Abstract
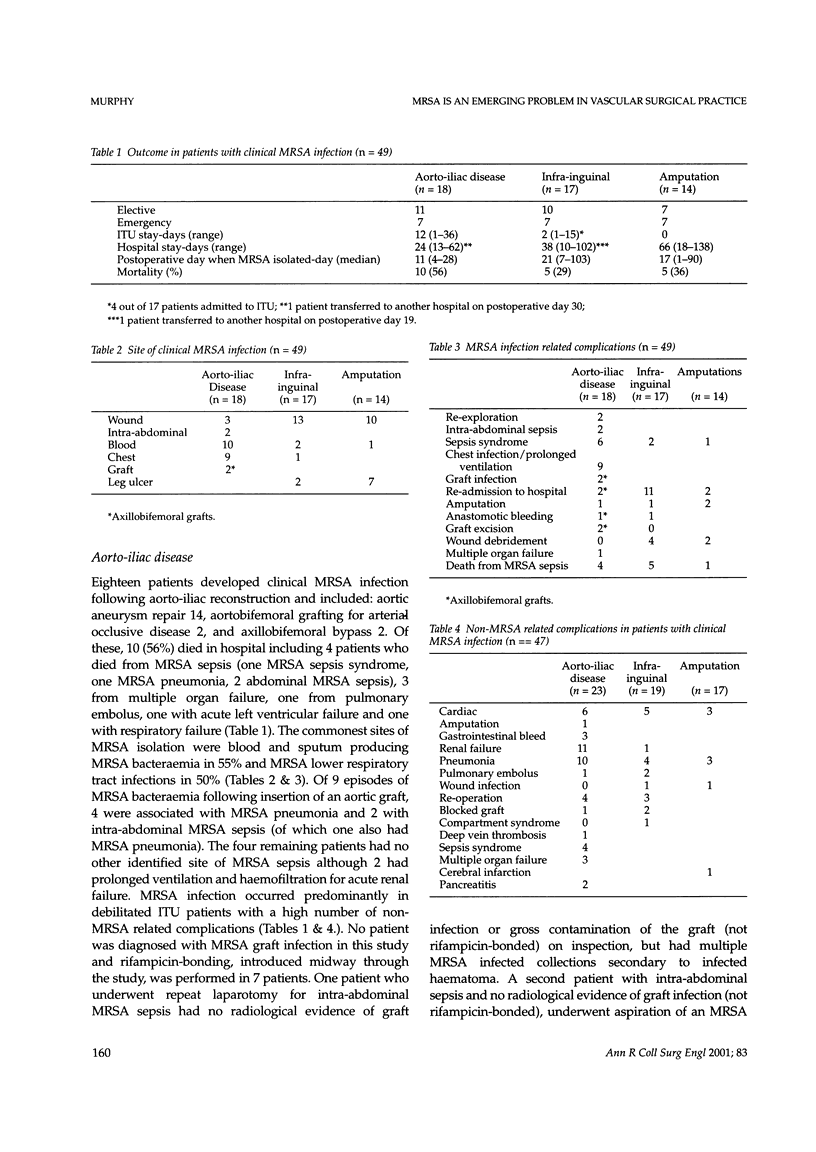
BACKGROUND: Methicillin-resistant Staphylococcus aureus (MRSA) infection is emerging as a major problem in vascular surgical practice. The aim of this study was to review the management of patients with MRSA infection complicating vascular surgical operations. METHODS: Data were obtained from the vascular audit, case notes, intensive therapy unit (ITU) notes, high dependency unit (HDU) notes and microbiological records of patients who underwent either arterial reconstruction (n = 464) or limb amputation (n = 110) between April 1994 and October 1998. RESULTS: Forty-nine vascular surgical patients developed clinical MRSA infection (9%). Clinical MRSA infection in patients who had undergone aorto-iliac reconstruction (n = 18) was associated with a 56% mortality (n = 10) and the most common infections were bacteraemia (55%) and pneumonia (50%). MRSA infection occurred in 17 patients who had undergone infra-inguinal bypass and was associated with a 29% mortality (n = 5). The most common site of MRSA infection was the groin wound (76%) leading to anastomotic dehiscence and death in one patient (11%) and necessitating wound debridement in 4 patients (22%). MRSA infection of the groin wound in the presence of a prosthetic graft (n = 3) led to anastomotic dehiscence in 2 patients, and graft excision in 2 patients. Similar complications were not observed in the presence of an underlying autogeneous long saphenous vein graft (n = 16). MRSA infection following major lower limb amputation (n = 14) was associated with death in 5 patients (36%). Wound infection in 10 amputees (71%) led to revision of the amputation to a higher level in 2 (14%) and wound debridement in 2 (14%). CONCLUSIONS: MRSA infection has a high mortality in vascular surgical patients in general, and following aorto-iliac reconstruction in particular. Autogeneous vein may confer some protection against local complications following groin wound infection. Strategies aimed at reducing the incidence of infection, including strict adherence to infection control procedures, may reduce the severity of this problem.
