Abstract
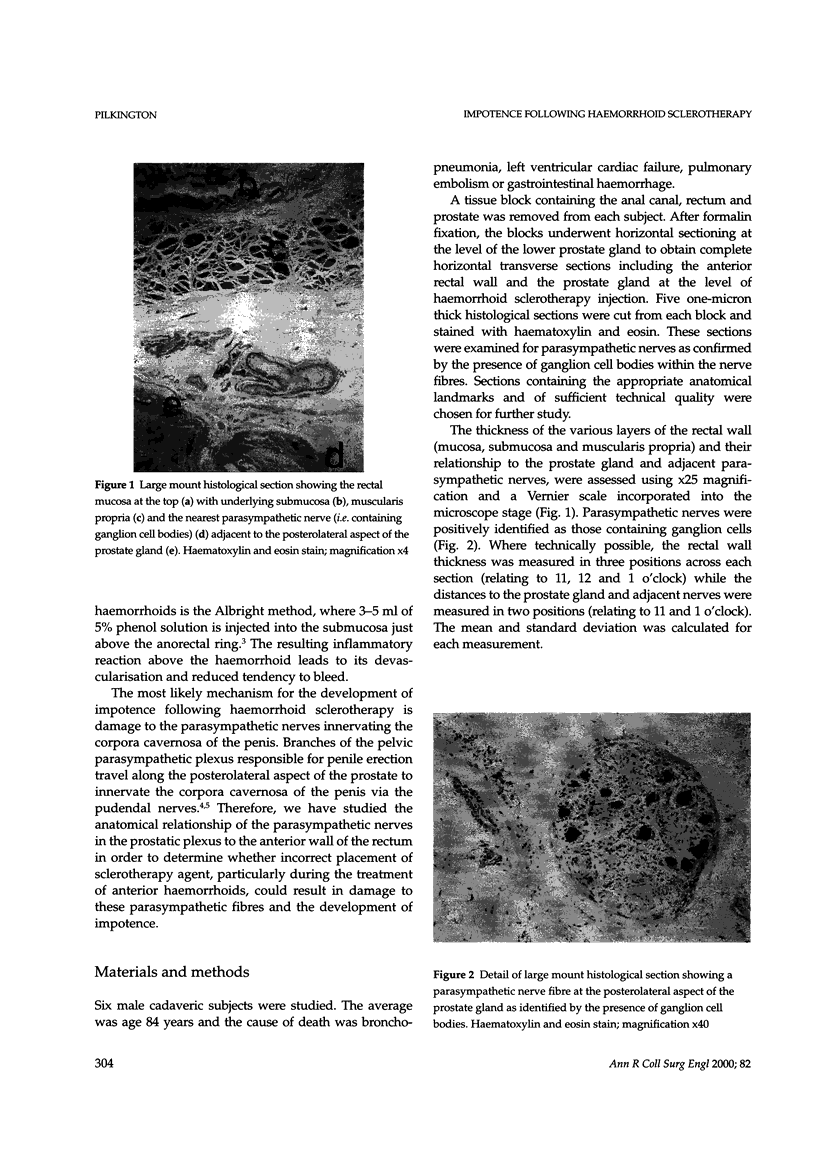
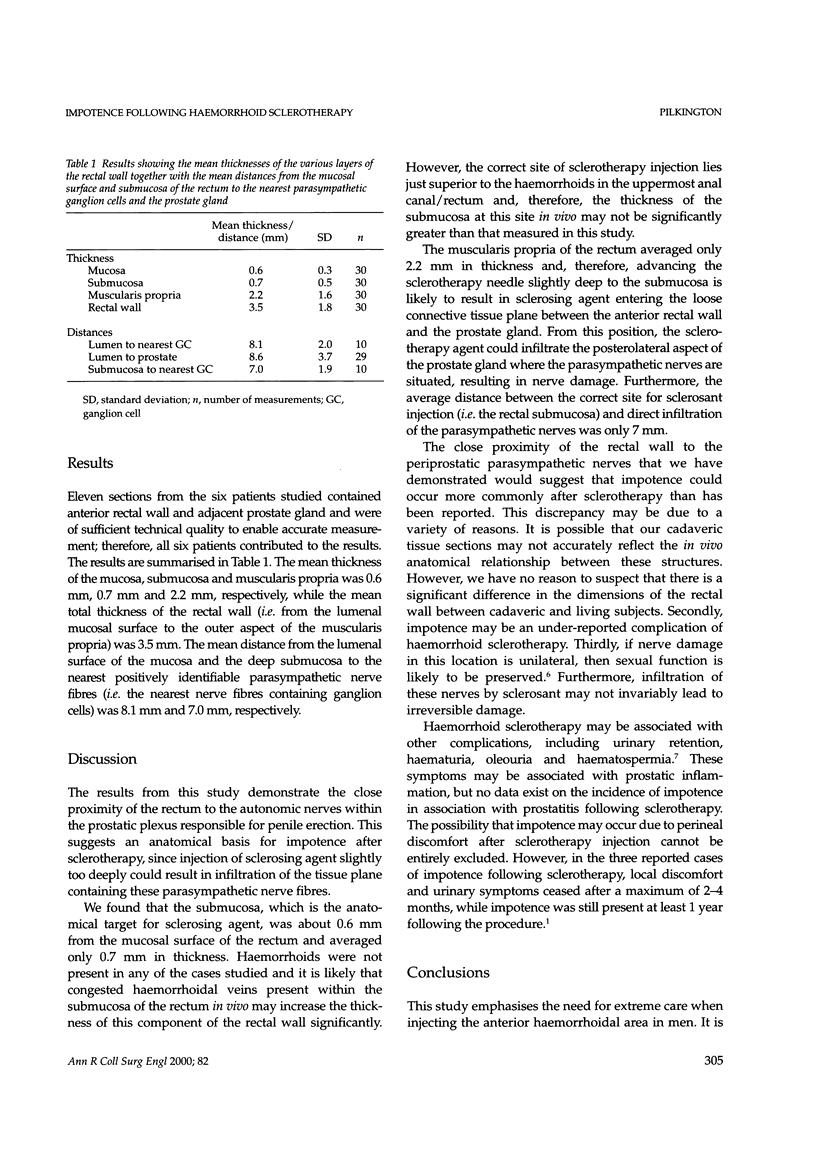
Impotence has been reported as a rare but important complication of sclerotherapy for haemorrhoids. The relationship between the anterior wall of the rectum and the periprostatic parasympathetic nerves responsible for penile erection was studied to investigate a potential anatomical explanation for this therapeutic complication. A tissue block containing the anal canal, rectum and prostate was removed from each of six male cadaveric subjects. The dimensions of the components of the rectal wall and the distance between the rectal lumen and parasympathetic nerves in the periprostatic plexus were measured in horizontal transverse histological sections of the tissue blocks at the level of the lower prostate gland (i.e. the correct level for sclerosant injection). The correct site of sclerosant in the submucosa was on average 0.6 mm (SD 0.3 mm) deep to the rectal mucosal surface and only 0.7 mm (SD 0.5 mm) in thickness. The nearest parasympathetic ganglion cells were a mean of only 8.1 mm (SD 2.0 mm) deep to the rectal lumen. The close proximity of the rectum to the periprostatic parasympathetic nerves defines an anatomical basis for impotence following sclerotherapy. This emphasises the need for all practitioners to be particularly careful when injecting in this area and for strict supervision of trainees.
