Abstract
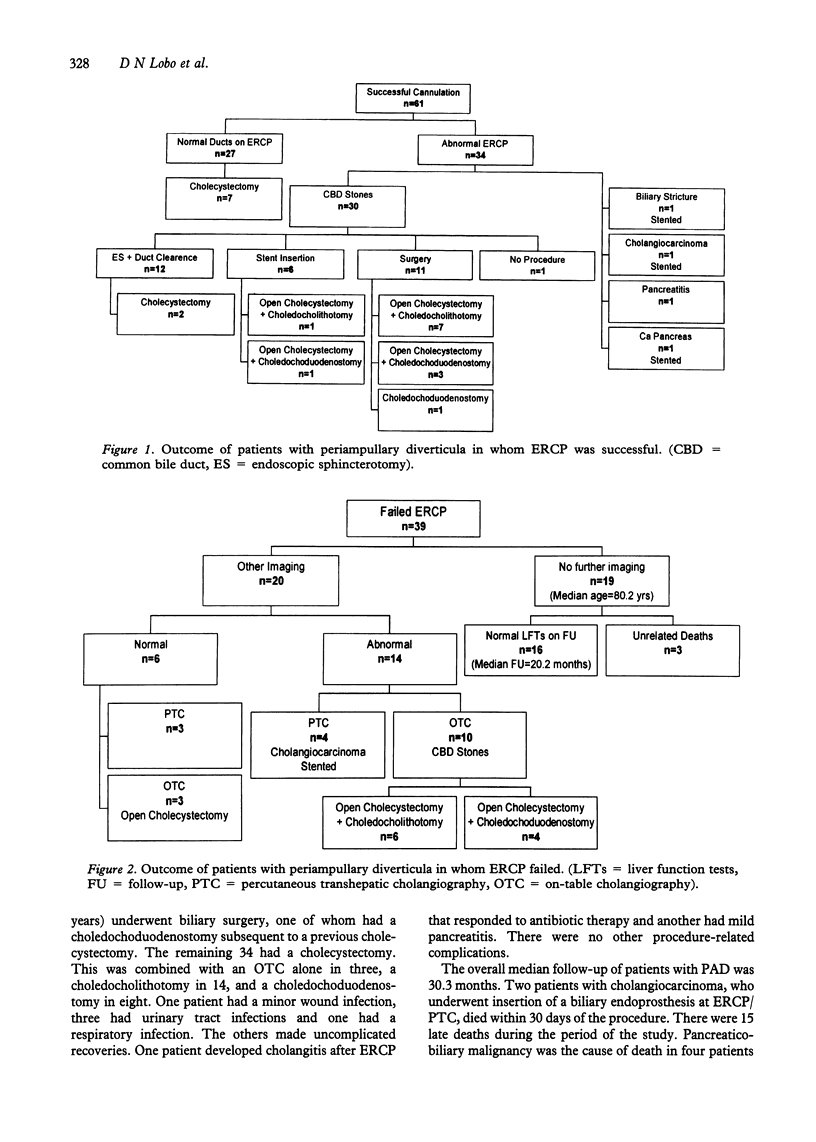
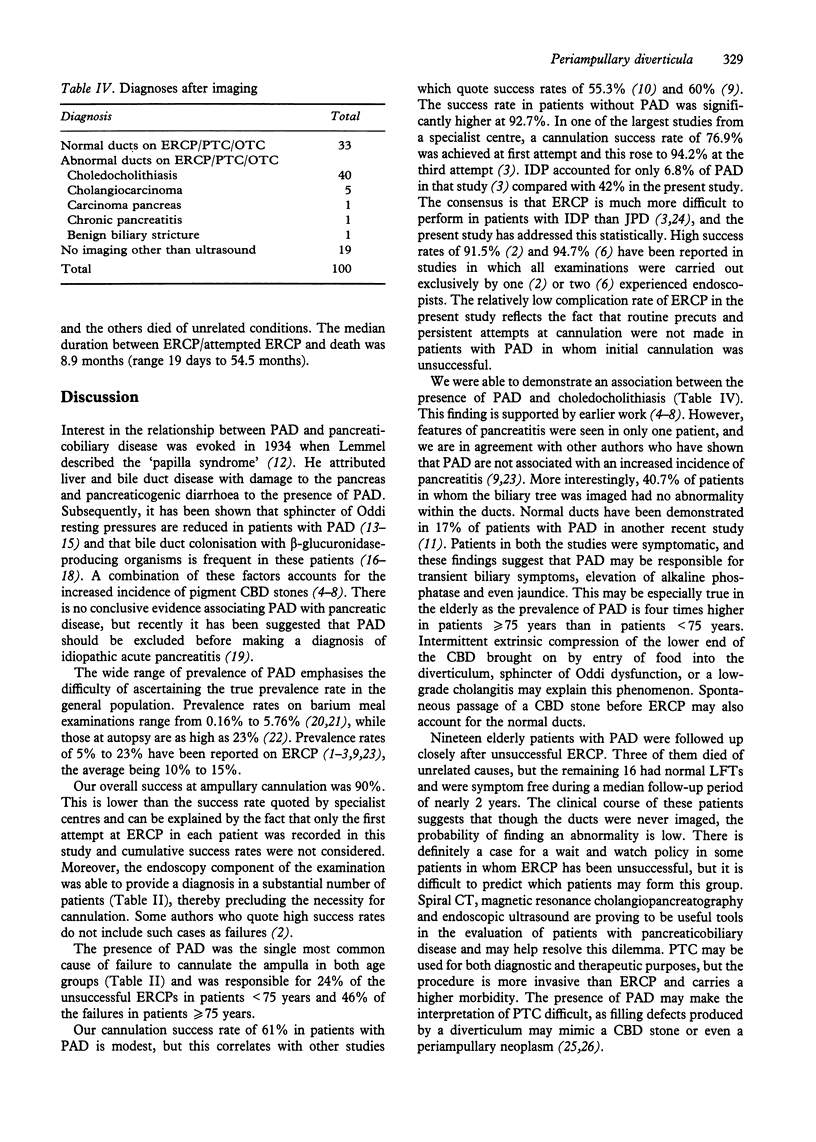
Periampullary diverticula (PAD) are associated with biliary disease and contribute to failure of endoscopic retrograde cholangiopancreatography (ERCP), especially in elderly patients. The presence of PAD and causes of failure to cannulate the ampulla were noted in 1211 consecutive patients undergoing ERCP. Case notes of 100 consecutive patients with PAD were reviewed retrospectively. Overall prevalence of PAD was 9%. Prevalence was higher in patients > or = 75 years when compared with those < 75 years (19.2% vs 4.8%, P < 0.0001). Ampullary cannulation was successful in 62.4% of patients with PAD and 92.7% without PAD (P < 0.0001). Success rates were lower in patients with intradiverticular papillae than in those with juxtapapillary diverticula (38.1% vs 77.6%; P < 0.0001). Of 19 patients with PAD who did not have any imaging other than ultrasound, 16 were asymptomatic over a median follow-up of 20 months. Biliary surgery was performed on 35 patients, with no major complication. PAD are a major cause of failed ERCP. Failure rates are higher in patients with intradiverticular papillae than juxtapapillary diverticula. Though a large proportion of patients not imaged remain asymptomatic on follow-up, it is difficult to predict which patients may form this group. Surgery, when indicated, is safe and effective in elderly patients in whom ERCP has failed.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bellamy P. R. The mucosal rosette: a peri-ampullary pseudotumour within a duodenal diverticulum. Clin Radiol. 1993 Feb;47(2):117–118. doi: 10.1016/s0009-9260(05)81185-7. [DOI] [PubMed] [Google Scholar]
- CHITAMBAR I. A., SPRINGS C. Duodenal diverticula. Surgery. 1953 May;33(5):768–791. [PubMed] [Google Scholar]
- Chang-Chien C. S. Do juxtapapillary diverticula of the duodenum interfere with cannulation at endoscopic retrograde cholangiopancreatography? A prospective study. Gastrointest Endosc. 1987 Aug;33(4):298–300. doi: 10.1016/s0016-5107(87)71602-2. [DOI] [PubMed] [Google Scholar]
