Abstract
Although toxoplasmosis is considered harmless for a non-pregnant woman, it is potentially harmful during pregnancy, especially at first trimester. Τhe aim of this study is to increase our alertness and monitoring in case of toxoplasmosis during pregnancy, given that when diagnosed it can be effectively treated.
We present a case of a healthy 26 years old adult woman, found with toxoplasmosis during the 13th week of pregnancy. The role of frequent maternal and fetus immunological tests, PCR-tests of the amniotic fluid and ultrasound screening of the fetus throughout pregnancy was of great value. The patient was treated with spiramycin (1gr x 3) from the 16th week of pregnancy
The patient was subjected to cesarean delivery at the 36th week of pregnancy due to preterm contractions and history of previous cesarean delivery. The newborn was a healthy girl with a birth weight of 2880 gr. A two-year follow up of the baby revealed no medical condition.
Maternal infections are a serious medical condition during pregnancy. Toxoplasmosis when diagnosed on time and treated properly can lead to healthy offspring.
Keywords: toxoplasmosis, pregnancy, amniocentesis, cordocentesis
Toxoplasmosis is caused by a ubiquitous protozoan parasite, Toxoplasma gondii. It is generally a self-limited, asymptomatic disease in immunocompetent patients, although infection can reactivate at a later time if the patient becomes immunosuppressed. Primary maternal infection during pregnancy can be transmitted to the fetus and result in serious sequelae1.
Case report
A 26 years old female, attending our antenatal outpatients section, was found positive for toxoplasmosis, during the 13th week of pregnancy. She reported no other maternal medical conditions and the infection was confirmed during routine tests. This was her second pregnancy and she had a history of previous cesarean delivery. Her history was negative although she reported that she was taking care of a cat recently. All the other antenatal tests were normal.
The patient was admitted to our center. Physical examination during admission was normal. Her initial serologic tests were: IgG 249 IU/ml (normal range 0-6 IU/ml), IgG avidity 0.010% (normal range 0-0.2%), IgM >160 IU/ml (normal range 0-10 IU/ml). Tests were repeated and additionally IgA was measured. The new laboratory results were: IgG > 400 IU/ml, IgG avidity 4.4%, IgM 63 IU/ml and IgA 13 IU/ml. The finding of positive IgA and the gradual increase of IgG avidity confirmed the presence of a recent infection that happened during the last six weeks. In view of these findings an amniocentesis was conducted at 15 weeks in order to examine whether the fetus was affected. PCR-DNA test of the amniotic fluid was negative. Although there was no evidence of vertical transmission the infection was confirmed and the patient received treatment with spiramycin 1gr three times a day (t.i.d.).
Serologic tests were repeated during the 20th week: IgG 440 IU/ml, IgG avidity 23%, IgM 51 IU/ml and IgA negative. At this point a new amniocentesis was conducted and this time PCR-DNA test of the amniotic fluid was positive for the parasite. At 23 weeks of gestation a cordocentesis was operated and serologic tests results were: IgG 310 IU/ml, IgG avidity (considered to be of maternal origin since fetus cannot produce IgG) 16%, IgM and IgA negative. Fortunately fetal blood PCR did not reveal infection of the fetus. Serologic tests at 35 weeks of gestation were: IgG 84 IU/ml, IgM 17 IU/ml and IgA negative. Ultrasound examinations were performed monthly and no fetal abnormality was detected at any time point.
The patient suffered preterm contractions since the 35th week of pregnancy and finally was subjected to cesarean delivery at 36 weeks of pregnancy. The newborn was a healthy girl with a birth weight of 2880 gr. Serological tests of the child (blood sampling from umbilical cord) were: IgG 74 IU/ml, IgG avidity (considered of maternal origin because newborn also cannot produce IgG) 64%, IgM and IgA negative. Tests were repeated one month later with the same results.
