbmA).
Inactivation of the SbmA protein causes PR-39 resistance.
Strain DA12088, in which sbmA was deleted by linear transformation, displayed the same MIC, resistance pattern, and fitness as the PR-39-resistant mutants isolated on agar plates containing PR-39 (Tables 1, 3, and 4; Fig. 2, 3, and 4). To verify that loss of the SbmA protein was responsible for the observed PR-39 resistance, the wild-type sbmA gene was cloned in an arabinose-inducible expression vector and used to transform the wild-type strain to DA12088 (ΔsbmA) and to DA10899 (sbmA Q179Stop). Induction of the SbmA protein returned the MICs of the mutants to levels comparable to those of the wild-type bacterium (Table 1), confirming the association of sbmA with the resistance phenotype. Furthermore, overproduction of SbmA in the wild-type strain resulted in a small reduction of the MIC (1.5 μM compared to 3 μM in these specific experiments), indicating that SbmA overproduction slightly increases PR-39 susceptibility.
TABLE 3.
CIs and relative fitnesses of PR-39-resistant strains in LB, M9 medium, and mice
| Strains | CIa
|
Relative fitnessc
|
||||||
|---|---|---|---|---|---|---|---|---|
| LB | M9 medium + glycerol | Miceb
|
LB | M9 medium + glycerol | Miceb
|
|||
| Spleen | Liver | Spleen | Liver | |||||
| DA10898 | 0.96 | 0.43 | ND | ND | 1.00 | 0.99 | ND | ND |
| DA10899 | 2.48 | 1.02 | 5.08 | 4.47 | 1.01 | 1.01 | 1.22 | 1.20 |
| DA10905 | 2.56 | 0.28 | 1.08 | 1.25 | 1.01 | 0.99 | 1.01 | 1.03 |
| DA10914 | 1.19 | 0.29 | 1.26 | 0.88 | 1.00 | 1.00 | 1.03 | 0.98 |
| DA12088 | 2.20 | 0.50 | 1.20 | 0.77 | 1.01 | 0.99 | 1.02 | 0.96 |
Measured after 130 generations of growth in laboratory media and after 10 generations of growth in mice (end point of experiments) as the number of mutant colonies divided by the number of wild-type colonies. For each in vitro competition experiment, the CI was measured at regular intervals and plotted against the number of generations of growth. A selection coefficient (s) was calculated from the following regression model: s = [lnR(t)/R(0)]/[t × ln(2)], where R is the CI and t equals the number of generations of growth. For the in vivo competitions, the equation used to calculate s was s = ln(CI)/10 ln(2).
ND, not determined.
Fitness of the wild-type parental strain was set to 1, and relative fitness of the mutants was calculated as 1 + smutant (the selection coefficient of each mutant).
TABLE 4.
Susceptibility of PR-39-resistant mutants to various antibiotics and AMPs
| Antibiotic or AMPb | MIC (μg/ml)a
|
||
|---|---|---|---|
| DA6192 | DA10899 | DA12088 | |
| Ampicillin | 0.75 | 0.75 | 0.75 |
| Cefepime | 0.064 | 0.064 | 0.064 |
| Cefpodoxime | 0.38 | 0.38 | 0.38 |
| Cefuroxime | 4 | 4 | 4 |
| Cephalothin | 3 | 3 | 3 |
| Chloramphenicol | 4 | 4 | 4 |
| Ciprofloxacin | 0.008 | 0.008 | 0.008 |
| Colistin | 0.5 | 0.5 | 0.5 |
| Kanamycin | 1.5 | 1.5 | 1.5 |
| Nalidixic acid | 4 | 4 | 4 |
| Nitrofurantoin | 8 | 8 | 8 |
| Streptomycin | 3 | 3 | 3 |
| Tetracycline | 3 | 3 | 3 |
| Bleomycin | 0.4 | 1.8 | 1.8 |
| CNY 100 H-L | 18 | 18 | 18 |
| CRAMP (mouse) | 32 | 32 | 32 |
| rCRAMP (rat) | 23 | 23 | 30 |
| LL-37 | 66 | 66 | 66 |
| Protamine sulfate | 31 | 31 | 31 |
| PR-39 | 8.5 | 28 | 28 |
MICs were determined by Etest.
