Abstract
The U.S. health care system is one of the world's most advanced systems. Yet, the health care system suffers from unexplained practice variations, major gaps between evidence and practice, and suboptimal quality. Although information processing, communication, and management are key to health care delivery and considerable evidence links information/communication technology (IT) to improvements in patient safety and quality of care, the health care system has a longstanding gap in its investment. In the Crossing the Quality Chasm and Building a Better Delivery System reports, The Institute of Medicine and National Academy of Engineering identified IT integration as critical to improving health care delivery systems. This paper reviews the state of IT use in the U.S. health care system, its role in facilitating evidence-based practices, and identifies key attributes of an ideal IT infrastructure and issues surrounding IT implementation. We also examine structural, financial, policy-related, cultural, and organizational barriers to IT implementation for evidence-based practice and strategies to overcome them.
Keywords: information technology, implementation, evidence-based practices
The U.S. health care system is a $1.6-trillion industry that is undergoing rapid changes, facing increasing market pressure and competition for scarce resources.1 The industry involves multiple private and public stakeholders, including provider associations, health care delivery organizations, insurers, consumers, community networks, and local, state, and federal agencies. It is an information intensive industry,2 and yet it has lagged behind other industries in its investments and use of communication and information technology (IT).3–5
The acquisition and implementation of IT have great implications for the operations of health care organizations because of: (1) rapidly rising health care costs; (2) escalating concerns surrounding issues of patient safety and medical errors; (3) call for improving the provision of evidence-based care; and (4) increasing regulatory requirements.2,6 In particular, the Institute of Medicine (IOM) and the National Academy of Engineering have identified IT as crucial for building an improved health care delivery system that achieves the 6 health system 21st century attributes of being safe, effective, patient-centered, timely, efficient, and equitable.3 Industry groups outside of health care, such as the Leapfrog Group, as well as the U.S. government, have encouraged IT investments as a solution to reduce medication errors and patient safety problems.7–9 IT use has been shown to yield significant improvements in quality, cost containment, and patient safety in several empirical studies.10–12 However, relatively little research has focused on identifying effective approaches for IT implementation and applications in evidence-based practices (EBPs). Evidence-based practice is the process of using current best evidence from well-designed research conscientiously and judiciously, in conjunction with patient values and clinical expertise, to guide health care decisions.
To explore these issues, Veterans Health Administration (VHA) convened a State-of-the-Art Conference (SOTA) on “Implementing the Evidence: Transforming Practices, Systems, and Organizations” in December 2004. This synthesis of literature was undertaken as background to the SOTA conference. Given the limited amount of information in this area, evidence for this project came from: (1) MEDLINE search and review of published literature; (2) general world wide web search; and (3) expert opinions from discussions of the paper at the SOTA workshop. Our objectives in this paper are to: (1) provide a summary of current IT implementation efforts and its role in facilitating EBPs; (2) identify key stakeholder issues and barriers surrounding IT implementation to support EBPs; and (3) outline strategies for IT implementation and management to support EBPs as part of a better delivery system. Although other nations have also launched IT implementation efforts,13,14 our literature synthesis will focus exclusively on the U.S. health care system.
DEFINITION AND CURRENT APPLICATIONS OF IT
Information technology is defined as the development, installation, and implementation of computer systems and applications, including hardware, software, networking, and communication tools. In the past decade, IT development activities within the health care industry have increased as executives and providers recognized the urgent need for strategic information management and inadequacies of traditional information storage, retrieval, and analysis tools.15,16 However, most IT investments in health care have focused on administration rather than care delivery.
Current IT applications in the health care industry can be divided into 3 categories: (1) infrastructure, such as electronic health records (EHRs) as storage and retrieval systems, automated mechanisms for capturing data, and an electronic library of medical literature; (2) performance enhancement, such as computer-based clinical decision support (CDS) systems, continuing medical and patient education; and (3) performance evaluation, such as demonstration and measurement of the cost, effectiveness, and outcomes of different systems.15,16 All 3 applications can support the delivery of EBPs. In general, most health care information systems are composed of automated billing and financial management, patient admission, discharge, transfers and registration, coordination of communications infrastructure, claims processing, customer service, and electronic data sharing.2
CURRENT IT IMPLEMENTATION TRENDS
The establishment of a national health information infrastructure is considered a top priority. During fiscal year 2004, the president requested $50 million for IT projects related to patient safety and $12 million to develop IT standards. The Agency for Healthcare Research and Quality allocated $60 million in 2004 to promote research and demonstrations to advance IT use for care improvement.6,17 Similarly, the Food and Drug Administration proposed new regulations for bar coding medications to potentially reduce medication errors.
From a financial perspective, the implementation of a national health information infrastructure could yield as much as $142–371 billion in savings for the health care system.6 From a human perspective, improved IT use in care delivery may help prevent the multiple deaths that are expected to occur because of medical errors.18 Efforts in IT use may intensify as requirements to address administrative simplification emanated from the Health Insurance Portability and Accountability Act impel the health care industry to use more efficient and standardized electronic communications.2,6 More efficient coordination of information and communication could better support the delivery of EBPs. However, important technical, cost, organizational, social, and policy issues remain to be resolved before IT systems could be widely adopted and implemented. Table 1 outlines priorities according to expert opinion in IT implementation, and identifies barriers and strategies to promote EBPs.