- De Koster E., Denis P., Mante M., Otero J., Nyst J., Jonas C., Van Gossum M., De Reuck M., Deltenre M. Juxtapapillary duodenal diverticula: association with biliary stone disease. Acta Gastroenterol Belg. 1990 May-Jun;53(3):338–343. [PubMed] [Google Scholar]
- Dowsett J. F., Vaira D., Hatfield A. R., Cairns S. R., Polydorou A., Frost R., Croker J., Cotton P. B., Russell R. C., Mason R. R. Endoscopic biliary therapy using the combined percutaneous and endoscopic technique. Gastroenterology. 1989 Apr;96(4):1180–1186. doi: 10.1016/0016-5085(89)91639-9. [DOI] [PubMed] [Google Scholar]
- Hagège H., Berson A., Pelletier G., Fritsch J., Choury A., Liguory C., Etienne J. P. Association of juxtapapillary diverticula with choledocholithiasis but not with cholecystolithiasis. Endoscopy. 1992 May;24(4):248–251. doi: 10.1055/s-2007-1010476. [DOI] [PubMed] [Google Scholar]
- Hall R. I., Ingoldby C. J., Denyer M. E. Periampullary diverticula predispose to primary rather than secondary stones in the common bile duct. Endoscopy. 1990 May;22(3):127–128. doi: 10.1055/s-2007-1012817. [DOI] [PubMed] [Google Scholar]
- Hasan A. H., Moule B., Carter D. C. Duodenal diverticula and jaundice: percutaneous transhepatic cholangiography may be misleading. Br J Surg. 1988 May;75(5):490–491. doi: 10.1002/bjs.1800750529. [DOI] [PubMed] [Google Scholar]
- Kimura W., Nagai H., Kuroda A., Muto T. No significant correlation between histologic changes of the papilla of Vater and juxtapapillary diverticulum. Special reference to the pathogenesis of gallstones. Scand J Gastroenterol. 1992 Nov;27(11):951–956. doi: 10.3109/00365529209000169. [DOI] [PubMed] [Google Scholar]
- Kirk A. P., Summerfield J. A. Incidence and significance of juxtapapillary diverticula at endoscopic retrograde cholangiopancreatography. Digestion. 1980;20(1):31–35. doi: 10.1159/000198411. [DOI] [PubMed] [Google Scholar]
- Leivonen M. K., Halttunen J. A., Kivilaakso E. O. Duodenal diverticulum at endoscopic retrograde cholangiopancreatography, analysis of 123 patients. Hepatogastroenterology. 1996 Jul-Aug;43(10):961–966. [PubMed] [Google Scholar]
- Lintott D. J., Ruddell W. S., Axon A. T. Pseudostone at ERCP due to juxtapapillary diverticulum. Clin Radiol. 1981 Mar;32(2):173–176. doi: 10.1016/s0009-9260(81)80154-7. [DOI] [PubMed] [Google Scholar]
