Abstract
Hand-held based optical imaging systems are a recent development towards diagnostic imaging of breast cancer. To date, all the hand-held based optical imagers are used to perform only surface mapping and target localization, but are not capable of demonstrating tomographic imaging. Herein, a novel hand-held probe based optical imager is developed towards three-dimensional (3-D) optical tomography studies. The unique features of this optical imager, which primarily consists of a hand-held probe and an intensified charge coupled device detector, are its ability to; (i) image large tissue areas (5×10 sq. cm) in a single scan, (ii) perform simultaneous multiple point illumination and collection, thus reducing the overall imaging time; and (iii) adapt to varying tissue curvatures, from a flexible probe head design. Experimental studies are performed in the frequency domain on large slab phantoms (∼650 ml) using fluorescence target(s) under perfect uptake (1:0) contrast ratios, and varying target depths (1–2 cm) and X-Y locations. The effect of implementing simultaneous over sequential multiple point illumination towards 3-D tomography is experimentally demonstrated. The feasibility of 3-D optical tomography studies has been demonstrated for the first time using a hand-held based optical imager. Preliminary fluorescence-enhanced optical tomography studies are able to reconstruct 0.45 ml target(s) located at different target depths (1–2 cm). However, the depth recovery was limited as the actual target depth increased, since only reflectance measurements were acquired. Extensive tomography studies are currently carried out to determine the resolution and performance limits of the imager on flat and curved phantoms.
Keywords: fluorescence optical tomography, hand-held, optical tomography, fluorescence, phantoms
INTRODUCTION
Diagnostic imaging of early-stage breast cancer is essential for decreasing the cancer death rate in women in the United States. The conventional anatomical based screening techniques are neither comprehensive nor infallible, especially in women with dense breast tissues. Over the past 20 years, near-infrared (NIR) optical imaging approaches have been developed for breast cancer diagnosis, based upon the endogenous absorption contrast owing to the nonspecific process of angiogenesis1, 2, 3, 4, 5, 6, 7, 8, 9, 10 NIR light between 700 and 900 nm wavelengths is minimally absorbed and preferentially scattered, allowing its propagation through deep tissues. In recent years, external contrast agents are used to enhance the optical contrast between the diseased and normal tissue regions (i.e., fluorescence-enhanced optical imaging) and thus molecularly target metastatic cancer cells within the breast tissue.11, 12, 13, 14, 15
NIR optical imaging (with or without fluorescence) employs different source-detector imaging configurations during actual experimental studies. These imaging configurations can be broadly classified into:10, 16 (i) compressed tissue-based configuration, (ii) circular configuration, and (iii) subsurface configuration. To date, most three-dimensional (3-D) optical imaging studies towards breast cancer diagnosis are restricted either to compressed tissue configuration2, 17, 18, 19, 20, 21 or circular configuration.22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36 The compressed tissue configuration is analogous to x-ray mammography, and is disadvantageous due to minimal patient comfort from tissue compression and limited information obtained around the entire breast tissue volume. The circular configuration has minimal patient discomfort, but is limited by the bulky and nonportable instrumentation. Subsurface configuration is a relatively new method that requires no tissue compression, and can be designed to mimic a portable and flexible imaging probe.32, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50 However, 3-D tomography studies using the subsurface imaging configuration are limited32, 49, 50 and challenging due to limited depth information obtained using only reflectance-based measurements during imaging reconstructions.
In recent years, hand-held based optical imaging systems, employing the subsurface imaging configuration, are developed in an attempt to translate the technology to the clinic, with maximum patient comfort and portability (against the bulky optical imagers available). However, the hand-held optical imagers available to date37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48 are not capable of: (i) performing 2-D or 3-D optical tomography, since the source and detector points are not co-registered onto the tissue contours, thus limiting them to only surface imaging and 2-D target localization; and (ii) contouring along tissue curvatures with good surface contact, since the hand-held probes have a flat surface.
Herein, a novel hand-held probe based optical imaging system is developed and 3-D optical tomography using fluorescence contrast agents has been demonstrated under different experimental conditions. A frequency-domain intensified charge-coupled device (ICCD) based detection system was coupled to a unique hand-held optical probe, such that simultaneous multiple point illumination and collection is possible over large areas (5×10 cm2). The effect of simultaneous multiple point illumination measurement geometry over sequential single point illumination geometry, in terms of total area of detected fluorescence amplitude and overall signal strength, has been demonstrated experimentally. Three-dimensional (fluorescence-enhanced) optical tomography has been successfully performed for the first time using a hand-held based optical imager, accounting for the excitation leakage issues as well.
MATERIALS AND METHODS
Instrumentation: The hand-held probe based optical imager
Hand-held probe
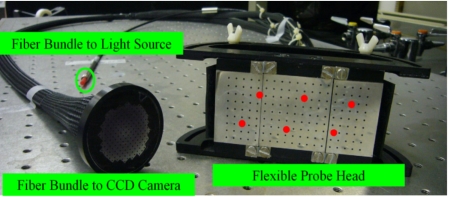
A portable and flexible hand-held optical probe was recently developed in our Optical Imaging Laboratory.51 The unique features of this probe are its ability to: (i) perform simultaneous multiple point illumination and collection, thus decreasing the total data acquisition time; and (ii) adapt to varying tissue curvatures, thus obtaining both trans-illumination and reflectance measurements. The major components of the hand-held probe are the 5×10 cm2 probe head constituting the illuminating∕collecting optical fibers, a source fiber bundle, and a collection fiber bundle (Romack Inc., Williamsburg, VA) (see Fig. 1). The probe head consists of six illumination points and 165 collection points, with all points distributed 0.5 cm apart (see Fig. 1). The appropriate number of illuminating and collecting fibers for the given probe head area, along with their appropriate layout, were determined from homogeneous fluorescence simulation studies performed on slab phantoms.51 Herein, the hand-held optical probe is coupled to the source end (laser diode) and detector end (intensified charge coupled device, ICCD) via the source fiber bundle and collection fiber bundle, respectively.
Figure 1.
The hand-held probe consists of a probe head, a source fiber bundle, and a collection fiber bundle. The solid dots on the probe represent the six illumination points.
