Abstract
Regional lymph-node abscesses often occur among infants and young children following BCG vaccination, and the purpose of this study was to find ways to avoid glandular complications, or at least minimize their frequency, without jeopardizing the success of vaccination.
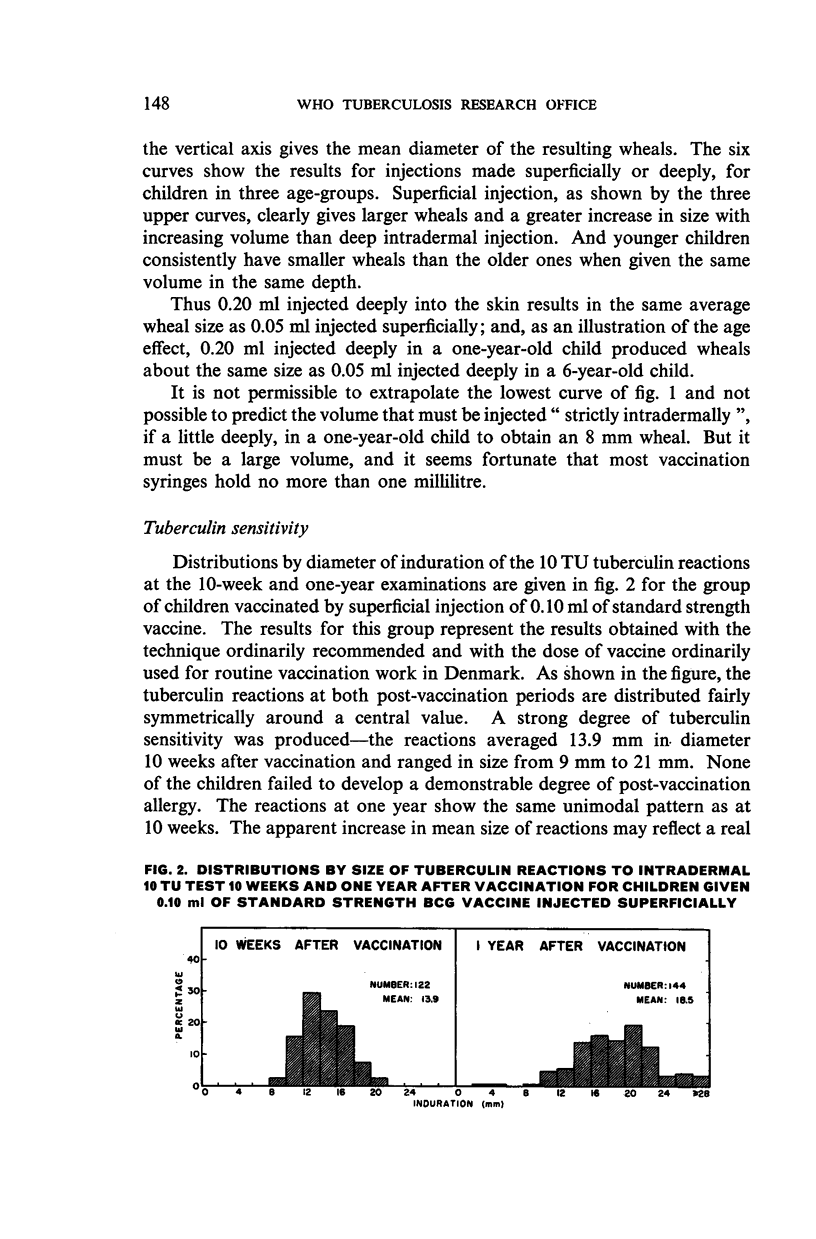