Table 1.
Priorities, Barriers, and Strategies to Effective Implementation of Information Technology (IT) Applications Supporting Evidence-Based Practice and Management
| Priority | Barriers | Strategies |
|---|---|---|
| Priority 1: | ||
| Support knowledge-based decisions | Information and provider overload | Research on prioritization Research to include data on added value in terms of mortality and morbidity |
| Lack of integration | National patient data record Patient ownership of patient data, guidelines, and reminders Common patient identifier Common provider identifier Integration across systems Research on what information users need | |
| Operationalizing evidence | Basic research in managing information complexity Alignment of research priorities with clinical management Performance measures focused on how much evidence informs practice Regular presentation of significant translation research findings to senior leadership | |
| Priority 2: | ||
| Reporting/evaluation functions | Threats to provider autonomy | Flexibility in decision support with required feedback about reasons for non-compliance and barriers to compliance Local review of compliance with local solutions (tailored training)Add autonomy in other areas: e.g., guideline input, self-review, link to reference materials |
| Data issues | More data automation (e.g., link diagnosis to test)Review and monitoring of data quality Linkages to other information in electronic health record to eliminate duplicate entry | |
| Reporting complexity | Move reports off system—put analytical tools on a system separate from patient care system | |
| System resources | Simplify user generation of report | |
| Priority 3: | ||
| Information system needs to evolve with health care system | Emphasis on provider-level activities and provider-entered data | Develop patient-centered data collection methods, core data elements, and system capacity for patient-based health data sets Encourage basic research on capturing home care data for all stakeholders |
| Emphasis on workload rather than care received by patient | Focus on outcomes (maintaining/improving functional status of the patient), not workload Encourage “just in time” rather than “just in case” visits, collect interim data remotely | |
Adapted from discussion of the white paper by attendees at the Department of Veterans Affairs State-of-the-Art Conference in August 2004.
Currently, the VA medical system has the most broadly implemented federal health IT system. The VA also launched the Quality Enhancement Research Initiative (QUERI) in the late 1990s, designed to integrate care delivery, quality improvement (QI), and health services research to identify and implement EBPs in routine care settings for individuals with chronic illness.19,20 The VA has successfully used IT within its health care system to improve quality through the use of clinical reminders,21 EHRs, and other innovative approaches.20 However, the VA's information system currently lacks rigorous data standards, which limits the sharing and usability of data across health information systems and in QI.22,23
IT AND THE IMPLEMENTATION OF NEW EVIDENCE
Major efforts are warranted to reengineer health care in the United States to improve quality, safety, and bridge the gap between evidence and practice.8,24,25 The President's Information Technology Advisory Committee (PITAC) attributes the gap between evidence and practice to a number of problems inherent in care delivery.22 On an individual level, providers cannot maintain or consider all details of patients' medical history, or all best medical practices needed in order to deliver optimal care.26 Moreover, ready access to patient data for medical decision-making is often unavailable at the point of care. On a system level, there is urgent need for change in how health care is organized and delivered to make it more evidence based.
Synthesizing recommendations from the IOM's Quality Chasm report, 5 priority areas have been identified to bridge this gap, including building organizational support for change, applying evidence to health care delivery, developing IT, aligning payment policies with QI, and preparing the workforce.27 In addition to enhancing information access and supporting decision making, IT may help meet other objectives, particularly the delivery of EBPs.3 The informatics infrastructure needed for EBP includes data acquisition methods, health care standards including standardized terminologies, data repositories, clinical event monitors, data-mining techniques, digital sources of evidence, and communication technologies.28,29Table 2 identifies attributes of an ideal IT system to support EBP and health care delivery.
Table 2.
Attributes of the Ideal Information System to Support Evidence-based Practice
| I. Attributes related to the information technology (IT) system |
| The IT system is |
| Usable |
| Flexible |
| Integrated |
| All electronic |
| Transparent to users |
| Non-intrusive |
| Easily up-datable |
| Reliable |
| Equitable: “No service/facility left behind” |
| Dynamic |
| Sustainable |
| Current contents |
| Secure |
| Accurate |
| Correct contents |
| Timely |
| Standardized |
| Compatible with other systems |
| II. Functionality of the ideal IT system |
| The IT system: |
| Supports knowledge-based decisions |
| Supports shared clinical decision-making |
| Provides evaluation and reporting capabilities |
| Evolves with the health care system |
| Has defined accountability (e.g., organization vs provider) |
Adapted from discussion of the white paper by attendees at the Department of Veterans Affairs State-of-the-Art Conference in August 2004.
The President's Information Technology Advisory Committee has proposed a framework for a 21st century health care IT infrastructure with 4 key elements: (1) readily available EHRs to equip patients and providers to share the decision-making in making health care decisions; (2) CDS to use state of the art knowledge in making treatment decisions; (3) computerized provider order entry (CPOE) for tests, medicine, and procedures; and (4) secure, private, interoperable, electronic health information exchange.22 Additional IT applications supporting the implementation of EBP include population-based care systems, and functional baseline estimates against which future information system enhancements can be measured.30 All of these tools coordinate information dissemination and sharing from various databases to equip the provider in providing patient-specific, appropriate, timely, and evidence-based care.3,22Table 3 provides examples of how potential IT applications can support EBPs.
