Abstract
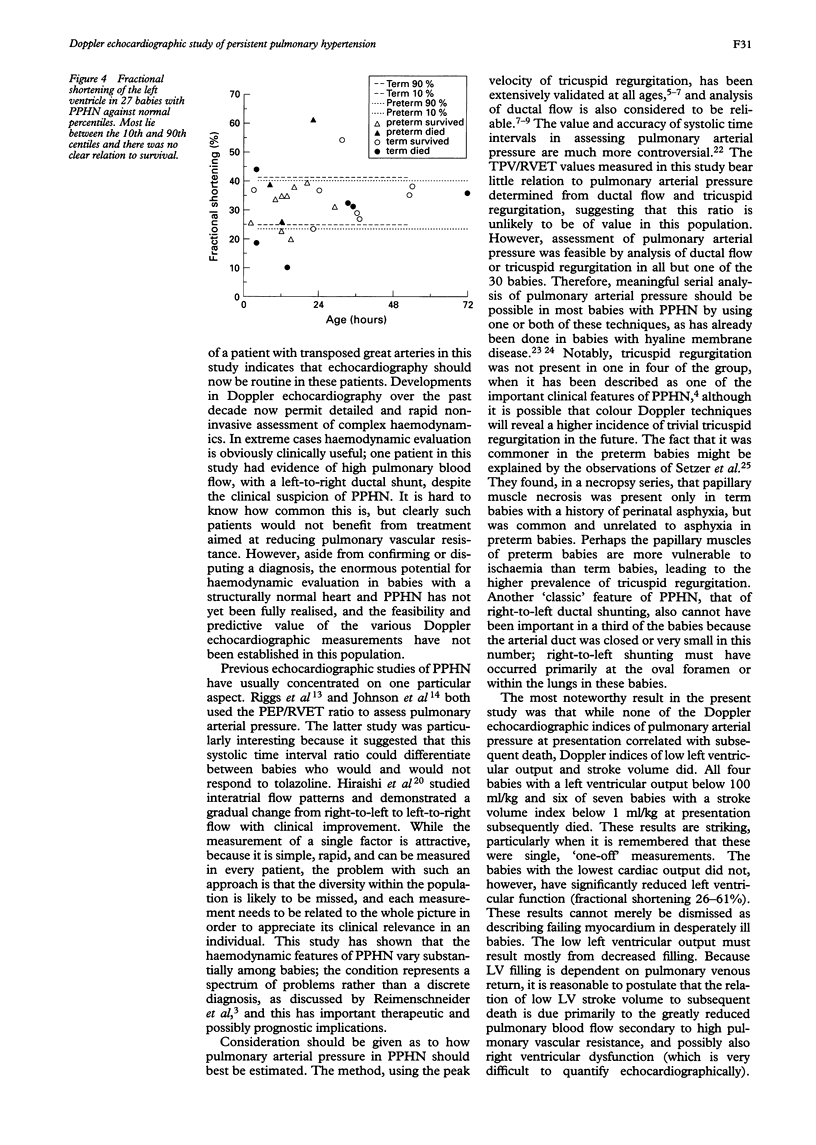
Thirty four newborns presenting with persistent hypoxaemia in the first three days of life underwent detailed haemodynamic assessment using Doppler echocardiography, including measurements of pulmonary arterial pressure (PAP), left ventricular (LV) function, and left ventricular output (LVO). Results were compared with values from 51 healthy babies, and those of survivors were compared with non-survivors. Four of the 34 babies were excluded from this analysis because one was found to have transposed great arteries, one had a large left-to-right shunt with no evidence of persistent pulmonary hypertension, and two had diffuse skeletal myopathy. Tricuspid regurgitation was present in 70%, permitting systolic PAP estimation. The pulmonary:systemic arterial pressure ratio range was 0.7:1 to 1.83:1 (mean 1.02:1). A patent duct was present in 83%, and flow patterns indicated PAP approaching, or above, systemic pressure in all. Systolic time interval ratio TPV/RVET (time to peak velocity at the pulmonary valve/right ventricular ejection time) was mostly (65%) in the normal range, and did not correlate with other PAP measurements. LV function was below the 10th centile in only 11%, but values for LVO lay below the 10th centile in 41%, and for left ventricular stroke volume index (LSVI) in 66%. Results of 18 survivors were compared with 10 non-survivors (excluding two premature babies who died early with pulmonary interstitial emphysema). There were no significant differences for any parameter of PAP or LV function, but LVO and LSVI were significantly lower in non-survivors: LVO survivors (mean (SD)), 205 (57), non-survivors 138 (63) ml/kg/minute (P < 0.01); LSVI survivors, 1.29 (0.51), non-survivors 0.86 (0.31) ml/kg (P < 0.05). All four babies with LVO < 100 ml/kg/minute died, and 6/7 babies with LSVI < 1 ml/kg died. Detailed echocardiographic evaluation shows that the haemodynamic features of persistent pulmonary hypertension are diverse and that clinical diagnosis can be incorrect. Low LV output and stroke volume, usually with normal LV function, were the only Doppler echocardiographic parameters to predict subsequent death. This correlation with outcome requires further prospective evaluation.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alverson D. C., Eldridge M., Dillon T., Yabek S. M., Berman W., Jr Noninvasive pulsed Doppler determination of cardiac output in neonates and children. J Pediatr. 1982 Jul;101(1):46–50. doi: 10.1016/s0022-3476(82)80178-9. [DOI] [PubMed] [Google Scholar]
- Currie P. J., Seward J. B., Chan K. L., Fyfe D. A., Hagler D. J., Mair D. D., Reeder G. S., Nishimura R. A., Tajik A. J. Continuous wave Doppler determination of right ventricular pressure: a simultaneous Doppler-catheterization study in 127 patients. J Am Coll Cardiol. 1985 Oct;6(4):750–756. doi: 10.1016/s0735-1097(85)80477-0. [DOI] [PubMed] [Google Scholar]
- Davis J. M., Spitzer A. R., Cox C., Fox W. W. Predicting survival in infants with persistent pulmonary hypertension of the newborn. Pediatr Pulmonol. 1988;5(1):6–9. doi: 10.1002/ppul.1950050103. [DOI] [PubMed] [Google Scholar]
- Evans N. J., Archer L. N. Postnatal circulatory adaptation in healthy term and preterm neonates. Arch Dis Child. 1990 Jan;65(1 Spec No):24–26. doi: 10.1136/adc.65.1_spec_no.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gersony W. M. Neonatal pulmonary hypertension: pathophysiology, classification, and etiology. Clin Perinatol. 1984 Oct;11(3):517–524. [PubMed] [Google Scholar]
- Halliday H., Hirschfeld S., Riggs T., Liebman J., Fanaroff A., Bormuth C. Respiratory distress syndrome: echocardiographic assessment of cardiovascular function and pulmonary vascular resistance. Pediatrics. 1977 Oct;60(4):444–449. [PubMed] [Google Scholar]