Imaging system
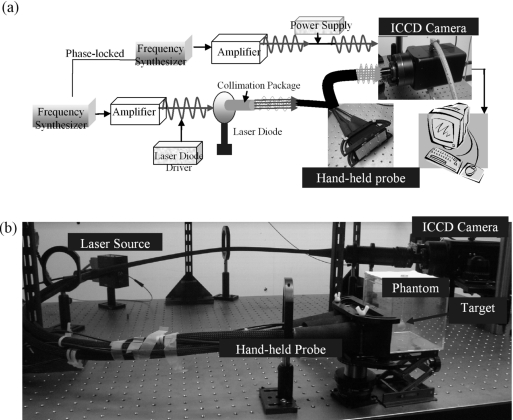
A frequency-domain based imaging system is developed for the current studies (see Fig. 2). A modulated (100 MHz) laser light source is generated using a 785-nm-wavelength laser diode (530 mW, HPD1005-9MM, Intense Ltd., North Brunswick, NJ) and a frequency synthesizer (HP 8656B, Hayward, CA). The ac and dc power levels for the laser source are chosen such that the modulation depth (ac∕dc) at the source end is maintained at 95%. In our case, the dc current of laser light is set to 217 mA, and the rf signal (i.e., ac signal) is set to +29.7 dBM. The rf signal is provided by a +27 dBM rf amplifier (ENI500L, ENI Inc., Rochester, NY) and the frequency synthesizer (−127 dBM to +13 dBM range), with power set to +2.7 dBM. The modulation source light is connected to source fiber bundle of the hand-held probe via a collimator-diffuser package, such that the single modulated laser source output can be split into six equal-intensity simultaneous modulated point sources.51
Figure 2.
(a) Schematic of the instrumentation for the hand-held probe based frequency domain ICCD optical imager. The hand-held probe is coupled to the laser source and ICCD detector for illumination and detection, respectively. (b) Experimental setup of the hand-held probe based optical imager for obtaining fluorescence measurements from a slab phantom. During actual experiments, the acrylic container was filled with 1% Liposyn solution as well.
A gain modulated ICCD detection system is developed in order to acquire optical signals from various point locations simultaneously. The ICCD detector consists of an image intensifier (FS9910, ITT Night Vision, VA) that is optically coupled to a 16 bit frame transfer CCD camera (PI-SCX 7495-0002, Roper Scientific, Trenton, NJ). The detector is modulated at the image intensifier end (at its photocathode), using a second frequency synthesizer (PTS 310, Programmed Test Sources Inc., Littleton, MA) that is phase locked with the frequency synthesizer at the source end. The dc (−24 V) and ac values (+53 dBM) at the image intensifier are chosen such that the modulation depth is ∼90% at the detector end. The ac (or rf) signal is provided by a +40 dBM rf amplifier (ENI503L, ENI Inc., Rochester, NY) and the PTS frequency synthesizer (0 dBM to +13 dBM range), with power set to +13 dBM. The ICCD detector acquires the modulated optical signal from the tissue surface via the collection fiber bundle. The fiber bundle is coupled to the ICCD camera using a focusing lens (50 mm, f∕1.8D AF model, Nikon Inc., Melville, NY). The weak fluorescence optical signals are filtered from the attenuated, yet strong excitation signal via interference filters. In the current study, two 830 nm interference filters of blocking OD 4 and 6 (HRF-830.0, blocking OD 6 and F-830.0, blocking OD 4, CVI Laser, Albuquerque, NM) are used together, in order to eliminate the excitation leakage and collect only the fluorescence signals. Preliminary experimental studies on nonfluorescing homogenous phantoms showed that the use of two interference filters (OD6 and OD4) reduced the excitation leakage by two orders of magnitude over using a single interference (OD6) filter.
During our instrument assessment studies, it was observed that maximum recovered modulation depth in homogeneous fluorescence phantoms was ∼90%. This recovered modulation depth was close to the modulation depth at the source and detector ends (95% and 90%, respectively), which indicates that the quality of the recovered frequency-domain signal is high. In other words, the high modulated fluorescence signal is an indicator of the effectiveness of the imaging system to operate as a frequency-domain imaging system and recover the modulated (yet weak) fluorescence signals effectively.
Data acquisition
Homodyne based imaging is performed in order to acquire frequency-domain measurements, wherein the modulation frequency at the source and detector end are maintained constant. A phase delay is introduced between the two phase locked frequency synthesizers.33, 52 Steady-state phase-sensitive images are acquired by the CCD camera, at phase delays (here 32) varying between 0 to 2π. For all experiments, the exposure time of the CCD camera is set to 0.2 s, and the acquired image of 1024×1024 pixels is hardware binned to 128×128 pixels, in order to improve signal to noise ratio, and also shorten the image readout time. The amplitude and phase (ac and θ) information for each of the 128×128 pixel is extracted using fast Fourier transforms (FFTs), followed by extracting the ac and θ values for the 165 collection point locations on the hand-held probe head.
A referencing technique is applied to the fluorescence optical measurements (ac and θ), in order to overcome the various instrument effects. The amplitude and phase measurement at each point location (i) are referenced with respect to the point location (ref) with maximum fluorescence amplitude, in each experimental case.
| (1) |
where acr represents ac ratio (i.e. referenced ac), and RPS represents relative phase shift (i.e. referenced phase shift).
A subtraction-based postprocessing technique (or “subtraction technique”) was employed on acquired fluorescence measurements to further eliminate excitation leakage, apart from using two interference filters. Initially, optical measurements (using both interference filters) were obtained from a nonfluorescence homogenous phantom, wherein the signals detected are a representation of the excitation leakage (or background noise). By subtracting this background noise from fluorescence measurements of any given phantom study, the excitation leakage can be removed to a greater extent.
Experimental studies
Experimental studies were performed on heterogeneous phantoms to demonstrate the feasibility of 3-D tomography using the hand-held based imaging system. The heterogeneous phantom studies employed a single fluorescence target under perfect uptake conditions (i.e., no fluorescence in the background). In all these phantom studies, 1% Liposyn solution (Liposyn II, 20%, Henry Schein, Melville, NY) was used to mimic the human breast tissue for its similarities in optical scattering coefficient.53 The 1% Liposyn solution was filled into a transparent acrylic container (10×10×10 cm3) up to a volume of 650 ml. A hollow clear plastic sphere (volume of 0.45 cm3) was filled with 1 μM Indocyanine green dye (ICG, fluorescing contrast agent) in 1% Liposyn solution, and suspended in the slab phantom to mimic a target (i.e., a tumor) as shown in Fig. 2b. Sodium polyaspartate (MW 3000-8000) (Sigma-Aldrich Chemical Co., St. Louis, CO) was used as a stabilizer for ICG, since ICG is highly unstable and tends to degrade in aqueous solution.54 The optical properties of 1% Liposyn solution are shown in Table 1. The optical properties of the fluorescence agent (ICG) were determined from its concentration and extinction coefficient (also listed in Table 1).33 The light transmission loss (∼10%) due to acrylic sphere was taken into account for the quantum efficiency of ICG (during simulation studies).
Table 1.