Table 3.
Information Technology (IT) Applications Supporting Evidence-based Practice and Management
| Application | Utility | Support for EBPs |
|---|---|---|
| Population-based health care systems | These systems support creation of large, integrated databases of patient-specific information that allow real-time management of populations of similar patients | These databases may facilitate evaluation of new implementation strategies and provide insights into new associations between management approaches and health states |
| Computer-based decision support | Clinical decision support (CDS) may help health care providers utilize state-of-the-art medical knowledge in treatment decisions | CDS provides information management tools for the acquisition, manipulation, application, distribution, and display of appropriate patient- and task-specific clinical data to providers and patients that is conducive to correct, timely, and evidence-based clinical decision-making |
| Computerized provider order entry | Computerized provider order entry (CPOE) can help the tracking and analysis of health care processes | CPOE for tests, medicine, and procedures has the potential to decrease medical error, improve quality. It can help provider coordinate and collect patient-specific information |
| Electronic health records | Electronic health records (EHRs) would equip patients with personal health data, reliable patient-specific tools and resources | EHRs provide every patient and their caregivers with the necessary information required for optimal care. They can help patients to better understand the complexity of medical care and more readily participate in clinical decision-making and preventive health behaviors |
| Electronic health information exchange | This exchange ensures security, privacy, and system compatibility | The exchange between organizations would facilitate sharing patient information at the point of the care delivery to eliminate unnecessary testing, improve safety, and facilitate efforts to improve quality |
Adapted from the Kaiser Permanente's Agenda for Clinical Information System Research.30
Nevertheless, evidence describing IT's impact on EBPs has been mixed. Shea et al.'s metaanalyses reported that improvement in preventive care such as vaccinations and cancer screenings can be attributed to the use of clinical reminders.31–33 On the other hand, the evidence on the effect of CDS on practice is quite variable. Hunt et al.'s analysis noted that while a number of studies showed a correlation between CDS and improved clinical performance, some did not find any benefit.32,34 Further evaluation and more evidence are needed to assess the utility of these IT tools and determine how best to design and implement them to support EBPs.
ISSUES IN IT IMPLEMENTATION
Tan and Modrow have advocated for overall industry performance standards or measures, in order to define accountability expectations for IT.35,36 As IT becomes more integrated into the care delivery system, IT implementation is likely to expand to include other participants in the health care setting. The IT system needs to interface with, and be responsive to, patients, managers, providers, researchers, and the public. Key stakeholder groups, including managers, providers, and other clinicians, patients, and health care organizations, have identified different barriers and facilitators to IT use in improving EBPs. Therefore, any IT implementation plans should address concerns of the stakeholders in order to build a better system.35
Clinician/Provider Issues
The utilization of IT in health care delivery systems depends upon IT availability and acceptance by health care providers. In the next few years, the most important IT clinical applications are likely to include CPOE, clinical information systems, CDS, and improved medication management.2 Providers, other clinicians, and managers share many concerns regarding the use of IT in implementing EBPs.33,35
An example of an important clinician issue is that outpatient laboratory test results are often not reviewed and acted upon within reasonable time frames.37 Clinicians desire a system that allows them to review and act upon test results safely and efficiently. Clinical decision support for laboratory test results might be used to classify the extent of abnormality for given results, provide context-appropriate advice to help manage abnormal results, generate letters to patients using templates, and help set reminders for follow-up testing.37
Taking full advantage of IT may require a team approach, where active involvement of interdisciplinary groups of providers and users is important. For example, to achieve maximum medication safety, introducing a CPOE system with advanced CDS, as well as involving both clinical pharmacists and other providers, may be particularly effective.38
Patient Issues
Patient-centered care, defined as care that elicits, respects, and incorporates patients' wishes and maximizes patients' subjective outcomes, is increasingly recognized as an important dimension of health care quality. In promoting patient-centered care, IT provides opportunities to enhance patient-provider interactions and patients' use of their own health data. Information technology use may empower patients in their exchange with providers and promotes the alignment of care between hospital/clinics and patients' home.39 Furthermore, IT tools may facilitate patient education and activation in enhancing the patient's role as an active participant in the care process.
Information technology provides patients with chronic conditions new tools to manage their illness. For example, a “Home Telecare System” that integrates clinical signs monitoring, automated scheduling, and medication reminders, access to health education, and daily logs, can help patients self-manage their chronic disease.40 There are also a number of examples of systems that facilitate patient-EHR interactions and studies have shown a benefit to having patients view their medical data.40–42
As IT development accelerates, and access to information and interface capability increases, there is increasing opportunity to engage patients in further IT use. Information technology resources that are currently available to patients range from general information to personalized tools. For example, static web sites (e.g., WebMD, American Diabetes Association, etc.) can disseminate disease-specific information to a broad audience. Interactive web sites (e.g., Care Wise, Caresteps, E-Diets) can create community platforms for information sharing between providers and patients as well as for the dissemination of educational information to targeted patient cohorts.