Full text
PDF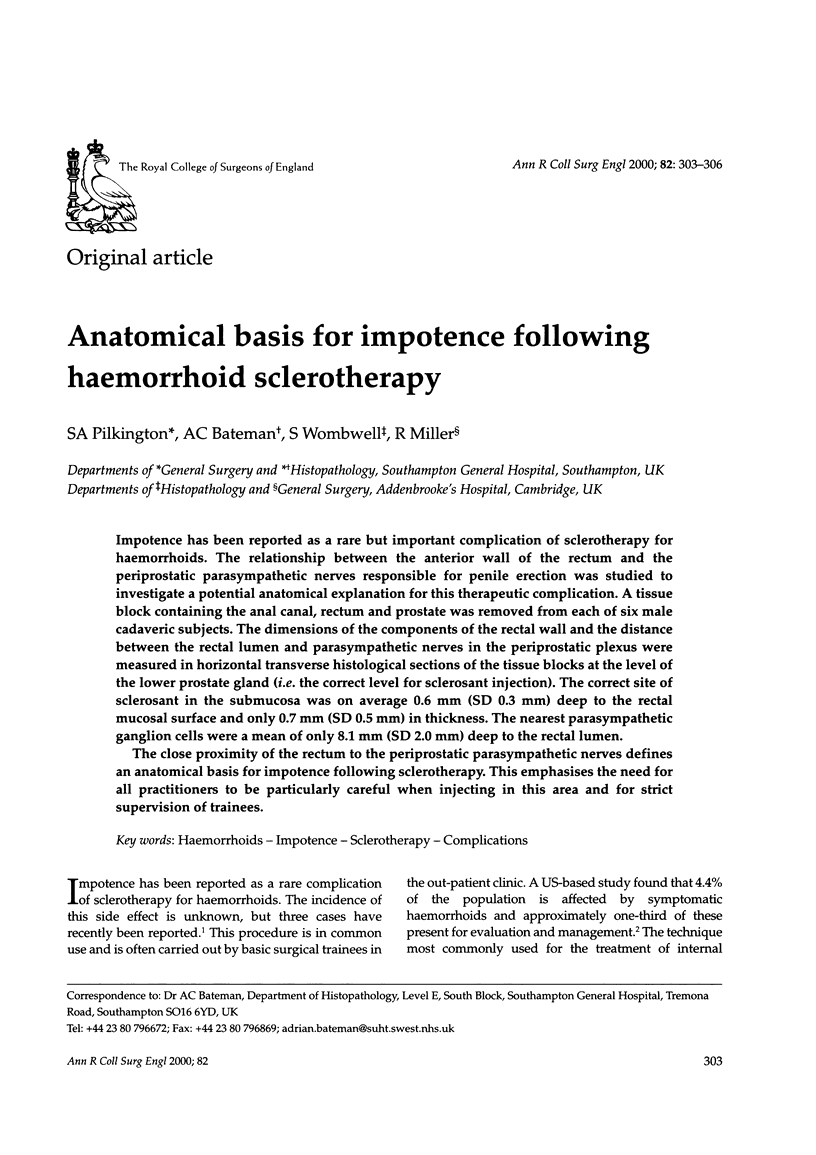

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bullock N. Impotence after sclerotherapy of haemorrhoids: case reports. BMJ. 1997 Feb 8;314(7078):419–419. doi: 10.1136/bmj.314.7078.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johanson J. F., Sonnenberg A. The prevalence of hemorrhoids and chronic constipation. An epidemiologic study. Gastroenterology. 1990 Feb;98(2):380–386. doi: 10.1016/0016-5085(90)90828-o. [DOI] [PubMed] [Google Scholar]
- Lepor H., Gregerman M., Crosby R., Mostofi F. K., Walsh P. C. Precise localization of the autonomic nerves from the pelvic plexus to the corpora cavernosa: a detailed anatomical study of the adult male pelvis. J Urol. 1985 Feb;133(2):207–212. doi: 10.1016/s0022-5347(17)48885-9. [DOI] [PubMed] [Google Scholar]
- Lue T. F., Zeineh S. J., Schmidt R. A., Tanagho E. A. Neuroanatomy of penile erection: its relevance to iatrogenic impotence. J Urol. 1984 Feb;131(2):273–280. doi: 10.1016/s0022-5347(17)50344-4. [DOI] [PubMed] [Google Scholar]
- WRIGHT A. D. Complications of rectal injections. Proc R Soc Med. 1950 Apr;43(4):263–266. [PMC free article] [PubMed] [Google Scholar]
- Walsh P. C., Schlegel P. N. Radical pelvic surgery with preservation of sexual function. Ann Surg. 1988 Oct;208(4):391–400. doi: 10.1097/00000658-198810000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]