Discussion
Prevalence
Seroprevalence rates of toxoplasmosis vary substantially among different countries (from approximately 15 percent in the United States to more than 50 percent in certain European countries). The incidence of maternal infection ranges from 1 to 8 per 1000 susceptible pregnancies, with the highest reported rates in France2. The risk of transmitting infection to the fetus increases steeply with the gestational age at seroconversion3. Women infected prior to conception do not transmit infection to the fetus, with the rare exception of immune compromised women (eg, AIDS, immunosuppressive medications). Among HIV-infected patients, seroprevalence of antibodies to Toxoplasma gondii is similar to the one reported in the general population4.
Pathogenesis
Toxoplasma gondii is an obligate intracellular parasite existing in three forms: the oocyst, shed only in cat feces, the tachyzoite (a rapidly dividing form observed in the acute phase of infection), and the bradyzoite (a slow growing form observed within tissue cysts). During a primary infection a cat can seed millions of oocysts daily for a period of one to three weeks. These oocysts may remain infectious for over a year1,5.
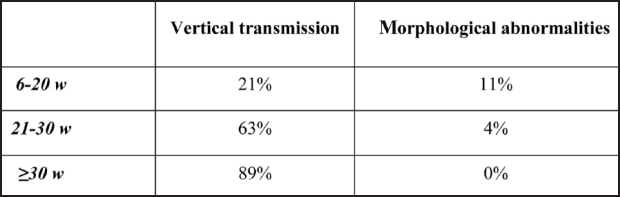
Maternal infection usually results from ingestion of oocysts shed into the environment or from ingestion of bradyzoites or tachyzoites contained in meat or meat products. Fetoplacental infection can occur immediately after maternal infection, possibly even before development of the maternal serologic response6,7. Although the risk of vertical transmission increases with increasing gestational age, frequency of death or morphological abnormalities of fetus decreases as shown in Table 1.
Table 1. Risk of vertical transmission and frequency of morphological abnormalities of fetus with increasing gestational age.
The risk of vertical transmission increases but the frequency of morphological abnormalities of fetus decreases as pregnancy progresses.
Clinical manifestations
Acute infection in adult humans goes unrecognized in as many as 90% of cases, because either it is subclinical or symptoms are nonspecific and it is falsely taken as a viral illness1,8. The most common manifestations are nontender lymphadenopathy, fatigue, headache, malaise and myalgia. The infection is usually self-limited and requires no treatment1. First trimester fetal infection on the other hand, often results in miscarriage, stillbirth, or severe sequelae in the newborn7. Most infants with congenital toxoplasmosis (70-90%) are asymptomatic or without apparent abnormalities at birth9, 10. Even though subclinical disease is the rule, signs present at birth may include fever, a maculopapular rash, hepatosplenomegaly, microcephaly, seizures, jaundice, thrombocytopenia, and rarely generalized lymphadenopathy. The so-called classic triad of congenital toxoplasmosis consists of chorioretinitis, hydrocephalus and intracranial calcifications5,10.
Diagnosis
Maternal infection. Serologic tests represent the most commonly used method to establish the diagnosis; documentation of recent seroconversion is the best evidence of recent infection. IgG antibodies appear within one to two weeks of infection, peak in six to eight weeks and then decline over the next two years; they remain detectable for life. IgM antibodies may appear within the first week of infection and generally decline within a few months; however, they sometimes persist for years after the initial infection. Thus, the presence of IgM antibodies should not be used to confirm a recent or acute infection.
Alternatively, anti-Toxoplasma gondii IgG antibodies in saliva provide a reliable estimation of the presence of infection11 even in immunodeficiency virus-infected patients12.
