Abstract
The purpose of this paper is to review the evidence estimating an impact of occupational factors on mood disorders and suicide, and the efficacy of interventions. This review is based on literature searches using Medline and Psych INFO from 1966 to 2007 (keywords: work stress, job insecurity, job strain, shift work, violence, occupational health, mood disorders, depression, and suicide). To establish the relationship between occupational variables and mood disorders, we focused on clinically significant disorders rather than depressive symptoms. During the last decade, prospective epidemiological studies have suggested a predictive association between the work environment and mood disorders. Recently, increasing numbers of clinical trials have shown favorable effect size of intervention and suggested preferable return-on-investment results. However, low awareness and social stigma still decrease workers access to treatment. Mental health professionals in conjunction with employers have to devise a creative system to make the quality care being offered more accessible to employees. In addition, further outcome data is needed to evaluate the benefit of managing mood disorders in the workplace, and to foster awareness of positive implications for employees, employers, their families, and the society at large. In addition, the work environment, with its chemical (e.g. chemosensory factors, pollutants), physical (e.g. lighting, noise, temperature, outdoor views and activities), biological (e.g., chronobiological factors, allergens, infectious agents), psychological (e.g. demand-control, effort-reward balance), social (e.g. cohesiveness, support), and organizational (e.g. leadership styles) component should meet minimal standards, and may improve with striving towards the optimum.
Keywords: depression, work stress, occupational health, suicide
INTRODUCTION
Work and love are two major domains of our lives from which most people get satisfaction and find meaning; at the same time these can act as life-threatening stressors. Rapid economic change is one of the most significant aspects of our times. Behind the curtain of world economy globalization, the occupational environment is delivering increasing stress, such as job insecurity, increasing workload, and the burden of lifelong learning. Larger proportion of employees became involved in service- and knowledge-based industries requiring heavy technological preparedness and mental stress. If the pace of change exceeds the capacity of the workers to cope, negative stress reactions can occur. These include psychosomatic reactions (e.g. depression, insomnia) as well as vocational consequences (e.g. job dissatisfaction, decreased organizational commitment, reduced job performance, and absenteeism) (1). Negative stress reactions are not limited to the individual worker, but also may affect the worker’s family, and the community in which they live. More attention is required to the psychosocial impact of both the psychosocial work environment and physical work environment.
It is well-known that mood disorders cause the largest disease burden in general population and loss of work productivity in working population (2). At least 5% of workers are affected by mood disorders. Using the National Comorbidity Survey Replication, Kessler and coworkers (3) reported that 1.1% of the workers met criteria for bipolar disorder (I or II) and 6.4% for major depressive disorder (MDD). A study of 24,000 working Canadians also reported that 4.6% met criteria for major depressive episode (MDE) in the past year (4). The Office of Applied Studies (OAS) of Substance Abuse and Mental Health Services Administration (SAMHSA) also reported that an annual average of 7.0% (10.1% for female vs. 4.7% for male) of full-time adult workers experienced a MDE in the past year (5). Some researchers propose that increasing work stress can be associated with the increasing prevalence of depressive disorder and suicide (6–8), but whether it is just a coincidence or the function of any causal relationship has yet to be defined. Therefore, while the effect of depression on functioning has received substantial attention, we have to obtain a greater understanding of the impact of the work environment on mood disorders in order to prevent significant losses to both the individual and society.
How many social resources have to be invested in this area? Who has to take care of these problems? In what areas do we have to intervene first? Given the multiple potential variables proposed to be related in this matter, we would like to clarify the terms and concepts to answer to those questions.
CLARIFICATION OF THE DIAGNOSIS
Most of the past research has focused on psychological distress symptoms (depression, dysphoria, and burn-out) showing elevated rates in workers with higher job stress (9–11). Yet solid studies on clinically significant psychiatric disorders have not been performed until very recently (5,7,12).
There are some important differences between subclinical symptoms and clinically significant psychiatric disorders. On an individual level, differences between psychological symptoms and clinical conditions seem to be marked by symptomatic constellations, duration of symptoms and functional impact. As subclinical mood symptoms are by far the most common in everyday lives of workers, it is reasonable to use those concepts in occupational research. However, the severity and impact on the health care system and productivity are much more detrimental in mood disorders compared to mood symptoms. Furthermore, treatment implications are quite different. Subject population has to be clearly categorized to define the amount of loss from direct medical cost and to compare it with other conditions. Thus, using definite diagnostic categories such as those from the Diagnostic and Statistical Manual of Mental Disorders (DSM) (13), although having their own imperfections, are preferable in performing health economics studies, such as cost-effectiveness analysis, and cost-benefit analysis. These studies are essential to decide how much investment is required to address a certain problem and who has to take care of this new social epidemic.
The community knows that work can be stressful and cause, among other forms of distress, depressive symptoms. Based on this empirical knowledge, we can easily decide to put public revenue into management of could easily conclude to put public revenue into management of depressive symptoms. However, what about depressive disorders? Can the working environment directly contribute to a depressive disorder that requires intensive clinical attention and costs a lot of money? If so, the burden is placed on the employers. However, if the work environment can only trigger the onset or aggravate mood disorders in a vulnerable worker who is predisposed to get it, the burden should belong to an individual employee. This may potentially result in huge political and economic ramifications. In this article, we will focus on mood “disorders” rather than “symptoms” based on their unique health outcome and medical concerns.
Depression can be re-classified into three forms—MDE, depressive syndrome, and dysphoria—and examined by their differential association with occupational variables (6). Depressive syndrome (which is equivalent to a subsyndromal major depression) shows some symptoms of DSM-IV MDE criteria A, but does not fulfill all criteria for MDE. Dysphoria signifies having feelings of sadness or unhappiness. We differentiated previous studies according to the diagnostic methods that were used (see table 1).
Table 1.
Diagnostic Methods for Three Levels of Conditions Related with Mood Disorder
| Psychological Well-Being | Symptoms | Disorder |
|---|---|---|
| Self-rating scale | Self-rating scale | Clinical diagnosis with/without structured interview |
|
|
|
RELATIONSHIP BETWEEN THE OCCUPATIONAL ENVIRONMENT AND MOOD DISORDERS
In general, there is a consensus that acute and chronic life stressors can lead to psychological and physical responses. The workplace can also make manifest latent mood disorders, destabilize, and aggravate symptoms and courses of mood disorders among workers. The relationship between occupational environment and mood disorders seems to be reciprocal, creating vicious cycles in many cases (see figure 1). For example, depressive episodes resulting from work-related stress can impact vocational performance by ‘presenteeism’ (reduced work productivity while present at work) due to decreased concentration, reduced motivation, and decision errors, as well as ‘absenteeism’ (lost productivity from absence, e.g. non-attendant workdays, arriving late or leaving earlier than usual). Negative feedback from the organization, decreased self-esteem, and reduced salary may follow and add on the stress level of depressed workers. If these impacts persist or get worse, more serious mental health outcomes, such as chronic disability and suicide attempt, as well as vocational consequences including repeated job loss can happen. Unemployment and job loss have been consistently reported to elevate the risk for depression to raise the risk for depression and suicide attempt, especially in young workers (14,15).
Fig. 1.