- Løtveit T., Osnes M., Aune S., Larsen S. Studies of the choledocho-duodenal sphincter in patients with and without juxta-papillary duodenal diverticula. Scand J Gastroenterol. 1980;15(7):875–880. doi: 10.3109/00365528009181545. [DOI] [PubMed] [Google Scholar]
- Løtveit T., Skar V., Osnes M. Juxtapapillary duodenal diverticula. Endoscopy. 1988 Aug;20 (Suppl 1):175–178. doi: 10.1055/s-2007-1018171. [DOI] [PubMed] [Google Scholar]
- Miyazaki S., Sakamoto T., Miyata M., Yamasaki Y., Yamasaki H., Kuwata K. Function of the sphincter of Oddi in patients with juxtapapillary duodenal diverticula: evaluation by intraoperative biliary manometry under a duodenal pressure load. World J Surg. 1995 Mar-Apr;19(2):307–312. doi: 10.1007/BF00308647. [DOI] [PubMed] [Google Scholar]
- Rankin F. W., Martin W. J. Diverticula of the Small Bowel. Ann Surg. 1934 Dec;100(6):1123–1135. doi: 10.1097/00000658-193412000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandstad O., Osnes T., Skar V., Urdal P., Osnes M. Common bile duct stones are mainly brown and associated with duodenal diverticula. Gut. 1994 Oct;35(10):1464–1467. doi: 10.1136/gut.35.10.1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shemesh E., Friedman E., Czerniak A., Bat L. The association of biliary and pancreatic anomalies with periampullary duodenal diverticula. Correlation with clinical presentations. Arch Surg. 1987 Sep;122(9):1055–1057. doi: 10.1001/archsurg.1987.01400210093014. [DOI] [PubMed] [Google Scholar]
- Sherman S., Hawes R. H., Lehman G. A. A new approach to performing endoscopic sphincterotomy in the setting of a juxtapapillary duodenal diverticulum. Gastrointest Endosc. 1991 May-Jun;37(3):353–355. doi: 10.1016/s0016-5107(91)70730-x. [DOI] [PubMed] [Google Scholar]
- Shinagawa N., Fukui T., Mashita K., Kitano Y., Yura J. The relationship between juxtapapillary duodenal diverticula and the presence of bacteria in the bile. Jpn J Surg. 1991 May;21(3):284–291. doi: 10.1007/BF02470948. [DOI] [PubMed] [Google Scholar]
- Siegel J. H., Cohen S. A., Kasmin F. E., Veerappan A. Stent-guided sphincterotomy. Gastrointest Endosc. 1994 Sep-Oct;40(5):567–572. doi: 10.1016/s0016-5107(94)70254-3. [DOI] [PubMed] [Google Scholar]