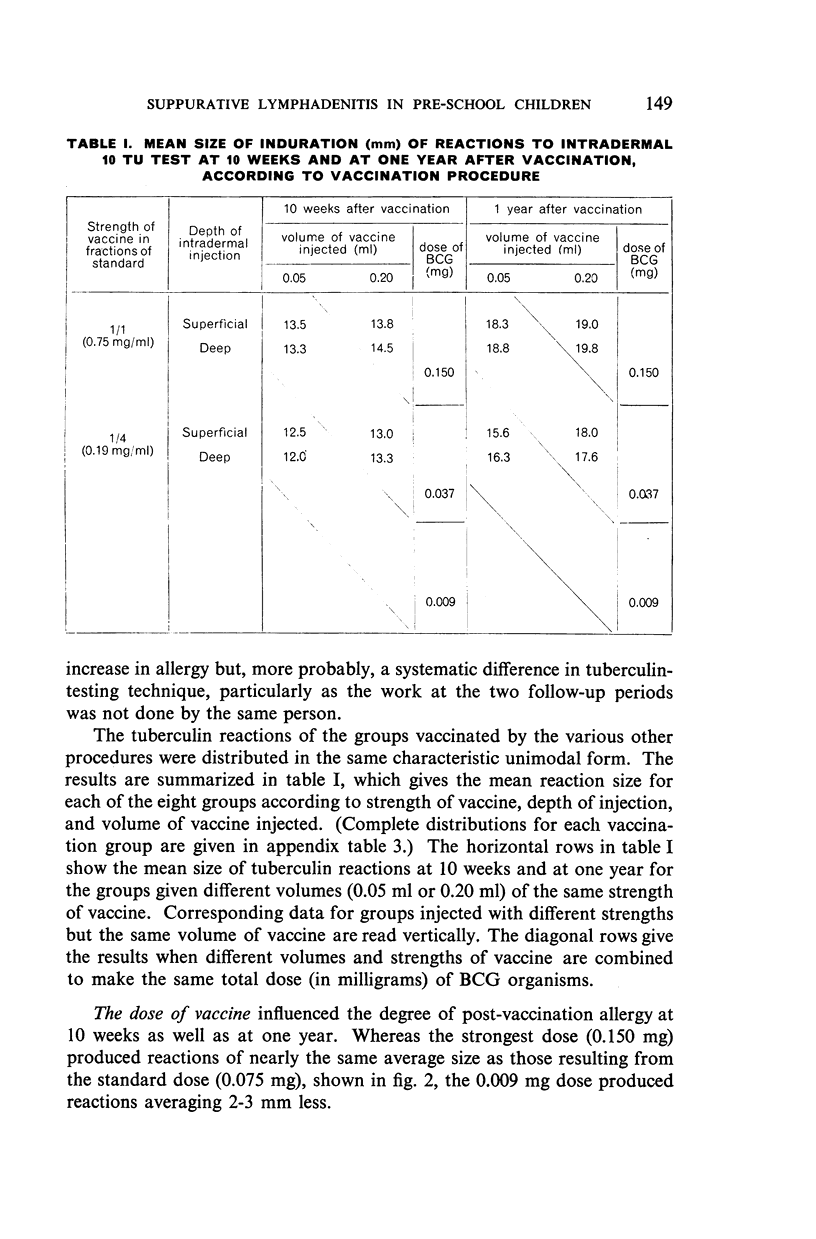
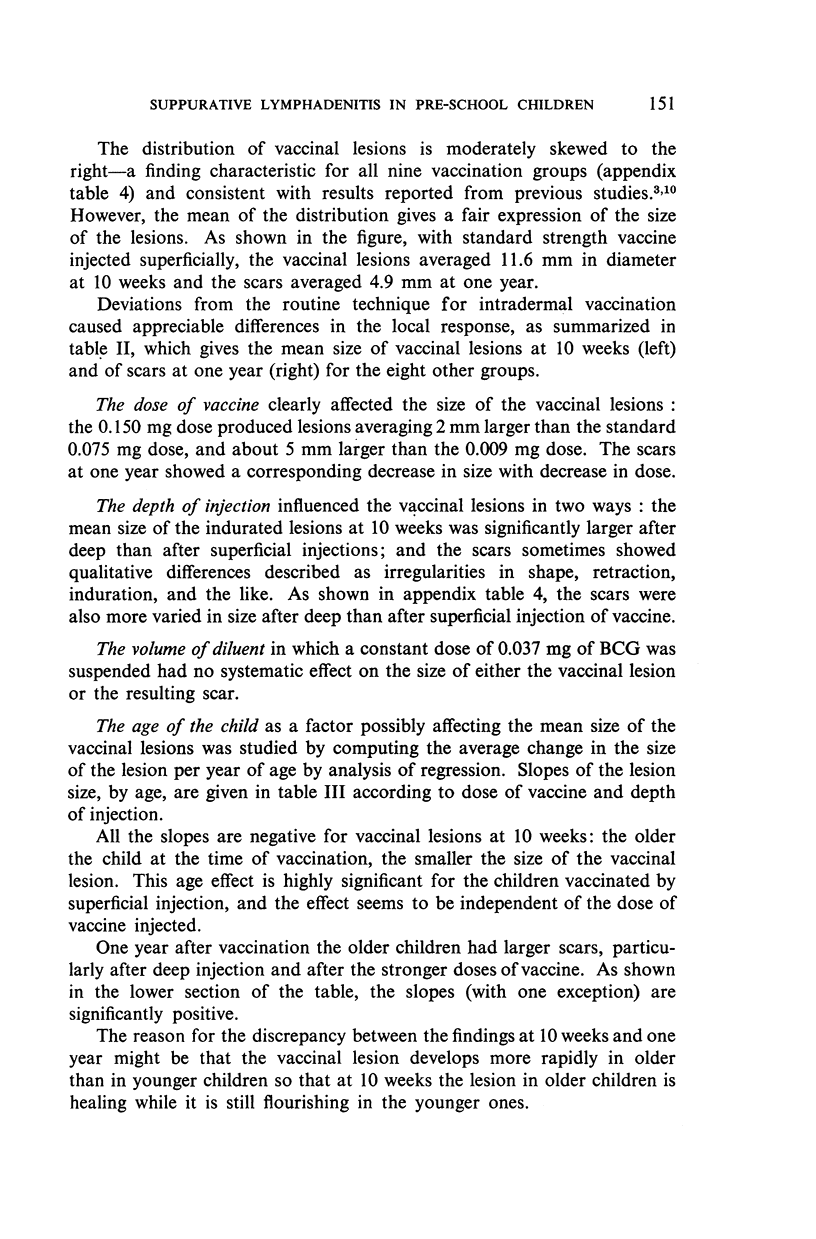
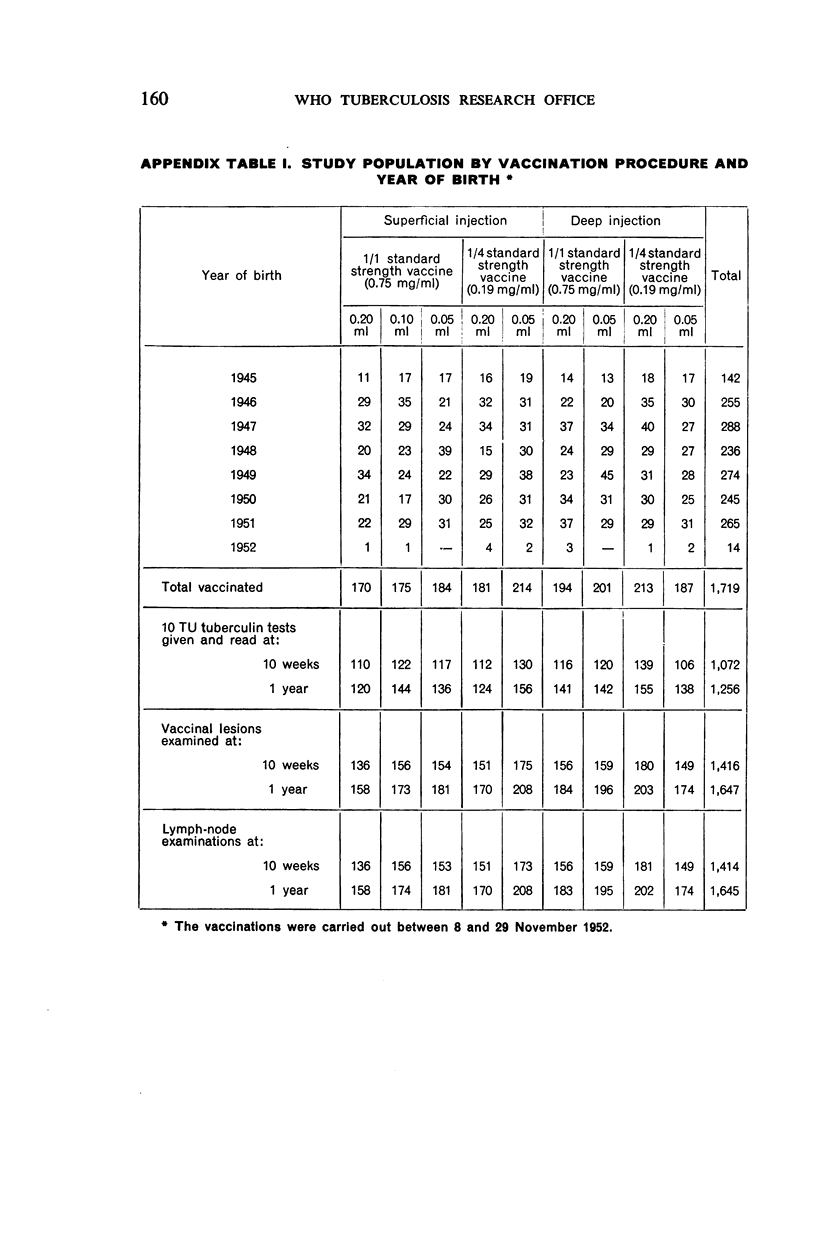
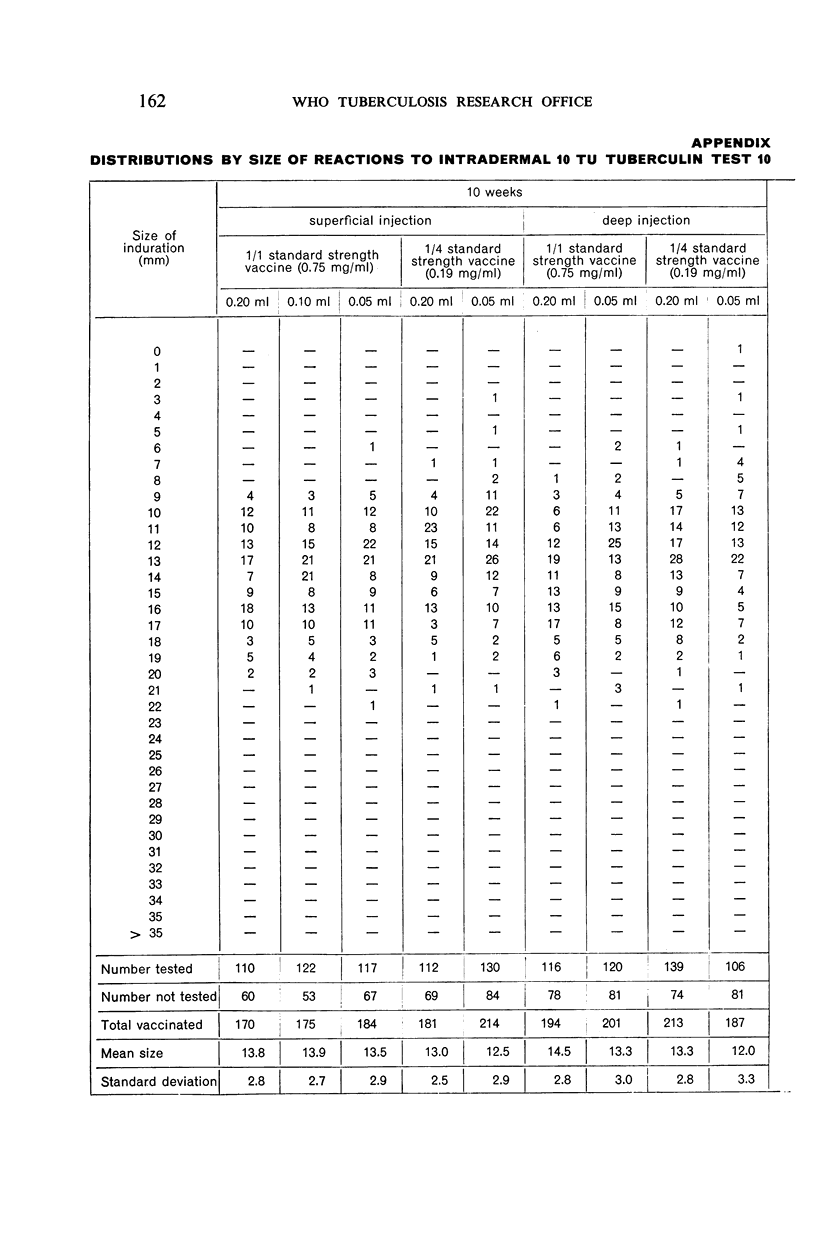
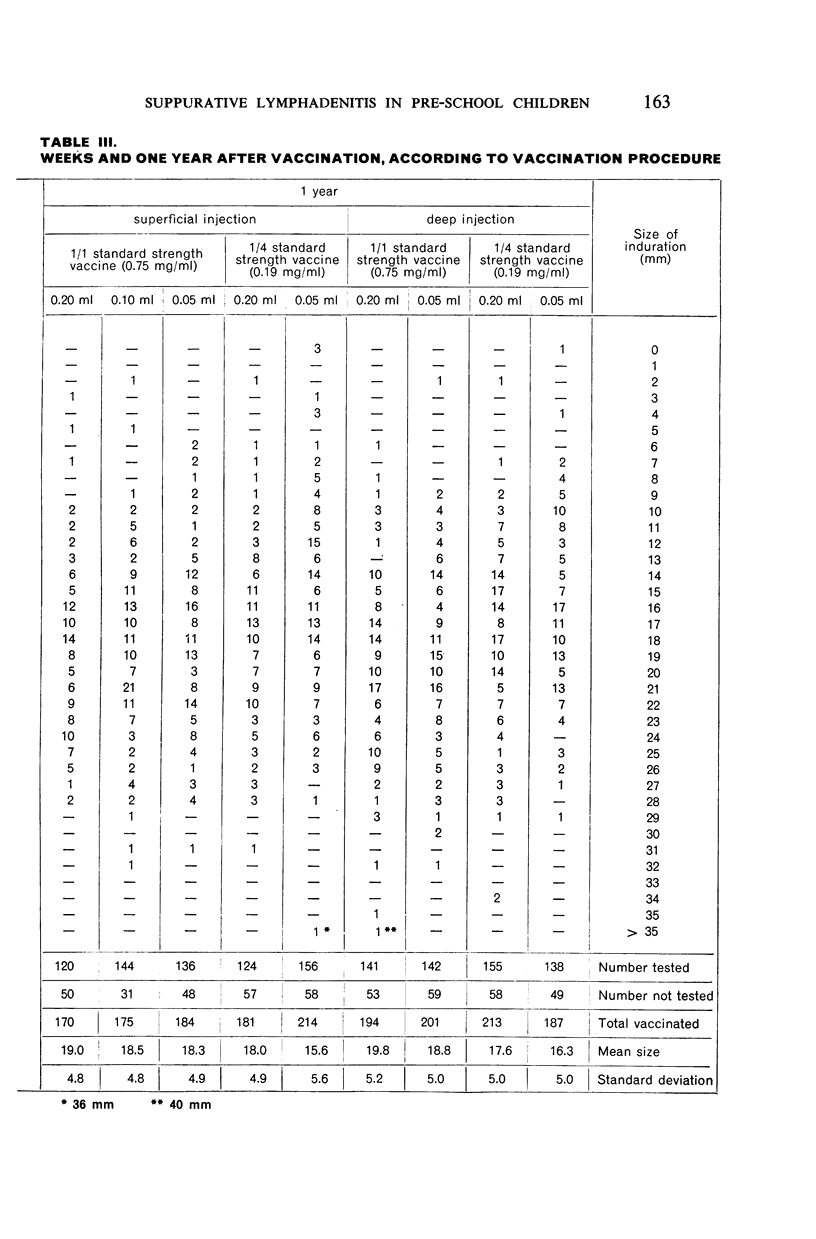
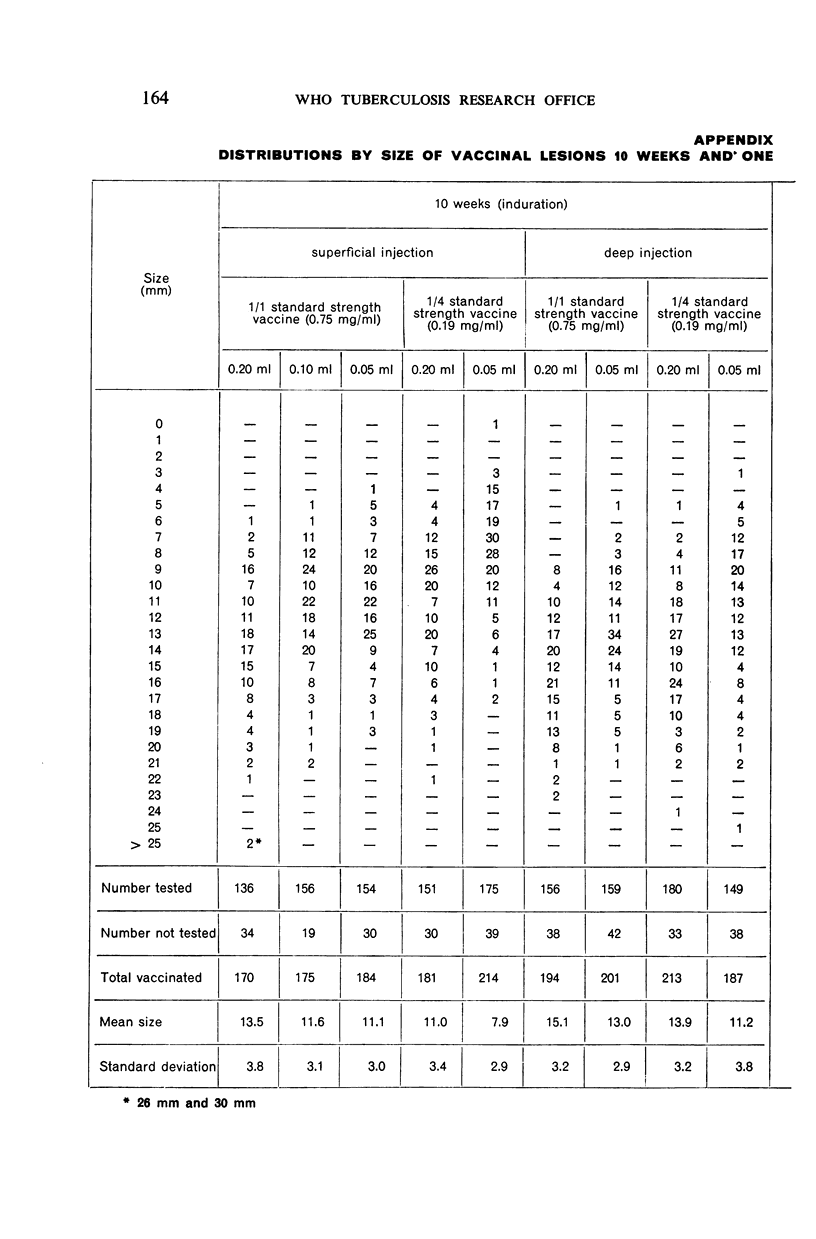
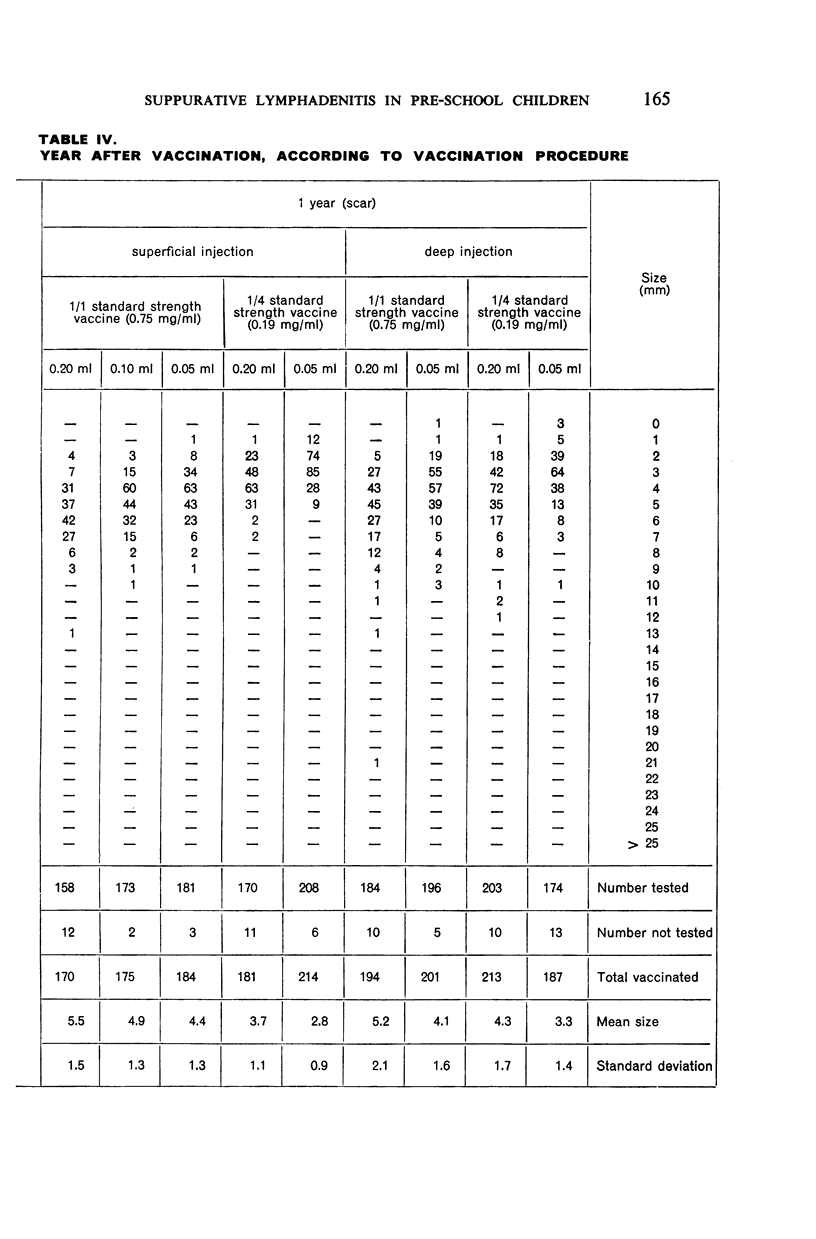
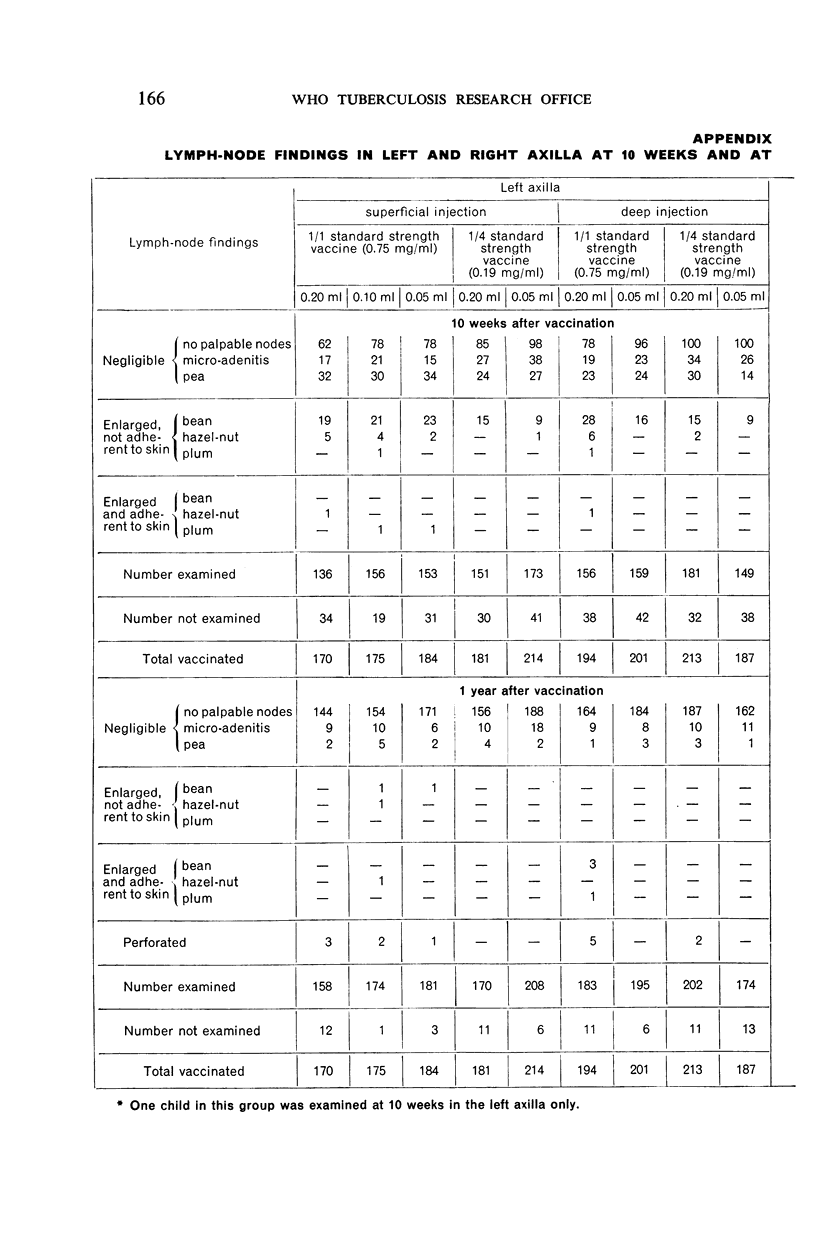
