Abstract
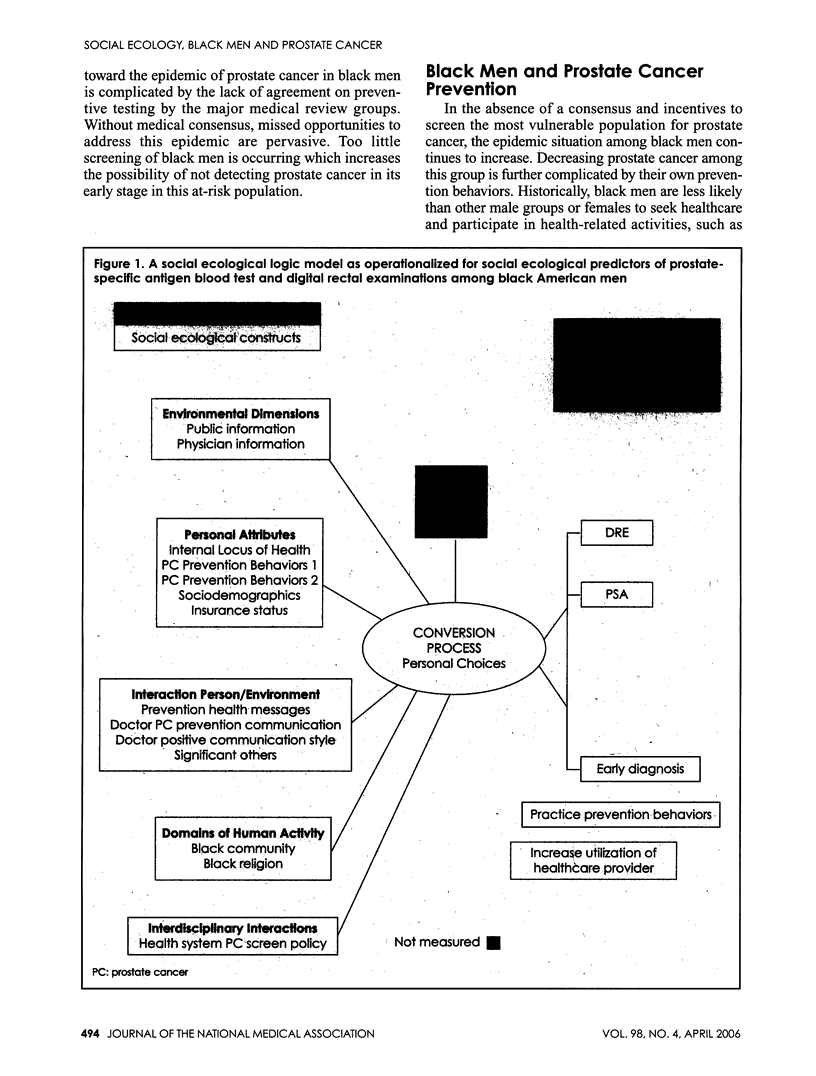
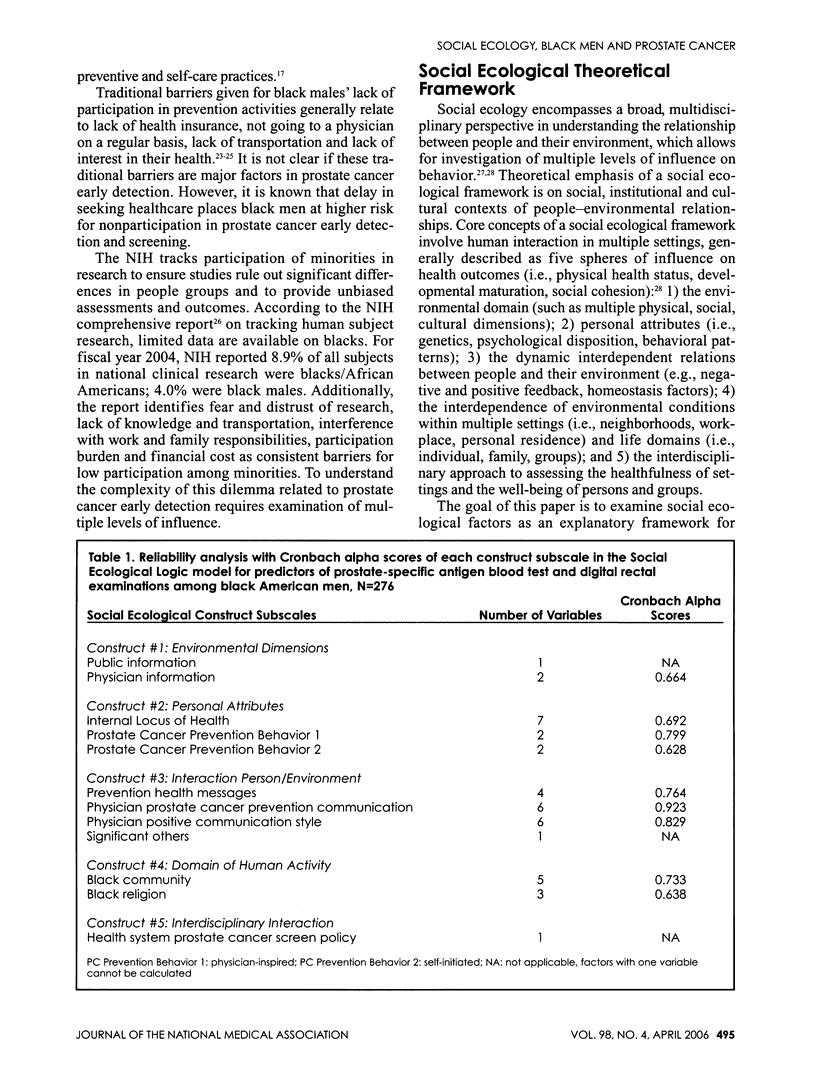
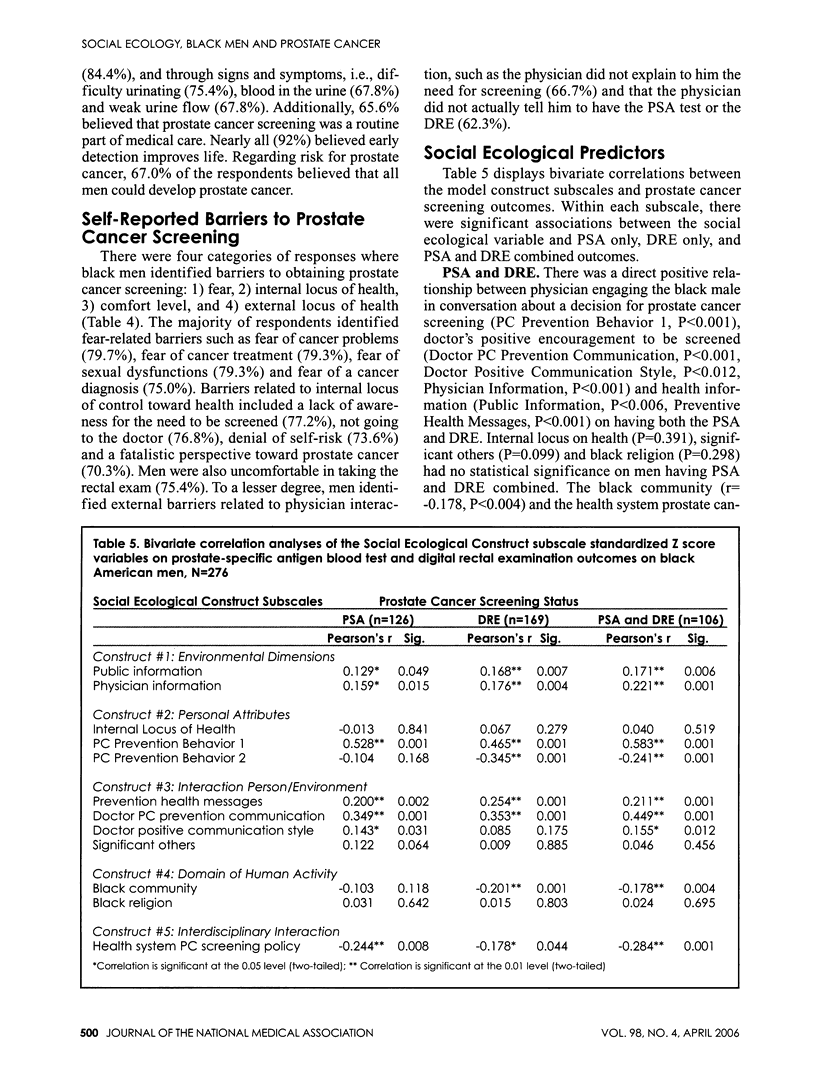
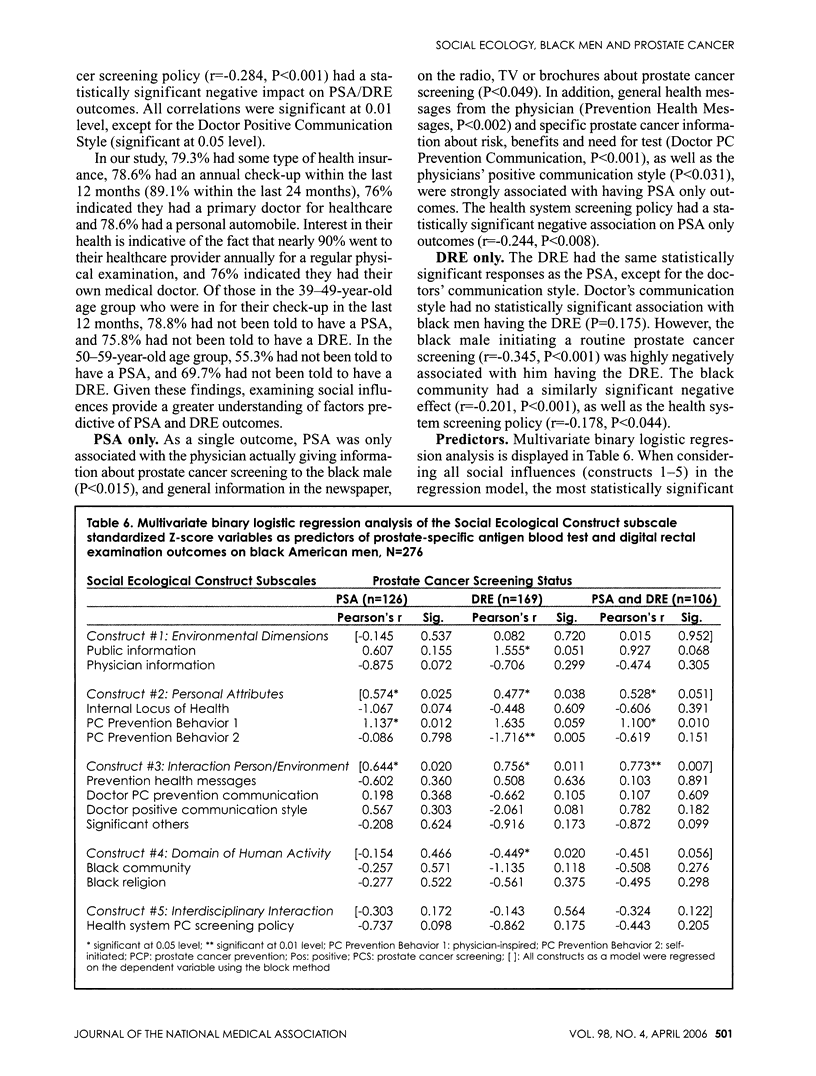
BACKGROUND: Black American men continue to suffer disproportionately from epidemically higher rates of prostate cancer. We hypothesize that complex reasons for persistently higher death rates of prostate cancer in this group are steeped in social factors associated with health access. METHODS: We utilized data from the It's All About U prostate cancer prevention study among black men to investigate: 1) what social ecological factors were predictive of prostate-specific antigen (PSA) testing and digital rectal examinations (DRE); 2) if black men were aware of prostate cancer screening and, if screening was available, would they take the PSA and DRE? Quantitative cross-sectional data from a cohort of 276 black men with no diagnosis of prostate cancer were analyzed to identify characteristics, beliefs, practices and attitudes of this group toward prostate cancer screening. We created a social ecological model to examine which social factors (i.e., environmental, personal, person/environment interplay, black culture and institutional policy) were predictive of PSA and DRE, PSA only and DRE only. To reduce data and identify data patterns, factor analyses (tested for