MICs for bleomycin, CNY 100 H-L, CRAMP (mouse), rCRAMP, LL-37, and protamine sulfate were determined in liquid culture (Mueller-Hinton broth). MIC for PR-39 was determined in liquid culture (Iso-Sensitest broth).
FIG. 3.
Fitnesses of PR-39-resistant mutants measured as the growth rates in Iso-Sensitest medium relative to that of the wild-type parental strain. The error bars represent the standard errors of the mean.
FIG. 4.
Stationary-phase survival of a ΔsbmA strain compared to that of the parental strain. Five independent cultures of DA12088 and of DA6192 were incubated in LB at 37°C over an extended period of time and monitored for the numbers of viable cells at regular intervals. Relative survival was calculated as the average number of viable cells at each time point divided by the number of viable cells at the start of the experiment. Filled diamonds, DA6192 (wild type); open triangles, DA12088 (ΔsbmA).
Fitness of PR-39-resistant mutants.
For 10 of the resistant mutants, growth rates were measured at regular intervals over 16 h in Iso-Sensitest medium. All of the sbmA mutants, irrespective of the type of mutation, showed similar growth patterns. Compared to the wild type (fitness set to 1.0), no significant differences in fitness could be detected with this method (Fig. 3). The relative growth rates of the mutants ranged between 0.97 and 1.04. To obtain a more sensitive and accurate estimate of fitness, five of the mutants were competed against the wild-type strain at a 1:1 starting ratio in LB and M9 minimal medium with glycerol. The bacteria were grown for 130 generations (13 serial passages), and samples were taken at different time points to determine the ratio of mutant to wild-type bacteria. The CI was calculated for each time point and plotted against the number of generations of growth. From these curves, a selection coefficient (s) could be estimated for each strain by using the regression model described in Materials and Methods. No substantial differences in fitness between mutants and the wild type could be detected from competitions in LB and M9 medium. The CIs remained relatively constant over the course of the experiment, resulting in small s values ranging between −0.004 and 0.01 in LB and between −0.006 and 0.005 in M9 medium-glycerol. The fitness of the wild type was set to 1, and the relative fitness of each mutant was calculated as 1 + smutant and is presented in Table 3 together with the CI at the end of the experiment (after 130 generations of growth). The estimated growth rate differences between the mutants and the wild type were less than 1% for all strains in both media.
In a more natural environment, the genes affecting fitness could be very different from those in an in vitro situation. Therefore, we studied the fitness of four of the sbmA mutants in a mouse infection model. Equal numbers of mutant and wild-type bacteria were mixed and inoculated intraperitoneally into four mice. After 3 days, bacteria were harvested from the spleens and livers of the mice and plated on LA and LA-kanamycin plates to determine the number of mutants versus the number of wild-type bacteria. For DA12088 (ΔsbmA), DA10905 (S251L), and DA10914 (L379P), no differences in fitness could be observed (Table 3). In contrast, strain DA10899 (sbmA Q179Stop) showed a significant advantage in the competition with the wild-type strain. The s value was estimated to be 0.22 in the spleen and 0.20 in the liver, resulting in a fitness of about 1.2 relative to that of the wild-type strain (Table 3).
We further examined whether deletion of sbmA affected the ability of DA12088 to survive in stationary phase. Five independent lineages of DA12088 and of DA6192 were started in LB. The decline in the number of viable bacteria was monitored over time by plating samples on LA and by comparing the number of survivors to the initial number of viable cells in each culture. The fractions of viable bacteria remaining at different time points are plotted in Fig. 4. The survival curve of DA12088 was indistinguishable from that of the wild-type strain. The number of viable cells decreased to about 0.1% of the original population in 32 days.
Resistance of sbmA mutants to antibiotics and other peptides.