Optical properties of fluorescent target and nonfluorescent background for all phantom studies.
| μax(cm−1) | μam(cm−1) | |||||||
|---|---|---|---|---|---|---|---|---|
| Optical properties | μaxfa | μaxib | μamfa | μamib | μsx(cm−1)c | μsm(cm−1)c | Φd | τd (ns) |
| Target | 0.3 | 0.04 | 0.506 | 0.046 | 10.87 | 9.82 | 0.01088 | 0.56 |
| Background | 0.00 | 0.04 | 0.00 | 0.046 | 9.42 | 6.95 | ||
Absorption coefficient due to the fluorophores at excitation and emission wavelengths, respectively.
Absorption coefficient due to the chromophores at excitation and emission wavelengths, respectively.
Scattering coefficient due to the chromophores at excitation and emission wavelengths, respectively.
Quantum efficiency and lifetime for ICG, respectively.
Two sets of experimental studies were performed. In experimental study I, the effect of implementing the unique simultaneous multiple point illumination geometry for 3-D tomographic imaging was assessed in comparison to the conventionally used sequential multiple point illumination geometry. In this study, the slab phantom had a single target located 1 cm deep from the imaging surface (i.e., at [5 2.5 1] cm). Fluorescence measurements were acquired using both the illumination geometries, under the same experimental conditions. For sequential multiple point illumination, each of the six point sources were illuminated sequentially (while the rest of source fibers were covered by light-blocking materials) and the fluorescence measurements from the 165 collection points were acquired simultaneously. During both the simultaneous and sequential illumination geometry based studies, the integration time of the camera was constant (0.2 s) and only the gain settings at the image intensifier end were adjusted in order to amplify the weak fluorescence signals. The subtraction technique was implemented to the fluorescence measurements obtained from both the illumination geometries and the measurements were referenced (as described in Sec. 2A3) prior to performing the 3-D image reconstructions. The 3-D tomographic results obtained using both the illumination geometries were compared (as described in Sec. 3A).
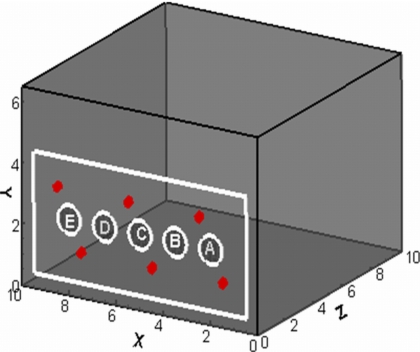
In experimental study II, the effect of implementing the unique simultaneous multiple point illumination geometry on target depth recovery was assessed. In this study, the tissue phantom had a single target located at five different x-y locations, and under two target depths of 1.5 and 2 cm deep from the imaging surface (see Table 2 and Fig. 3). In these studies as well, the integration time of the camera was constant (0.2 s) and the gain settings at the image intensifier were varied in order to amplify the weak fluorescence signals. For all phantom studies, the probe head was positioned ∼2 mm away from the phantom surface without actually contacting it. The fluorescence amplitude (ac) measurements obtained under different experimental conditions were presented as 2-D surface contour plots, post to implementing the subtraction technique. Three-dimensional image reconstructions were performed using the referenced fluorescence measurements (post to implementing the subtraction technique) and the tomographic results are described in Sec. 3B.
Table 2.
The target location details for different experimental cases (A–E) at two different target depths.
| A | B | C | D | E | |
|---|---|---|---|---|---|
| X (cm) | 2 | 3.5 | 5 | 6.5 | 8 |
| Y (cm) | 2.5 | 2.5 | 2.5 | 2.5 | 2.5 |
| Z (cm) | 1.5 & 2 | 1.5 & 2 | 1.5 & 2 | 1.5 & 2 | 1.5 & 2 |
Figure 3.
Target’s X-Y location with respect to the slab phantom for different experimental cases (A-E) shown as white hollow circles. The same X-Y locations were used for different target depths of 1.5 and 2.0 cm deep, during the heterogeneous phantom studies. The gray shaded circles represent the six simultaneous points of illumination. The white rectangular box on the phantom surface represents the location of the hand-held probe during imaging.
Three-dimensional image reconstructions
Forward problem
A Galerkin finite element based method55 was used to solve for the forward problem of the coupled diffusion equations. The 3-D phantom of 10×6.5×10 cm3 (since 1% Liposyn was filled only up to 650 ml in the 10×10×10 cm3 acrylic container) was generated and discretized into tetrahedral elements using Gambit 2.1.6 software (Fluent Inc., Lebanon, NH). The simulated phantom consisted of 10 835 nodes and 53 467 volume elements. The illumination∕collection surface (at Y=6.5 cm plane) consisted of 2080 elements and 1160 nodes, among which 171 nodes were corresponding to the six illuminating and 165 detecting (prefixed) point locations. Partial-current boundary condition56 was applied to all the six boundary surfaces, of which the top surface (Z=0 cm) is Liposyn∕air interface and rest of the surfaces are acrylic∕air interfaces. The input parameters for forward simulation studies were: (i) the optical properties of the experimental phantom; and (ii) the output power of each source fiber, which was measured using an optical power meter (PM 100, Thorlabs Inc., Newton, NJ). Although equal intensity of six sources had been attempted, the actual source strengths were unequal, and hence accounted for in the forward model.
Inverse problem
Three-dimensional image reconstructions were performed using a computationally efficient version of the Approximate Extended Kalman Filter (AEKF) algorithm,17, 33 in order to obtain the 3-D optical property map of the fluorescence absorption coefficient at excitation wavelength (μaxf). The extensive details of the complete AEKF algorithm have been described elsewhere,17, 32, 33, 34, 35 and hence briefly described here. The AEKF algorithm recursively minimizes the variance of parameter error (i.e., error in μaxf for this study), given the estimation of measurement error covariance R, model error covariance Q, and parameter error covariance P.57 The measurement error covariance R was estimated from the variances of the means of five repeated experimental measurements from each detector point. From preliminary experimental studies, it was observed that upon increasing the number of repeated measurements from five to ten, there was not a marked reduction in the measurement error for the cost of doubling the image acquisition time. Hence, the number of repetitions was limited to five, in order to minimize the total imaging time. The model error covariance Q was empirically chosen to be equal to 1∕4 of the measurement error covariance R.17, 33, 57 The covariance of measurement error and model error were implemented in the inversions to weight the updates at each iteration. The parameter error covariance P is defined as the error in the spatially distributed (unknown) parameter values (μaxf), which is used to damp into the inversion for better convergence. The reconstructions were assumed to have converged, when the root mean square output error (RMSE) was less than 1%, or the total number of iterations exceeded 50 times. The initial guess of reconstruction parameter μaxf was arbitrarily set to 0.003 cm−1 for all the reconstruction cases. The same reconstruction algorithm was implemented to measurements obtained from both sequential and simultaneous multiple point illumination geometry, with minor changes to the way the fluorescence measurements were implemented in the MATLAB-based inversion code. Three-dimensional iso-surface contour maps of the reconstructed parameter (μaxf) of the entire phantom volume were presented in TecPlot, in order to qualitatively determine the reconstructed target size and location. For quantitative estimation of the reconstructed target with respect to the background, a cutoff value of μaxf was selected based on the first break point of histogram plot of μaxf. The comparison of reconstructed vs. true target details are tabulated in terms of: (i) target centroid location; (ii) target volume, which is the total volume of all the elements whose μaxf is higher than the chosen cutoff value; and (iii) target μaxf, which is the volume weighted μaxf value of all the elements whose μaxf is above the cutoff value as shown in following formula:
| (2) |
where suffix element represents the tetrahedral elements of the finite element mesh.