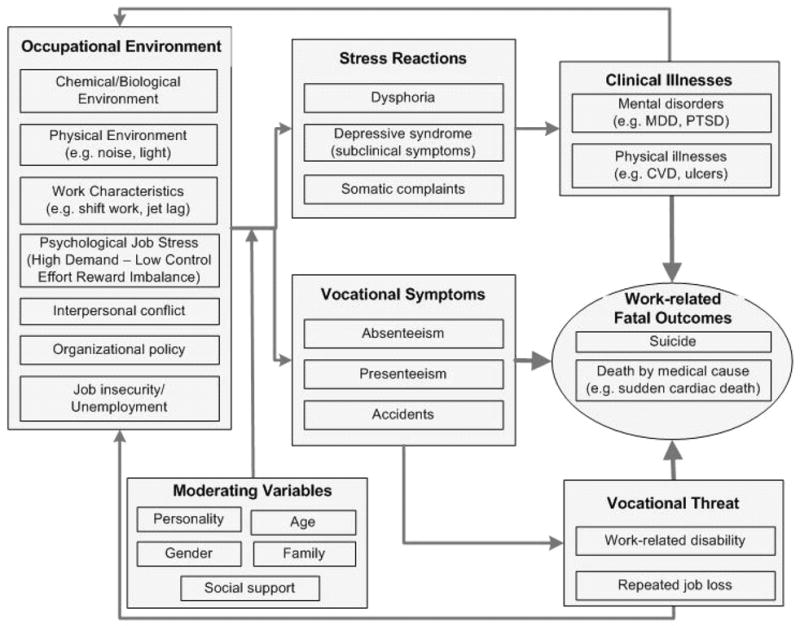
A Model of Occupational Stressors and Mood Disorder. Absenteeism: sickness absence, early leaving, late arrival; Presenteeism: reduced performance while present at work; MDD: Major Depressive Disorder; PTSD: Post-traumatic Stress Disorder; CVD: Cardiovascular Disorder
Methodological limitations can cause controversies in assessing the relationship between work stress and mood disorders. Self-report method can influence a reporting bias, as common perceptual set influences the reporting of both the ‘causal’ and ‘outcome’ variables. In addition to acute loss of income and overall socioeconomic status, overwhelming financial stress, inability to support oneself and one’s dependants, narcissistic frustration at unwanted change in career can contribute to the association between job loss, or being demoted, and depression (16). The effects of low occupational status can be confounding variables intermingled with the effects of work stress (11). Childhood depression can increase the risk for psychiatric disorders in adulthood, which can lead to more stressful jobs (17). Moreover, having a personality disorder comorbid with mood disorders may increase troubles at work, which could elevate work stress. As randomized studies are not feasible in this domain, large scale longitudinal cohort studies are necessary to understand the direction of causality.
However, we can keep in mind that the workplace can function as a secure base for promoting mental health. It is desirable to focus on how to get rid of any potential risk rather than who is most responsible for it. Many workers spend more time at work than at home when they are awake. Therefore, it is quite reasonable to manage their health problems at the workplace, regardless of the cause.
ARE CERTAIN OCCUPATIONS MORE DANGEROUS?
From the public health perspective, it is very important to define the risk for mood disorders by occupational categories. This is also important with regard to workers’ mental health claims and compensation issues. We have to explore and target the “dangerous trades” to establish priorities in policy making and to set up an effective primary intervention system (18).
Many studies have established a connection between specific occupations and depressive symptoms (5,8,19). Some professions and their occupational characteristics are suggested to have association with diagnosable mood disorders and suicide. Employment in human service occupations (e.g. health care, education, and social work) is consistently reported to display high risk for mood disorders (20). Some occupations (e.g. lawyers, dentists, artists, machinists, auto mechanics, and carpenters) are suggested to have higher risk for suicide, while others (e.g. clerks, elementary school teachers, and cooks) are reported to have lower risk (8). SAMHSA’s recent report (5) also demonstrates that the rate of depression varies by occupation and industry. Among the 21 major occupational categories, the personal care and service occupations (10.8%) followed by the food preparation and serving related occupations (10.3%) recorded the highest. Engineering, architecture and surveying (4.3%), life, physical, and social science (4.4%), and installation, maintenance, and repair (4.4%) recorded the lowest rates of the past year MDE.
It is not yet clear whether the alleged risk of certain occupations is due to the occupational stressors associated with them or due to the sociodemographic factors of the workers in those occupations (21). However, poor work conditions (e.g. physicochemical environment, shift work, jet lag, long working hours) and high job stress (e.g. high demand with low control, insufficient reward) are suggested to be the common cause of risk in some occupations in many studies (7,12,22). For example, excessive exposure to occupational toxicants, irritants, odors, extremely hot or cold temperature, and severe noise, as well as inadequate lighting can contribute to the poor response to treatment of and exacerbation of psychiatric conditions, including mood disorders.
CHEMICAL ENVIRONMENT
Acute and toxic exposure can definitely lead to organic brain damage with cognitive and behavioral impairment. Chronic exposure to low-to-moderate dose can cause anxiety and mood disturbances (23). Specifically, lead exposure with increased blood lead level can contribute to depression and anxiety (24–25). One study has found that even low levels of lead exposure can overstimulate protein kinase C (26) which is involved in dysregulation of affect and behavior, which can be a feature of many psychiatric disorders including bipolar disorder. Exposure to lead can act as a stressor to people who are genetically predisposed to mood disorders. Neurotoxic levels of organic mercury can also contribute to the high prevalence of depression and anxiety among chemical workers after acute exposure, as well as during chronic exposure to high levels (27–28).
Organophosphate (OP) pesticides are widely used in agriculture. They are rapidly absorbed and exert their toxic effects. Acute and moderate OP poisoning has been reported to induce depression, anxiety, and irritability (29,30). Beseler and his colleagues reported nearly 6 times risk for depression after OP pesticides poisoning among farmer applicators. They also reported the increased odds of having depression (odds ratio (OR) = 3.26; 95% confidence interval (CI) 0.91–1.31) in the presence of a history of pesticide poisoning among farm women who are not themselves applicators (31–32). In the United Kingdom, there have been social debates on the effects of sheep dip on farmers’ depression and suicide. Sheep dip is a kind of OP compound that is used to protect sheep from external infestation. Anecdotally, the use of sheep dip has been linked with a flu-like syndrome, such as headache, limb pains, fatigability, sleep disturbance, poor concentration, mood change, and suicidal thoughts (31,33). However, the long-term health effects of long-term, low-level exposure is not clear. Some researchers report a probable association between chronic low-dose exposure and depression (31), but others suggest that this relation is only temporary, nonspecific, and involves psychological rather than biological mechanisms (33–34).
Exposure to organic solvents has been consistently reported to be associated with depression (35,36). Rayon manufacturing workers can suffer depression as well as other neurological disturbances due to chronic exposure to carbon disulfide (37). Prevalence of mood and anxiety disorders is significantly higher among workers who used organic solvents (22). Chronic low-level exposure to substances in modern ordinary environment can also cause mood disturbances with many somatic complaints, so called “idiopathic environmental intolerance” or “multiple chemical sensitivity” (MCS), which involve mood symptoms and syndromes (38).
Odors can also alter mood, cognition, and behavior. Some kinds of odors can elevate the level of mood and activity, while aversive odors can make depressive patients more depressed. For example, exposure to pleasant odors elevate mood both in healthy adults (39) and in depressed patients with seasonal affective disorder (SAD) winter type (40), who have been reported to have a greater olfactory acuity than control subjects (41). Olfactory neurons are only two synapses away from the amygdala, which is known to be a part of the neuronal circuitry of anxiety and depression, and can be activated by olfactory aversive stimuli (42).
Workers can be exposed to various levels of odors, aromas, and irritants at the workplace. For example, workers in the swine industry or at slaughter houses can be exposed to extreme pungent odors for a long period. On the other hand, excessive odors of any hedonic valence can be difficult to bear and fragrances can also act as irritants when present in very intense concentrations. People who are more sensitive to odorants than others can suffer from MCS (43). It is important to note that some chemicals may cause irritation at levels below which their odor can be detected. Therefore, setting occupational exposure limits (OELs) for odorous or irritating chemicals is needed to promote safety at work (44). Positive environmental interventions using odors to improve mood are difficult, except in relatively confined work spaces that allow individualized approaches, as people’s individual sensitivities, preferences, and behavioral effects vary. We strongly believe that affecting even a few negatively to affect many positively is not an ethically acceptable approach for an occupational environmental consultant.
PHYSICAL ENVIRONMENT
In humans, light has potent biological and therapeutic effects. Light also suppresses melatonin secretion (45), modulate the release of serotonin (46), shifts the circadian rhythms according to a phase response curve (47) and is necessary to synchronize circadian rhythms in humans (48). Bright light and the deprivation of it can affect the internal biological clock, sleeping patterns, and energy levels (49). Sensitive individuals may notice changes in their mood associated with the doses of sunlight exposure, such that they may feel gloomy during long stretches of cloudy winter days and experience mood improvement on sunny summer days.