Susceptibility to commonly used antibiotics and to the glycopeptide colistin was investigated using Etests, and the susceptibilities to the antibiotic bleomycin and the membrane-active peptides protamine sulfate, CNY 100 H-L, LL-37, rCRAMP, and extended-form CRAMP were assayed in Mueller-Hinton broth with increasing concentrations of the peptides. These peptides were chosen to represent different classes of AMPs. LL-37 is a cathelicidin peptide isolated from humans, and CRAMP and rCRAMP are cathelicidins found in mice and rats, respectively (15, 18, 49). Protamine sulfate from salmon sperm is a cationic peptide with activity against several bacteria, and CNY 100 H-L is a synthetic variant of the C3a-derived peptide CNY-21 (30, 38). The only significant difference in resistance found was to bleomycin, for which the MIC of the PR-39-resistant mutants was 1.8 μg/ml compared to 0.4 μg/ml for the wild-type strain (Table 4). No cross-resistance to the other tested antibiotics or peptides was observed, indicating that the resistance mechanism does not confer resistance to lytic peptides or any of the common classes of antibiotics (Table 4).
DISCUSSION
AMPs generally kill rapidly and have a broad spectrum of activity, and in addition, there are few reports of emerging bacterial resistance toward these molecules, making them promising leads for new pharmaceuticals. The rarity of reported emergence of AMP resistance has led several researchers to speculate that it will be very difficult for bacteria to develop resistance to these peptides. In this study, we were able to isolate spontaneous, independent mutants of S. enterica serovar Typhimurium with increased levels of resistance to the AMP PR-39 simply by plating bacteria on agar plates containing peptide. These mutants appeared rapidly, and the mutation rate to PR-39 resistance was calculated to be approximately 10−6 per cell and generation, which is in fact a higher mutation rate to resistance than for many conventional antibiotics. The mutants showed a three- to fourfold increase in MIC but were also able to survive and recover from treatment with much higher concentrations of peptide.
All 21 of the isolated mutants had mutations in the same area of the chromosome, as determined by cotransduction of a tetracycline marker and the PR-39 resistance mutation. The exact locations of the mutations were determined for 10 mutants. All 10 mutations were found to be at different sites in the gene sbmA, which encodes a putative transporter protein, and included amino acid substitutions, small deletions, and nonsense mutations.
The resistant mutants had similar MICs and growth patterns, regardless of the type of mutation. These characteristics were also similar to those seen in the ΔsbmA strain, DA12088, indicating that all the mutations resulted in near or complete loss of function of the gene. Upon reintroduction of sbmA into DA12088 and DA10899 via a plasmid vector, the MIC was reduced to wild-type levels again, establishing the connection between SbmA and the resistance phenotype. When SbmA was overexpressed in the wild-type strain, the MIC decreased about twofold, further indicating that SbmA expression sensitizes the cell to PR-39. In a recent study of E. coli by Mattiuzzo et al., an amino acid substitution in SbmA, E276K, was found to be responsible for reduced susceptibility to Bac7 and other proline-rich peptides, including PR-39 (35). By using fluorescently labeled peptides, this group showed that the peptide concentration in the mutant bacteria was much lower than in the parental strain. Given the high sequence similarity between S. enterica serovar Typhimurium and E. coli, it is likely that reduced uptake of peptide is the mechanism behind the observed resistance in S. enterica serovar Typhimurium as well. We further examined cross-resistance of the PR-39-resistant mutants to a number of antibiotics and a set of lytic AMPs and found the resistance pattern to be nearly identical to that of the wild-type strain except for sensitivity to bleomycin, for which the MIC increased about fivefold in the mutants. SbmA-associated resistance to bleomycin has been observed earlier (52), and other studies have demonstrated that mutations in sbmA confer resistance to several additional proline-rich peptides and to the microcins 25 and B17 (35, 46), which were not included in this study.
Surprisingly, since antibiotic resistance is often associated with a negative effect on fitness (2, 33, 39), the sbmA mutants were, neither in vitro nor in vivo, negatively affected in growth compared to the wild-type parental strain. Furthermore, mutations in sbmA had no negative effect on long-term survival (1 month) of Salmonella in stationary phase. In fact, we observed only one significant fitness parameter that is altered by an sbmA mutation. One particular mutant strain, DA10899 (Q179Stop), out-competed the wild-type strain during the competition experiment with mice. This observation is somewhat difficult to account for, since no competitive advantage was observed for strains DA12088, DA10905, and DA10914. Possible explanations for these differences are that the kanamycin cassette used to inactivate sbmA in DA12088 affected the expression of the downstream gene yaiW (even though the cassette was eliminated to avoid polar effects) and that the point mutations in DA10905 and DA10914 did not fully inactivate the SbmA protein. Since ATP binding cassette transport systems can be involved in the uptake and export of a wide variety of molecules (11), it is possible that inactivation of sbmA results in a survival advantage in DA10899 by increasing the resistance to bacterial growth suppressors present in mice, such as AMPs, so that the strains carrying missense mutations are still capable of transporting. In this study, we did not observe any cross-resistance of sbmA mutants to CRAMP, an AMP found in mice. However, it is still possible that the mutants are resistant under different environmental conditions than those tested or that they are less susceptible to other antimicrobial molecules encountered in mice.