New devices are being developed and tested to enhance individually tailored disease management. For example, biometric devices, which are home-based measurement devices that monitor and collect daily readings and symptom information, are increasingly used in care delivery.42 Handheld devices (e.g., personal digital assistants) allow patients to track daily progress such as weight and medications. Connectivity-facilitated workflow management, which deploys clinical and administrative workflow support through web-based connectivity among health plans, physician offices, and hospitals, gives patients customized, real-time delivery of alerts, guidelines, reminders, and other targeted information at the point of care.42
Emerging technology has the potential to increase patient participation in IT-facilitated, evidence-based, patient-centered care. Obtaining regular patient input in the design of health care IT systems can facilitate making the EHR responsive to patients needs.41
Organizational Issues
Within the health care industry, over one half of health care executives identified the top IT priority as implementation.2 However, most health care organizations are still at the stages ranging from considering adoption through early implementation.43,44 The lack of financial support for widespread IT applications is considered a primary barrier to its implementation by both managers and clinicians.2,45 The financial burden of implementation, including acquisition and implementation costs, slow and uncertain financial payoffs, and disruption to clinical practices, is directly related to both the size of organization and its readiness for conversion.46,47
The complexity of IT implementation not only requires significant resource investment by the organization, but it also involves many levels of personnel and system interaction and management, representing a major organizational change effort. Case studies in hospitals that have implemented advanced clinical information systems with extensive CDS provide important lessons. Implementation of some systems have been well accepted by providers and managers and have improved clinical processes, whereas there have also been significant and costly failures. Successful implementation requires leadership, a long-term commitment to improving and documenting health care processes, and efforts to involve clinicians and sustain productivity.48
In health care organizations, using IT for clinical documentation and order entry may provide an opportunity to improve processes of care and capture QI efforts into data warehouses to support better care delivery systems.49 Using IT systems to document and generate performance measures may make the accreditation processes with agencies such as the Joint Commission on Accreditation of Healthcare Organizations, Centers for Medicare & Medicaid Services, the National Center for Quality Assurance, and the National Quality Forum, more efficient.49 In addition, the use of IT tools has the potential to facilitate networking and benchmarking among collaborating health care organizations.50 However, health care organizations need to adopt these applications with caution as unexpected inaccuracies or problems with data collection, entry, and processing may arise.
Human Factors Issues
Human factors such as product usability, process complexity, and user-engagement methods routinely influence IT uptake.51 Prior experience with an IT application, different implementation approaches, and differential utility of structured data entry, can also influence user satisfaction.52 Notably, significant concerns remain regarding liability, patient electronic communication, and reimbursement.53
New IT solutions are often not adequately piloted, tested, and revised for usability in care prior to deployment. It is crucial to regularly observe user-IT interactions, particularly in the development phase. For example, in evaluating clinical reminders use, ease of use, access to workstations, perceived value, and relative benefits to administrators versus clinicians all impact their uptake.21,54,55 Similarly, in using a CDS system to set the dosage of anticoagulant and time interval to the next appointment, nurses found it stressful to override program-generated recommendations.56
MANAGEMENT AND IMPLEMENTATION STRATEGIES
As IT is accepted and adopted by more health care organizations, challenges remain in the area of IT management and appropriate implementation. Much of the present discussions in the literature have focused on the correlation between IT and outcomes of care processes or behavior modification, whereas information on IT management has been limited. Based on our literature synthesis and expert opinions, we summarized some potential strategies for IT management and implementation.
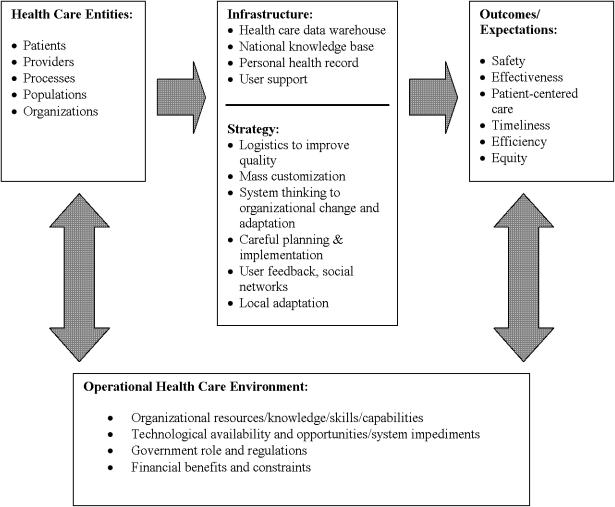
Information technology management encompasses the health care entities it serves, its infrastructure, strategies for use, and expected outcomes (Fig. 1). The context in which IT management is examined should consider key dimensions of the health care delivery system (patient and families, providers, organizations, patient populations, clinical knowledge, and care processes), the environment in which the organizations operate, as well as QI and evidence implementation efforts.30,57 Components of an informatics infrastructure to promote EBP, such as a health care data warehouse, knowledge database, personal health records, and user support, have demonstrated promising results in the limited settings in which they have been formally evaluated.29
Figure 1.
Framework and context for IT management and implementation.
Information technology management may involve issues emanated from both within the organization and with other organizations. Within an organization, Simpson58 has suggested that effective IT management should take into account the 3 “Ps:” people, process, and programs. To achieve “buy-in” from potential IT users, coordination among providers, a formal process to provide technical support for individual users, programs to integrate IT into workflow, and the ability to document system problems and obtain prompt administrator feedback are essential.59–61 Strategies that are related to the people, process, and program dimensions of IT management are further elaborated in Table 4.2
Table 4.