Fetal infection. When the disease is suspected, based upon maternal serology or fetal sonographic findings, fetal evaluation is required. Prenatal diagnosis of congenital toxoplasmosis is made by detection of the Toxoplasma gondii parasite in fetal blood or amniotic fluid or presence of Toxoplasma gondii IgM or IgA antibodies in fetal blood; however, polymerase chain reaction (PCR) testing is the preferred diagnostic modality13–15. Certain abnormalities on antenatal sonography are suggestive, but not diagnostic, of fetal infection16. They include intracranial densities, increased placental thickness and/or hyperdensity, ventricular dilatation, intrahepatic densities, hepatomegaly, ascites, pericardial and/or pleural effusion.
If pregnancy termination is requested on the basis of a positive result on PCR testing of amniotic fluid in the absence of sonographic findings, confirmation of the diagnosis by a second amniocentesis for PCR testing at a reference laboratory is required. The prenatal diagnosis of congenital toxoplasmosis is a complex problem, and should be conducted only in laboratories with proven highly sensitive and specific PCR technology17–19.
Newborn infection diagnosis. In symptomatic infants, the diagnosis of congenital toxoplasmosis is strongly suggested by history and physical examination. Ophthalmologic, auditory, and neurologic examinations, as well as lumbar puncture and computed tomography (CT) of the head, should be performed. Toxoplasmosis must be differentiated from the other TORCH (TOxoplasma – Rubella – Cytomegalovirus – Herpes) infections, which can have similar presentations in the newborn.
Many diagnostic tests are available, but results must be interpreted carefully. Toxoplasma gondii can be isolated from the placenta, umbilical cord, or infant blood by inoculation into mice or cell culture. PCR for Toxoplasma gondii on white blood cells, cerebrospinal fluid (CSF), and placenta are also available20. However, PCR testing for this pathogen has not been standardized19.
Serum from the newborn can also be tested for IgM and IgA antibodies. A number of different assays are applied, including immunofluorescence (IFA), enzyme linked immunosorbent assay (ELISA), and immunosorbent agglutination assay (ISAGA). IgM measurement appears to be more sensitive when conducted with ELISA and ISAGA than IFA. IgA antibody measurment may be more sensitive than IgM, but specificity is not assured. Most experts recommend a combination of serologic tests.
Prevention
Prevention of primary infection is based upon educating women on the modes of Toxoplasma gondii transmission and avoidance of risky behaviors. Fruits and vegetables should be washed before eating. Cutting boards, knives, and the sink and counters should be washed after food preparation. Consumption of raw eggs, unpasteurized milk, or unfiltered water should be avoided as well as tasting meat while it is cooking. Smoked or cured in brine meat is not safe. Meat should be cooked to 66℃ (152℉) or higher or frozen for a day in a household freezer; both these measures are lethal to tachyzoites and bradyzoites21,22. Mucous membrane contact when handling uncooked meat, shellfish, fruit, and vegetables should be avoided, and hands should be washed thoroughly afterward. Women with cats should have someone else change the litter box daily (fresh cat feces are not infectious). They should wear gloves if they are gardening or if they must change the litter themselves. Cats that live exclusively indoors and eat cooked food are not at risk of acquiring toxoplasmosis. Women should wash hands with soap and water after working with soil, after handling the cat or litter box, or after touching raw or undercooked meat.
Preconceptional counseling aimed at primary prevention of toxoplasmosis can reduce the seroconversion rate during pregnancy by 60 percent23. Whether all pregnant women should undergo serological screening for toxoplasmosis is controversial24. It is a routine practice in some areas of relatively high prevalence, such as France.
Treatment
Immunocompetent, nonpregnant patients generally do not require treatment unless symptoms are severe or prolonged beyond a few weeks. However, an acute infection based upon results of toxoplasma serology is generally treated immediately with the macrolide spiramycin (1 gr orally every eight hours without food). Spiramycin is concentrated in the placenta where it is thought to treat infection and thereby help to prevent transmission to the fetus25; however, the ability of this drug to reduce the incidence of vertical transmission is controversial26. Spiramycin does not cross the placenta well; thus, it is not effective for treatment of an infected fetus. For this reason, amniocentesis and PCR testing of amniotic fluid for Toxoplasma gondii at least four weeks after acute maternal infection in the second trimester, is recommended. If PCR results are negative, spiramycin is continued for the remainder of the pregnancy. If the PCR is positive, suggesting fetal infection, alternative agents are necessary.