The lack of growth defects in the resistant strains is a worrying finding since it suggests that AMP-resistant mutants might show fitness similar to that of a susceptible strain when growing in a host. Thus, as with antibiotic-resistant mutants, it is likely that AMP-resistant mutants without any reduction in fitness will appear more rapidly in a population and, most importantly, will be less likely to disappear in the absence of a selective pressure than resistant mutants that show a fitness reduction (4, 45, 50).
In conclusion, in contrast to what has been suggested (5, 25, 29, 54), this study demonstrates that S. enterica serovar Typhimurium can mutate at a high rate to achieve increased resistance to an AMP (PR-39) and that the particular resistance mechanism does not confer any measurable negative effects on bacterial fitness. Thus, resistance is a realistic threat to the efficacy of AMPs and, as with antibiotics, the potential risk of resistance development toward AMPs used for therapeutic purposes needs to be evaluated carefully by experiment.
Acknowledgments
We thank Martin Malmsten, Mats Andersson, and Birgitta Agerberth for generously providing CNY-100 H-L, PR-39, and CRAMP/rCRAMP, respectively.
This work was supported by grants from the Swedish Research Council, EU 6th FP, and Söderberg's Foundation to D.I.A.
Footnotes
Published ahead of print on 2 June 2008.
REFERENCES
- 1.Agerberth, B., J. Y. Lee, T. Bergman, M. Carlquist, H. G. Boman, V. Mutt, and H. Jornvall. 1991. Amino acid sequence of PR-39. Isolation from pig intestine of a new member of the family of proline-arginine-rich antibacterial peptides. Eur. J. Biochem. 202:849-854. [DOI] [PubMed] [Google Scholar]
- 2.Andersson, D. I., and B. R. Levin. 1999. The biological cost of antibiotic resistance. Curr. Opin. Microbiol. 2:489-493. [DOI] [PubMed] [Google Scholar]
- 3.Bergman, P., L. Johansson, H. Wan, A. Jones, R. L. Gallo, G. H. Gudmundsson, T. Hokfelt, A. B. Jonsson, and B. Agerberth. 2006. Induction of the antimicrobial peptide CRAMP in the blood-brain barrier and meninges after meningococcal infection. Infect. Immun. 74:6982-6991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Björkman, J., D. Hughes, and D. I. Andersson. 1998. Virulence of antibiotic-resistant Salmonella typhimurium. Proc. Natl. Acad. Sci. USA 95:3949-3953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boman, H. G. 2003. Antibacterial peptides: basic facts and emerging concepts. J. Intern. Med. 254:197-215. [DOI] [PubMed] [Google Scholar]
- 6.Boman, H. G., B. Agerberth, and A. Boman. 1993. Mechanisms of action on Escherichia coli of cecropin P1 and PR-39, two antibacterial peptides from pig intestine. Infect. Immun. 61:2978-2984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cherepanov, P. P., and W. Wackernagel. 1995. Gene disruption in Escherichia coli: TcR and KmR cassettes with the option of Flp-catalyzed excision of the antibiotic-resistance determinant. Gene 158:9-14. [DOI] [PubMed] [Google Scholar]
- 8.Chromek, M., Z. Slamova, P. Bergman, L. Kovacs, L. Podracka, I. Ehren, T. Hokfelt, G. H. Gudmundsson, R. L. Gallo, B. Agerberth, and A. Brauner. 2006. The antimicrobial peptide cathelicidin protects the urinary tract against invasive bacterial infection. Nat. Med. 12:636-641. [DOI] [PubMed] [Google Scholar]
- 9.Cotter, P. D., C. Hill, and R. P. Ross. 2005. Bacteriocins: developing innate immunity for food. Nat. Rev. Microbiol. 3:777-788. [DOI] [PubMed] [Google Scholar]
- 10.Datsenko, K. A., and B. L. Wanner. 2000. One-step inactivation of chromosomal genes in Escherichia coli K-12 using PCR products. Proc. Natl. Acad. Sci. USA 97:6640-6645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Davidson, A. L., and J. Chen. 2004. ATP-binding cassette transporters in bacteria. Annu. Rev. Biochem. 73:241-268. [DOI] [PubMed] [Google Scholar]