Poor lighting conditions at work represent a factor that may be conducive to depression, especially in patients with syndromal or subsyndromal SAD, which together reach 15% to 20% prevalence at temperate latitudes (50). Prolonged reduction of exposure to light in winter can affect the mood status of an individual vulnerable to seasonal changes or who already has spent too much time indoors. Especially for, but not confined to, this population, bright lighting at the workplace can improve mood status of workers. Bright light therapy is supported by the American Psychiatric Association for the treatment of patients with major depression (51), as it has demonstrated its effectiveness not only for SAD but also as an adjunct in MDD or dysthymia with seasonal exacerbations. Bright light might be also beneficial for mood in healthy people (49). Beyond usage of an artificial light treatment device, it is important to mention that in one study of patients with SAD, a one hour walk outside each day for one week significantly reduced depressive symptoms, with no significant relapse after withdrawal. The response rate of 65% was similar to the results of previous studies with bright light treatment by the same group (52). In general, increasing outdoor activities on weekends, being exposed to morning light during winter, and taking outdoor breaks can be recommended to workers. With a consideration for a personalized space, a location near a window would be strongly recommended for individuals with SAD. In the absence of a window, workers with SAD should be encouraged to use a light treatment device close to their workspace during the fall and winter. Obviously, for those individuals, the treatment should be supervised by a qualified professional.
Temperature conditions, as well as humidity and air flow, which greatly affect thermoregulation, of outdoor and indoor work are also important for patients with mood disorders, as thermoregulatory neurotransmitters and neurotransmitters of mood regulation overlap and weather and individual mood may be related (53). Exposure to heat was suggested to be a triggering mechanism in vulnerable individuals of summer SAD, a condition characterized by depression during the summer and spontaneous remission in the fall (54). This would suggest that air conditioning may be an important preventive intervention for these individuals, but recent research failed to confirm this hypothesis. In Romania, a country with hot summers and low availability of air conditioners, contrary to the authors’ hypothesis, those who possess an air conditioner had a higher, rather than a lower, rate of summer SAD (55). Hot temperatures can also be associated with increased perspiration, dehydration, and increased toxicity risks from psychotropic medications used in mood disorders.
Exposure to noise is an important stressor and predicts irritability, somatic complaints, anxiety, and depression (56). Although intense noise is difficult to bear for practically anyone, even mild or intermittent noise may affect certain vulnerable subjects with “noise annoyance” (the emotional reaction to noise at exposure). Noise annoyance is associated with “noise sensitivity” (the physiological reaction to noise), an individual trait quite stable over time which may predict depression (57).
BIOLOGICAL FACTORS
In a routine working environment, infectious agents, pollutants containing endotoxins of bacterial origin, and aeroallergens are commonly encountered. As upper respiratory infections have a very high incidence, allergies have a very high prevalence (58). Changes in allergic symptom severity correlate with changes in depression symptom severity in patients with mood disorders who are exposed to environmental peaks in aeroallergens (59). Additionally, the induction of inflammation in the upper airway results in increased cytokine gene expression in the brain and depression-like behaviors in laboratory animals (60). Therefore, efforts to reduce exposure to viruses, pollutants, allergens, and bacteria cannot be overemphasized.
SHIFTWORK AND JET LAG
Sleep disturbance is a very important risk factor for depression, bipolar disorder, and suicidality (61–62). Sleep impairment can be a common factor in mood disorders that could be aggravated by work environments either as sacrificed duration of sleep to catch up with work or as a consequence of mood disorders. Modern society is by and large sleep-deprived. In addition to impaired sleep, the timing of sleep and activity is essential for both performance and well being. Let’s look around us. Doctors, nurses, police, emergency services, gasoline stations, pharmacies, grocery stores and many others work on a 24-hour schedule. On interstate highways, huge tractor trailers are driving mainly at night to avoid roadblocks related to rush hours, and train and airport operators work many night hours.
Shift work is suggested to increase the risk of developing or aggravating mood disorders at least in vulnerable individuals (63). High incidence of MDD was observed during and after shift work experience and this risk is associated with the duration of exposure (64). Some researchers deny direct effect of night shift on mood disorders and suggest that job characteristics or other organizational factors are related to the association between them (65–66). Further examination of these issues is needed with improved research designs, including consideration of particular shift-work rotation schedules.
The treatment of shift-work sleep disorders involves institutional, micro-environmental, and individual approaches. Institutional intervention includes the shift protocol and the occasional medication focusing on circadian rhythm sleep disorder, jet lag type. Micro-environmental intervention includes the lighting and rest/nap schedule at work. An individual approach includes informed allocation of time and timing for personal needs vs. work and scheduling sleep and wake. Factors to promote sleep and wake at adverse timing includes bright light, avoidance of light, and wake promoting agents in more severe or refractory cases. The treatment and prevention of jet lag includes elaborated schedules of light exposure and avoidance, approximating “portable microclimates” to promote sleep in adverse conditions, timed administration of melatonin, and sleep-promoting or wake-promoting pharmacological agents. The use of bright light to alleviate mood disturbances associated with shift work needs extensive empirical testing (63). The in-depth discussion of these interventions is beyond the scope of this article. However, shift work and jet lag should always be a consideration for clinicians treating patients with recurrent mood disorders, or at risk for suicide. In certain cases of high risk (e.g. bipolar I disorder), the physician should advocate medical leave or even vocational change.
PSYCHOLOGICAL WORK ENVIRONMENT AND MOOD DISORDERS
There are established correlations between a high level of occupational stress and a wide range of mental health problems (7). Recently, several longitudinal studies reported the important role of psychological work stress in developing clinically diagnosed mood disorders. An epidemiologic study revealed that work stress can be an independent risk factor for the development of MDE (67). Workers presenting scores of work stress above the 75th percentile had an elevated risk for MDE (7.1%) and work stress was significantly associated with the risk for MDE in multivariate analysis (OR = 2.35, 95% CI 1.54–3.77). In addition, high job demands (excessive workload, extreme time pressures) increased the risk for MDD or generalized anxiety disorder (GAD) twofold and in previously healthy young workers were associated with the onset of new MDD and GAD (7). Among vulnerable individuals, however, work stress may play only an additive role in the manifestation of a pre-existent condition, e.g, a chronic pain condition (68).
Two models have long been proposed to explain the job characteristics and health implications of work stress; the Demand-Control (DC) model by Karasek (69) and the Effort-Reward Imbalance (ERI) model by Siegrist (70). Some studies have reported that both low control and ERI at work are both associated with depressive symptoms (71).
The DC model is based on the very simplified assumption that the characteristics of the job itself, rather than the perception of an individual worker, induce job strain that can predict a broad range of health and behavioral outcomes (69). This model characterizes the job according to the combination of two basic dimensions: job demand and control. Control, or decision latitude, includes the two factors of skill use and decision authority. According to this model, “high strain”—a combination of high demand and low control —at work will lead to psychological stress, which can eventually lead to chronic disease, including depression (34). Lack of control, in particular, is a relatively consistent predictor of depression (72,73). Overall, the proportion of variance in depression explained by job strain factors varies from approximately 10% to 50%, with a wide percentage margin, due to the difference in measures used (11).
The ERI model is based on the broader concept of the job, including work role, and reflects the individual worker’s emotional needs and characteristics. This model proposes that insufficient reward (income, esteem, and occupational status control) compared to workers’ effort (demands and obligations) can lead to adverse health effects. Most studies using Siegrist’s ERI questionnaire suggest a positive relation between ERI and depression (71,74). An extensive review of the ERI model concludes that employees working in a high-effort, low-reward situation had a significantly elevated risk for psychosomatic symptoms, including depression (75).
As these two models have societal perspectives as well as medical perspectives, most studies using these two models have discussed general symptoms rather than clinical disorders. However, a series of recent reports demonstrated that these models can be validly applied to clinically diagnosed mood disorders (4,6).
SOCIAL ENVIRONMENT AT WORK
Every worker has relationships with others, whether these are supportive, neutral, or full of conflicts. The social environment at work can predict the prevalence and severity of depression in most occupational groups. The level of social support can modulate the effect of work stress on depression (72). Karasek’s DC model is extended to include the degree of social support and thus becomes the Demand-Control-Support model (76). A “socially isolated” status means neither supportive co-workers nor supervisors present. On the other hand, too much interaction with others can be also troublesome (77). Interpersonal conflicts at work predicted an increased risk for psychiatric morbidity. Violence, threatening, bullying, and sexual harassment can be some of the most severe cases of stress from other workers. Employment in occupations involving exposure to work-related threats and violence is a strong risk factor for depression and stress-related disorders in both genders (78).
Recently, a group of European researchers raised the concept of “justice at work” to represent the organizational climate and social relations (79,80). The components of “justice at work” are consistent and sufficient information from the line manager, the line manager’s listening to problems about work and praise, as well as the absence of unfair criticism. The relevant research suggests that employees who perceive that they are treated unfairly by their supervisors are at increased risk of poor mental health. In addition, workplace bullying is a significant risk factor for incident depression in employees. On the other hand, an increase in fair treatment reduces the risk of mental health problems (80).