Full text
PDF




Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Asensio A., Guerrero A., Quereda C., Lizán M., Martinez-Ferrer M. Colonization and infection with methicillin-resistant Staphylococcus aureus: associated factors and eradication. Infect Control Hosp Epidemiol. 1996 Jan;17(1):20–28. doi: 10.1086/647184. [DOI] [PubMed] [Google Scholar]
- Braithwaite B. D., Davies B., Heather B. P., Earnshaw J. J. Early results of a randomized trial of rifampicin-bonded Dacron grafts for extra-anatomic vascular reconstruction. Joint Vascular Research Group. Br J Surg. 1998 Oct;85(10):1378–1381. doi: 10.1046/j.1365-2168.1998.00878.x. [DOI] [PubMed] [Google Scholar]
- Chalmers R. T., Wolfe J. H., Cheshire N. J., Stansby G., Nicolaides A. N., Mansfield A. O., Barrett S. P. Improved management of infrainguinal bypass graft infection with methicillin-resistant Staphylococcus aureus. Br J Surg. 1999 Nov;86(11):1433–1436. doi: 10.1046/j.1365-2168.1999.01267.x. [DOI] [PubMed] [Google Scholar]
- Chang F. Y., Singh N., Gayowski T., Drenning S. D., Wagener M. M., Marino I. R. Staphylococcus aureus nasal colonization and association with infections in liver transplant recipients. Transplantation. 1998 May 15;65(9):1169–1172. doi: 10.1097/00007890-199805150-00004. [DOI] [PubMed] [Google Scholar]
- Cheong I., Samsudin L. M., Law G. H. Methicillin-resistant Staphylococcus aureus bacteraemia at a tertiary teaching hospital. Br J Clin Pract. 1996 Jul-Aug;50(5):237–239. [PubMed] [Google Scholar]
- D'Addato M., Curti T., Freyrie A. The rifampicin-bonded gelseal graft. Eur J Vasc Endovasc Surg. 1997 Dec;14 (Suppl A):15–17. doi: 10.1016/s1078-5884(97)80146-3. [DOI] [PubMed] [Google Scholar]
- Edwards W. H., Jr, Martin R. S., 3rd, Jenkins J. M., Edwards W. H., Sr, Mulherin J. L., Jr Primary graft infections. J Vasc Surg. 1987 Sep;6(3):235–239. [PubMed] [Google Scholar]
- Fletcher J. P., Dryden M., Sorrell T. C. Infection of vascular prostheses. Aust N Z J Surg. 1991 Jun;61(6):432–435. doi: 10.1111/j.1445-2197.1991.tb00257.x. [DOI] [PubMed] [Google Scholar]
- Fukatsu K., Saito H., Matsuda T., Ikeda S., Furukawa S., Muto T. Influences of type and duration of antimicrobial prophylaxis on an outbreak of methicillin-resistant Staphylococcus aureus and on the incidence of wound infection. Arch Surg. 1997 Dec;132(12):1320–1325. doi: 10.1001/archsurg.1997.01430360066012. [DOI] [PubMed] [Google Scholar]
- Hayes P. D., Nasim A., London N. J., Sayers R. D., Barrie W. W., Bell P. R., Naylor A. R. In situ replacement of infected aortic grafts with rifampicin-bonded prostheses: the Leicester experience (1992 to 1998) J Vasc Surg. 1999 Jul;30(1):92–98. doi: 10.1016/s0741-5214(99)70180-1. [DOI] [PubMed] [Google Scholar]
- Ishikawa S., Ohtaki A., Takahashi T., Sato Y., Koyano T., Hasegawa Y., Yamagishi T., Ogino T., Ohki S., Kamiyoshihara M. Management of postoperative fever in cardiovascular surgery. J Cardiovasc Surg (Torino) 1998 Feb;39(1):95–97. [PubMed] [Google Scholar]
- Jones L., Braithwaite B. D., Davies B., Heather B. P., Earnshaw J. J. Mechanism of late prosthetic vascular graft infection. Cardiovasc Surg. 1997 Oct;5(5):486–489. doi: 10.1016/s0967-2109(97)00056-2. [DOI] [PubMed] [Google Scholar]