Combination of pyrimethamine and sulfadiazine, both folic acid antagonists with synergistic action, are often used to reduce the severity of congenital infection and increase the proportion of infants asymptomatic at birth27,28. Therapeutic abortion is another option. However, neonatal outcome is often good for treated fetuses who do not have sonographic abnormalities such as hydrocephalus28,29. Both pyrimethamine and sulfadiazine can cause dose-related bone marrow suppression with resultant anemia, leucopenia and thrombocytopenia. They are teratogenic in animals in large doses30 and can cause reversible acute renal failure. Due to the potential toxicity of these drugs, their use during pregnancy is only warranted if fetal infection has been documented. There are no direct maternal benefits from these drugs. Various dosing regimens have been proposed31. More often a three week course of pyrimethamine (50 mg/day orally) and sulfadiazine (3 gr/day orally in 2 to 3 divided doses), alternating with a three week course of spiramycin (1 gr orally three times a day) is administered until delivery. Alternatively, pyrimethamine (25 mg /day orally) and sulfadiazine (4 gr/day orally in 2 to 4 divided doses) can be administered continuously until term. Leucovorin (folinic acid) (10 to 25 mg/day orally) is added during pyrimethamine and sulfadiazine administration to prevent bone marrow suppression. Monitoring of complete blood counts and platelet counts should be performed weekly and treatment discontinued if a significantly abnormal result is reported.
An effective alternative to spiramycin to prevent in utero infection with Toxoplasma gondii may be azithromycin28, a Category B drug used for treatment of Chlamydia trachomatis infections in pregnancy. Azithromycin has successfully treated Toxoplasma gondii in both an animal model and in humans with AIDS32,33. A combination of pyrimethamine (100 mg loading dose orally followed by 25 to 50 mg/day) plus azithromycin (500 mg once daily) may also be tried. In women intolerant to pyrimethamine, trimethoprim-sulfamethoxazole may be used34. However, the safety and efficacy of these drugs for treating in-utero toxoplasmosis infection are unknown.
Immunosuppressed pregnant women
Toxoplasma gondii infection in non-immune pregnant women could result not only from acquired infection but also from reactivation35,36. Immunocompetent persons with primary infection are usually asymptomatic, but latent infection can persist for life. In immunosuppressed patients, especially with the acquired immunodeficiency syndrome (AIDS), the parasite can reactivate and cause disease, usually when the CD4 lymphocyte count falls below 100 cells/µL37. All immunosuppressed patients should be screened for Toxoplasma gondii antibodies. Counseling on preventing toxoplasmosis should be given to seronegative and prophylaxis to seropositive patients. Routine serologic tests cannot distinguish active from latent infection38.
Pregnant women with a human immunodeficiency virus infection may be at increased risk of having positive Toxoplasma gondii antibodies39. Furthermore, in HIV positive pregnant women Toxoplasma gondii infection oftenly coexists with HCV and HBV infections and can cause serious complications leading to miscarriage, stillbirth, birth defects (mental retardation, blindness, and epilepsy) and favor or enhance the mother-to-child transmission of HCV, HBV, and HIV vertical transmission40. However, vertical transmission of Toxoplasma gondii from a chronically infected mother in the setting of HIV infection is not a common phenomenon among those without severe immunocompromise41,42.
The prenatal patient with newly diagnosed HIV infection should be tested for Toxoplasma gondii IgG antibodies. If positive for IgG antibodies, IgM antibodies should be obtained in an attempt to rule out acute infection. Patients who test negative do not require any further testing until after the pregnancy, unless they are severely immunocompromised and reveal signs and symptoms of toxoplasmosis43.