RESULTS AND DISCUSSION
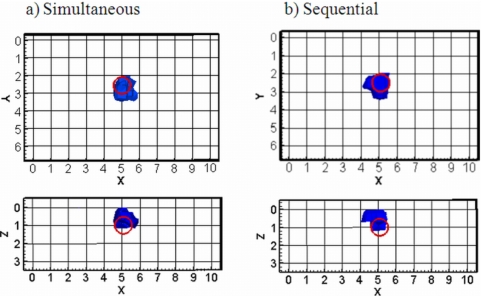
Study I: Comparison of sequential vs. simultaneous illumination
Three-dimensional image reconstructions were compared for the two illumination based geometries, i.e., sequential and simultaneous, for the experimental study I employing a single 1-cm-deep target under perfect uptake conditions. The qualitative reconstruction results are shown in Fig. 4 and the quantitative details are provided in Table 3. From Fig. 4, it is evident that the novel hand-held based optical imager employing the simultaneous multiple point illumination geometry has demonstrated the feasibility of 3-D tomographic imaging (for the first time). In addition, the target was comparably reconstructed using both the illumination geometries. This indicates that the simultaneous multiple point illumination geometry tends to maintain the quality of image reconstructions as obtained using the conventionally used sequential multiple point illumination geometry, without introducing any artifacts. This is possibly because the current experiments were carried out under the perfect uptake conditions where there was no fluorescence in the background, thus minimizing the probability of artifacts using either illumination geometry. Extensive fluorescence tomography studies are currently carried out under different experimental conditions of optical contrast ratios (i.e., include fluorescence in the background as well), target size, number, and volume in order to validate the effectiveness of simultaneous multiple point illumination geometry over the conventional sequential multiple point illumination geometry.
Figure 4.
Iso-surface contour plots of the 3-D image reconstructions presented in the X-Y and X-Z planes for heterogeneous phantoms under 1:0 fluorescence contrast ratio at a fixed target location (x=5 cm, y=2.5 cm, z=1 cm). The hollow circle in each plot represented the true target location and the irregular solid region represents the reconstructed target location. A cutoff value (selected based on the first break point of histogram plot of μaxf) was applied to iso-surface contour plots. Only 3 cm along the depth is represented in the plot, although the total depth, Z=10 cm.
Table 3.
Details of 3-D image reconstructions using simultaneous and sequential illumination for the perfect uptake (1:0) phantom study at target 3-D location of (x=5 cm, y=2.5 cm, and z=1 cm).
| Target location (cm) | Target volume (cm3) | Target μaxf value (cm−1) | ||||
|---|---|---|---|---|---|---|
| Experiment | True | Reconstructed | True | Reconstructed | True | Reconstructed |
| Simultaneous | (5.0, 2.5, 1) | (5.0, 2.7,0.3) | 0.45 | 0.67 | 0.3 | 0.8 |
| Sequential | (5.0, 2.5, 1) | (4.9, 2.6, 0.2) | 0.41 | 0.8 | ||
Apart from the comparable image quality using both the measurement geometries, the simultaneous illumination based geometry is advantageous over the sequential illumination geometry, in terms of the overall imaging time, which was reduced to l∕6th of the actual data acquisition time (without even accounting for the optical switching time and the time lost in altering the gain settings for each source during sequential illumination). During the initial design of this novel hand-held probe,51 the source-detector layout on the probe head was appropriately chosen such that a constant setting of the integration time and gain at the detector end was sufficient to recover optical signals from most of the detectors above the noise floor, when implementing simultaneous multiple point illumination geometry.
Study II: Phantom studies using simultaneous illumination
Two-dimensional surface imaging
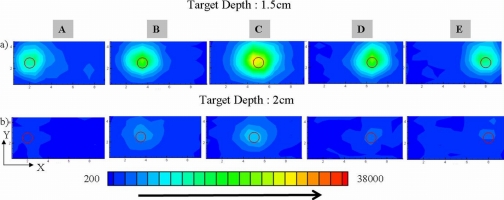
The 2-D surface contour plots (in X-Y plane) of fluorescence amplitude (ac) measurements on the illumination∕collection surface for five different target locations, and two target depths (1.5 and 2 cm deep) are presented in Fig. 5. When the target was positioned at 1.5 cm deep [Fig. 5a], for any given X-Y location, the target’s presence and 2-D location can be observed close to the true location. When the target was located 2 cm deep [Fig. 5b], for any given X-Y location, the target’s location was observed, although it was not distinctly differentiated from the background. This is possibly from the weakened fluorescence signals, which exponentially decrease with target depth.
Figure 5.
Two-dimensional surface contour plots of detected fluorescence amplitude on the imaging plane of heterogeneous phantoms under 1:0 fluorescence contrast ratio, at different target depths of 1.5 cm [rows (a)] and 2.0 cm deep [rows (b)], and different experimental target X-Y locations (cases A–E). The hollow circle in each plot represents the true target location. The fluorescence intensity of surface signal was indicated by the color map scale in the bottom of plots. In order to compare the signal strength of different experimental cases, the measurements were not referenced, but all plots were generated using the same color map scale.
With the implementation of a real-time co-registering technique, which is a focus of our ongoing efforts, a co-registered 2-D location of the target on 3-D breast tissues can serve as a real-time imaging tool (similar to ultrasound) in a clinical environment. Besides, the estimated 2-D target location can also be used as a priori information during 3-D tomography studies (part of our future studies) to reduce the computational time and possibly improve target localization, especially in large tissue volumes. However, in order to obtain more detailed target information such as target size, depth, and optical properties, 3-D tomography studies are indispensable.