- Skar V., Løtveit T., Osnes M. Juxtapapillary duodenal diverticula predispose to common bile duct stones. Scand J Gastroenterol. 1989 Mar;24(2):202–204. doi: 10.3109/00365528909093037. [DOI] [PubMed] [Google Scholar]
- Skar V., Skar A. G., Bratlie J., Osnes M. Beta-glucuronidase activity in the bile of gallstone patients both with and without duodenal diverticula. Scand J Gastroenterol. 1989 Mar;24(2):205–212. doi: 10.3109/00365528909093038. [DOI] [PubMed] [Google Scholar]
- Skar V., Skar A. G., Osnes M. The duodenal bacterial flora in the region of papilla of Vater in patients with and without duodenal diverticula. Scand J Gastroenterol. 1989 Aug;24(6):649–656. doi: 10.3109/00365528909093104. [DOI] [PubMed] [Google Scholar]
- Tantau M., Person B., Burtin P., Boyer J. Duodenal diverticula and ERCP: a new trick. Endoscopy. 1996 Mar;28(3):326–326. doi: 10.1055/s-2007-1005468. [DOI] [PubMed] [Google Scholar]
- Targarona E. M., Ayuso R. M., Bordas J. M., Ros E., Pros I., Martínez J., Terés J., Trías M. Randomised trial of endoscopic sphincterotomy with gallbladder left in situ versus open surgery for common bileduct calculi in high-risk patients. Lancet. 1996 Apr 6;347(9006):926–929. doi: 10.1016/s0140-6736(96)91413-0. [DOI] [PubMed] [Google Scholar]
- Tierney S., Lillemoe K. D., Pitt H. A. The current management of common duct stones. Adv Surg. 1995;28:271–299. [PubMed] [Google Scholar]
- Uomo G., Manes G., Ragozzino A., Cavallera A., Rabitti P. G. Periampullary extraluminal duodenal diverticula and acute pancreatitis: an underestimated etiological association. Am J Gastroenterol. 1996 Jun;91(6):1186–1188. [PubMed] [Google Scholar]
- Vaira D., Dowsett J. F., Hatfield A. R., Cairns S. R., Polydorou A. A., Cotton P. B., Salmon P. R., Russell R. C. Is duodenal diverticulum a risk factor for sphincterotomy? Gut. 1989 Jul;30(7):939–942. doi: 10.1136/gut.30.7.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viceconte G., Viceconte G. W., Bogliolo G. Endoscopic manometry of the sphincter of Oddi in patients with and without juxtapapillary duodenal diverticula. Scand J Gastroenterol. 1984 May;19(3):329–333. [PubMed] [Google Scholar]