Key Dimensions of Information Technology (IT) Management For Supporting Evidence-based Practice
| Dimensions | Management Issues |
|---|---|
| People | Prepare organizational participants for major change, manage differences in proficiency, and invest in change management |
| Devote “just-in-time” training to changes in work flow and process | |
| Create the right IT environment with proven management and leadership skills, dedicated IT staff, and respected clinical staff | |
| Establish programs to enhance participation and perceived ownership of the system | |
| Continuously monitor and address users' concerns | |
| Process | Identify ways to achieve efficiencies in system use and to evaluate benefits |
| Determine routing of patient requests to appropriate providers within an integrated delivery system | |
| Include patient care guidelines for prevention, diagnosis, and treatment to provide clinicians with information more efficiently | |
| Understand and incorporate clinical workflow | |
| Exploit system capabilities for staff, reengineering workflow | |
| Ensure consistent leadership and provide support and feedback | |
| Define proactive strategies to report and solve problems in IT applications in care | |
| Establish collaborative relationships with the IT vendor, management, and clinical leadership | |
| Programs | Configure the hardware and equipment to be conducive to performing manual tasks associated with the process (e.g., system software is compatible with tasks such as counseling patients) |
| Recognize the importance of managing security and confidentiality issues | |
| Provide real-time user support at all times | |
| Combine IT and operations | |
| Provide a robust, secure, available system and infrastructure to ensure user acceptance | |
| Tools usable enough to deliver benefits and support the delivery of health care, education, and cost control |
Adapted from the General Accounting Office Briefing (2003).
When interorganizational exchange occurs, IT management needs to focus on secure and affordable information exchange, which requires the adoption of appropriate technology and personnel training.2 This is a high priority strategy for health systems and government leadership nationally. Effective interorganizational exchange among various participants (e.g., physicians, other providers, hospitals, payers, and ancillary services) may lead to cost savings in labor and improved QI outcomes for all organizations.
A number of strategies have been suggested to facilitate IT implementation in health care settings. A crucial first step for the organization in the implementation process is to assess both current information-management capabilities and estimate future needs.62,63 Equally important is the assessment of readiness for major organizational change, such as the ability to invest in change management and training, as well as the culture and processes needed to support implementation.64 Information technology systems to be implemented need to align with processes within the health care organization to allow evolution and adaptation.65 One way to assess readiness is to employ a readiness assessment tool that can help the organization's decision making regarding IT implementation. Important factors for readiness assessment include external environment, organizational leadership, structure, and culture, care standardization, order management, access to information, information technology composition, and infrastructure.64
It has been suggested that efforts involved in successful IT implementation consist primarily (75% to 90%) of social engineering and less (20% to 25%) of technical implementation.2 Therefore, IT implementation requires individual participation and trust and system-level support. On an individual level, the organization and its management need to involve end users' input in improving their work practices. They also need to consider other factors, such as the usability, usefulness, and flexibility of IT tools and individualized training that will influence uptake.59–61 On a system level, a supportive culture, visibility of positive results from IT use, and a realistic timeline will enhance implementation.59–61 Developing and installing feedback and monitoring mechanisms, as IT is being adopted, implemented, and maintained provides opportunities for continual improvement.66 As tools for rapid application development are refined, they will increasingly allow IT infrastructures to be responsive and concentrate on process alignment and incorporation of evidence into practice.65
Lastly, IT implementation requires the support and resources of the organization and its management. As most health care systems have limited resources for QI, resource allocation warrants close examination to maximize the benefits of IT use and, in turn, the delivery of safe, effective, efficient, and high-quality care. Factors influencing organizational decisions surrounding IT implementation need to explore the following: (1) which clinical conditions, practices, and settings are likely to benefit from IT implementation; (2) which is the greatest evidence gap present; and (3) what are the expected costs and benefits of introducing EBPs or new IT to support adherence?25 IT implementation should be tailored to the needs of the organization, and not as a “one size fits all” solution. A balanced assessment of effectiveness and costs of the IT system is needed to make the implementation effort a successful one.
Acknowledgments
The authors appreciate comments on the draft white paper from Denise Hynes, RN, PhD, and discussion of the issues surrounding it by experts at the Veterans Health Administration (VHA) State-of-The-Art Conference: “Attributes of an Ideal Integrated Informatics System that Supports Implementation of Evidence,” VHA State of the Art Conference (SOTA) VII, Implementing the Evidence: Transforming Practices, Systems, and Organizations, Washington, DC, August 2004. Responsibility for the positions outlined in the manuscript reside with the authors.
The authors acknowledge grant support during the preparation of this review, including Department of Veterans, the Veterans Health Administration, Health Services Research and Development Service, Investigator Initiated Research (IIR) Grants CPI -01-141 (“Determinants of Clinical Guideline Implementation Effectiveness”), Epidemiology Merit Review (“Epidemiology and Control of Antimicrobial Resistance in Hospitals”), IIR Grant (“Economic Effects of Clinical Practice Guidelines”), Management Consultation Project (“Current Barriers and Facilitators to Use of Automated Clinical Reminders”), (“Information Management for Patient-Centered Treatment ([IMPACT[),” Infrastructure Grant # REA 03–278, and HSR&D Center Grant #HFP 04-148.