HIV-positive patients who have antibodies to Toxoplasma gondii should be considered at high risk for development of clinical disease. Reactivation of latent infection in the central nervous system (toxoplasma encephalitis) is a common HIV-related complication in these patients44. Typical presenting symptoms are headache, confusion, fever and focal neurologic deficits. Antitoxoplasma IgM antibodies are usually absent and quantitative IgG antibody titers are not helpful. The absence of antibodies to toxoplasma does not rule out the diagnosis. Neuroradiologic studies may be highly suggestive of toxoplasmic encephalitis, but the definitive diagnosis can be made only by biopsy and demonstration of toxoplasma in brain tissue45. However, due to high morbidity and even mortality associated with the procedure, it is common practice to presume diagnosis and treat immunosuppressed patients if the clinical suspicion is high. In patients with extracerebral toxoplasmosis, the demonstration of tachyzoites in tissue or fluid, such as bronchoalveolar lavage (BAL) fluid, is usually required to establish a definitive diagnosis.
Treatment regimens in immunosuppressed pregnant women do not vary from those administered in immunocompetent ones, with the difference that highly potent antiretroviral drugs for HIV infection (AZT, 3TC and nelfinavir) are also given.
However, in the presence of mother's clinical disease, three to four-fold higher doses are used. Most commonly a combination therapy of pyrimethamine (200 mg loading dose orally followed by 75 mg/day) and sulfadiazine (6 to 8 g/day PO in four divided doses) plus folinic acid to prevent drug-induced hematologic toxicity is administered. In patients intolerant to sulfadiazine, pyrimethamine could be combined with clindamycin (600 to 1200 mg IV or 450 mg orally four times a day) or azithromycin (1200 to 1500 mg orally once daily) or atovaquone (750 mg orally four times a day). Toxoplasmic encephalitis generally responds promptly to treatment. Extracerebral toxoplasmosis is treated with the same regimens as toxoplasmic encephalitis, although the response may not be as favorable. For patients who respond, the duration of therapy at the doses mentioned is typically six weeks. Afterwards, it is usually safe to decrease to a lower dose for secondary prophylaxis (chronic suppressive therapy).
Despite the concerns of the use of these high-dose combined therapies on the fetus during pregnancy, successful outcomes for both mother and child have been reported46.
References
- 1.Montoya G, Liesenfeld O. Toxoplasmosis. Lancet. 2004;363:1965–1976. doi: 10.1016/S0140-6736(04)16412-X. [DOI] [PubMed] [Google Scholar]
- 2.Gilbert RE, Peckham CS. Congenital toxoplasmosis in the United Kingdom: to screen or not to screen? J Med Screen. 2002;9:135–141. doi: 10.1136/jms.9.3.135. [DOI] [PubMed] [Google Scholar]
- 3.Thiebaut R, Leproust S, Chene G, Gilbert R. Effectiveness of prenatal treatment for congenital toxoplasmosis: a meta-analysis of individual patient's data. Lancet. 2007;369:115–122. doi: 10.1016/S0140-6736(07)60072-5. [DOI] [PubMed] [Google Scholar]