- Hiraishi S., Agata Y., Saito K., Oguchi K., Misawa H., Fujino N., Horiguchi Y., Yashiro K. Interatrial shunt flow profiles in newborn infants: a colour flow and pulsed Doppler echocardiographic study. Br Heart J. 1991 Jan;65(1):41–45. doi: 10.1136/hrt.65.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houston A. B., Lim M. K., Doig W. B., Gnanapragasam J., Coleman E. N., Jamieson M. P., Pollock J. C. Doppler flow characteristics in the assessment of pulmonary artery pressure in ductus arteriosus. Br Heart J. 1989 Oct;62(4):284–290. doi: 10.1136/hrt.62.4.284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson I., Houston A., Aitchison T., Holland B., Turner T. Reproducibility of measurements of cardiac output in newborn infants by Doppler ultrasound. Arch Dis Child. 1990 Jan;65(1 Spec No):15–19. doi: 10.1136/adc.65.1_spec_no.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson G. L., Cunningham M. D., Desai N. S., Cottrill C. M., Noonan J. A. Echocardiography in hypoxemic neonatal pulmonary disease. J Pediatr. 1980 Apr;96(4):716–720. doi: 10.1016/s0022-3476(80)80752-9. [DOI] [PubMed] [Google Scholar]
- Kosturakis D., Goldberg S. J., Allen H. D., Loeber C. Doppler echocardiographic prediction of pulmonary arterial hypertension in congenital heart disease. Am J Cardiol. 1984 Apr 1;53(8):1110–1115. doi: 10.1016/0002-9149(84)90646-5. [DOI] [PubMed] [Google Scholar]
- Linday L. A., Ehlers K. H., O'Loughlin J. E., LaGamma E. F., Engle M. A. Noninvasive diagnosis of persistent fetal circulation versus congenital cardiovascular defects. Am J Cardiol. 1983 Oct 1;52(7):847–851. doi: 10.1016/0002-9149(83)90426-5. [DOI] [PubMed] [Google Scholar]
- Musewe N. N., Poppe D., Smallhorn J. F., Hellman J., Whyte H., Smith B., Freedom R. M. Doppler echocardiographic measurement of pulmonary artery pressure from ductal Doppler velocities in the newborn. J Am Coll Cardiol. 1990 Feb;15(2):446–456. doi: 10.1016/s0735-1097(10)80076-2. [DOI] [PubMed] [Google Scholar]
- Riemenscneider T. A., Nielsen H. C., Ruttenberg H. D., Jaffe R. B. Disturbances of the transitional circulation: spectrum of pulmonary hypertension and myocardial dysfunction. J Pediatr. 1976 Oct;89(4):622–625. doi: 10.1016/s0022-3476(76)80404-0. [DOI] [PubMed] [Google Scholar]
- Riggs T., Hirschfeld S., Fanaroff A., Liebman J., Fletcher B., Meyer R. Persistence of fetal circulation syndrome: an echocardiographic study. J Pediatr. 1977 Oct;91(4):626–631. doi: 10.1016/s0022-3476(77)80521-0. [DOI] [PubMed] [Google Scholar]
- Sahn D. J., DeMaria A., Kisslo J., Weyman A. Recommendations regarding quantitation in M-mode echocardiography: results of a survey of echocardiographic measurements. Circulation. 1978 Dec;58(6):1072–1083. doi: 10.1161/01.cir.58.6.1072. [DOI] [PubMed] [Google Scholar]
- Setzer E., Ermocilla R., Tonkin I., John E., Sansa M., Cassady G. Papillary muscle necrosis in a neonatal autopsy population: incidence and associated clinical manifestations. J Pediatr. 1980 Feb;96(2):289–294. doi: 10.1016/s0022-3476(80)80832-8. [DOI] [PubMed] [Google Scholar]
- Skinner J. R., Milligan D. W., Hunter S., Hey E. N. Central venous pressure in the ventilated neonate. Arch Dis Child. 1992 Apr;67(4 Spec No):374–377. doi: 10.1136/adc.67.4_spec_no.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevenson J. G. Comparison of several noninvasive methods for estimation of pulmonary artery pressure. J Am Soc Echocardiogr. 1989 May-Jun;2(3):157–171. doi: 10.1016/s0894-7317(89)80053-7. [DOI] [PubMed] [Google Scholar]
- Walther F. J., Benders M. J., Leighton J. O. Persistent pulmonary hypertension in premature neonates with severe respiratory distress syndrome. Pediatrics. 1992 Dec;90(6):899–904. [PubMed] [Google Scholar]