- 12.Dhawan, V. K., M. R. Yeaman, A. L. Cheung, E. Kim, P. M. Sullam, and A. S. Bayer. 1997. Phenotypic resistance to thrombin-induced platelet microbicidal protein in vitro is correlated with enhanced virulence in experimental endocarditis due to Staphylococcus aureus. Infect. Immun. 65:3293-3299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dykhuizen, D. E. 1990. Experimental studies of natural selection in bacteria. Annu. Rev. Ecol. Syst. 21:373-398. [Google Scholar]
- 14.Frick, I. M., P. Akesson, M. Rasmussen, A. Schmidtchen, and L. Bjorck. 2003. SIC, a secreted protein of Streptococcus pyogenes that inactivates antibacterial peptides. J. Biol. Chem. 278:16561-16566. [DOI] [PubMed] [Google Scholar]
- 15.Gallo, R. L., K. J. Kim, M. Bernfield, C. A. Kozak, M. Zanetti, L. Merluzzi, and R. Gennaro. 1997. Identification of CRAMP, a cathelin-related antimicrobial peptide expressed in the embryonic and adult mouse. J. Biol. Chem. 272:13088-13093. [DOI] [PubMed] [Google Scholar]
- 16.Gallo, R. L., M. Ono, T. Povsic, C. Page, E. Eriksson, M. Klagsbrun, and M. Bernfield. 1994. Syndecans, cell surface heparan sulfate proteoglycans, are induced by a proline-rich antimicrobial peptide from wounds. Proc. Natl. Acad. Sci. USA 91:11035-11039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ge, Y., D. L. MacDonald, K. J. Holroyd, C. Thornsberry, H. Wexler, and M. Zasloff. 1999. In vitro antibacterial properties of pexiganan, an analog of magainin. Antimicrob. Agents Chemother. 43:782-788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gudmundsson, G. H., B. Agerberth, J. Odeberg, T. Bergman, B. Olsson, and R. Salcedo. 1996. The human gene FALL39 and processing of the cathelin precursor to the antibacterial peptide LL-37 in granulocytes. Eur. J. Biochem. 238:325-332. [DOI] [PubMed] [Google Scholar]
- 19.Guina, T., E. C. Yi, H. Wang, M. Hackett, and S. I. Miller. 2000. A PhoP-regulated outer membrane protease of Salmonella enterica serovar Typhimurium promotes resistance to alpha-helical antimicrobial peptides. J. Bacteriol. 182:4077-4086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gunn, J. S., and S. I. Miller. 1996. PhoP-PhoQ activates transcription of pmrAB, encoding a two-component regulatory system involved in Salmonella typhimurium antimicrobial peptide resistance. J. Bacteriol. 178:6857-6864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gunn, J. S., S. S. Ryan, J. C. Van Velkinburgh, R. K. Ernst, and S. I. Miller. 2000. Genetic and functional analysis of a PmrA-PmrB-regulated locus necessary for lipopolysaccharide modification, antimicrobial peptide resistance, and oral virulence of Salmonella enterica serovar Typhimurium. Infect. Immun. 68:6139-6146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guo, L., K. B. Lim, C. M. Poduje, M. Daniel, J. S. Gunn, M. Hackett, and S. I. Miller. 1998. Lipid A acylation and bacterial resistance against vertebrate antimicrobial peptides. Cell 95:189-198. [DOI] [PubMed] [Google Scholar]
- 23.Guzman, L. M., D. Belin, M. J. Carson, and J. Beckwith. 1995. Tight regulation, modulation, and high-level expression by vectors containing the arabinose PBAD promoter. J. Bacteriol. 177:4121-4130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hancock, R. E., and H. G. Sahl. 2006. Antimicrobial and host-defense peptides as new anti-infective therapeutic strategies. Nat. Biotechnol. 24:1551-1557. [DOI] [PubMed] [Google Scholar]
