Abstract
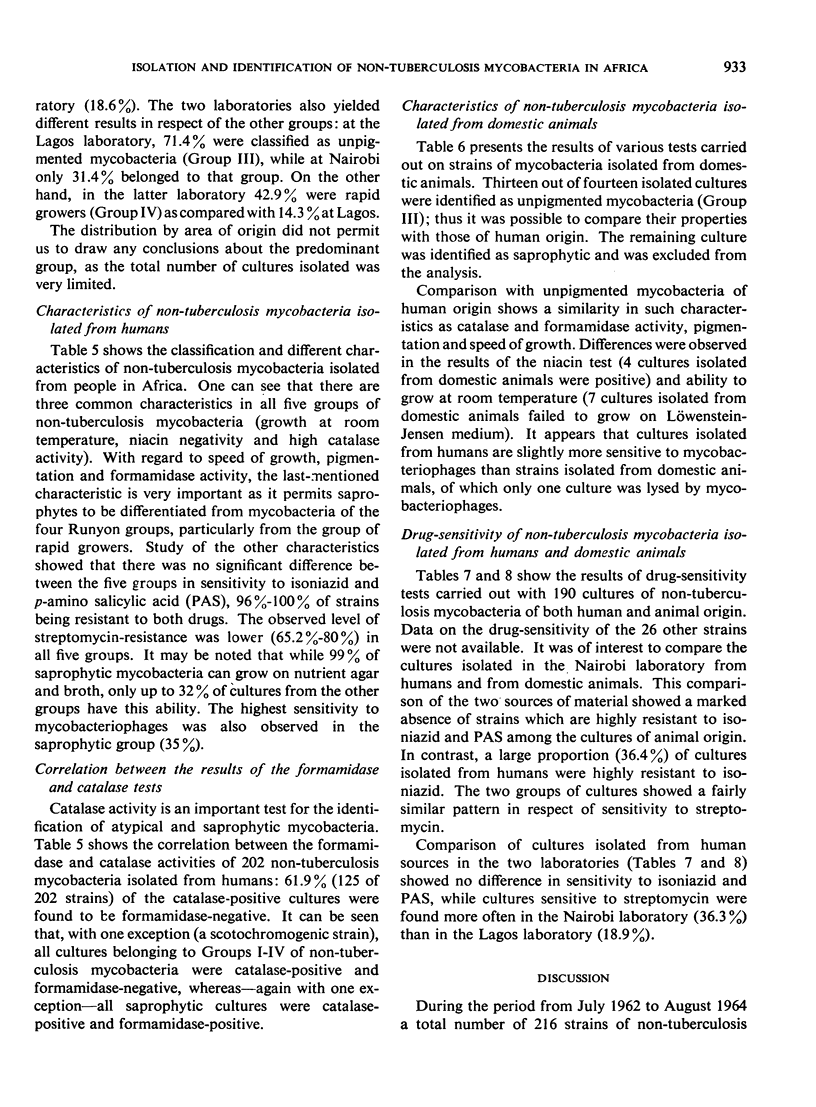
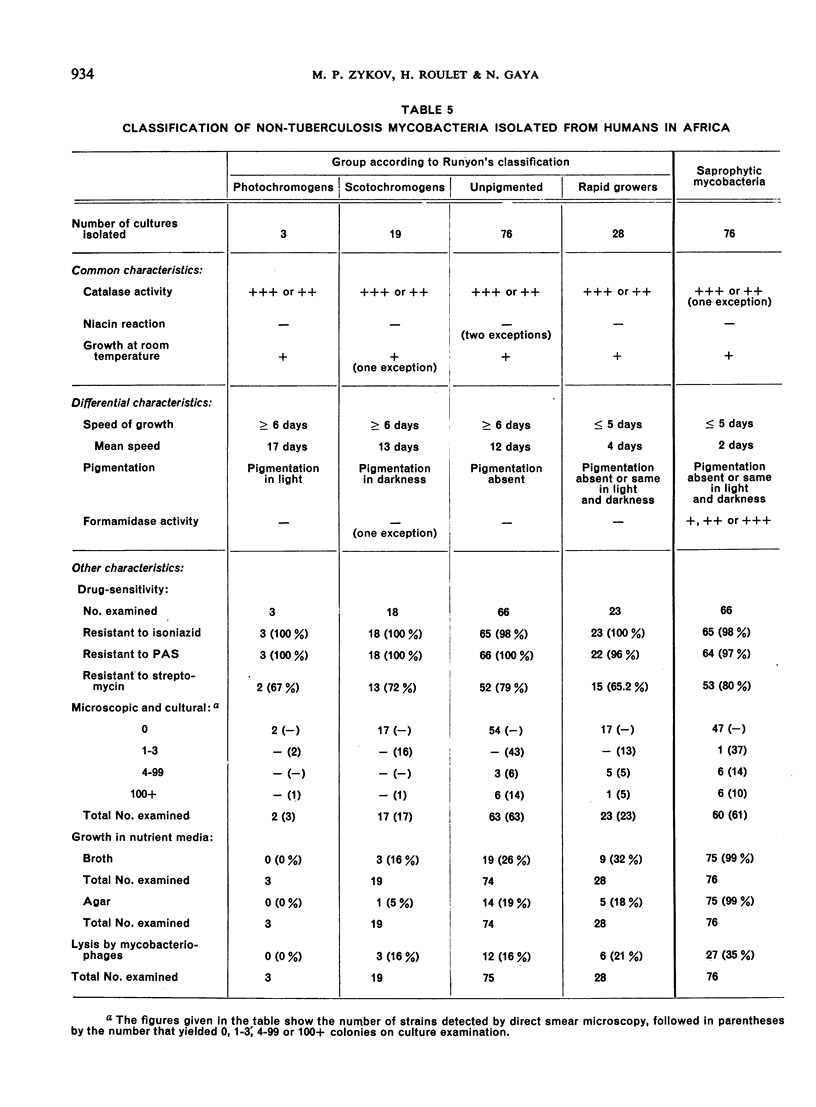
In tropical and subtropical countries, the presence of non-tuberculosis mycobacteria may invalidate case-finding programmes; experience has shown that many of the acid-fast bacilli discovered on examination of sputum specimens are non-tuberculosis mycobacteria—either photochromogens, scotochromogens, unpigmented or rapid