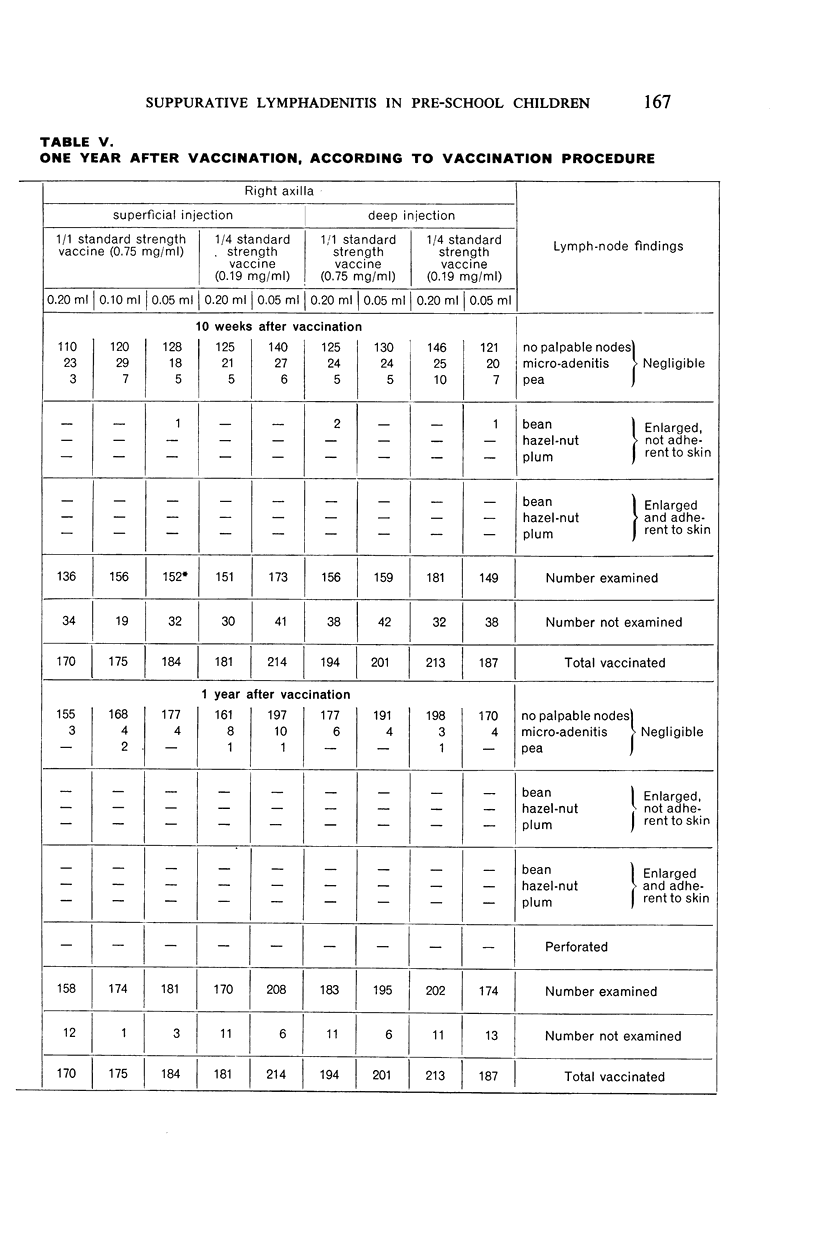
Over 1,700 children ranging in age from 6 months to 7 years were vaccinated by one of nine different procedures obtained by various combinations of two strengths of vaccine, two depths of injection, and three volumes of vaccine, in an attempt to reproduce, experimentally, some of the kinds