POTENTIAL MECHANISMS
We can assume biological, psychological, psychosomatic, and behavioral mechanisms contribute to the influence of work stress on the risk for mood disorders. While the effects of the discussed physicochemical factors pertinent to the work environment have multiple mechanisms, which would require a discussion with a length which will surpass the scope of this article, we focus here only on the effects of social and psychological factors associated with work. Any intense or sustained stress elevates corticosteroids, and persistently elevated corticosteroids can directly affect brain structure (81) and can induce down-regulation of the glucocorticoid receptors, thereby impairing affect regulation (82). Rydmark (83) reported that the cortisol response to corticotropin-releasing hormone (CRH) showed significantly dampened response in patients with job-stress related depression. However, prefrontocortical and hippocampal volumes were not changed. This contrasts to what has been described in MDD and suggests the difference between endogenous depression and reactive depression due to environmental change. High job demands and lack of decision latitude implies an inability to influence one’s own condition and may induce feelings of helplessness and hopelessness. If this continues for a long time, an individual can be conditioned to “learned helplessness”, which is a well known psychological cause and manifestation of depression. Work stress can result in psychosomatic symptoms, such as fatigue, sleep disturbance, and concentration difficulty, all of which can be both symptoms and risk factors for mood disorders. Finally, behavioral difficulties, such as inability to engage in leisure activities and to maintain strong social networks, can lead to mood disorders (76).
GENDER IMPLICATIONS
Certain work related risk factors and triggers for mood disorders and suicide are different in men and women. For example, a recent Canadian survey showed that men with high strain jobs and women with low decision authority had elevated odds of incident depression, while lack of social support was related to depression in both gender. This result may reflect the difference in the types of jobs held, as many women tend to take less-strained jobs to balance work and family (4).
The fact that women are absent from work more often than men is a very often reported finding (84), but there is very limited explanation as to why this is so (85). An often suggested explanation is that women’s high rates of absence are related to them bearing the majority of the load in childcare and family responsibilities. However, despite the face validity of this “double burden” (childcare and work) hypothesis, it is not supported empirically (85). In fact, more recently, it appears that there is no difference between absenteeism for childcare reasons between men and women. Also, having more children is a factor reducing rather than increasing absenteeism in women (86). In fact, women with multiple roles have better health, stronger relationships, and less depression (87). As such, one very likely explanation for an increased absenteeism in women is their poorer health, including physical symptoms, insomnia, migraine headaches, and depression (88). It is well known that depression and anxiety disorders are more prevalent in women. Many biological, psychological and social factors have been proposed to explain this difference in prevalence. Among occupational factors which could add to a potential increased vulnerability of women to depressogenic factors, we mention implicit and explicit work discrimination, such as lower salaries, more difficult promotion, and an increased risk to be bullied or harassed.
With regard to suicide, it is well known that women attempt suicide more often, often with overdoses, but that men commit suicide more often. However, certain occupational considerations may increase the risk of completed suicide in women, such as availability of lethal poisons, or professional knowledge to use them to lethal ends. For instance, older generation pesticides, more lethal in overdose, are responsible for the greater rate of suicide completion in women than in men in China as compared to the rest of the world (89,90). In the hands of doctors and nurses, means of self-poisoning, which otherwise would result only in suicide attempt, result in suicide completions because of professional knowledge to use them “more effectively” and increased access to lethal doses (91).
JOB INSECURITY AND UNEMPLOYMENT
There is no guarantee that high-caliber professionals or the most profitable company of this year will survive some years later. Tougher competition, organizational restructuring, and abrupt lay-offs can cause negative affect, such as feelings of insecurity, inferiority, and uncertainty about the future. Job loss can damage one’s self-esteem and cause feelings of helplessness that can continue for some years. Job loss and unemployment can trigger the chain of adversity: financial and relational strain, being trapped in worries of another job loss, and loss of personal control, and these can lead to depression and even suicide (92–93). Suicide risk is strongly associated with unemployment, lack of job security, and sickness-related absence from work especially in male subjects (94–95).
On the other hand, some jobs might be as bad for mental health as unemployed status. The unemployed reported worse health when compared to all employees, but poor quality jobs (i.e. those featuring high job insecurity, low marketability, and high job strain) were also associated with worse health when compared with jobs with fewer or no stressors. And ‘bad’ jobs with combined psychosocial stressors were as bad for one’s health as having no job at all (14). Nonstandard employment, such as part-time work, temporary work, and daily work, were shown to lead to increased depression and suicidal ideation (96).
WORK-RELATED SUICIDE
Workplace suicide is the most severe outcome of mental health problems at the workplace. Whether it is associated with work-related stress (e.g. karo jisatsu - suicide from overwork) or just takes place at the victim’s workplace (e.g. on-the-job suicide), it signifies detrimental loss to the victim and his/her family members, colleagues, and the workplace as a whole.
Certain occupations have more suicide risk than others. The data from the Bureau of Labor Statistics (BLS) Census of Fatal Occupational Injuries (CFOI) indicated the highest relative risk (RR) of on-the-job suicide among police and detectives in public service (RR 6.99) and workers in military occupation (RR 5.39) (97). Access to lethal weapons can be an occupation-specific risk factor for suicide in the police and military personnel (98), as well as accessibility and knowledgeable use of poisons increases the risk of overdose suicide in medical personnel (91). Total number of workplace suicide victims was the highest in managerial and professional specialty occupations. On-the-job suicide may not be related to work-related issues or exposures, but this result can be applied to devise suicide prevention strategies for professions at risk.
Severe work stress can be an important risk factor for suicide, especially when combined with individual characteristics and poor social support (15,94). A prospective study investigated the association between psychosocial job characteristics and the risk for completed suicide among Japanese male workers. The result showed that low control at work increased the suicidal risk more than fourfold (99). A psychological autopsy also showed that most of the suicide victims had suffered from low social support, high psychological demand, low decision latitude, and long working hours (100). Even though half of them saw a general practitioner because of unspecified somatic complaints, none of them had a psychiatric consultation and effective treatment of job stress or depression.
This result calls for appropriate countermeasures, including job redesign aimed at increasing worker’s control and psychiatric quality care to treat workers under stress. Systemic interventions to increase awareness and destigmatize mental health, and regular monitoring for high-risk populations are also in urgent need. Listing telephone numbers with suicide crisis hotlines in every directory, with confidential telephone calls and the availability of referral networks are expected to contribute to a reduction of work-related suicides. Reducing access to suicide means, such as high places from which one can jump, firearm policies, ceilings fixtures that would not be able to support a human body in case of hanging, and work flows that encourage human contact and reporting concerns to a supervisor immediately might be beneficial. Identifying temporal windows of possible increased risk, such as recent hire, being demoted or promoted, being transferred, being laid-off, and offering free counseling may also represent positive steps.
TOWARD THE HAPPIER, HEALTHIER, AND MORE PRODUCTIVE WORKPLACE
As the occupational factors involved in mood disorders are various and complicated, interventions can be devised at multiple levels of approaches. Interventions can be classified into individual approaches and organizational approaches. Individual approaches can include traditional psychiatric/psychological interventions in a clinical setting, such as cognitive-behavioral treatment and pharmacotherapy. Stress reduction programs, such as teaching effective coping skills and relaxation techniques, may help workers to manage work stress better and reduce their risk of depression (101). An extensive review reported a moderate effect from cognitive-behavioral interventions and multimodal interventions, and a small effect from relaxation techniques (102). Pharmacotherapy with psychiatric quality care to the clinical population has consistently proven the cost-effectiveness and cost-benefit to both employers and employees (103,104). However, some investigators are quite skeptical towards the long-term benefits of these individual approaches, because they usually will not change the root cause.
The organizational approach focuses on an assessment of hazardous work conditions and a mobilization of organizational resources to support workers’ mental health. Though this could be theoretically ideal, the feasibility requires testing. It is very difficult to tell which specific occupational factors contribute to the development and/or worsening of mood disorders. It is also more difficult for an individual worker to change the nature of his workplace and occupation. Only a few reports showed the efficacy of the organizational approach towards general symptoms (105). The authors could not find such a report on clinically diagnosed psychiatric disorders.