- Lingnau W., Allerberger F. Control of an outbreak of methicillin-resistant Staphylococcus aureus (MRSA) by hygienic measures in a general intensive care unit. Infection. 1994;22 (Suppl 2):S135–S139. doi: 10.1007/BF01793578. [DOI] [PubMed] [Google Scholar]
- Marples R. R., Speller D. C., Cookson B. D. Prevalence of mupirocin resistance in Staphylococcus aureus. J Hosp Infect. 1995 Feb;29(2):153–155. doi: 10.1016/0195-6701(95)90197-3. [DOI] [PubMed] [Google Scholar]
- Martin M. A. Methicillin-resistant Staphylococcus aureus: the persistent resistant nosocomial pathogen. Curr Clin Top Infect Dis. 1994;14:170–191. [PubMed] [Google Scholar]
- Pick F. C., Rose M., Wang D., Gardner B. P., Gillett A. P. The prevention of spread of methicillin resistant Staphylococcus aureus in a spinal injuries centre. Paraplegia. 1994 Nov;32(11):732–735. doi: 10.1038/sc.1994.118. [DOI] [PubMed] [Google Scholar]
- Pujol M., Peña C., Pallares R., Ariza J., Ayats J., Dominguez M. A., Gudiol F. Nosocomial Staphylococcus aureus bacteremia among nasal carriers of methicillin-resistant and methicillin-susceptible strains. Am J Med. 1996 May;100(5):509–516. doi: 10.1016/s0002-9343(96)00014-9. [DOI] [PubMed] [Google Scholar]
- Revised guidelines for the control of methicillin-resistant Staphylococcus aureus infection in hospitals. British Society for Antimicrobial Chemotherapy, Hospital Infection Society and the Infection Control Nurses Association. J Hosp Infect. 1998 Aug;39(4):253–290. doi: 10.1016/s0195-6701(98)90293-6. [DOI] [PubMed] [Google Scholar]
- Romero-Vivas J., Rubio M., Fernandez C., Picazo J. J. Mortality associated with nosocomial bacteremia due to methicillin-resistant Staphylococcus aureus. Clin Infect Dis. 1995 Dec;21(6):1417–1423. doi: 10.1093/clinids/21.6.1417. [DOI] [PubMed] [Google Scholar]
- Santini C., Baiocchi P., Serra P. Perioperative antibiotic prophylaxis in vascular surgery. Eur J Vasc Endovasc Surg. 1997 Dec;14 (Suppl A):13–14. doi: 10.1016/s1078-5884(97)80145-1. [DOI] [PubMed] [Google Scholar]
- Shimada M., Kamakura T., Itasaka H., Matsumata T., Hashizume M., Sugimachi K. The significance of methicillin-resistant Staphylococcus aureus infection in general surgery: a multivariate analysis of risk factors and preventive approaches. Surg Today. 1993;23(10):880–884. doi: 10.1007/BF00311366. [DOI] [PubMed] [Google Scholar]
- Spartera C., Morettini G., Bafile G., Di Cesare E., Alagia G., Ventura M. Diagnostic imaging techniques in vascular graft infection. Eur J Vasc Endovasc Surg. 1997 Dec;14 (Suppl A):24–26. doi: 10.1016/s1078-5884(97)80148-7. [DOI] [PubMed] [Google Scholar]
- Speller D. C., Johnson A. P., James D., Marples R. R., Charlett A., George R. C. Resistance to methicillin and other antibiotics in isolates of Staphylococcus aureus from blood and cerebrospinal fluid, England and Wales, 1989-95. Lancet. 1997 Aug 2;350(9074):323–325. doi: 10.1016/s0140-6736(97)12148-1. [DOI] [PubMed] [Google Scholar]
- Torsello G., Sandmann W. Use of antibiotic-bonded grafts in vascular graft infection. Eur J Vasc Endovasc Surg. 1997 Dec;14 (Suppl A):84–87. doi: 10.1016/s1078-5884(97)80161-x. [DOI] [PubMed] [Google Scholar]
- Vandenbroucke-Grauls C. M., Frénay H. M., van Klingeren B., Savelkoul T. F., Verhoef J. Control of epidemic methicillin-resistant Staphylococcus aureus in a Dutch university hospital. Eur J Clin Microbiol Infect Dis. 1991 Jan;10(1):6–11. doi: 10.1007/BF01967090. [DOI] [PubMed] [Google Scholar]