- 4.Falusi O, French A, Seaberg EC, et al. Prevalence and predictors of Toxoplasma seropositivity in women with and at risk for human immunodeficiency virus infection. Clin Infect Dis. 2002;35:1414–1417. doi: 10.1086/344462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hill D, Dubey P. Toxoplasma gondii: transmission, diagnosis and prevention. Clin Microbiol Infect. 2002;8:634–640. doi: 10.1046/j.1469-0691.2002.00485.x. [DOI] [PubMed] [Google Scholar]
- 6.Singh S. Mother-to-child transmission and diagnosis of toxoplasma gondii infection during pregnancy. Indian J Med Microbiol. 2003;21:69–76. [PubMed] [Google Scholar]
- 7.Kravetz J, Federman D. Toxoplasmosis in pregnancy. Am J Med. 2005;118:212–216. doi: 10.1016/j.amjmed.2004.08.023. [DOI] [PubMed] [Google Scholar]
- 8.Montoya J, Rosso F. Diagnosis and management of toxoplasmosis. Clin Perinatol. 2005;32:705–726. doi: 10.1016/j.clp.2005.04.011. [DOI] [PubMed] [Google Scholar]
- 9.Gratzl R, Hayde M, Kohlhauser C, et al. Follow-up of infants with congenital toxoplasmosis detected by polymerase chain reaction analysis of amniotic fluid. Eur J Clin Microbiol Infect Dis. 1998;17:853–858. doi: 10.1007/s100960050206. [DOI] [PubMed] [Google Scholar]
- 10.Berrebi A, Bardou M, Bessieres M, et al. Outcome for children infected with congenital toxoplasmosis in the first trimester and with normal ultrasound findings: A study of 36 cases. Eur J Obstet Gynecol Reprod Biol. 2007;135:53–57. doi: 10.1016/j.ejogrb.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 11.Stroehle A, Schmid K, Heinzer I, Naguleswaran A, Hemphill A. Performance of a Western immunoblot assay to detect specific anti-Toxoplasma gondii IgG antibodies in human saliva. J Parasitol. 2005;91:561–563. doi: 10.1645/GE-423R. [DOI] [PubMed] [Google Scholar]
- 12.Singh MP, Dubey ML, Sud A, Malla N. Antibody response to Toxoplasma gondii in saliva samples from human immunodeficiency virus-infected patients. Br J Biomed Sci. 2005;62:81–84. doi: 10.1080/09674845.2005.11732690. [DOI] [PubMed] [Google Scholar]
- 13.Foulon W, Pinon J, Stray-Pedersen B, et al. Prenatal diagnosis of congenital toxoplasmosis: a multicenter evaluation of different diagnostic parameters. Am J Obstet Gynecol. 1999;181:843–847. doi: 10.1016/s0002-9378(99)70311-x. [DOI] [PubMed] [Google Scholar]
- 14.Cazenave J, Forestier F, Bessieres M, Broussin B, Begueret J. Contribution of a new PCR assay to the prenatal diagnosis of congenital toxoplasmosis. Prenat Diagn. 1992;12:119–127. doi: 10.1002/pd.1970120207. [DOI] [PubMed] [Google Scholar]
- 15.Hohlfeld P, Daffos F, Costa JM, Thulliez P, Forestier F, Vidaud M. Prenatal diagnosis of congenital toxoplasmosis with a polymerase-chain-reaction test on amniotic fluid. N Engl J Med. 1994;331:695–699. doi: 10.1056/NEJM199409153311102. [DOI] [PubMed] [Google Scholar]
- 16.Hohlfeld P, MacAleese J, Capella-Pavlovski M, et al. Fetal toxoplasmosis: ultrasonographic signs. Ultrasound Obstet Gynecol. 1991;1:241–244. doi: 10.1046/j.1469-0705.1991.01040241.x. [DOI] [PubMed] [Google Scholar]
- 17.Noordhoek G, van Embden J, Kolk A. Reliability of nucleic acid amplification for detection of Mycobacterium tuberculosis: an international collaborative quality control study among 30 laboratories. J Clin Microbiol. 1996;34:2522–2525. doi: 10.1128/jcm.34.10.2522-2525.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guy E, Pelloux H, Lappalainen M, et al. Interlaboratory comparison of polymerase chain reaction for the detection of Toxoplasma gondii DNA added to samples of amniotic fluid. Eur J Clin Microbiol Infect Dis. 1996;15:836–839. doi: 10.1007/BF01701532. [DOI] [PubMed] [Google Scholar]