The irony that some workers can do even more harm to the organization while present at work suggests the need of more active intervention at the organizational level. For example, more and more executives are affected by stress from an unpredictable economy, increasing responsibility, and pressure to keep up profitability. If some executives have a vulnerability to, or already suffer from mood disorders, work stress may wreak more havoc on his or her mental health over time. Emotionally unstable executives can cause disturbances in the company and make an irrevocable loss to the whole organization. It is quite clear that they had better take a few weeks leave, make more personal time, and take proper evaluation and management to get back to normal performance level. It is beneficial both for the individual and for the organization to develop a more accessible system that can provide practical solutions with timely referral to professional care. At some point of treatment, psychiatrists and other health professionals can recommend that the worker take a leave of absence. Educational efforts have to take place at the level of the organization to help the management keep in mind the greater negative effects of presenteeism as compared to absenteeism on the organization as a whole.
We should not wait until workers become aged and suffer from chronic problems. Rather, long-term intervention must be started from young adulthood or even adolescence. Significant numbers of new cases of depression can be attributable to work stress and younger workers with depression are suffering from even more severe absenteeism (106). Adequate interventions can significantly improve employment outcomes and reduce workplace conflicts in depressed employed persons (107).
Preventing and managing mood disorders among workers is a vital issue for employers. Organizational concern and effort can save money while creating a healthier, happier, and more productive workplace. If a worker in the service industry is not happy by any means, he or she cannot smile at the customers, cannot be kind enough, can ruin the relationship with them, and cannot keep the sales record as a result. If a researcher in the information technology industry is not emotionally healthy, then his ability to generate creative, relevant, and testable ideas will fade out and thus he cannot be productive.
What, in our opinion, is an ideal work environment for the workers with mood disorders? We summarize the requirements for the optimal ‘mood-friendly’ and thus more productive workplace in table 2. Considering the enormous impact of mood status on the performance level, more comprehensive professional consultation service, requiring medical, psychological, and organizational knowledge and experience, is urgently needed. This discipline could be called ‘thymo-ecology’, focused on optimizing affective status of workers by manipulating various environmental conditions, both at an individual and an organizational level. Psychiatrists with occupational or organizational experience and occupational physicians with proper psychological training can be candidates for this new professional area. For example, shorter working hours, monitoring the environmental risks on mood status, using noise canceling headphones, allowing one to take outdoor walks or naps (in a ‘nap space’) during the workday, access to a window based on vulnerabilities, and managing behavioral risks are several examples of recommendations from a ‘thymo-ecologically’ minded occupational consultant.
Table 2.
Checklist for an ideal work environment
Common requirements
|
Specific requirements
|
CONCLUSION
Mood disorders are closely related to the occupational environment. Depressive disorders cause more severe functional impairment than any other illness; suicides cause explosive loss. These losses are not confined to the individuals they directly affect, but are substantial for our society at large. However, the government and companies have little awareness of and, thus, limited investment in them. Considering the robust evidence proving efficacy of treatment for depression, the investment and unprejudiced attention of employers would be very helpful to their employees’ mental health and business productivity. These efforts are expected to reduce suicide risk factors such as depression, hopelessness, and sleep impairment. Finally, adequate efforts for increased awareness, education, early detection and referral, help hotlines, availability of counseling, as well as asking about suicide ideation/intent/attempts during routine medical checkups, may contribute to a reduction of work-related suicide and suicide in general, a public health priority.
Acknowledgments
Dr. Woo was supported by the Inje Research and Scholarship Foundation in 2007. Dr. Postolache was supported by R21 MH075905, R01MH074891 and a NARSAD Independent Investigator Award. The authors thank Joseph Soriano and Sarah Zimmerman for their substantial help with this article.
References
- 1.Collins JJ, Baase CM, Sharda CE, Ozminkowski RJ, Nicholson S, Billotti GM, Turpin RS, Olson M, Berger ML. The assessment of chronic health conditions on work performance, absence, and total economic impact for employers. J Occup Environ Med. 2005;47(6):547–57. doi: 10.1097/01.jom.0000166864.58664.29. [DOI] [PubMed] [Google Scholar]
- 2.Greenberg PE, Kessler RC, Birnbaum HG, Leong SA, Lowe SW, Berglund PA, Corey-Lisle PK. The economic burden of depression in the United States: how did it change between 1990 and 2000? J Clin Psychiatry. 2003;64(12):1465–75. doi: 10.4088/jcp.v64n1211. [DOI] [PubMed] [Google Scholar]
- 3.Kessler RC, Akiskal HS, Ames M, Birnbaum H, Greenberg P, Hirschfeld RM, Jin R, Merikangas KR, Simon GE, Wang PS. Prevalence and effects of mood disorders on work performance in a nationally representative sample of U.S. workers. Am J Psychiatry. 2006;163(9):1561–8. doi: 10.1176/appi.ajp.163.9.1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Blackmore ER, Stansfeld SA, Weller I, Munce S, Zagorski BM, Stewart DE. Major depressive episodes and work stress: results from a national population survey. Am J Public Health. 2007;97(11):2088–93. doi: 10.2105/AJPH.2006.104406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Substance Abuse and Mental Health Services Administration (SAMHSA), Office of Applied Studies. [(Accessed 15 October 2007)];The NSDUH Report: Depression among Adults Employed Full-Time, by Occupational Category [Web Page] 2007 11 October; Available at http://www.oas.samhsa.gov/2k7/depression/occupation.htm.
- 6.Mausner-Dorsch H, Eaton WW. Psychosocial work environment and depression: epidemiologic assessment of the demand-control model. Am J Public Health. 2000;90(11):1765–70. doi: 10.2105/ajph.90.11.1765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Melchior M, Caspi A, Milne BJ, Danese A, Poulton R, Moffitt TE. Work stress precipitates depression and anxiety in young, working women and men. Psychol Med. 2007;37(8):1119–29. doi: 10.1017/S0033291707000414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Steven S. Occupation and Suicide. Soc Sci Q. 2001;82(2):384–96. [Google Scholar]
- 9.Paterniti S, Niedhammer I, Lang T, Consoli SM. Psychosocial factors at work, personality traits and depressive symptoms. Longitudinal results from the GAZEL Study. Br J Psychiatry. 2002;181:111–7. [PubMed] [Google Scholar]
- 10.Stansfeld SA, Fuhrer R, Head J, Ferrie J, Shipley M. Work and psychiatric disorder in the Whitehall II Study. J Psychosom Res. 1997;43(1):73–81. doi: 10.1016/s0022-3999(97)00001-9. [DOI] [PubMed] [Google Scholar]