growers (Groups I to IV, respectively, of Runyon's classification) or saprophytes.
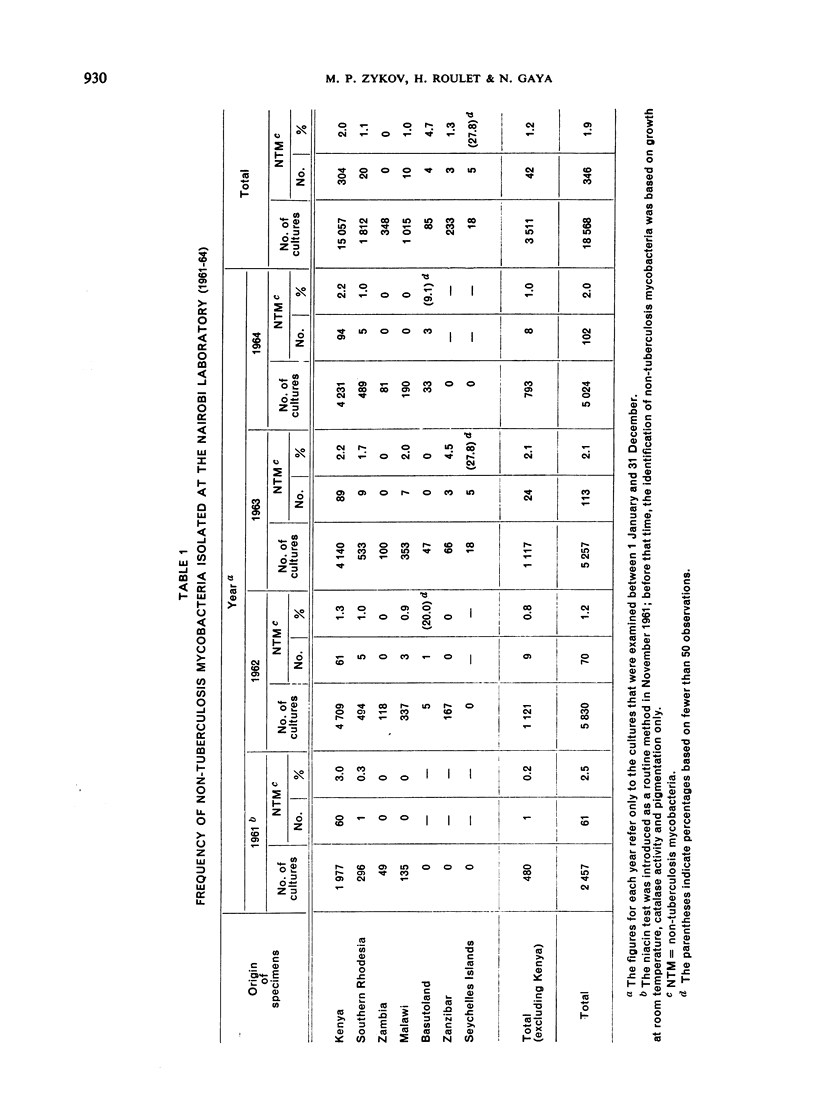
Studies have recently been undertaken to determine the frequency of various types of non-tuberculosis strains in different parts of Africa. This paper describes the first of these studies, devoted to the isolation and identification of non-tuberculosis mycobacteria from seven countries.