reliability by calculating Cronbach alpha scores) were performed. Variables were standardized with Z scores and analyzed with predictive analytic software technology (SPSS, version 12). A multivariate binary logistic regression was conducted to identify predictors of PSA and DRE. RESULTS: A significant predictor of both PSA and DRE was the physician's direct prostate cancer communication message (P<0.010). Significant correlations exist in PSA and DRE outcomes with a physician's engaging communication style (P<0.012), encouragement to screen (P<0.001) and sharing prostate cancer information (P<0.001); as was men understanding the serious risk of prostate cancer (P<0.001), culture (P<0.004), positive interaction with healthcare staff, significant other(s) and providers (P<0.001), and environmental dimensions (P<0.006). A profile of four major self-reported barriers to screening were identified (i.e., fear, internal locus of health, comfort level and external locus of health). Lastly, men who utilized health systems with a prostate cancer screening policy had high percentages of PSA and DRE (63.3%), PSA only (70.9%) and DRE only (81.7%). CONCLUSION: A physician's aggressive, positive engagement in shared decision-making, tailored social influences promoting prostate cancer prevention among black men, as well as institutional screening policy, has the potential to increase early detection and reduce morbidity among this group.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Corbie-Smith Giselle, Thomas Stephen B., St George Diane Marie M. Distrust, race, and research. Arch Intern Med. 2002 Nov 25;162(21):2458–2463. doi: 10.1001/archinte.162.21.2458. [DOI] [PubMed] [Google Scholar]
- Freimuth V. S., Quinn S. C., Thomas S. B., Cole G., Zook E., Duncan T. African Americans' views on research and the Tuskegee Syphilis Study. Soc Sci Med. 2001 Mar;52(5):797–808. doi: 10.1016/s0277-9536(00)00178-7. [DOI] [PubMed] [Google Scholar]
- Kravitz R. L., Melnikow J. Engaging patients in medical decision making. BMJ. 2001 Sep 15;323(7313):584–585. doi: 10.1136/bmj.323.7313.584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krupat E., Bell R. A., Kravitz R. L., Thom D., Azari R. When physicians and patients think alike: patient-centered beliefs and their impact on satisfaction and trust. J Fam Pract. 2001 Dec;50(12):1057–1062. [PubMed] [Google Scholar]
- Nivens A. S., Herman J., Pweinrich S., Weinrich M. C. Cues to participation in prostate cancer screening: a theory for practice. Oncol Nurs Forum. 2001 Oct;28(9):1449–1456. [PubMed] [Google Scholar]
- Stokols D. Social ecology and behavioral medicine: implications for training, practice, and policy. Behav Med. 2000 Fall;26(3):129–138. doi: 10.1080/08964280009595760. [DOI] [PubMed] [Google Scholar]