of variation that may occur in practical programmes. Follow-up examinations were made at 10 weeks and at one year, the local and glandular responses being observed and measured and the degree of tuberculin sensitivity assessed by an intradermal 10 TU test.
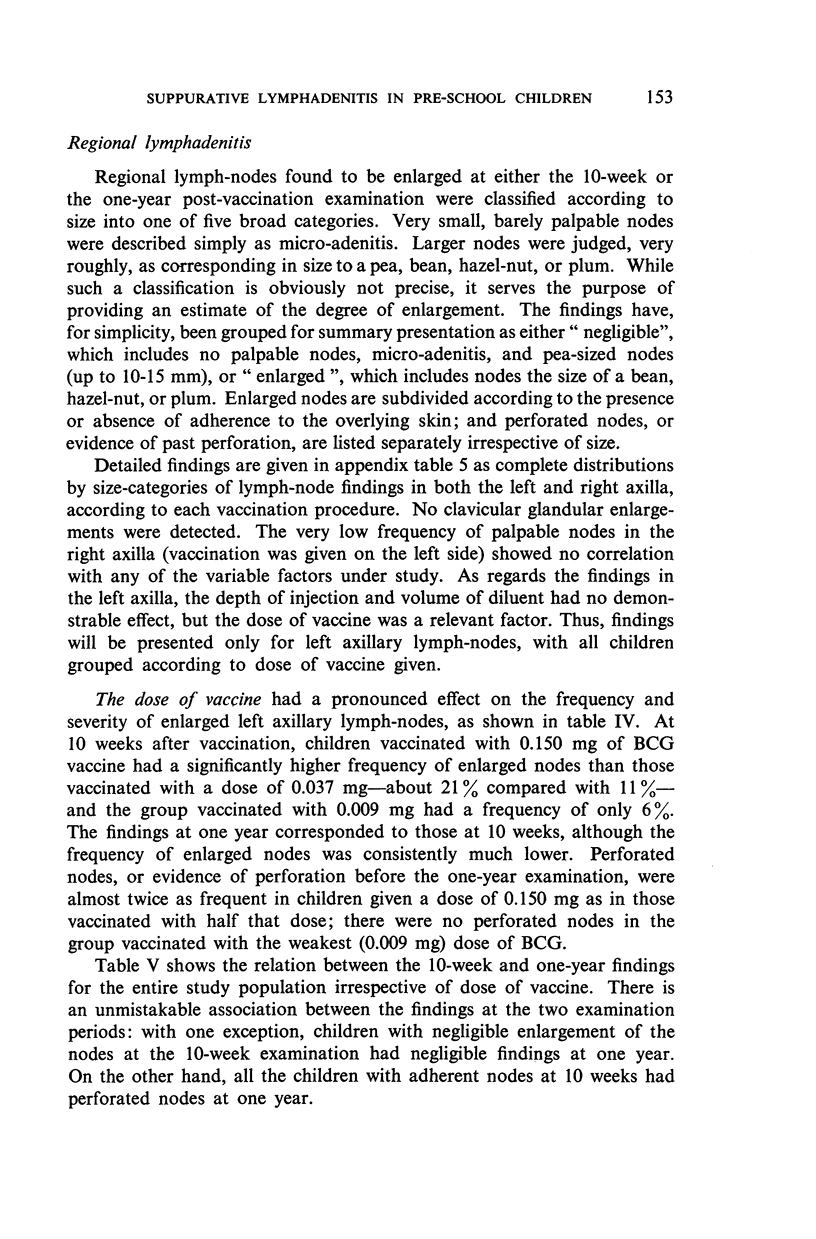
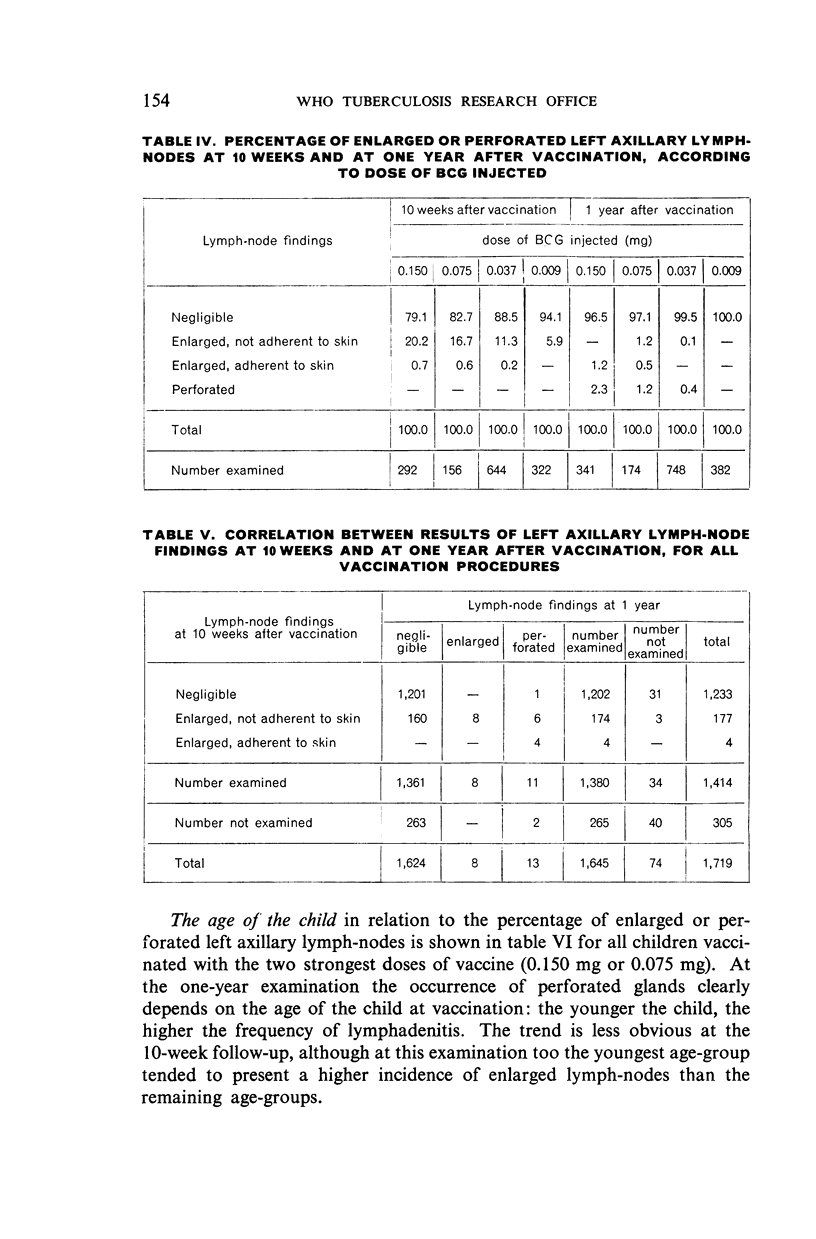