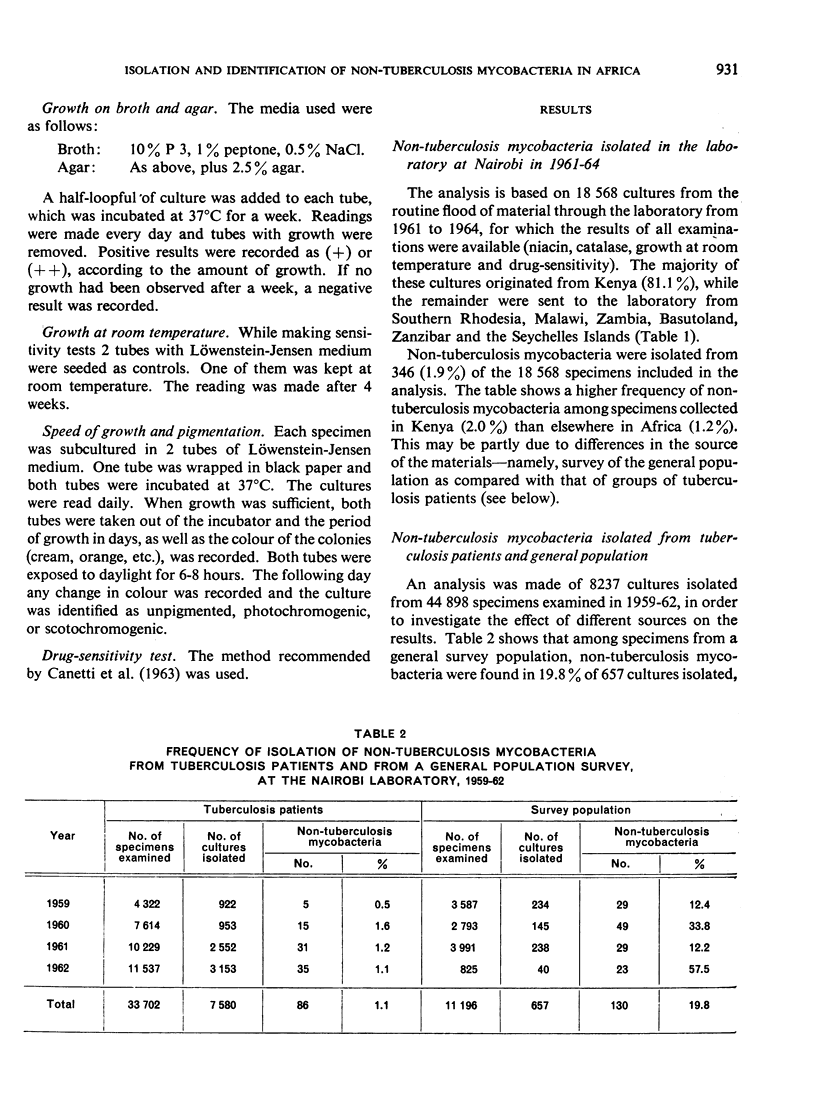
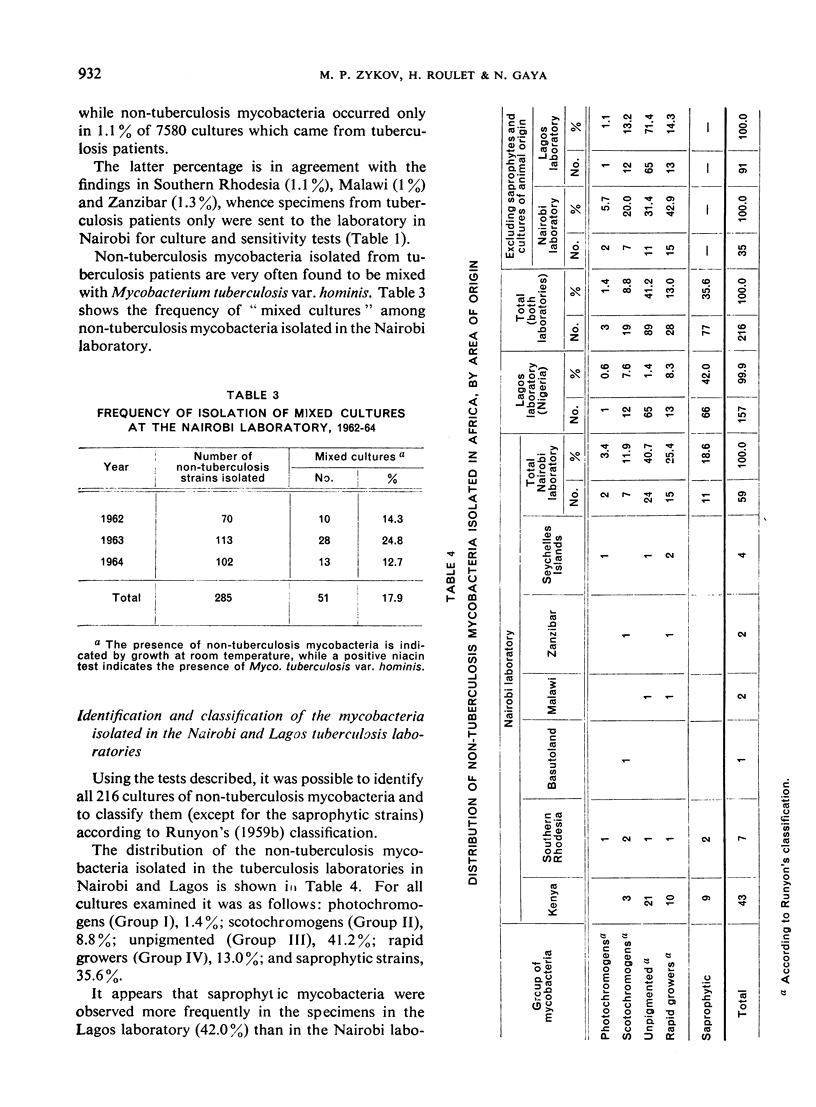
Of 18 568 cultures examined at the Central Tuberculosis Laboratory, Nairobi, in 1961-64, 1.9% were non-tuberculosis strains. However, valid conclusions as to prevalence cannot be drawn from this figure, since some specimens came from tuberculosis patients and others from general population surveys. An earlier comparison, based on 7580 cultures from tuberculosis patients and 657 from a random survey, had shown a significant difference in the frequency of non-tuberculosis strains, the figures being 1.1% and 19.8%, respectively.
Of the identification tests studied, the formamidase test was found very useful for differentiating saprophytic mycobacteria from the other non-tuberculosis mycobacteria, particularly the rapid growers. This test is discussed in greater detail in the third study of the series.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- LANYI M. The isolation of chromogenic mycobacteria from laryngeal cultures. J Clin Pathol. 1958 Jan;11(1):69–70. doi: 10.1136/jcp.11.1.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MAGARAO M. F., LORIAN V. [Abnormal mycobacteria in our pneumological practice]. Acta Tuberc Pneumol Scand. 1962;41:252–259. [PubMed] [Google Scholar]
