Abstract
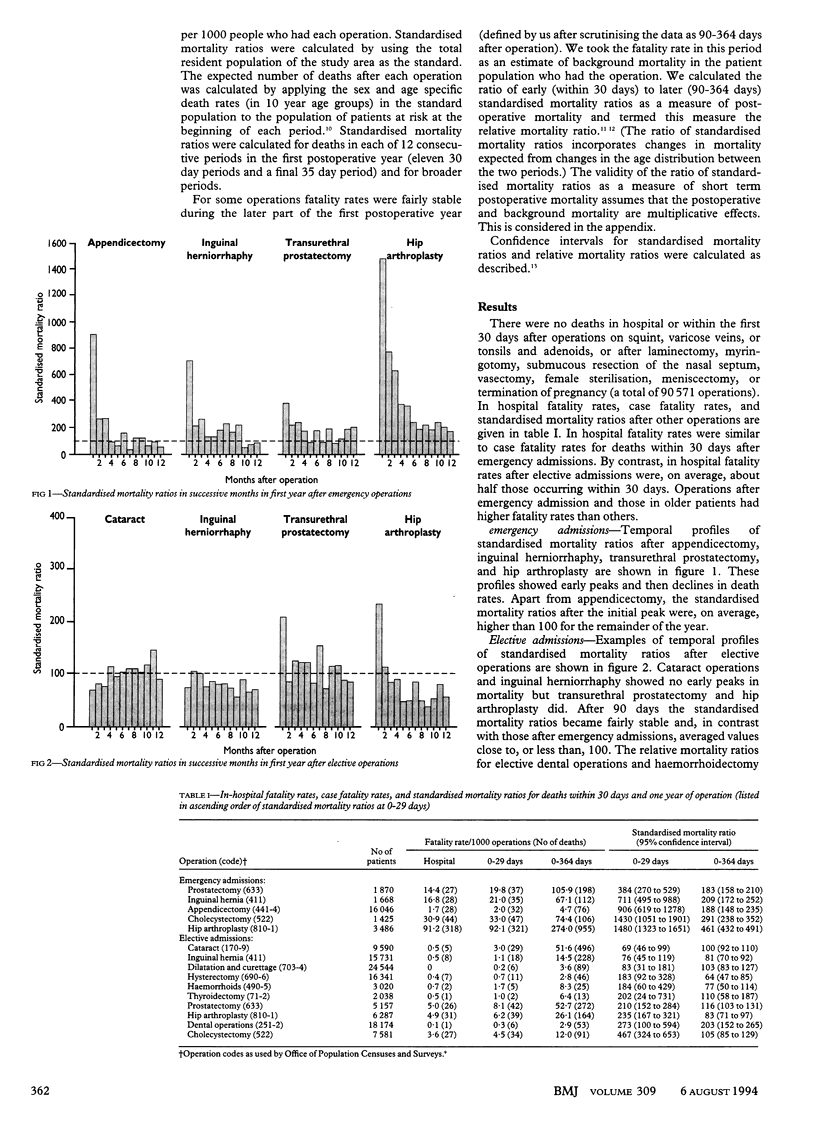
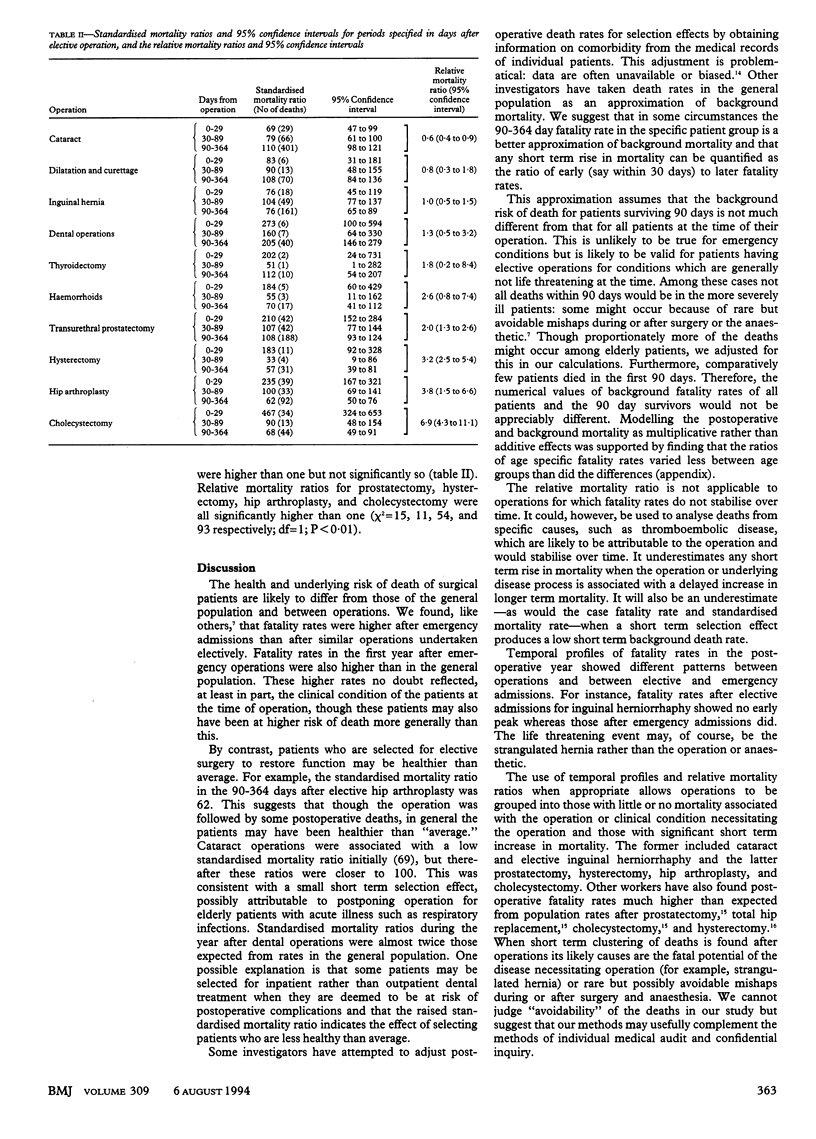
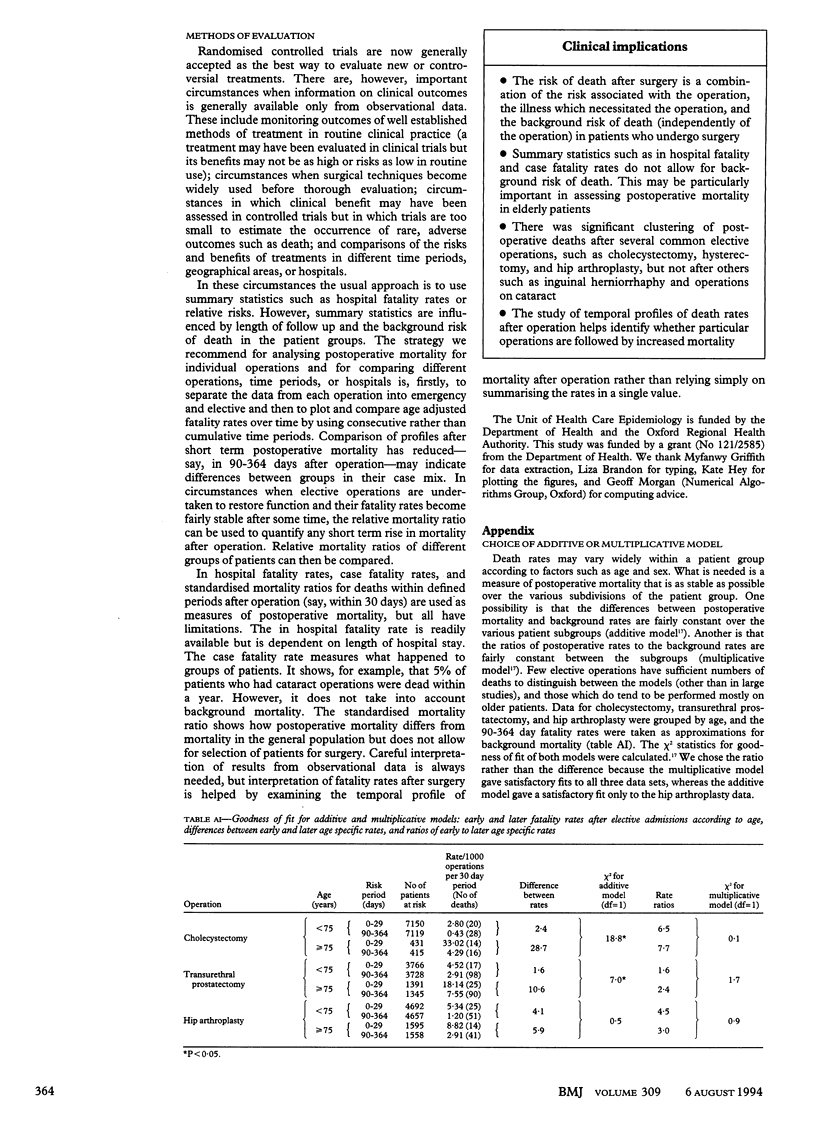
OBJECTIVE--To quantify the short term risk of postoperative mortality in ways which take account of deaths after discharge and the background risks of death in patients who come to operation. DESIGN--Analysis of linked abstracts of hospital admission records and death certificates for common operations. SETTING--Six health districts in the Oxford region. SUBJECTS--Records of 223,529 operations performed in 1980-6. MAIN OUTCOME MEASURES--In hospital fatality rates, case fatality rates, and standardised mortality ratios at selected time periods during the year after operation and the ratio of early (< 30 days) to late (90-364 days after operation) fatality rates. RESULTS--Fatality rates throughout the year after operations performed after emergency admissions were generally higher than those for similar operations performed after elective admissions and higher than expected from population rates. Examples were prostatectomy, hip arthroplasty, inguinal herniorrhaphy, and cholecystectomy. Common elective operations such as inguinal herniorrhaphy and cataract operations showed no early peak in mortality, but others did. These included transurethral prostatectomy (ratio of early to late mortality 2.0; 95% confidence interval 1.3 to 2.6), hysterectomy (3.2; 1.5 to 6.6), hip arthroplasty (3.8; 2.5 to 5.4), and cholecystectomy (6.9; 4.3 to 11.1). CONCLUSIONS--Temporal profiles of death rates in the year after operation show which operations have early peaks in mortality and which do not. Emergency and elective operations have very different profiles and should be analysed separately. For elective operations for conditions which pose no immediate threat to life the ratio of early to later fatality rates provides a measure of increase in mortality after operation while allowing for the background risk of death in the patient groups.