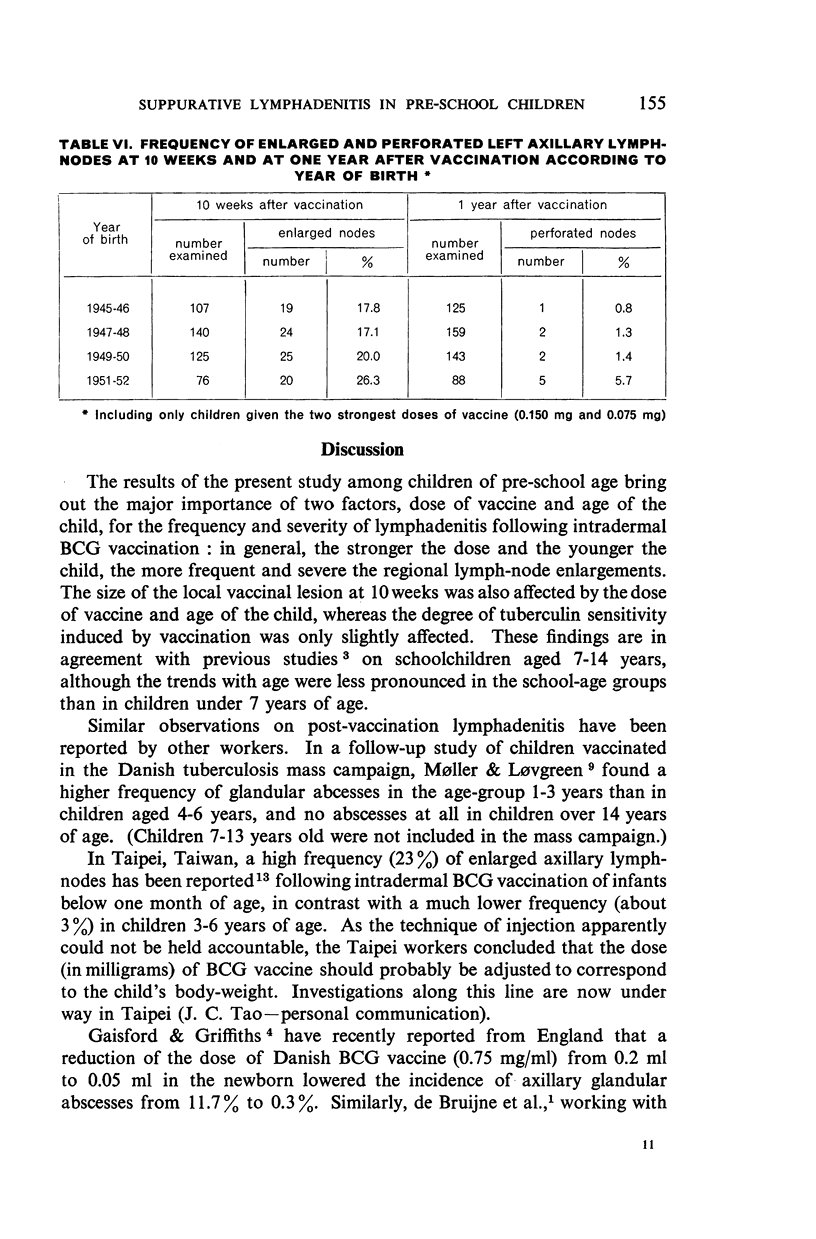
Both the dose of vaccine and the age of the child were found to have a striking effect on the frequency and severity of lymphadenitis: the larger the dose and the younger the child, the higher the frequency of enlarged or perforated axillary lymph nodes. Furthermore, there was a close association between the findings at the two follow-up periods: with only one exception, children with negligible enlargement of the nodes at the 10-week examination had negligible findings at one year, whereas all the children with enlarged and adherent nodes at 10 weeks had evidence of perforation at one year.