- 11.Tennant C. Work-related stress and depressive disorders. J Psychosom Res. 2001;51(5):697–704. doi: 10.1016/s0022-3999(01)00255-0. [DOI] [PubMed] [Google Scholar]
- 12.Wang J, Patten SB. Perceived work stress and major depression in the Canadian employed population, 20–49 years old. J Occup Health Psychol. 2001;6(4):283–9. doi: 10.1037//1076-8998.6.4.283. [DOI] [PubMed] [Google Scholar]
- 13.American Psychiatric Association (APA) DSM-IV: Diagnostic and statistical manual of mental disorders. 4. Washington, DC: APA; 1994. [Google Scholar]
- 14.Broom DH, D’Souza RM, Strazdins L, Butterworth P, Parslow R, Rodgers B. The lesser evil: bad jobs or unemployment? A survey of mid-aged Australians. Soc Sci Med. 2006;63(3):575–86. doi: 10.1016/j.socscimed.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 15.Qin P, Agerbo E, Westergard-Nielsen N, Eriksson T, Mortensen PB. Gender differences in risk factors for suicide in Denmark. Br J Psychiatry. 2000;177:546–50. doi: 10.1192/bjp.177.6.546. [DOI] [PubMed] [Google Scholar]
- 16.Glass D, McKnight JD. Perceived control, depressive symptomatology, and professional burnout: a review of the evidence. Psychol Health. 1996;11(1):23–48. [Google Scholar]
- 17.Kim-Cohen J, Caspi A, Moffitt TE, Harrington H, Milne BJ, Poulton R. Prior juvenile diagnoses in adults with mental disorder: developmental follow-back of a prospective-longitudinal cohort. Arch Gen Psychiatry. 2003;60(7):709–17. doi: 10.1001/archpsyc.60.7.709. [DOI] [PubMed] [Google Scholar]
- 18.Alice Hamilton. Exploring the Dangerous Trades: The Autobiography of Alice Hamilton, M. Boston MA: Northeastern University Press; 1985. [Google Scholar]
- 19.Roberts RE, Lee ES. Occupation and the prevalence of major depression, alcohol, and drug abuse in the United States. Environ Res. 1993;61(2):266–78. doi: 10.1006/enrs.1993.1071. [DOI] [PubMed] [Google Scholar]
- 20.Wieclaw J, Agerbo E, Mortensen PB, Bonde JP. Risk of affective and stress related disorders among employees in human service professions. Occup Environ Med. 2006;63(5):314–9. doi: 10.1136/oem.2004.019398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Eaton WW, Anthony JC, Mandel W, Garrison R. Occupations and the prevalence of major depressive disorder. J Occup Med. 1990;32(11):1079–87. doi: 10.1097/00043764-199011000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Morrow LA, Gibson C, Bagovich GR, Stein L, Condray R, Scott A. Increased incidence of anxiety and depressive disorders in persons with organic solvent exposure. Psychosom Med. 2000;62(6):746–50. doi: 10.1097/00006842-200011000-00002. [DOI] [PubMed] [Google Scholar]
- 23.Morrow LA, Stein L, Bagovich GR, Condray R, Scott A. Neuropsychological assessment, depression, and past exposure to organic solvents. Appl Neuropsychol. 2001;8(2):65–73. doi: 10.1207/S15324826AN0802_1. [DOI] [PubMed] [Google Scholar]
- 24.Rhodes D, Spiro A, 3rd, Aro A, Hu H. Relationship of bone and blood lead levels to psychiatric symptoms: the normative aging study. J Occup Environ Med. 2003;45(11):1144–51. doi: 10.1097/01.jom.0000094995.23808.7b. [DOI] [PubMed] [Google Scholar]
- 25.Baker EL, Feldman RG, White RF, Harley JP. The role of occupational lead exposure in the genesis of psychiatric and behavioral disturbances. Acta Psychiatr Scand Suppl. 1983;303:38–48. doi: 10.1111/j.1600-0447.1983.tb00940.x. [DOI] [PubMed] [Google Scholar]
- 26.Birnbaum SG, Yuan PX, Wang M, Vijayraghavan S, Bloom AK, Davis DJ, et al. Protein kinase C overactivity impairs prefrontal cortical regulation of working memory. Science. 2004;306(5697):882–4. doi: 10.1126/science.1100021. [DOI] [PubMed] [Google Scholar]
- 27.Haut MW, Morrow LA, Pool D, Callahan TS, Haut JS, Franzen MD. Neurobehavioral effects of acute exposure to inorganic mercury vapor. Appl Neuropsychol. 1999;6(4):193–200. doi: 10.1207/s15324826an0604_1. [DOI] [PubMed] [Google Scholar]
- 28.Powell TJ. Chronic neurobehavioural effects of mercury poisoning on a group of Zulu chemical workers. Brain Inj. 2000;14(9):797–814. doi: 10.1080/026990500421912. [DOI] [PubMed] [Google Scholar]
- 29.Metcalf DR, Holmes JH. VII. Toxicology and physiology. EEG, psychological, and neurological alterations in humans with organophosphorus exposure. Ann N Y Acad Sci. 1969;160(1):357–65. doi: 10.1111/j.1749-6632.1969.tb15857.x. [DOI] [PubMed] [Google Scholar]
- 30.Mearns J, Dunn J, Lees-Haley PR. Psychological effects of organophosphate pesticides: a review and call for research by psychologists. J Clin Psychol. 1994;50(2):286–94. doi: 10.1002/1097-4679(199403)50:2<286::aid-jclp2270500223>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 31.Stallones L, Beseler C. Pesticide poisoning and depressive symptoms among farm residents. Ann Epidemiol. 2002;12(6):389–94. doi: 10.1016/s1047-2797(01)00298-8. [DOI] [PubMed] [Google Scholar]
- 32.Beseler C, Stallones L, Hoppin JA, Alavanja MC, Blair A, Keefe T, et al. Depression and pesticide exposures in female spouses of licensed pesticide applicators in the agricultural health study cohort. J Occup Environ Med. 2006;48(10):1005–13. doi: 10.1097/01.jom.0000235938.70212.dd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Solomon C, Poole J, Palmer KT, Peveler R, Coggon D. Neuropsychiatric symptoms in past users of sheep dip and other pesticides. Occup Environ Med. 2007;64(4):259–66. doi: 10.1136/oem.2005.023879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rees H. Exposure to sheep dip and the incidence of acute symptoms in a group of Welsh sheep farmers. Occup Environ Med. 1996;53(4):258–63. doi: 10.1136/oem.53.4.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Morrow LA, Kamis H, Hodgson MJ. Psychiatric symptomatology in persons with organic solvent exposure. J Consult Clin Psychol. 1993;61(1):171–4. doi: 10.1037//0022-006x.61.1.171. [DOI] [PubMed] [Google Scholar]
- 36.Hakkola M. Neuropsychological symptoms among tanker drivers with exposure to solvents. Occup Med (Lond) 1994;44(5):243–6. doi: 10.1093/occmed/44.5.243. [DOI] [PubMed] [Google Scholar]
- 37.Takebayashi T, Omae K, Ishizuka C, Nomiyama T, Sakurai H. Cross sectional observation of the effects of carbon disulphide on the nervous system, endocrine system, and subjective symptoms in rayon manufacturing workers. Occup Environ Med. 1998;55(7):473–9. doi: 10.1136/oem.55.7.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hausteiner C, Mergeay A, Bornschein S, Zilker T, Forstl H. New aspects of psychiatric morbidity in idiopathic environmental intolerances. J Occup Environ Med. 2006;48(1):76–82. doi: 10.1097/01.jom.0000182207.68987.d7. [DOI] [PubMed] [Google Scholar]
- 39.Schiffman SS, Suggs MS, Sattely-Miller EA. Effect of pleasant odors on mood of males at midlife: comparison of African-American and European-American men. Brain Res Bull. 1995;36(1):31–7. doi: 10.1016/0361-9230(94)00134-m. [DOI] [PubMed] [Google Scholar]
- 40.Williams SS, Rosenthal NE, Gilbert AN, Stiller JW, Hardin TA, Postolache TT. Brief exposure to distinct olfactory stimuli alters mood reports in depressed patients. Int J Child Health Hum Dev. 2008;1(2) In print. [Google Scholar]
- 41.Postolache TT, Wehr TA, Doty RL, Sher L, Turner EH, Bartko JJ, Rosenthal NE. Patients with seasonal affective disorder have lower odor detection thresholds than control subjects. Arch Gen Psychiatry. 2002;59(12):1119–22. doi: 10.1001/archpsyc.59.12.1119. [DOI] [PubMed] [Google Scholar]