Full text
PDF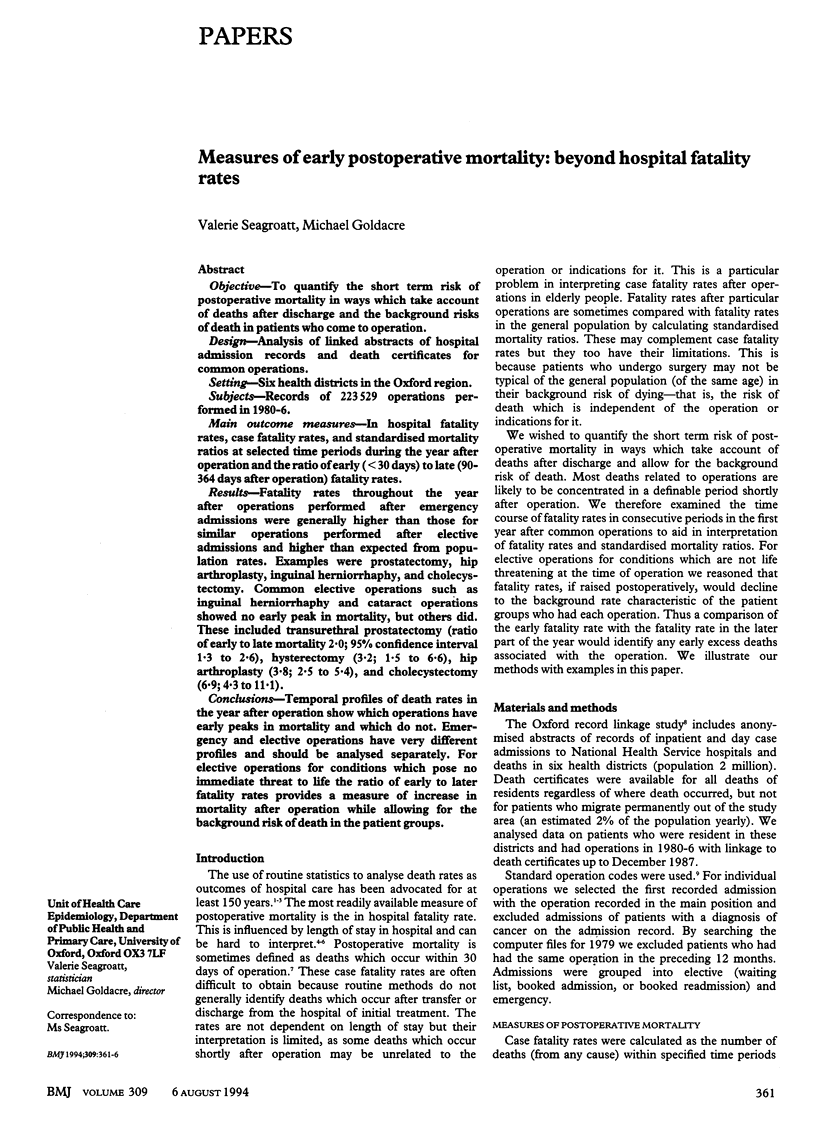

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Goldacre M. J. Hospital inpatient statistics: some aspects of interpretation. Community Med. 1981 Feb;3(1):60–68. [PubMed] [Google Scholar]
- Goldacre M., Seagroatt V., Hawton K. Suicide after discharge from psychiatric inpatient care. Lancet. 1993 Jul 31;342(8866):283–286. doi: 10.1016/0140-6736(93)91822-4. [DOI] [PubMed] [Google Scholar]
- Jencks S. F., Williams D. K., Kay T. L. Assessing hospital-associated deaths from discharge data. The role of length of stay and comorbidities. JAMA. 1988 Oct 21;260(15):2240–2246. [PubMed] [Google Scholar]
- Loft A., Andersen T. F., Brønnum-Hansen H., Roepstorff C., Madsen M. Early postoperative mortality following hysterectomy. A Danish population based study, 1977-1981. Br J Obstet Gynaecol. 1991 Feb;98(2):147–154. doi: 10.1111/j.1471-0528.1991.tb13360.x. [DOI] [PubMed] [Google Scholar]
- Lubitz J., Riley G., Newton M. Outcomes of surgery among the Medicare aged: mortality after surgery. Health Care Financ Rev. 1985 Summer;6(4):103–115. [PMC free article] [PubMed] [Google Scholar]
- Seagroatt V., Tan H. S., Goldacre M., Bulstrode C., Nugent I., Gill L. Elective total hip replacement: incidence, emergency readmission rate, and postoperative mortality. BMJ. 1991 Dec 7;303(6815):1431–1435. doi: 10.1136/bmj.303.6815.1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verheul H. A., Dekker E., Bossuyt P., Moulijn A. C., Dunning A. J. Background mortality in clinical survival studies. Lancet. 1993 Apr 3;341(8849):872–875. doi: 10.1016/0140-6736(93)93073-a. [DOI] [PubMed] [Google Scholar]