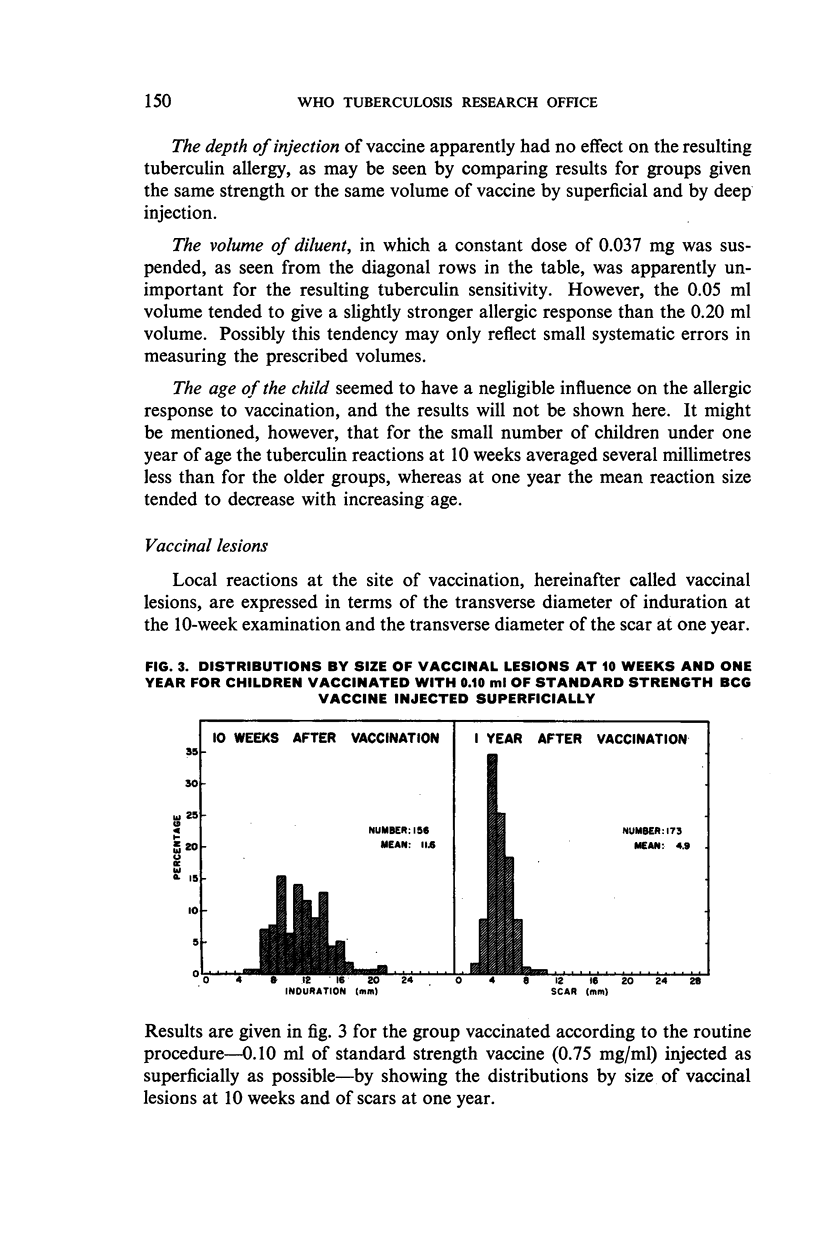
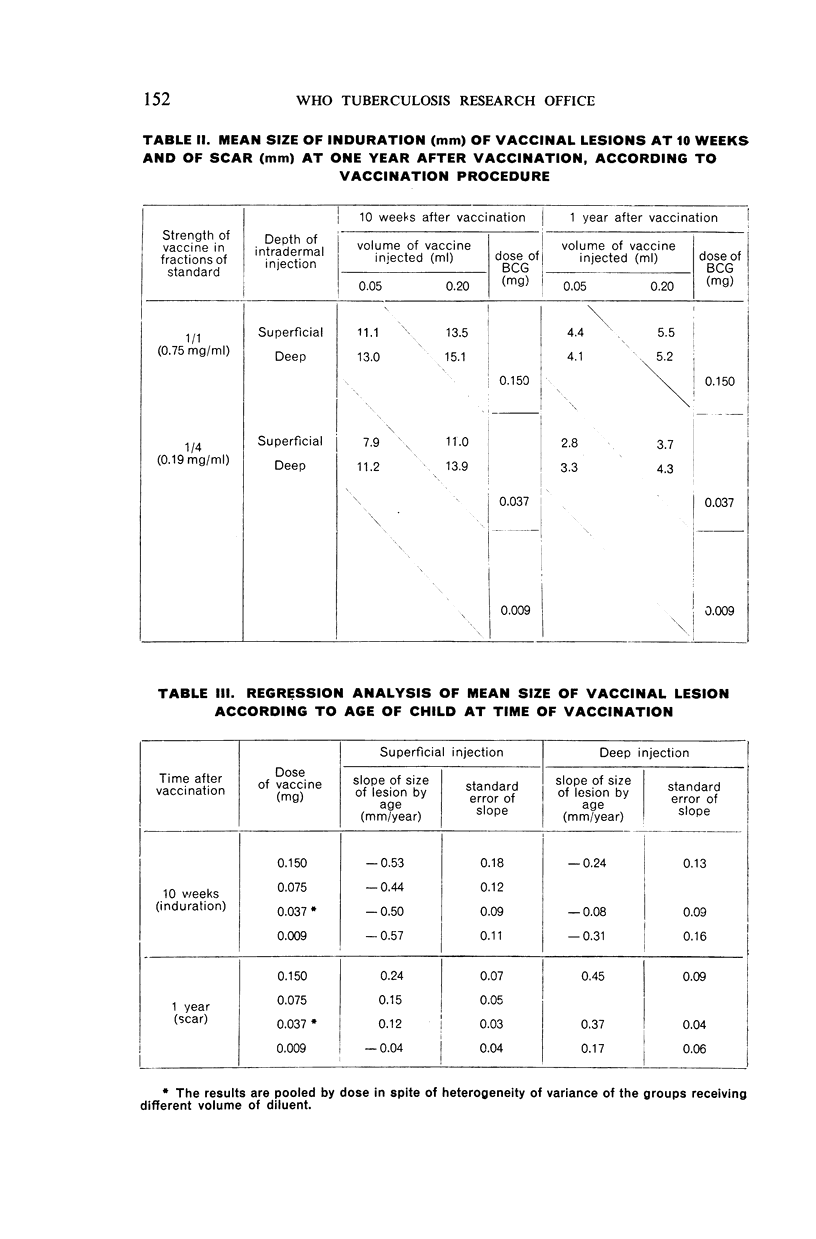
The size of the vaccinal lesion was also affected by vaccine dose and by age of child: the lesion was larger in the younger children and with the stronger doses. The degree of tuberculin sensitivity was affected only slightly by the variations in dose and still less by the age of the child.