- 19.Pelloux H, Guy E, Angelici MC, et al. A second European collaborative study on polymerase chain reaction for Toxoplasma gondii, involving 15 teams. FEMS Microbiol Lett. 1998;165:231–237. doi: 10.1111/j.1574-6968.1998.tb13151.x. [DOI] [PubMed] [Google Scholar]
- 20.Boyer K. Diagnostic testing for congenital toxoplasmosis. Pediatr Infect Dis J. 2001;20:59–60. doi: 10.1097/00006454-200101000-00011. [DOI] [PubMed] [Google Scholar]
- 21.Warnekulasuriya MR, Johnson JD, Holliman RE. Detection of Toxoplasma gondii in cured meats. Int J Food Microbiol. 1998;45:211–215. doi: 10.1016/s0168-1605(98)00158-5. [DOI] [PubMed] [Google Scholar]
- 22.Cook A, Gilbert R, Buffolano W, et al. Sources of toxoplasma infection in pregnant women: European multicentre case-control study. European Research Network on Congenital Toxoplasmosis. BMJ. 2000;321:142–147. doi: 10.1136/bmj.321.7254.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Foulon W, Naessens A, Derde M. Evaluation of the possibilities for preventing congenital toxoplasmosis. Am J Perinatol. 1994;11:57–62. doi: 10.1055/s-2007-994537. [DOI] [PubMed] [Google Scholar]
- 24.Boyer K, Holfels E, Roizen N, et al. Risk factors for Toxoplasma gondii infection in mothers of infants with congenital toxoplasmosis: Implications for prenatal management and screening. Am J Obstet Gynecol. 2005;192:564–571. doi: 10.1016/j.ajog.2004.07.031. [DOI] [PubMed] [Google Scholar]
- 25.Couvreur J, Desmonts G, Thulliez P. Prophylaxis of congenital toxoplasmosis. Effects of spiramycin on placental infection. J Antimicrob Chemother. 1988;(Suppl B):193–200. doi: 10.1093/jac/22.supplement_b.193. [DOI] [PubMed] [Google Scholar]
- 26.Wallon M, Liou C, Garner P, Peyron F. Congenital toxoplasmosis: systematic review of evidence of efficacy of treatment in pregnancy. BMJ. 1999;318:1511–1514. doi: 10.1136/bmj.318.7197.1511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Daffos F, Forestier F, Capella-Pavlovsky M, et al. Prenatal management of 746 pregnancies at risk for congenital toxoplasmosis. N Engl J Med. 1988;318:271–275. doi: 10.1056/NEJM198802043180502. [DOI] [PubMed] [Google Scholar]
- 28.Hohlfeld P, Daffos F, Thulliez P, et al. Fetal toxoplasmosis: outcome of pregnancy and infant follow-up after in utero treatment. J Pediatr. 1989;115:765–769. doi: 10.1016/s0022-3476(89)80660-2. [DOI] [PubMed] [Google Scholar]
- 29.Berrebi A, Kobuch W, Bessieres M, et al. Termination of pregnancy for maternal toxoplasmosis. Lancet. 1994;344:36–39. doi: 10.1016/s0140-6736(94)91054-5. [DOI] [PubMed] [Google Scholar]
- 30.McCabe RE, Oster S. Current recommendations and future prospects in the treatment of toxoplasmosis. Drugs. 1989;38:973–987. doi: 10.2165/00003495-198938060-00008. [DOI] [PubMed] [Google Scholar]
- 31.Georgiev V. Management of toxoplasmosis. Drugs. 1994;48:179–188. doi: 10.2165/00003495-199448020-00005. [DOI] [PubMed] [Google Scholar]
