Abstract
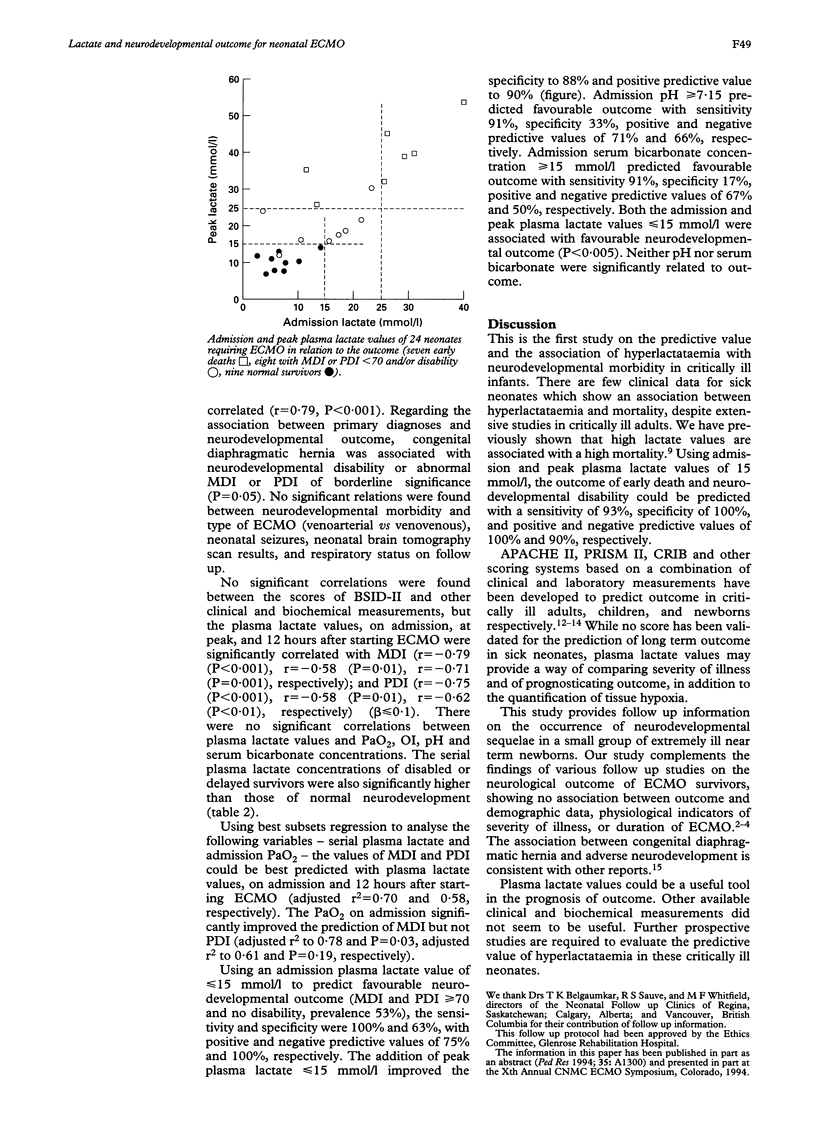
Although plasma lactate concentration has been widely used as an indicator of tissue hypoxia, no clinical study has been conducted to relate these values to the neurological outcome of sick neonates. Seventeen consecutively cared for and surviving neonates with severe hypoxaemia requiring extracorporeal membrane oxygenation (ECMO) were evaluated at a mean age of 19.6 months. The serial plasma lactate concentrations were significantly correlated with the scores of the Bayley Scales of Infant Development. Admission and peak plasma lactate of < or = 15 mmol/l predicted favourable outcome (MDI and PDI > 70 and no disability): sensitivity 100%, specificity 88%, positive predictive value 90%, and negative predictive value 100%. Plasma lactate values could help predict neurodevelopmental outcome in these sick neonates.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Cheung P. Y., Finer N. N. Plasma lactate concentration as a predictor of death in neonates with severe hypoxemia requiring extracorporeal membrane oxygenation. J Pediatr. 1994 Nov;125(5 Pt 1):763–768. doi: 10.1016/s0022-3476(94)70076-1. [DOI] [PubMed] [Google Scholar]
- Flusser H., Dodge N. N., Engle W. E., Garg B. P., West K. W. Neurodevelopmental outcome and respiratory morbidity for extracorporeal membrane oxygenation survivors at 1 year of age. J Perinatol. 1993 Jul-Aug;13(4):266–271. [PubMed] [Google Scholar]
- Glass P., Miller M., Short B. Morbidity for survivors of extracorporeal membrane oxygenation: neurodevelopmental outcome at 1 year of age. Pediatrics. 1989 Jan;83(1):72–78. [PubMed] [Google Scholar]
- Hofkosh D., Thompson A. E., Nozza R. J., Kemp S. S., Bowen A., Feldman H. M. Ten years of extracorporeal membrane oxygenation: neurodevelopmental outcome. Pediatrics. 1991 Apr;87(4):549–555. [PubMed] [Google Scholar]
- Knaus W. A., Draper E. A., Wagner D. P., Zimmerman J. E. APACHE II: a severity of disease classification system. Crit Care Med. 1985 Oct;13(10):818–829. [PubMed] [Google Scholar]
- Lund D. P., Mitchell J., Kharasch V., Quigley S., Kuehn M., Wilson J. M. Congenital diaphragmatic hernia: the hidden morbidity. J Pediatr Surg. 1994 Feb;29(2):258–264. doi: 10.1016/0022-3468(94)90329-8. [DOI] [PubMed] [Google Scholar]
- Mizock B. A., Falk J. L. Lactic acidosis in critical illness. Crit Care Med. 1992 Jan;20(1):80–93. doi: 10.1097/00003246-199201000-00020. [DOI] [PubMed] [Google Scholar]
- Mujsce D. J., Towfighi J., Vannucci R. C. Physiologic and neuropathologic aspects of hypothermic circulatory arrest in newborn dogs. Pediatr Res. 1990 Oct;28(4):354–360. doi: 10.1203/00006450-199010000-00011. [DOI] [PubMed] [Google Scholar]
- Robertson C. M., Finer N. N., Sauve R. S., Whitfield M. F., Belgaumkar T. K., Synnes A. R., Grace M. G. Neurodevelopmental outcome after neonatal extracorporeal membrane oxygenation. CMAJ. 1995 Jun 15;152(12):1981–1988. [PMC free article] [PubMed] [Google Scholar]
- Vincent J. L., Dufaye P., Berré J., Leeman M., Degaute J. P., Kahn R. J. Serial lactate determinations during circulatory shock. Crit Care Med. 1983 Jun;11(6):449–451. doi: 10.1097/00003246-198306000-00012. [DOI] [PubMed] [Google Scholar]