Three-dimensional image reconstructions
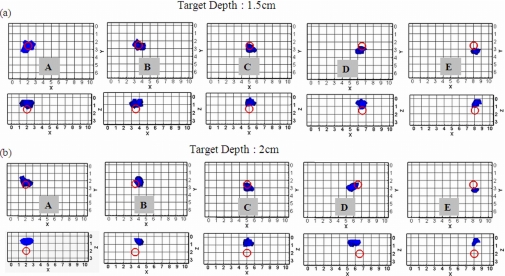
Three-dimensional image reconstructions were performed for all the ten experimental cases from study II, as described in Sec. 2B. The 3-D iso-surface contour plots are presented at X-Y and X-Z plane in order to illustrate the size and location of reconstructed target with respect to the true target size∕location, for the 1.5 cm [Fig. 6a] and 2-cm-deep target(s) [Fig. 6b]. In all the tomographic reconstructions, a single target was reconstructed without any artifacts, at both the target depths. Details of the reconstructed target location, size, and optical property (μaxf) for the 1.5- and 2-cm-deep target(s) are given in Tables 4, 5, respectively. These quantitative results showed that most of the reconstructed parameters for all experimental cases were recovered, for both the target depth cases.
Figure 6.
Iso-surface contour plots of the 3-D image reconstructions presented in the X-Y and X-Z planes for heterogeneous phantoms under 1:0 contrast ratio, different target depths of (a) 1.5 cm, and (b) 2.0 cm. The five columns in each row represent the five different target locations (A–E). The hollow circle in each plot represented the true target location and the irregular solid region represents the reconstructed target location. A cutoff value (selected based on the first break point of histogram plot of μaxf) was applied to iso-surface contour plots. Only 3 cm along the depth is represented in the plot, although the total depth, Z=10 cm.
Table 4.
Details of 3-D image reconstructions for the perfect uptake (1:0) phantom study under a target depth of 1.5 cm.
| Target location (cm) | Target volume (cm3) | Target μaxf value (cm−1) | ||||
|---|---|---|---|---|---|---|
| Experiment | True | Reconstructed | True | Reconstructed | True | Reconstructed |
| A | (2, 2.5, 1.5) | (1.9, 2.7, 0.7) | 0.81 | 0.7 | ||
| B | (3.5, 2.5, 1.5) | (3.6, 2.6, 0.8) | 0.69 | 0.7 | ||
| C | (5, 2.5, 1.5) | (5.0, 2.8, 0.5) | 0.45 | 0.39 | 0.3 | 0.8 |
| D | (6.5, 2.5, 1.5) | (6.2, 3.1, 0.5) | 0.29 | 0.8 | ||
| E | (8, 2.5, 1.5) | (8.3, 3.2, 0.3) | 0.34 | 0.3 | ||
Table 5.
Details of 3-D image reconstructions for the perfect uptake (1:0) phantom study under a target depth of 2.0 cm.
| Target location (cm) | Target volume (cm3) | Integrated μaxf value (cm−1) | ||||
|---|---|---|---|---|---|---|
| Experiment | True | Reconstructed | True | Reconstructed | True | Reconstructed |
| A | (2, 2.5, 2) | (2.1, 2.3, 0.7) | 0.49 | 0.4 | ||
| B | (3.5, 2.5, 2) | (3.9, 2.1, 0.6) | 0.36 | 0.4 | ||
| C | (5, 2.5,2) | (5.1, 2.8, 0.5) | 0.45 | 0.27 | 0.3 | 0.6 |
| D | (6.5, 2.5, 2) | (5.8, 2.8, 0.6) | 0.31 | 0.5 | ||
| E | (8, 2.5, 2) | (8.1, 3.2, 0.3) | 0.21 | 0.2 | ||
However, in all the experimental cases, the reconstructed target depth (Z axis) was closer to the phantom surface (observed even from qualitative results in Fig. 6). This could possibly be due to the fact that only reflectance measurements are acquired (from flat phantom surfaces) and used towards reconstructions. Simulations studies have been performed prior to experimental studies, using reflectance measurement obtained from similar target volumes (0.45 cm3) and depths (1.5 and 2.0 cm deep) as in the experimental cases. The simulation tomography results (using simulated measurements without adding any noise) also reconstructed the target(s) closer to the surface (not shown due to brevity). This further confirms that it is probably the underlying physics of reflectance based measurement that affects the depth recovery.
The difficulty in depth recovery from 3-D tomography studies using only reflectance-based measurements was also reported by other researchers.32, 58, 59, 60, 61 Although different researchers used different measurement geometries (sequential multiple point illumination, and area illumination), instrumentation setups, and reconstruction algorithms, all the studies commonly acquired only reflectance-based measurements. Consistently it was observed that the reconstructed target was closer to the surface for different depth studies. In our current study, since a different illumination scheme (multiple point simultaneous illumination) has been employed, tomography studies were performed at various target depths (reaching the reported limits of 1.5–2 cm deep) in order to determine if the overall improved signal strength from simultaneous multiple point illumination over sequential illumination34, 51 improves the depth recovery. However, the current studies demonstrated that the limitation in depth recovery was independent of the nature of illumination geometry, and was still affected by the physics of reflectance-based measurements.
These tomography studies also imply that trans-illumination based measurements are possibly required apart from reflectance measurements, in order to recover the target depth accurately. Tomographic imaging studies using trans-illumination measurements acquired by the hand-held based optical imager are the focus of our future work on curved phantoms under different experimental conditions. During our instrumentation design and development phase, the probe head was built such that it is capable of contouring to the tissue curvatures (i.e., the curved phantoms) and obtain trans-illumination measurements apart from reflectance measurements.
CONCLUSIONS
A novel hand-held probe based optical imaging system has been developed with the following unique features: (i) a hand-held optical probe with multiple sources and detectors that allows imaging over larger areas (5×10 cm2) in a single scan, (ii) simultaneous illumination and collection based measurement geometry that allows rapid data acquisitions (<20 s per location of the probe); (iii) a gain-modulated ICCD detector for rapid data acquisitions of weaker optical (fluorescence) signals; (iv) a flexible hand-held probe that can contour along any tissue curvature (part of future studies to implement the probe on curved surfaces); and (v) a portable setup to allow bedside imaging in a clinical environment. Three-dimensional fluorescence tomography studies have been successfully demonstrated for the first time using a hand-held based optical imager. From the preliminary tomography studies on large slab phantoms (∼650 ml), target(s) of 0.45 ml were reconstructed at various target depths (1–2 cm), upon using ICG under perfect uptake conditions. The target depth recovery was limited (as observed by other researchers as well) and appears to be predominantly affected by the physics of reflectance-based measurements.