- 25.Hilpert, K., R. Volkmer-Engert, T. Walter, and R. E. Hancock. 2005. High-throughput generation of small antibacterial peptides with improved activity. Nat. Biotechnol. 23:1008-1012. [DOI] [PubMed] [Google Scholar]
- 26.Hornef, M. W., M. J. Wick, M. Rhen, and S. Normark. 2002. Bacterial strategies for overcoming host innate and adaptive immune responses. Nat. Immunol. 3:1033-1040. [DOI] [PubMed] [Google Scholar]
- 27.Huang, H. J., C. R. Ross, and F. Blecha. 1997. Chemoattractant properties of PR-39, a neutrophil antibacterial peptide. J. Leukoc. Biol. 61:624-629. [DOI] [PubMed] [Google Scholar]
- 28.Islam, D., L. Bandholtz, J. Nilsson, H. Wigzell, B. Christensson, B. Agerberth, and G. Gudmundsson. 2001. Downregulation of bactericidal peptides in enteric infections: a novel immune escape mechanism with bacterial DNA as a potential regulator. Nat. Med. 7:180-185. [DOI] [PubMed] [Google Scholar]
- 29.Jenssen, H., P. Hamill, and R. E. Hancock. 2006. Peptide antimicrobial agents. Clin. Microbiol. Rev. 19:491-511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Johansen, C., A. Verheul, L. Gram, T. Gill, and T. Abee. 1997. Protamine-induced permeabilization of cell envelopes of gram-positive and gram-negative bacteria. Appl. Environ. Microbiol. 63:1155-1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kristian, S. A., X. Lauth, V. Nizet, F. Goetz, B. Neumeister, A. Peschel, and R. Landmann. 2003. Alanylation of teichoic acids protects Staphylococcus aureus against Toll-like receptor 2-dependent host defense in a mouse tissue cage infection model. J. Infect. Dis. 188:414-423. [DOI] [PubMed] [Google Scholar]
- 32.Lea, D. E., and C. A. Coulson. 1949. The distribution of the numbers of mutants in bacterial populations. J. Genetics 49:264-285. [DOI] [PubMed] [Google Scholar]
- 33.Macvanin, M., J. Bjorkman, S. Eriksson, M. Rhen, D. I. Andersson, and D. Hughes. 2003. Fusidic acid-resistant mutants of Salmonella enterica serovar Typhimurium with low fitness in vivo are defective in RpoS induction. Antimicrob. Agents Chemother. 47:3743-3749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Marr, A. K., W. J. Gooderham, and R. E. Hancock. 2006. Antibacterial peptides for therapeutic use: obstacles and realistic outlook. Curr. Opin. Pharmacol. 6:468-472. [DOI] [PubMed] [Google Scholar]
- 35.Mattiuzzo, M., A. Bandiera, R. Gennaro, M. Benincasa, S. Pacor, N. Antcheva, and M. Scocchi. 2007. Role of the Escherichia coli SbmA in the antimicrobial activity of proline-rich peptides. Mol. Microbiol. 66:151-163. [DOI] [PubMed] [Google Scholar]
- 36.Nilsson, A. I., E. Kugelberg, O. G. Berg, and D. I. Andersson. 2004. Experimental adaptation of Salmonella typhimurium to mice. Genetics 168:1119-1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nizet, V., T. Ohtake, X. Lauth, J. Trowbridge, J. Rudisill, R. A. Dorschner, V. Pestonjamasp, J. Piraino, K. Huttner, and R. L. Gallo. 2001. Innate antimicrobial peptide protects the skin from invasive bacterial infection. Nature 414:454-457. [DOI] [PubMed] [Google Scholar]
- 38.Nordahl, E. A., V. Rydengard, P. Nyberg, D. P. Nitsche, M. Morgelin, M. Malmsten, L. Bjorck, and A. Schmidtchen. 2004. Activation of the complement system generates antibacterial peptides. Proc. Natl. Acad. Sci. USA 101:16879-16884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Paulander, W., S. Maisnier-Patin, and D. I. Andersson. 2007. Multiple mechanisms to ameliorate the fitness burden of mupirocin resistance in Salmonella typhimurium. Mol. Microbiol. 64:1038-1048. [DOI] [PubMed] [Google Scholar]
- 40.Perron, G. G., M. Zasloff, and G. Bell. 2006. Experimental evolution of resistance to an antimicrobial peptide. Proc. Biol. Sci. 273:251-256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Peschel, A. 2002. How do bacteria resist human antimicrobial peptides? Trends Microbiol. 10:179-186. [DOI] [PubMed] [Google Scholar]