REFERENCES
- 1.Kaiser Family Foundation and Health Research and Educational Trust. Employer Health Benefits 2003 Annual Survey. Kaiser Family Foundation. [December 2004]. Available at http://www.kff.org/insurance/ehbs2003-1-set.cfm 2003.
- 2.General Accounting Office. Use of Information Technology for Selected Health Care Functions. Washington, DC: Briefing for the Minority Staff of the Senate Committee on Health, Education, Labor, and Pensions; 2003. [Google Scholar]
- 3.Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- 4.Kaushal R, Shojania KG, Bates DW. Effects of computerized physician order entry and clinical decision support systems on medication safety: a systematic review. Arch Intern Med. 2003;163:1409–16. doi: 10.1001/archinte.163.12.1409. [DOI] [PubMed] [Google Scholar]
- 5.Reid PP, Compton D, Grossman JH, Fanjiang G. Committee on Engineering and the Health Care System. Building a Better Delivery System: A New Engineering/Health Care Partnership. Washington, DC: National Academy Press; 2005. [Google Scholar]
- 6.The Commonwealth Fund. How Information Technology Can Improve Health Care Quality: Core Lessons. Washington, DC: Alliance for Health Reform/Commonwealth Fund Roundtable; 2003. [Google Scholar]
- 7.Morrissey J. An info-tech disconnect. Even as groups such as Leapfrog push IT as an answer to quality issues, doctors and executives say, “not so fast.”. Mod Healthcare. 2003;33:6–7. [PubMed] [Google Scholar]
- 8.Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2003. [PubMed] [Google Scholar]
- 9.Cors WK. Physician executives must leap with the frog. Accountability for safety and quality ultimately lie with the doctors in charge. Physician Exec. 2001;27:14–6. [PubMed] [Google Scholar]
- 10.Bates DW, Leape LL, Cullen DJ, et al. Effect of computerized physician order entry and a team intervention on prevention of serious medication errors. JAMA. 1998;280:1311–6. doi: 10.1001/jama.280.15.1311. [DOI] [PubMed] [Google Scholar]
- 11.Bates DW, Teich JM, Lee J, et al. The impact of computerized physician order entry on medication error prevention. J Am Med Inform Assoc. 1999;6:313–21. doi: 10.1136/jamia.1999.00660313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barlow S, Johnson J, Steck J. The economic effect of implementing an EMR in an outpatient clinical setting. J Healthc Inf Manag. 2004;18:46–51. [PubMed] [Google Scholar]
- 13.Pagliari C. E-Health scoping exercise: review of the traditional research literature. 2005. The Service Delivery and Organization Programme, National Health Services.
- 14.Pagliari C. E-health scoping exercise: review of wider web-based information sources. 2005 Service Delivery and Organization Programme, National Health Services. [Google Scholar]
- 15.Altman RB. Ten grand challenges for medical informatics. [December 2004]. Available at http://www.smi.stanford.edu/pubs/smi_reports/smi-96-0655.pdf.
- 16.McDonald CJ, Overhage JM, Dexter PR, et al. Canopy computing: using the web in clinical practice. JAMA. 1998;280:1325–9. doi: 10.1001/jama.280.15.1325. [DOI] [PubMed] [Google Scholar]
- 17.Hillestad R, Bigelow J, Bower A, et al. Can electronic medical record systems transform health care? Potential health benefits, savings, and costs. Health Aff (Millwood) 2005;24:1103–17. doi: 10.1377/hlthaff.24.5.1103. [DOI] [PubMed] [Google Scholar]
- 18.Reuters. Report says 1,95,000 deaths due to hospital error. 7-27-2004. [December 2004]. Available at http://reuters.com/printerFriendly.
- 19.McQueen L, Mittman BS, Demakis JG. Overview of the veterans health administration (VHA) quality enhancement research initiative (QUERI) J Am Med Inform Assoc. 2004;11:339–43. doi: 10.1197/jamia.M1499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hynes DM, Perrin RA, Rappaport S, Stevens JM, Demakis JG. Informatics resources to support health care quality improvement in the veterans health administration. J Am Med Inform Assoc. 2004;11:344–50. doi: 10.1197/jamia.M1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fung CH, Woods JN, Asch SM, Glassman P, Doebbeling BN. Variation in implementation and use of computerized clinical reminders in an integrated healthcare system. Am J Manag Care. 2004;10:878–85. [PubMed] [Google Scholar]
- 22.President's Information Technology Advisory Committee. 2004. Revolutionizing Health Care through Information Technology. 6–1–.