- 42.Zald DH, Pardo JV. Emotion, olfaction, and the human amygdala: amygdala activation during aversive olfactory stimulation. Proc Natl Acad Sci U S A. 1997;94(8):4119–24. doi: 10.1073/pnas.94.8.4119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hillert L, Musabasic V, Berglund H, Ciumas C, Savic I. Odor processing in multiple chemical sensitivity. Hum Brain Mapp. 2007;28(3):172–82. doi: 10.1002/hbm.20266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gaffney SH, Paustenbach DJ. A proposed approach for setting occupational exposure limits for sensory irritants based on chemosensory models. Ann Occup Hyg. 2007;51(4):345–56. doi: 10.1093/annhyg/mem019. [DOI] [PubMed] [Google Scholar]
- 45.Lewy AJ, Wehr TA, Goodwin FK, Newsome DA, Markey SP. Light suppresses melatonin secretion in humans. Science. 1980;210(4475):1267–9. doi: 10.1126/science.7434030. [DOI] [PubMed] [Google Scholar]
- 46.Reiter RJ, Hurlbut EC, Esquifino AI, Champney TH, Steger RW. Changes in serotonin levels, N-acetyltransferase activity, hydroxyindole-O-methyltransferase activity, and melatonin levels in the pineal gland of the Richardson’s ground squirrel in relation to the light-dark cycle. Neuroendocrinology. 1984;39(4):356–60. doi: 10.1159/000124004. [DOI] [PubMed] [Google Scholar]
- 47.Lewy AJ, Ahmed S, Jackson JM, Sack RL. Melatonin shifts human circadian rhythms according to a phase-response curve. Chronobiol Int. 1992;9(5):380–92. doi: 10.3109/07420529209064550. [DOI] [PubMed] [Google Scholar]
- 48.Czeisler CA, Kronauer RE, Allan JS, Duffy JF, Jewett ME, Brown EN, Ronda JM. Bright light induction of strong (type 0) resetting of the human circadian pacemaker. Science. 1989;244(4910):1328–33. doi: 10.1126/science.2734611. [DOI] [PubMed] [Google Scholar]
- 49.Partonen T, Lonnqvist J. Bright light improves vitality and alleviates distress in healthy people. J Affect Disord. 2000;57(1–3):55–61. doi: 10.1016/s0165-0327(99)00063-4. [DOI] [PubMed] [Google Scholar]
- 50.Kasper S, Wehr TA, Bartko JJ, Gaist PA, Rosenthal NE. Epidemiological findings of seasonal changes in mood and behavior. A telephone survey of Montgomery County. Maryland Arch Gen Psychiatry. 1989;46(9):823–33. doi: 10.1001/archpsyc.1989.01810090065010. [DOI] [PubMed] [Google Scholar]
- 51.American Psychiatric Association. APA practice guideline for the treatment of patients with major depression. Revised edn. Washington, DC: APA; 2000. [Google Scholar]
- 52.Wirz-Justice A, Graw P, Krauchi K, Sarrafzadeh A, English J, Arendt J, Sand L. ‘Natural’ light treatment of seasonal affective disorder. J Affect Disord. 1996;37(2–3):109–20. doi: 10.1016/0165-0327(95)00081-x. [DOI] [PubMed] [Google Scholar]
- 53.Boker SM, Leibenluft E, Deboeck PR, Virk G, Postolache TT. Mood oscillations and coupling between mood and weather in patients with rapid cycling bipolar disorder. Int J Child Health Hum Dev. 2008;1(2) [PMC free article] [PubMed] [Google Scholar]
- 54.Wehr TA, Giesen HA, Schulz PM, Anderson JL, Joseph-Vanderpool JR, Kelly K, et al. Contrasts between symptoms of summer depression and winter depression. J Affect Disord. 1991;23(4):173–83. doi: 10.1016/0165-0327(91)90098-d. [DOI] [PubMed] [Google Scholar]
- 55.Soriano JJ, Ciupagea C, Rohan KJ, Neculai DB, Yousufi SM, Guzman A, et al. Seasonal variations in mood and behavior in Romanian postgraduate students. ScientificWorldJournal. 2007;7:870–9. doi: 10.1100/tsw.2007.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Melamed S, Luz J, Green MS. Noise exposure, noise annoyance and their relation to psychological distress, accident and sickness absence among blue-collar workers—the Cordis Study. Isr J Med Sci. 1992;28(8–9):629–35. [PubMed] [Google Scholar]
- 57.Stansfeld SA. Noise, noise sensitivity and psychiatric disorder: epidemiological and psychophysiological studies. Psychol Med Suppl. 1992;22:1–44. [PubMed] [Google Scholar]
- 58.Arbes SJ, Jr, Gergen PJ, Elliott L, Zeldin DC. Prevalences of positive skin test responses to 10 common allergens in the US population: results from the third National Health and Nutrition Examination Survey. J Allergy Clin Immunol. 2005;116(2):377–83. doi: 10.1016/j.jaci.2005.05.017. [DOI] [PubMed] [Google Scholar]
- 59.Postolache TT, Lapidus M, Sander ER, Langenberg P, Hamilton RG, Soriano JJ, et al. Changes in allergy symptoms and depression scores are positively correlated in patients with recurrent mood disorders exposed to seasonal peaks in aero-allergens. ScientificWorldJournal. 2007;7:1968–77. doi: 10.1100/tsw.2007.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tonelli LH, Holmes A, Postolache TT. Intranasal immune challenge induces sex-dependent depressive-like behavior and cytokine expression in the brain. Neuropsychopharmacology. 2008;33(5):1038–48. doi: 10.1038/sj.npp.1301488. [Published online 2007 June 27.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Papadimitriou GN, Dikeos DG, Soldatos CR. Sleep disturbance in unipolar and bipolar depression: relationship to psychiatric family history. Neuropsychobiology. 2003;48(3):131–5. doi: 10.1159/000073629. [DOI] [PubMed] [Google Scholar]
- 62.Sjöström N, Waern M, Hetta J. Nightmares and sleep disturbances in relation to suicidality in suicide attempters. Sleep. 2007;30(1):91–5. doi: 10.1093/sleep/30.1.91. [DOI] [PubMed] [Google Scholar]
- 63.Cole RJ, Loving RT, Kripke DF. Psychiatric aspects of shiftwork. Occup Med. 1990;5(2):301–14. [PubMed] [Google Scholar]
- 64.Scott AJ, Monk TH, Brink LL. Shiftwork as a Risk Factor for Depression: A Pilot Study. Int J Occup Environ Health. 1997;3(Suppl 2):S2–S9. [PubMed] [Google Scholar]
- 65.Skipper JK, Jr, Jung FD, Coffey LC. Nurses and shiftwork: effects on physical health and mental depression. J Adv Nurs. 1990;15(7):835–42. doi: 10.1111/j.1365-2648.1990.tb01915.x. [DOI] [PubMed] [Google Scholar]
- 66.Goodrich S, Weaver KA. Differences in depressive symptoms between traditional workers and shiftworkers. Psychol Rep. 1998;83(2):571–6. doi: 10.2466/pr0.1998.83.2.571. [DOI] [PubMed] [Google Scholar]
- 67.Wang J. Work stress as a risk factor for major depressive episode(s) Psychol Med. 2005;35(6):865–71. doi: 10.1017/s0033291704003241. [DOI] [PubMed] [Google Scholar]
- 68.Munce SE, Weller I, Robertson Blackmore EK, Heinmaa M, Katz J, Stewart DE. The role of work stress as a moderating variable in the chronic pain and depression association. J Psychosom Res. 2006;61(5):653–60. doi: 10.1016/j.jpsychores.2006.03.048. [DOI] [PubMed] [Google Scholar]
- 69.Karasek RA. Job demands, job decision latitude and mental strain: implications for job redesign. Adm Sci Q. 1979;24:285–307. [Google Scholar]
- 70.Siegrist J. Adverse health effects of high-effort/low-reward conditions. J Occup Health Psychol. 1996;1(1):27–41. doi: 10.1037//1076-8998.1.1.27. [DOI] [PubMed] [Google Scholar]
- 71.Tsutsumi A, Kayaba K, Theorell T, Siegrist J. Association between job stress and depression among Japanese employees threatened by job loss in a comparison between two complementary job-stress models. Scand J Work Environ Health. 2001;27(2):146–53. doi: 10.5271/sjweh.602. [DOI] [PubMed] [Google Scholar]
- 72.Jimmieson NL, Terry DJ. Responses to an in-basket activity: the role of work stress, behavioral control, and informational control. J Occup Health Psychol. 1997;2(1):72–83. doi: 10.1037//1076-8998.2.1.72. [DOI] [PubMed] [Google Scholar]
- 73.Kawakami N, Haratani T, Araki S. Effects of perceived job stress on depressive symptoms in blue-collar workers of an electrical factory in Japan. Scand J Work Environ Health. 1992;18(3):195–200. doi: 10.5271/sjweh.1588. [DOI] [PubMed] [Google Scholar]
- 74.Larisch M, Joksimovic L, von dem Knesebeck O, Starke D, Siegrist J. [Effort-reward imbalance at work and depressive symptoms—a cross-sectional investigation of middle-aged employees] Psychother Psychosom Med Psychol. 2003;53(5):223–8. doi: 10.1055/s-2003-38867. [DOI] [PubMed] [Google Scholar]