- Street Richard L., Jr, Krupat Edward, Bell Robert A., Kravitz Richard L., Haidet Paul. Beliefs about control in the physician-patient relationship: effect on communication in medical encounters. J Gen Intern Med. 2003 Aug;18(8):609–616. doi: 10.1046/j.1525-1497.2003.20749.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weir Hannah K., Thun Michael J., Hankey Benjamin F., Ries Lynn A. G., Howe Holly L., Wingo Phyllis A., Jemal Ahmedin, Ward Elizabeth, Anderson Robert N., Edwards Brenda K. Annual report to the nation on the status of cancer, 1975-2000, featuring the uses of surveillance data for cancer prevention and control. J Natl Cancer Inst. 2003 Sep 3;95(17):1276–1299. doi: 10.1093/jnci/djg040. [DOI] [PubMed] [Google Scholar]
- Woods V. Diane, Montgomery Susanne B., Belliard Juan Carlos, Ramirez-Johnson Johnny, Wilson Colwick M. Culture, black men, and prostate cancer: what is reality? Cancer Control. 2004 Nov-Dec;11(6):388–396. doi: 10.1177/107327480401100606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods V. Diane, Montgomery Susanne B., Herring R. Patti. Recruiting Black/African American men for research on prostate cancer prevention. Cancer. 2004 Mar 1;100(5):1017–1025. doi: 10.1002/cncr.20029. [DOI] [PubMed] [Google Scholar]