- 23.Weaver FM, Hatzakis M, Evans CT, et al. A comparison of multiple data sources to identify vaccinations for veterans with spinal cord injuries and disorders. J Am Med Inform Assoc. 2004;11:377–9. doi: 10.1197/jamia.M1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kuperman GJ, Gibson RF. Computer physician order entry: benefits, costs, and issues. Ann Intern Med. 2003;139:31–9. doi: 10.7326/0003-4819-139-1-200307010-00010. [DOI] [PubMed] [Google Scholar]
- 25.Grimshaw JM, Thomas RE, MacLennan G, et al. Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technol Assessment (Winchester, England) 2004;8:iii–iv. doi: 10.3310/hta8060. [DOI] [PubMed] [Google Scholar]
- 26.Miller GA. The magical number seven plus or minus two: some limits on our capacity for processing information. Psychol Rev. 1956;63:81–97. [PubMed] [Google Scholar]
- 27.Fernandopulle R, Ferris T, Epstein A, et al. A research agenda for bridging the “quality chasm. Health Aff (Millwood) 2003;22:178–90. doi: 10.1377/hlthaff.22.2.178. [DOI] [PubMed] [Google Scholar]
- 28.Bakken S, Hripcsak G. An informatics infrastructure for patient safety and evidence-based practice in home healthcare. J Healthc Qual. 2004;26:24–30. doi: 10.1111/j.1945-1474.2004.tb00492.x. [DOI] [PubMed] [Google Scholar]
- 29.Bakken S, Cimino JJ, Hripcsak G. Promoting patient safety and enabling evidence-based practice through informatics. Med Care. 2004;42(suppl 2):II49–56. doi: 10.1097/01.mlr.0000109125.00113.f4. [DOI] [PubMed] [Google Scholar]
- 30.Sittig DF, Hazlehurst BL, Palen T, Hsu J, Jimison H, Hornbrook MCA. Clinical information system research agenda for kaiser permanente. Permanente J. 2002;6:41–4. [Google Scholar]
- 31.Shea S, DuMouchel W, Bahamonde L. A meta-analysis of 16 randomized controlled trials to evaluate computer-based clinical reminder systems for preventive care in the ambulatory setting. J Am Med Inform Assoc. 1996;3:399–409. doi: 10.1136/jamia.1996.97084513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hunt DL, Haynes RB, Hanna SE, Smith K. Effects of computer-based clinical decision support systems on physician performance and patient outcomes: a systematic review. JAMA. 1998;280:1339–46. doi: 10.1001/jama.280.15.1339. [DOI] [PubMed] [Google Scholar]
- 33.Litzelman DK, Dittus RS, Miller ME, Tierney WM. Requiring physicians to respond to computerized reminders improves their compliance with preventive care protocols. J Gen Intern Med. 1993;8:311–7. doi: 10.1007/BF02600144. [DOI] [PubMed] [Google Scholar]
- 34.Johnston ME, Langton KB, Haynes RB, Mathieu A. Effects of computer-based clinical decision support systems on clinician performance and patient outcome. A critical appraisal of research. Ann Intern Med. 1994;120:135–42. doi: 10.7326/0003-4819-120-2-199401150-00007. [DOI] [PubMed] [Google Scholar]
- 35.Lyons SS, Tripp-Reimer T, Sorofman BA, et al. VA QUERI informatics paper: information technology for clinical guideline implementation: perceptions of multidisciplinary stakeholders. J Am Med Inform Assoc. 2005;12:64–71. doi: 10.1197/jamia.M1495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tan JK, Modrow RE. Strategic relevance and accountability expectations: new perspectives for health care information technology design. Top Health Inf Manag. 1999;19:84–97. [PubMed] [Google Scholar]
- 37.Poon EG, Wang SJ, Gandhi TK, Bates DW, Kuperman GJ. Design and implementation of a comprehensive outpatient results manager. J Biomed Inform. 2003;36:80–91. doi: 10.1016/s1532-0464(03)00061-3. [DOI] [PubMed] [Google Scholar]
- 38.Bobb A, Gleason K, Husch M, Feinglass J, Yarnold PR, Noskin GA. The epidemiology of prescribing errors: the potential impact of computerized prescriber order entry. Arch Intern Med. 2004;164:785–92. doi: 10.1001/archinte.164.7.785. [DOI] [PubMed] [Google Scholar]
- 39.Nebeker JR, Hurdle JF, Bair BD. Future history: medical informatics in geriatrics. J Gerontol A Biol Sci Med Sci. 2003;58:M820–5. doi: 10.1093/gerona/58.9.m820. [DOI] [PubMed] [Google Scholar]
- 40.Celler BG, Lovell NH, Basilakis J. Using information technology to improve the management of chronic disease. Med Dir Aust. 2003;179:242–6. doi: 10.5694/j.1326-5377.2003.tb05529.x. [DOI] [PubMed] [Google Scholar]
- 41.Beun JG. Electronic healthcare record: a way to empower the patient. Int J Med Inform. 2003;69:191–6. doi: 10.1016/s1386-5056(03)00060-1. [DOI] [PubMed] [Google Scholar]
- 42.Nobel JJ, Norman GK. Emerging information management technologies and the future of disease management. Dis Manag. 2003;6:219–31. doi: 10.1089/109350703322682531. [DOI] [PubMed] [Google Scholar]
- 43.Rogers EM. Lessons for guidelines from the diffusion of innovations. Jt Comm J Qual Improv. 1995;21:324–8. doi: 10.1016/s1070-3241(16)30155-9. [DOI] [PubMed] [Google Scholar]
- 44.Rogers EM. A prospective and retrospective look at the diffusion model. J Health Commun. 2004;9(suppl 1):13–9. doi: 10.1080/10810730490271449. [DOI] [PubMed] [Google Scholar]