- 75.van Vegchel N, de Jonge J, Bosma H, Schaufeli W. Reviewing the effort-reward imbalance model: drawing up the balance of 45 empirical studies. Soc Sci Med. 2005;60(5):1117–31. doi: 10.1016/j.socscimed.2004.06.043. [DOI] [PubMed] [Google Scholar]
- 76.Karasek RA, Theorell T. Healthy work: Stress, productivity and the reconstruction of working life. New York: Basic Books; 1990. [Google Scholar]
- 77.Romanov K, Appelberg K, Honkasalo ML, Koskenvuo M. Recent interpersonal conflict at work and psychiatric morbidity: a prospective study of 15,530 employees aged 24–64. J Psychosom Res. 1996;40(2):169–76. doi: 10.1016/0022-3999(95)00577-3. [DOI] [PubMed] [Google Scholar]
- 78.Wieclaw J, Agerbo E, Mortensen PB, Burr H, Tuchsen F, Bonde JP. Work related violence and threats and the risk of depression and stress disorders. J Epidemiol Community Health. 2006;60(9):771–5. doi: 10.1136/jech.2005.042986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kivimaki M, Vahtera J, Elovainio M, Virtanen M, Siegrist J. Effort-reward imbalance, procedural injustice and relational injustice as psychosocial predictors of health: complementary or redundant models? Occup Environ Med. 2007;64(10):659–65. doi: 10.1136/oem.2006.031310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ferrie JE, Head J, Shipley MJ, Vahtera J, Marmot MG, Kivimaki M. Injustice at work and incidence of psychiatric morbidity: the Whitehall II study. Occup Environ Med. 2006;63(7):443–50. doi: 10.1136/oem.2005.022269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Sapolsky RM, Krey LC, McEwen BS. The neuroendocrinology of stress and aging: the glucocorticoid cascade hypothesis. Endocr Rev. 1986;7(3):284–301. doi: 10.1210/edrv-7-3-284. [DOI] [PubMed] [Google Scholar]
- 82.Pariante CM, Miller AH. Glucocorticoid receptors in major depression: relevance to pathophysiology and treatment. Biol Psychiatry. 2001;49(5):391–404. doi: 10.1016/s0006-3223(00)01088-x. [DOI] [PubMed] [Google Scholar]
- 83.Rydmark I, Wahlberg K, Ghatan PH, Modell S, Nygren A, Ingvar M, et al. Neuroendocrine, cognitive and structural imaging characteristics of women on long-term sickleave with job stress-induced depression. Biol Psychiatry. 2006;60(8):867–73. doi: 10.1016/j.biopsych.2006.04.029. [DOI] [PubMed] [Google Scholar]
- 84.Johns G. How methodological diversity has improved our understanding of absenteeism from work. Hum Resour Manage Rev. 2003;13(2):157–84. [Google Scholar]
- 85.Patton E, Johns G. Women’s absenteeism in the popular press: Evidence for a gender-specific absence culture. Hum Relat. 2007;60:1579–612. [Google Scholar]
- 86.Bratberg E, Dahl SA, Risa AE. ‘The Double Burden’: Do combinations of career and family obligations increase sickness absence among women? Eur Sociol Rev. 2002;18:233–49. [Google Scholar]
- 87.Barnett RC, Hyde JS. Women, men, work, and family. An expansionist theory. Am Psychol. 2001;56(10):781–96. doi: 10.1037//0003-066x.56.10.781. [DOI] [PubMed] [Google Scholar]
- 88.Nelson DL, Burke RJ. A framework for examining gender, work stress, and health. In: Nelson DL, Burke RJ, editors. Gender, work stress, and health. Washington DC: American Psychological Association; 2002. pp. 1–14. [Google Scholar]
- 89.Li XY, Phillips MR, Zhang YP, Xu D, Yang GH. Risk factors for suicide in China’s youth: a case-control study. Psychol Med. 2008;38(3):397–406. doi: 10.1017/S0033291707001407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Yang GH, Phillips MR, Zhou MG, Wang LJ, Zhang YP, Xu D. Understanding the unique characteristics of suicide in China: national psychological autopsy study. Biomed Environ Sci. 2005;18(6):379–89. [PubMed] [Google Scholar]
- 91.Agerbo E, Gunnell D, Bonde JP, Bo Mortensen P, Nordentoft M. Suicide and occupation: the impact of socio-economic, demographic and psychiatric differences. Psychol Med. 2007;37(8):1131–40. doi: 10.1017/S0033291707000487. [DOI] [PubMed] [Google Scholar]
- 92.Price RH, Choi JN, Vinokur AD. Links in the chain of adversity following job loss: how financial strain and loss of personal control lead to depression, impaired functioning, and poor health. J Occup Health Psychol. 2002;7(4):302–12. doi: 10.1037//1076-8998.7.4.302. [DOI] [PubMed] [Google Scholar]
- 93.Claussen B, Bjorndal A, Hjort PF. Health and re-employment in a two year follow up of long term unemployed. J Epidemiol Community Health. 1993;47(1):14–8. doi: 10.1136/jech.47.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Johansson SE, Sundquist J. Unemployment is an important risk factor for suicide in contemporary Sweden: an 11-year follow-up study of a cross-sectional sample of 37,789 people. Public Health. 1997;111(1):41–5. doi: 10.1038/sj.ph.1900317. [DOI] [PubMed] [Google Scholar]
- 95.Lewis G, Sloggett A. Suicide, deprivation, and unemployment: record linkage study. BMJ. 1998;317(7168):1283–6. doi: 10.1136/bmj.317.7168.1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kim IH, Muntaner C, Khang YH, Paek D, Cho SI. The relationship between nonstandard working and mental health in a representative sample of the South Korean population. Soc Sci Med. 2006;63(3):566–74. doi: 10.1016/j.socscimed.2006.02.004. [DOI] [PubMed] [Google Scholar]
- 97.U.S. Department of Labor, BoLS. [(Accessed 15 October 2007)];An analysis of workplace suicides, 1992–2001. 2004 28 January; Available at http://www.bls.gov/opub/cwc/sh20040126ar01p1.htm.
- 98.Mahon MJ, Tobin JP, Cusack DA, Kelleher C, Malone KM. Suicide among regular-duty military personnel: a retrospective case-control study of occupation-specific risk factors for workplace suicide. Am J Psychiatry. 2005;162(9):1688–96. doi: 10.1176/appi.ajp.162.9.1688. [DOI] [PubMed] [Google Scholar]
- 99.Tsutsumi A, Kayaba K, Ojima T, Ishikawa S, Kawakami N. Low control at work and the risk of suicide in Japanese men: a prospective cohort study. Psychother Psychosom. 2007;76(3):177–85. doi: 10.1159/000099845. [DOI] [PubMed] [Google Scholar]
- 100.Amagasa T, Nakayama T, Takahashi Y. Karojisatsu in Japan: characteristics of 22 cases of work-related suicide. J Occup Health. 2005;47(2):157–64. doi: 10.1539/joh.47.157. [DOI] [PubMed] [Google Scholar]
- 101.Mino Y, Babazono A, Tsuda T, Yasuda N. Can stress management at the workplace prevent depression? A randomized controlled trial. Psychother Psychosom. 2006;75(3):177–82. doi: 10.1159/000091775. [DOI] [PubMed] [Google Scholar]
- 102.van der Klink JJ, Blonk RW, Schene AH, van Dijk FJ. The benefits of interventions for work-related stress. Am J Public Health. 2001;91(2):270–6. doi: 10.2105/ajph.91.2.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Lo Sasso AT, Rost K, Beck A. Modeling the impact of enhanced depression treatment on workplace functioning and costs: a cost-benefit approach. Med Care. 2006;44(4):352–8. doi: 10.1097/01.mlr.0000204049.30620.1e. [DOI] [PubMed] [Google Scholar]
- 104.Wang PS, Patrick A, Avorn J, Azocar F, Ludman E, McCulloch J, et al. The costs and benefits of enhanced depression care to employers. Arch Gen Psychiatry. 2006;63(12):1345–53. doi: 10.1001/archpsyc.63.12.1345. [DOI] [PubMed] [Google Scholar]
- 105.Mikkelsen A, Saksvik PO. Impact of a participatory organizational intervention on job characteristics and job stress. Int J Health Serv. 1999;29(4):871–93. doi: 10.2190/KLPQ-FTH3-WHH5-PPP1. [DOI] [PubMed] [Google Scholar]
- 106.Druss BG, Rosenheck RA, Sledge WH. Health and disability costs of depressive illness in a major U.S. corporation. Am J Psychiatry. 2000;157(8):1274–8. doi: 10.1176/appi.ajp.157.8.1274. [DOI] [PubMed] [Google Scholar]
- 107.Smith JL, Rost KM, Nutting PA, Libby AM, Elliott CE, Pyne JM. Impact of primary care depression intervention on employment and workplace conflict outcomes: is value added? J Ment Health Policy Econ. 2002;5(1):43–9. [PubMed] [Google Scholar]