- MALLMANN V. H., MALLMANN W. L., ROBINSON P. RELATIONSHIP OF ATYPICAL BOVINE AND PORCINE MYCOBACTERIA TO THOSE OF HUMAN ORIGIN. Health Lab Sci. 1964 Jan;1:11–20. [PubMed] [Google Scholar]
- MUFTIC M. MODIFIED TECHNIQUE FOR FORMAMIDASE TEST IN MYCOBACTERIA. Acta Tuberc Pneumol Scand. 1964;44:250–252. [PubMed] [Google Scholar]
- NAGAYAMA H., KONNO K., OKA S. Formamidase in Mycobacteria and its use in differentiating saprophytic Myco-bacteria from other Mycobacteria. Nature. 1961 Jun 24;190:1219–1220. doi: 10.1038/1901219a0. [DOI] [PubMed] [Google Scholar]
- RUNYON E. H. Anonymous mycobacteria in pulmonary disease. Med Clin North Am. 1959 Jan;43(1):273–290. doi: 10.1016/s0025-7125(16)34193-1. [DOI] [PubMed] [Google Scholar]
- Zykov M. P., Donec J. I., Godovannyi B. A. Non-tuberculosis mycobacteria in Africa. 2. Sensitivity to mycobacteriophages. Bull World Health Organ. 1967;37(6):939–946. [PMC free article] [PubMed] [Google Scholar]
- Zykov M. P., Roulet H. Non-tuberculosis mycobacteria in Africa. 3. Formamidase activity--its evaluation and practical application. Bull World Health Organ. 1967;37(6):947–951. [PMC free article] [PubMed] [Google Scholar]