Excitation leakage significantly contaminated the acquired weak fluorescence measurements, especially when the target was located deep (here, 2 cm). The use of appropriate optical (interference) filters along with a subtraction-based postprocessing technique remarkably aided in removing the artifacts arising from excitation leakage, both in 2-D surface contour plots and in 3-D image reconstructions. Extensive 3-D tomography studies are currently being carried out using different target depths, volumes, number, and target:background optical contrast ratios in order to determine the performance limits and resolution of our optical imager. In addition, future studies will implement the rough estimate of the target location (as obtained from 2-D surface contour plots) as a priori information, in order to improve the quality of reconstructions, and also reduce the computational time. Parallel to these studies, experiments are being carried out using the hand-held probe on curved phantoms (since the probe head is flexible to contour along curvatures up to 45°), wherein both reflectance and trans-illumination based measurements can possibly improve the quality of depth reconstructions. Efforts are made towards developing innovative methods to obtain real-time 3-D co-registered images of the tissue surface during multiple scans, using the hand-held optical imager.
In summary, the novel hand-held optical imaging system with its unique features, has potential to significantly impact the clinical translation of the optical imaging technology as a bedside portable hand-held based imaging device for 3-D target localization without the use of a second imaging modality (e.g., an expensive MRI image) for co-registration. On a long term, the developing hand-held based optical imaging technology also has applicability towards prognostic breast imaging, image-guided breast cancer therapy, and volumetric analysis of tumors in response to chemotherapeutic trials.
ACKNOWLEDGMENTS
This work was funded in part by the Florida Department of Health (06BB-08) and National Institutes of Health Grant No. R15CA119253-01A1.
References
- Franceschini M. A., Moesta K. T., Fantini S., Gaida G., Gratton E., Jess H., Mantulin W. W., Seeber M., Schlag P. M., and Kaschke M., “Frequency-domain techniques enhance optical mammography: Initial clinical results,” Proc. Natl. Acad. Sci. U.S.A. 10.1073/pnas.94.12.6468 94, 6468–6473 (1997). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fantini S., Walker S. A., Franceschini M. A., Kaschke M., Schlag P. M., and Moesta K. T., “Assessment of the size, position, and optical properties of breast tumors in vivo by noninvasive optical methods,” Appl. Opt. 37, 1982–1989 (1998). [DOI] [PubMed] [Google Scholar]
- Moesta K. T., Fantini S., Jess H., Totkas S., Franceschini M. A., Kaschke M., and Schlag P. M., “Contrast features of breast cancer in frequency-domain laser scanning mammography,” J. Biomed. Opt. 10.1117/1.429869 3, 129–136 (1998). [DOI] [PubMed] [Google Scholar]
- Grosenick D., Wabnitz H., Rinneberg H. H., Moesta K. T., and Schlag P. M., “Development of a time-domain optical mammograph and first in vivo applications,” Appl. Opt. 38, 2927–2943 (1999). [DOI] [PubMed] [Google Scholar]
- Colak S. B., van der Mark M. B., ’t Hooft G. W., Hoogenraad J. H., van der Linden E. S., and Kuijpers F. A., “Clinical optical tomography and NIR spectroscopy for breast cancer detection,” IEEE J. Sel. Top. Quantum Electron. 10.1109/2944.796341 5, 1143–1158 (1999). [DOI] [Google Scholar]
- Pogue B. W., Poplack S. P., McBride T. O., Wells W. A., Osterman K. S., Osterberg U. L., and Paulsen K. D., “Quantitative hemoglobin tomography with diffuse near-infrared spectroscopy: Pilot results in the breast,” Radiology 218, 261–266 (2001). [DOI] [PubMed] [Google Scholar]
- Jiang H., Xu Y., Iftimia N., Eggert J., Klove K., Baron L., and Fajardo L., “Three-dimensional optical tomographic imaging of breast in a human subject,” IEEE Trans. Med. Imaging 10.1109/42.974928 20, 1334–1340 (2001). [DOI] [PubMed] [Google Scholar]
- Li A., Boverman G., Zhang Y., Brooks D., Miller E. L., Kilmer M. E., Zhang Q., Hillman E. M., and Boas D. A., “Optimal linear inverse solution with multiple priors in diffuse optical tomography,” Appl. Opt. 10.1364/AO.44.001948 44(10), 1948–1956 (2005). [DOI] [PubMed] [Google Scholar]
- Zhang Q., Brukilacchio T. J., Li A., Stott J. J., Chaves T., Hillman E., Wu T., Chorlton M., Rafferty E., Moore R. H., Kopans D. B., and Boas D. A., “Coregistered tomographic x-ray and optical breast imaging: Initial results,” J. Biomed. Opt. 10(2), 024033 (2005). [DOI] [PubMed] [Google Scholar]
- Gibson A. P., Hebden J. C., and Arridge S. R., “Recent advances in diffuse optical imaging,” Phys. Med. Biol. 10.1088/0031-9155/50/4/R01 50(4), R1–43 (2005). [DOI] [PubMed] [Google Scholar]
- Hawrysz D. J. and Sevick-Muraca E. M., “Developments toward diagnostic breast cancer imaging using near-infrared optical measurements and fluorescent contrast agents,” Neoplasia 10.1038/sj/neo/7900118 2, 388–417 (2000). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Licha K., “Contrast agents for optical imaging,” Top. Curr. Chem. 222, 1–29 (2002). [Google Scholar]
- Sevick-Muraca E. M., Houston J. P., and Gurfinkel M., “Fluorescence-enhanced, near infrared diagnostic imaging with contrast agents,” Curr. Opin. Chem. Biol. 10.1016/S1367-5931(02)00356-3 6, 642–650 (2002). [DOI] [PubMed] [Google Scholar]
- Sevick-Muraca E. M., Godavarty A., Houston J. P., Thompson A. B., and Roy R., “Near-infrared imaging with fluorescent contrast agents,” in Handbook of Biomedical Fluorescence, edited by Pogue Brian W. and Mycek Mary-Ann (Dekker, New York, 2003). [Google Scholar]