- 42.Peschel, A., R. W. Jack, M. Otto, L. V. Collins, P. Staubitz, G. Nicholson, H. Kalbacher, W. F. Nieuwenhuizen, G. Jung, A. Tarkowski, K. P. van Kessel, and J. A. van Strijp. 2001. Staphylococcus aureus resistance to human defensins and evasion of neutrophil killing via the novel virulence factor MprF is based on modification of membrane lipids with l-lysine. J. Exp. Med. 193:1067-1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Peschel, A., M. Otto, R. W. Jack, H. Kalbacher, G. Jung, and F. Gotz. 1999. Inactivation of the dlt operon in Staphylococcus aureus confers sensitivity to defensins, protegrins, and other antimicrobial peptides. J. Biol. Chem. 274:8405-8410. [DOI] [PubMed] [Google Scholar]
- 44.Powers, J. P., and R. E. Hancock. 2003. The relationship between peptide structure and antibacterial activity. Peptides 24:1681-1691. [DOI] [PubMed] [Google Scholar]
- 45.Ramadhan, A. A., and E. Hegedus. 2005. Survivability of vancomycin resistant enterococci and fitness cost of vancomycin resistance acquisition. J. Clin. Pathol. 58:744-746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Salomón, R. A., and R. N. Farias. 1995. The peptide antibiotic microcin 25 is imported through the TonB pathway and the SbmA protein. J. Bacteriol. 177:3323-3325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shafer, W. M., X. Qu, A. J. Waring, and R. I. Lehrer. 1998. Modulation of Neisseria gonorrhoeae susceptibility to vertebrate antibacterial peptides due to a member of the resistance/nodulation/division efflux pump family. Proc. Natl. Acad. Sci. USA 95:1829-1833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shi, J., C. R. Ross, M. M. Chengappa, M. J. Sylte, D. S. McVey, and F. Blecha. 1996. Antibacterial activity of a synthetic peptide (PR-26) derived from PR-39, a proline-arginine-rich neutrophil antimicrobial peptide. Antimicrob. Agents Chemother. 40:115-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Termén, S., M. Tollin, B. Olsson, T. Svenberg, B. Agerberth, and G. H. Gudmundsson. 2003. Phylogeny, processing and expression of the rat cathelicidin rCRAMP: a model for innate antimicrobial peptides. Cell Mol. Life Sci. 60:536-549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wichelhaus, T. A., B. Boddinghaus, S. Besier, V. Schafer, V. Brade, and A. Ludwig. 2002. Biological cost of rifampin resistance from the perspective of Staphylococcus aureus. Antimicrob. Agents Chemother. 46:3381-3385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wu, T., M. R. Yeaman, and A. S. Bayer. 1994. In vitro resistance to platelet microbicidal protein correlates with endocarditis source among bacteremic staphylococcal and streptococcal isolates. Antimicrob. Agents Chemother. 38:729-732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yorgey, P., J. Lee, J. Kordel, E. Vivas, P. Warner, D. Jebaratnam, and R. Kolter. 1994. Posttranslational modifications in microcin B17 define an additional class of DNA gyrase inhibitor. Proc. Natl. Acad. Sci. USA 91:4519-4523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zaiou, M., and R. L. Gallo. 2002. Cathelicidins, essential gene-encoded mammalian antibiotics. J. Mol. Med. 80:549-561. [DOI] [PubMed] [Google Scholar]
- 54.Zasloff, M. 2002. Antimicrobial peptides of multicellular organisms. Nature 415:389-395. [DOI] [PubMed] [Google Scholar]
- 55.Zhang, G., C. R. Ross, S. S. Dritz, J. C. Nietfeld, and F. Blecha. 1997. Salmonella infection increases porcine antibacterial peptide concentrations in serum. Clin. Diagn. Lab. Immunol. 4:774-777. [DOI] [PMC free article] [PubMed] [Google Scholar]