- 32.Araujo FG, Guptill DR, Remington JS. Azithromycin, a macrolide antibiotic with potent activity against Toxoplasma gondii. Antimicrob Agents Chemother. 1988;32:755–757. doi: 10.1128/aac.32.5.755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Godofsky E. Treatment of presumed cerebral toxoplasmosis with azithromycin. N Engl J Med. 1994;330:575–576. doi: 10.1056/nejm199402243300817. [DOI] [PubMed] [Google Scholar]
- 34.Derouin F, Jacqz-Aigrain E, Thulliez P, Couvreur J, Leport C. Cotrimoxazole for prenatal treatment of congenital toxoplasmosis? Parasitol Today. 2000;16:254–256. doi: 10.1016/s0169-4758(00)01667-7. [DOI] [PubMed] [Google Scholar]
- 35.Biedermann K, Flepp M, Fierz W, Joller-Jemelka H, Kleihues P. Pregnancy, immunosuppression and reactivation of latent toxoplasmosis. J Perinat Med. 1995;23:191–203. doi: 10.1515/jpme.1995.23.3.191. [DOI] [PubMed] [Google Scholar]
- 36.Bachmeyer C, Mouchnino G, Thulliez P, Blum L. Congenital toxoplasmosis from an HIV-infected woman as a result of reactivation. J Infect. 2006;52:e55–e57. doi: 10.1016/j.jinf.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 37.Porter S, Sande M. Toxoplasmosis of the central nervous system in the acquired immunodeficiency syndrome. N Engl J Med. 1992;327:1643–1648. doi: 10.1056/NEJM199212033272306. [DOI] [PubMed] [Google Scholar]
- 38.Heitman B, Irizarry A. Recognition and management of toxoplasmosis. Nurse Pract. 1997;22:79–82. [PubMed] [Google Scholar]
- 39.Chintana T, Sukthana Y, Bunyakai B, Lekkla A. Toxoplasma gondii antibody in pregnant women with and without HIV infection. Southeast Asian J Trop Med Public Health. 1998;29:383–386. [PubMed] [Google Scholar]
- 40.Simpore J, Savadogo A, Ilboudo D, et al. Toxoplasma gondii, HCV, and HBV seroprevalence and co-infection among HIV-positive and -negative pregnant women in Burkina Faso. J Med Virol. 2006;78:730–733. doi: 10.1002/jmv.20615. [DOI] [PubMed] [Google Scholar]
- 41.Dunn D, Newell M, Gilbert R. Low risk of congenital toxoplasmosis in children born to women infected with human immunodeficiency virus. Pediatr Infect Dis J. 1997;16:84. doi: 10.1097/00006454-199701000-00023. [DOI] [PubMed] [Google Scholar]
- 42.Minkoff H, Remington JS, Holman S, Ramirez R, Goodwin S, Landesman S. Vertical transmission of toxoplasma by human immunodeficiency virus-infected women. Am J Obstet Gynecol. 1997;176:555–559. doi: 10.1016/s0002-9378(97)70547-7. [DOI] [PubMed] [Google Scholar]
- 43.Helfgott A. TORCH testing in HIV-infected women. Clin Obstet Gynecol. 1999;42:149–162. doi: 10.1097/00003081-199903000-00019. [DOI] [PubMed] [Google Scholar]
- 44.Vanhems P, Irion O, Hirschel B. Toxoplasmic encephalitis during pregnancy. AIDS. 1993;7:142–143. doi: 10.1097/00002030-199301000-00033. [DOI] [PubMed] [Google Scholar]
- 45.Conley F, Jenkins K, Remington J. Toxoplasma gondii infection of the central nervous system. Use of the peroxidase-antiperoxidase method to demonstrate toxoplasma in formalin fixed, paraffin embedded tissue sections. Hum Pathol. 1981;12:690–698. doi: 10.1016/s0046-8177(81)80170-0. [DOI] [PubMed] [Google Scholar]
- 46.Nogueira SA, Guedes AL, Machado ES, et al. Toxoplasmic encephalitis in an HIV infected pregnant woman: successful outcome for both mother and child. Braz J Infect Dis. 2002;6:201–205. doi: 10.1590/s1413-86702002000400008. [DOI] [PubMed] [Google Scholar]