- Gurfinkel M., Ke S., Wen X., Li C., and Sevick-Muraca E. M., “Near-infrared fluorescence optical imaging and tomography,” Dis. Markers 19(2-3), 107–121 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pogue B. W., McBride T. O., Osterberg U. L., and Paulsen K. D., “Comparison of imaging geometries for diffuse optical tomography of tissue,” Opt. Express 4(8), 270–286 (1999). [DOI] [PubMed] [Google Scholar]
- Eppstein M. J., Hawrysz D. J., Godavarty A., and Sevick-Muraca E. M., “Three-dimensional near-infrared fluorescence tomography with Bayesian methodologies for image reconstruction from sparse and noisy data sets,” Proc. Natl. Acad. Sci. U.S.A. 10.1073/pnas.112217899 99, 9619–9624 (2002). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milstein B., Stott J. J., Oh S., Boas D. A., Millane R. P., Bouman C. A., and Webb K. J., “Fluorescence optical diffusion tomography using multiple-frequency data,” J. Opt. Soc. Am. A 10.1364/JOSAA.21.001035 21(6), 1035–1049 (2004). [DOI] [PubMed] [Google Scholar]
- Lee J. and Sevick-Muraca E. M., “3-D Fluorescence enhanced optical tomography using references frequency-domain photon migration measurements at emission and excitation measurements,” J. Opt. Soc. Am. A 12, 759–771 (2002). [DOI] [PubMed] [Google Scholar]
- Quaresima V., Matcher S. J., and Ferrari M., “Identification and quantification of intrinsic optical contrast for near-infrared mammography,” Photochem. Photobiol. 10.1111/j.1751-1097.1998.tb05159.x 67, 4–14 (1998). [DOI] [PubMed] [Google Scholar]
- Li X., Culver J., Durduran T., Chance B., Yodh A. G., and Pattanayak D. N., “Diffraction tomography with diffuse-photon density waves: Clinical studies and background subtraction,” Advances in Optical Imaging and Photon Migration (AOIPM), (OSA, Orlando, FL, 1993). [Google Scholar]
- Ntziachristos Y. and Weissleder R., “Experimental three-dimensional fluorescence reconstruction of diffuse media by use of a normalized Born approximation,” Opt. Lett. 10.1364/OL.26.000893 26, 893–895 (2001). [DOI] [PubMed] [Google Scholar]
- Yang Y., Iftimia N., Xu Y., and Jiang H., “Frequency-domain fluorescent diffusion tomography of turbid media and in vivo tissues,” in Optical Tomography and Spectroscopy of Tissue IV, edited by B. Chance, R. R. Alfano, B. J. Tromberg, Proc. SPIE 10.1117/12.434529 4250, 537–545 (2001). [DOI] [Google Scholar]
- Ntziachristos V., Bremer C., and Weissleder R., “Fluorescence imaging with near-infrared light: New technological advances that enable in vivo molecular imaging,” Eur. Radiol. 13, 195–208 (2003). [DOI] [PubMed] [Google Scholar]
- Ntziachristos V. and Weissleder R., “Charge-coupled-device based scanner for tomography of fluorescent near-infrared probes in turbid media,” Med. Phys. 10.1118/1.1470209 29, 803–809 (2002). [DOI] [PubMed] [Google Scholar]
- Ntziachristos Y., Bremer C., Tung C., and Weissleder R., “Imaging cathepsin B up-regulation in HT-1080 tumor models using fluorescence-mediated molecular tomography (FMT),” Acad. Radiol. 9(suppl. 2), S323–S325 (2002). [DOI] [PubMed] [Google Scholar]
- Schulz R. B., Ripoll J., and Ntziachristos V., “Noncontact optical tomography of turbid media,” Opt. Lett. 10.1364/OL.28.001701 28(18), 1701–1703 (2003). [DOI] [PubMed] [Google Scholar]
- Ntziachristos V., Schellenberger E. A., Ripoll J., Yessayan D., Graves E., Bogdanov A., Josephson J. L., and Weissleder R., “Visualization of antitumor treatment by means of fluorescence molecular tomography with an annexin V-Cy5.5 conjugate,” Proc. Natl. Acad. Sci. U.S.A. 10.1073/pnas.0401137101 101(33), 12294–12299 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz R. B., Ripoll J., and Ntziachristos V., “Experimental fluorescence tomography of tissues with noncontact measurements,” IEEE Trans. Med. Imaging 10.1109/TMI.2004.825633 23(4), 492–500 (2004). [DOI] [PubMed] [Google Scholar]
- Bremer C., Ntziachristos V., Weitkamp B., Theilmeier G., Heindel W., and Weissleder R., “Optical imaging of spontaneous breast tumors using protease sensing ‘smart’ optical probes,” Invest. Radiol. 10.1097/01.rli.0000163797.23172.90 40(6), 321–327 (2005). [DOI] [PubMed] [Google Scholar]
- Colak S. B., Papaioannou D. G., t’Hooft G. W., van der Mark M. B., Schomberg H., Paasschens J. C. J., Melissen J. B., and van Asten N. J., “Tomographic image reconstruction from optical projections in light-diffusing media,” Appl. Opt. 36, 180–213 (1997). [DOI] [PubMed] [Google Scholar]
- Godavarty A., Thompson A. B., Roy R., Eppstein M. J., Zhang C., Gurfinkel M., and Sevick-Muraca E. M., “Diagnostic imaging of breast cancer using fluorescence-enhanced optical tomography: Phantom studies,” J. Biomed. Opt. 10.1117/1.1691027 9(3), 488–496 (2004). [DOI] [PubMed] [Google Scholar]
- Godavarty A., Eppstein M. J., Zhang C., Theru S., Thompson A. B., Gurfinkel M., and Sevick-Muraca E. M., “Fluorescence-enhanced optical imaging in large tissue volumes using a gain modulated ICCD camera,” Phys. Med. Biol. 10.1088/0031-9155/48/12/303 48, 1701–1720 (2003). [DOI] [PubMed] [Google Scholar]
- Godavarty A., Zhang C., Eppstein M. J., and Sevick-Muraca E. M., “Fluorescence-enhanced optical imaging of large phantoms using single and simultaneous dual point illumination geometries,” Med. Phys. 10.1118/1.1639321 31, 183–190 (2004). [DOI] [PubMed] [Google Scholar]
- Godavarty A., Sevick-Muraca E. M., and Eppstein M. J., “Three-dimensional fluorescence lifetime tomography,” Med. Phys. 10.1118/1.1861160 32, 992–1000 (2005). [DOI] [PubMed] [Google Scholar]
- Zhu B., Eppstein M. J., Sevick-Muraca E. M., and Godavarty A., “Noise pre-filtering techniques in fluorescence-enhanced optical tomography,” Opt. Express 10.1364/OE.15.011285 15(18), 11285–11300 (2007). [DOI] [PubMed] [Google Scholar]
- Tromberg B. J., Coquoz O., Fishkin J. B., Pham T., Anderson E. R., Butler J., Cahn M., Cross J. D., Venugopalan V., and Pham D., “Non-invasive measurements of breast tissue optical properties using frequency-domain photon migration,” Philos. Trans. R. Soc. London, Ser. B 10.1098/rstb.1997.0047 352(1354), 661–668 (1997). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pham T. H., Coquoz O., Fishkin J. B., Anderson E., and Tromberg B. J., “Broad bandwidth frequency domain instrument for quantitative tissue optical spectroscopy,” Rev. Sci. Instrum. 10.1063/1.1150665 71(6), 2500–2513 (2000). [DOI] [Google Scholar]