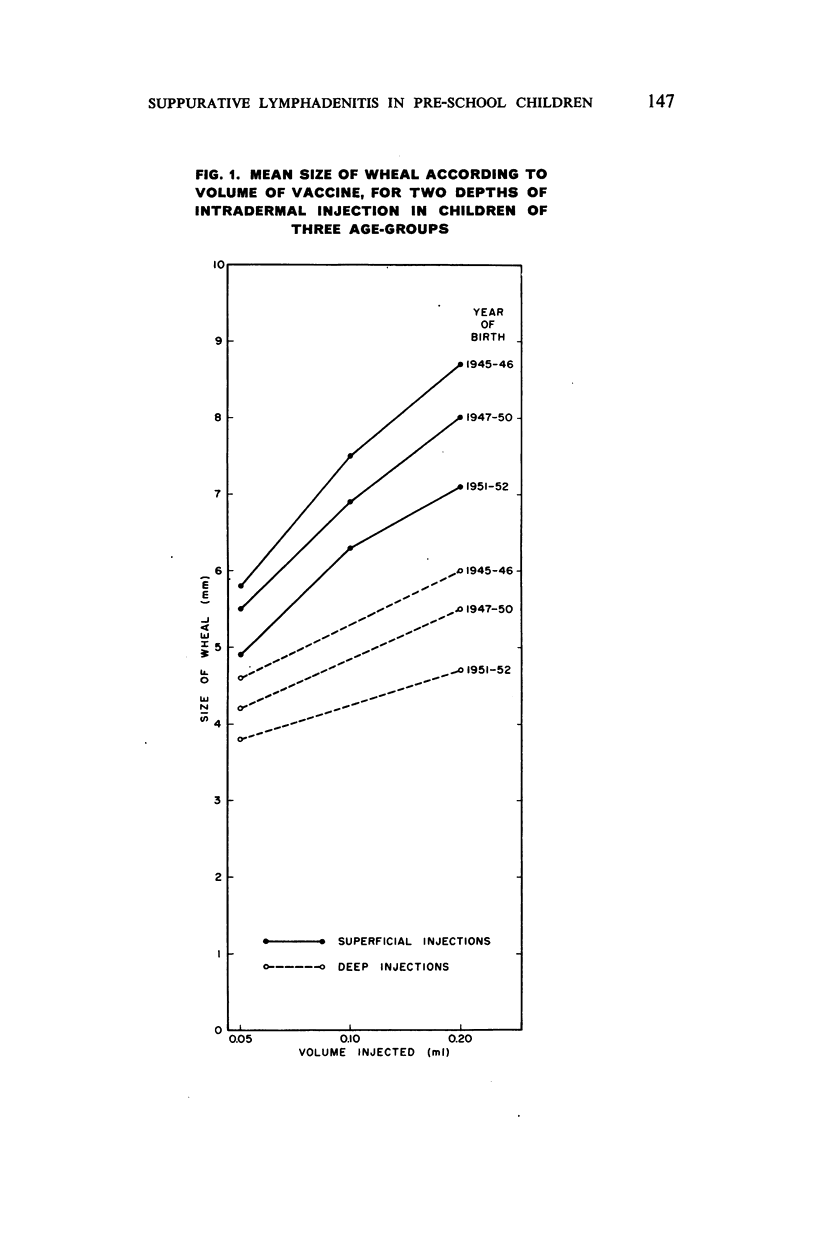
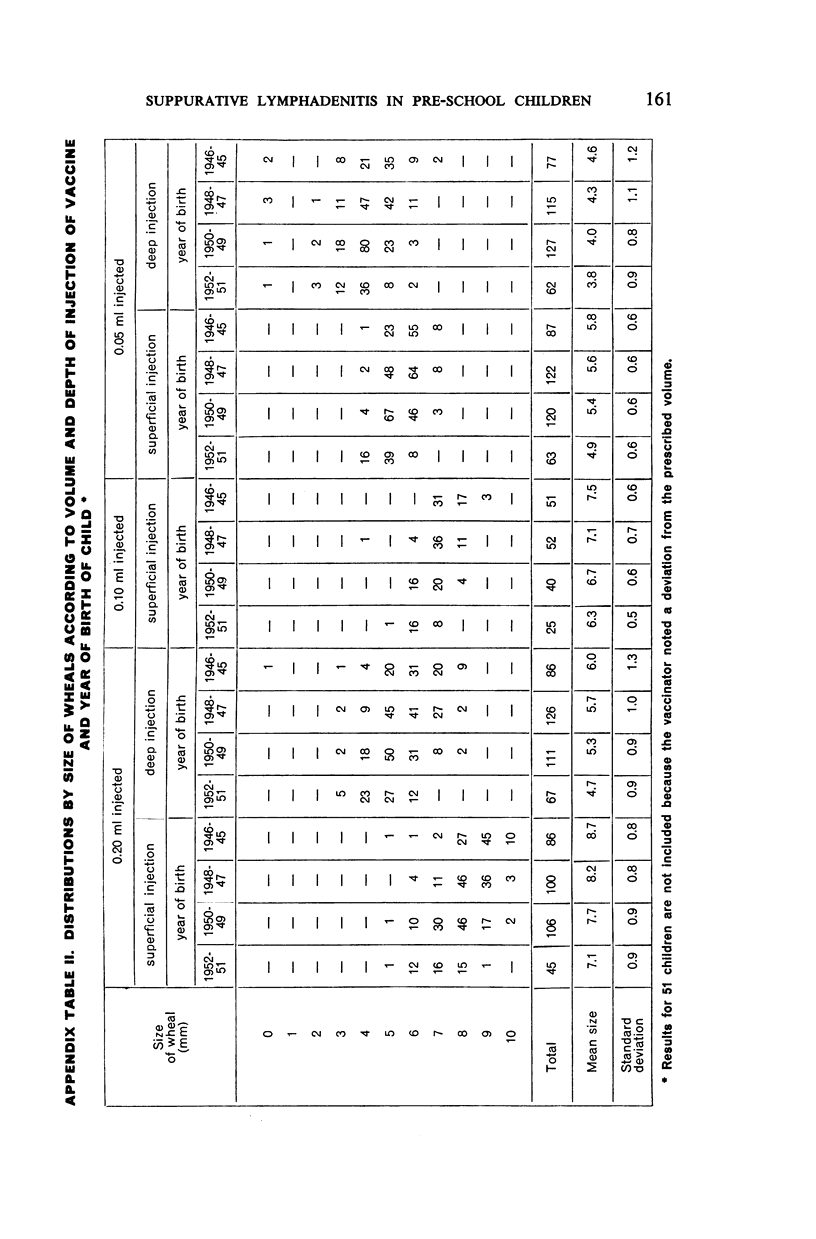
The size of the wheal raised by intradermal injection of vaccine was found to vary with the age of the child and with the depth of injection as much as it varied with the volume of vaccine injected. There can be no doubt that gauging the dose by the size of the wheal, rather than by the calibrations on a non-leaking syringe, is a very inaccurate procedure. When the dose of vaccine can be accurately measured, a stronger vaccine can be given (and perhaps a stronger degree of immunity attained) without causing an intolerable frequency of suppurative lymphadenitis.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- DE BRUIJNE J. I., VAN CREVELD S., PRAKKEN J. R., STOPPELMAN R. H. Complicaties na intracutane inenting van pasgeborenen met BCG-vaccine. Ned Tijdschr Geneeskd. 1952 Oct 25;96(43):2675–2681. [PubMed] [Google Scholar]
- EDWARDS L. B., GELTING A. S. BCG-vaccine studies. I. Effect of age of vaccine and variation in storage temperature and dosage on allergy production and vaccination lesions ten weeks after vaccination. Bull World Health Organ. 1950;3(1):1–24. [PMC free article] [PubMed] [Google Scholar]
- GAISFORD W., GRIFFITHS M. Immunity to tuberculosis in infancy; with special reference to vaccination in the newborn. Tubercle. 1954 Jan;35(1):7–14. doi: 10.1016/s0041-3879(54)80082-1. [DOI] [PubMed] [Google Scholar]
- GULD J., RUD C. Measurement of leakage of tuberculin syringes. Br Med J. 1953 Feb 14;1(4806):368–370. doi: 10.1136/bmj.1.4806.368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OLSEN G. Skulderen, en uheldig lokalisation for vaccinationer. Nord Med. 1952 Oct 10;48(41):1423–1424. [PubMed] [Google Scholar]
- PALMER C. E., EDWARDS P. Q. [Variation in technique of intracutaneous BCG vaccination]. Br Med J. 1953 Feb 14;1(4806):363–368. doi: 10.1136/bmj.1.4806.363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PURSER H. M. An account of 2,500 infant B.C.G. vaccinations. Br Med J. 1954 Feb 13;1(4858):368–370. doi: 10.1136/bmj.1.4858.368. [DOI] [PMC free article] [PubMed] [Google Scholar]