- 45.Valdes I, Kibbe DC, Tolleson G, Kunik ME, Petersen LA. Barriers to proliferation of electronic medical records. Inform Prim Care. 2004;12:3–9. doi: 10.14236/jhi.v12i1.102. [DOI] [PubMed] [Google Scholar]
- 46.Goldsmith J, Blumenthal D, Rishel W. Federal health information policy: a case of arrested development. Health Aff (Millwood) 2003;22:44–54. doi: 10.1377/hlthaff.22.4.44. [DOI] [PubMed] [Google Scholar]
- 47.Miller RH, Sim I. Physicians' use of electronic medical records: barriers and solutions. Health Aff (Millwood) 2004;23:116–26. doi: 10.1377/hlthaff.23.2.116. [DOI] [PubMed] [Google Scholar]
- 48.Doolan DF, Bates DW, James BC. The use of computers for clinical care: a case series of advanced U.S. sites. J Am Med Inform Assoc. 2003;10:94–107. doi: 10.1197/jamia.M1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Johnson T, Ventura R. Applied informatics for quality assessment and improvement. J Nurs Care Qual. 2004;19:100–4. doi: 10.1097/00001786-200404000-00005. [DOI] [PubMed] [Google Scholar]
- 50.Korner EJ, Oinonen MJ, Browne RC. The power of collaboration: using internet-based tools to facilitate networking and benchmarking within a consortium of academic health centers. J Med Syst. 2003;27:47–56. doi: 10.1023/a:1021057128835. [DOI] [PubMed] [Google Scholar]
- 51.Pagliari C, Gilmour M, Sullivan F. Electronic clinical communications implementation (ECCI) in Scotland: a mixed-methods programme evaluation. J Eval Clin Pract. 2004;10:11–20. doi: 10.1111/j.1365-2753.2004.00475.x. [DOI] [PubMed] [Google Scholar]
- 52.O'Connell RT, Cho C, Shah N, Brown K, Shiffman RN. Take note(s): differential EHR satisfaction with two implementations under one roof. J Am Med Inform Assoc. 2004;11:43–9. doi: 10.1197/jamia.M1409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Miller RH, Hillman JM, Given RS. Physician use of IT: results from the Deloitte Research Survey. J Healthc Inf Manag. 2004;18:72–80. [PubMed] [Google Scholar]
- 54.Militello L, Patterson E, Tripp –Reimer T, et al. Clinical reminders: why don't they use them? 2004:1651–5. The Human Factors and Ergonomics Society's 48th Annual Meeting. [Google Scholar]
- 55.Patterson ES, Doebbeling BN, Fung CH, Militello L, Anders S, Asch SM. Identifying barriers to the effective use of clinical reminders: bootstrapping multiple methods. J Biomed Inform. 2005;38:189–99. doi: 10.1016/j.jbi.2004.11.015. [DOI] [PubMed] [Google Scholar]
- 56.de Lusignan S, Singleton A, Wells S. Lessons from the implementation of a near patient anticoagulant monitoring service in primary care. Inform Prim Care. 2004;12:27–33. [PubMed] [Google Scholar]
- 57.Stead WW, Lorenzi NM. Health informatics: linking investment to value. J Am Med Inform Assoc. 1999;6:341–8. doi: 10.1136/jamia.1999.0060341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Simpson RL. Managing the three “P”s to improve patient safety: nursing administration's role in managing information technology. Int J Med Inf. 2004;73:559–61. doi: 10.1016/j.ijmedinf.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 59.Hendy J, Reeves BC, Fulop N, Hutchings A, Masseria C. Challenges to implementing the national programme for information technology (NPfIT): a qualitative study. BMJ. 2005;331:331–6. doi: 10.1136/bmj.331.7512.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.McAlearney AS, Schweikhart SB, Medow MA. Organizational and physician perspectives about facilitating handheld computer use in clinical practice: results of a cross-site qualitative study. J Am Med Inform Assoc. 2005;12:568–75. doi: 10.1197/jamia.M1816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Saleem JJ, Patterson ES, Militello L, Render ML, Orshansky G, Asch SM. Exploring barriers and facilitators to the use of computerized clinical reminders. J Am Med Inform Assoc. 2005;12:438–47. doi: 10.1197/jamia.M1777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Finch E, Mayne C. Thinking beyond CPOE to integrated IT strategy and management. J Healthc Inf Manag. 2004;18:24–9. [PubMed] [Google Scholar]
- 63.Major LF, Turner MG. Assessing the information management requirements for behavioral health providers. J Healthc Manag. 2003;48:323–33. [PubMed] [Google Scholar]
- 64.Stablein D, Welebob E, Johnson E, Metzger J, Burgess R, Classen DC. Understanding hospital readiness for computerized physician order entry. Jt Comm J Qual Saf. 2003;29:336–44. doi: 10.1016/s1549-3741(03)29041-9. [DOI] [PubMed] [Google Scholar]
- 65.Lenz R, Kuhn KA. Towards a continuous evolution and adaptation of information systems in healthcare. Int J Med Inform. 2004;73:75–89. doi: 10.1016/j.ijmedinf.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 66.McDonald CJ, Overhage JM, Tierney WM, et al. The regenstrief medical record system: a quarter century experience. Int J Med Inform. 1999;54:225–53. doi: 10.1016/s1386-5056(99)00009-x. [DOI] [PubMed] [Google Scholar]