- Shah N., Cerussi A., Eker C., Espinoza J., Butler J., Fishkin J., Hornung R., and Tromberg B., “Noninvasive functional optical spectroscopy of human breast tissue,” Proc. Natl. Acad. Sci. U.S.A. 10.1073/pnas.071511098 98(8), 4420–4425 (2001). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jakubowski D. B., Cerussi A. E., Bevilacqua F., Shah N., Hsiang D., Butler J., and Tromberg B. J., “Monitoring neoadjuvant chemotherapy in breast cancer using quantitative diffuse optical spectroscopy: A case study,” J. Biomed. Opt. 10.1117/1.1629681 9(1), 230–238 (2004). [DOI] [PubMed] [Google Scholar]
- Chen N., Huang M., Xia H., and Piao D., “Portable near-infrared diffusive light imager for breast cancer detection,” J. Biomed. Opt. 10.1117/1.1695410 9(3), 504–510 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah N., Cerussi A. E., Jakubowski D., Hsiang D., Butler J., and Tromberg B. J., “Spatial variations in optical and physiological properties of healthy breast tissue,” J. Biomed. Opt. 10.1117/1.1695560 9(3), 534–540 (2004). [DOI] [PubMed] [Google Scholar]
- Chance B., Nioka S., Zhang J., Conant E. F., Hwang E., Briest S., Orel S. G., Schnall M. D., and Czerniecki B. J., “Breast cancer detection based on incremental biochemical and physiological properties of breast cancers: A six-year, two-site study,” Acad. Radiol. 12(8), 925–933 (2005). [DOI] [PubMed] [Google Scholar]
- Tromberg B. J., “Optical scanning and breast cancer,” Acad. Radiol. 12(8), 923–924, (2005). [DOI] [PubMed] [Google Scholar]
- No K. S. and Chou P. H., “Mini-FDPM and heterodyne mini-FDPM: Handheld non-invasive breast cancer detectors based on frequency domain photon migration,” IEEE Trans. Circuits Syst., I: Fundam. Theory Appl. 10.1109/TCSI.2005.857927 52(12), 2672–2685 (2005). [DOI] [Google Scholar]
- Durduran T., Choe R., Yu G., Zhou C., Tchou J. C., Czerniecki B. J., and Yodh A. G., “Diffuse optical measurement of blood flow in breast tumors,” Opt. Lett. 10.1364/OL.30.002915 30(21), 2915–2917 (2005). [DOI] [PubMed] [Google Scholar]
- Chance B., Zhao Z., Wen S., and Chen Y., “Simple ac circuit for breast cancer detection and object detection,” Rev. Sci. Instrum. 10.1063/1.2205151 77, 064301 (2006). [DOI] [Google Scholar]
- No K. S., Xie Q., Kwong R., Cerussi A., Tromberg B. J., and Chou P., “HBS: A handheld breast cancer detector based on frequency domain photon migration with full heterodyne,” Proc. IEEE BioCAS, The British Library, London: (2006).
- Bremer C., Ntziachristos V., and Weissleder R., “Optical-based molecular imaging: Contrast agents and potential medical applications,” Eur. Radiol. 13, 231–243 (2003). [DOI] [PubMed] [Google Scholar]
- Roy R., Thompson A. B., Godavarty A., and Sevick-Muraca E. M., “Tomographic fluorescence imaging in tissue phantoms: A novel reconstruction algorithm and imaging geometry,” IEEE Trans. Med. Imaging 10.1109/TMI.2004.839359 24(2), 137–154 (2005). [DOI] [PubMed] [Google Scholar]
- Jayachandran B., Ge J., Regalado S., and Godavarty A., “Design and development of a hand-held optical probe towards fluorescence diagnostic imaging,” J. Biomed. Opt. 10.1117/1.2799193 12(5), 054014 (2007). [DOI] [PubMed] [Google Scholar]
- Lakowicz J. R. and Berndt K. W., “Lifetime-selective fluorescence imaging using an rf phase-sensitive camera,” Rev. Sci. Instrum. 10.1063/1.1142413 62(7), 1727–1734 (1991). [DOI] [Google Scholar]
- Spinelli L., Torricelli A., Pifferi A., Taroni P., Danesini G. M., and Cubeddu R., “Bulk optical properties and tissue components in the female breast from multiwavelength time-resolved optical mammography,” J. Biomed. Opt. 10.1117/1.1803546 9(6), 1137–1142 (2004). [DOI] [PubMed] [Google Scholar]
- Rajagopalan R., Uetrecht P., Bugaj J. E., Achilefu S. A., and Dorshow R. B., “Stabilization of the optical tracer agent indocyanine green using noncovalent interactions,” Photochem. Photobiol. 71, 347–350 (2000). [DOI] [PubMed] [Google Scholar]
- Fedele F., Laible J. P., and Eppstein M. J., “Coupled complex adjoint sensitivities for frequency-domain fluorescence tomography: Theory and vectorized implementation,” J. Comput. Phys. 10.1016/S0021-9991(03)00150-5 187, 597–619 (2003). [DOI] [Google Scholar]
- Haskell R. C., Scasssand L. O., Tsay T.-T., Feng T.-C., M., Adams, and Tromberg B. J., “Boundary conditions for the diffusion equation in radiative transfer,” J. Opt. Soc. Am. A 11, 2727–2741 (1994). [DOI] [PubMed] [Google Scholar]
- Eppstein M. J., Dougherty D. E., Hawrysz D. J., and Sevick-Muraca E. M., “Three dimensional Bayesian optical image reconstruction with domain decomposition,” IEEE Trans. Med. Imaging 10.1109/42.918467 20(3), 147–163 (2001). [DOI] [PubMed] [Google Scholar]
- Kepshire D. S., Davis S. C., Dehghani H., Paulsen K. D., and Pogue B. W., “Subsurface diffuse optical tomography can localize absorber and fluorescent objects but recovered image sensitivity is nonlinear with depth,” Appl. Opt. 10.1364/AO.46.001669 46(10), 1669–1678 (2007). [DOI] [PubMed] [Google Scholar]
- Kepshire D. S., Davis S. C., Dehghani H., Paulsen K. D., and Pogue B. W., “Challenges in sub-surface fluorescence diffuse optical imaging,” Proc. SPIE 6434, 1–9 (2007). [Google Scholar]
- Joshi A., Bangerth W., Hwang K., Rasmussen J. C., and Sevick-Muraca E. M., “Fully adaptive FEM based fluorescence optical tomography from time-dependent measurements with area illumination and detection,” Med. Phys. 10.1118/1.2190330 33(5), 1299–1310 (2006). [DOI] [PubMed] [Google Scholar]
- Joshi A., Bangerth W., Hwang K., Rasmussen J. C., and Sevick-Muraca E. M., “Plane-wave fluorescence tomography with adaptive finite elements,” Opt. Lett. 10.1364/OL.31.000193 31(2), 193–195 (2006). [DOI] [PubMed] [Google Scholar]