Abstract
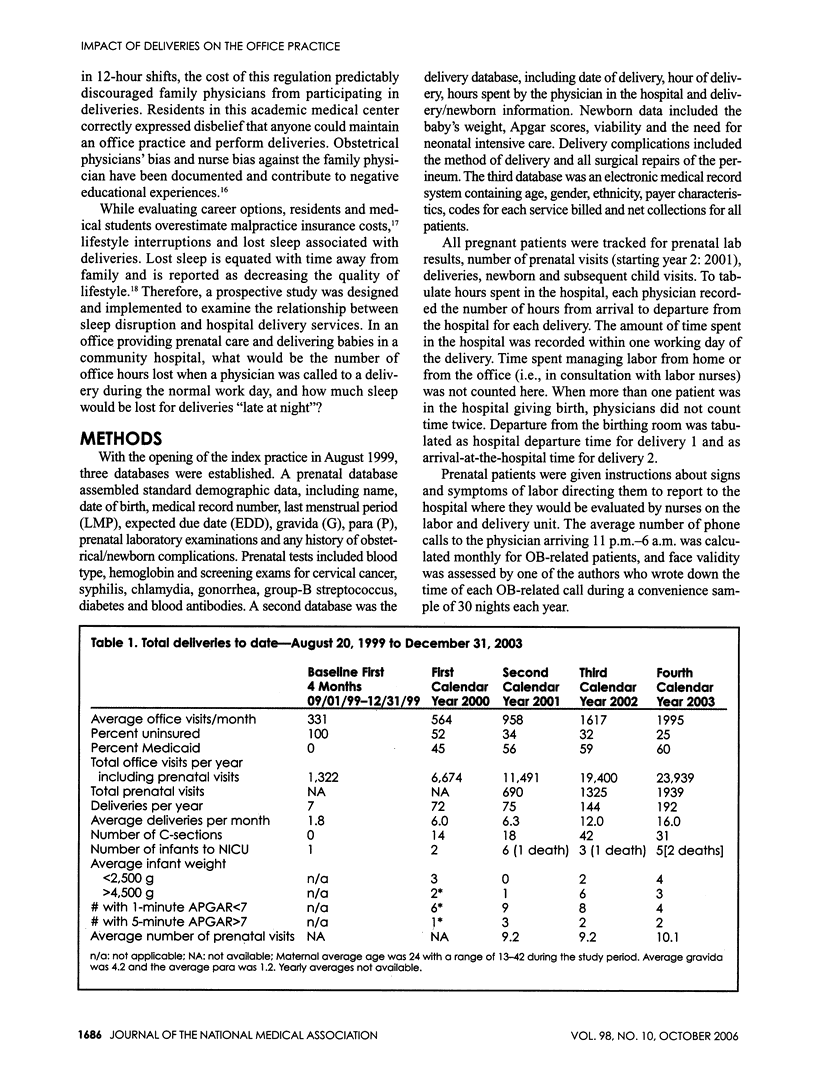
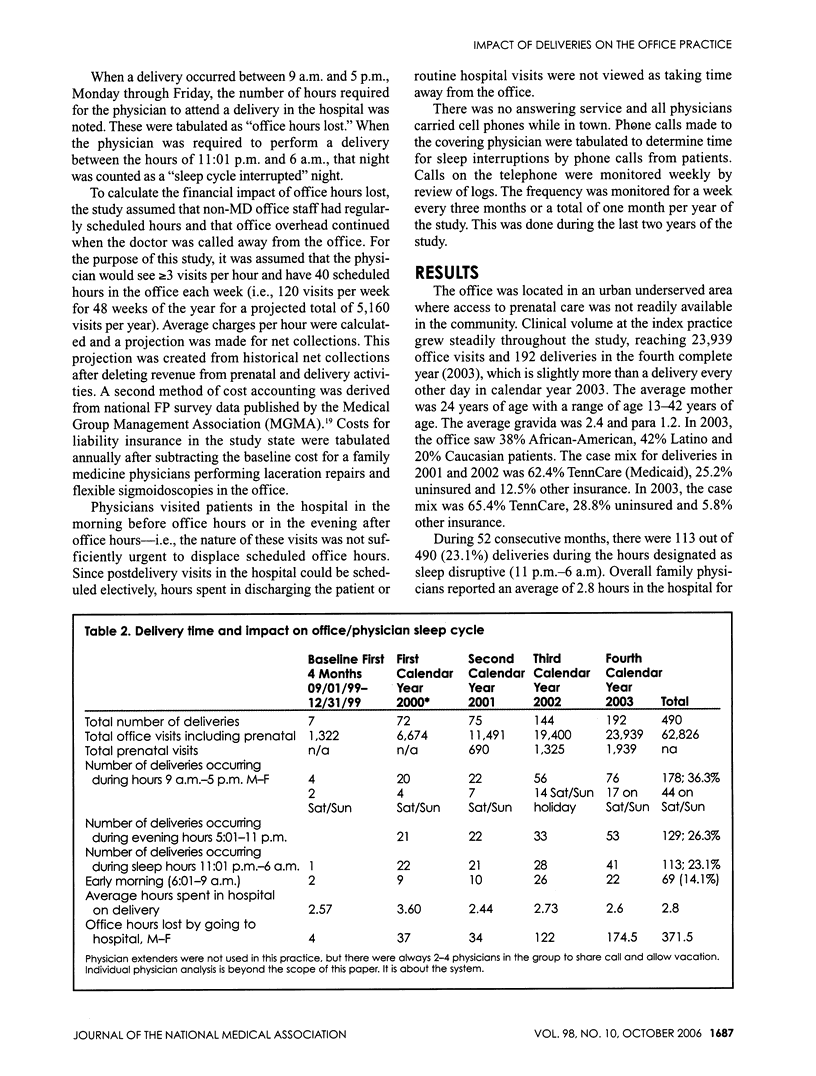
INTRODUCTION: To prospectively evaluate the frequency of late-night deliveries and the cost of lost office hours, physicians serving mainly uninsured and Medicaid patients in an urban area established databases tracking office demographics and detailed information on each delivery. SUBJECTS AND METHODS: Time needed in the hospital during routine office hours and late night was tabulated for each delivery. Complete calendar years 2000-2003 were tabulated separately and in total. Overhead and opportunity costs were calculated using historical norms and actual costs. RESULTS: During the study, there were 490 deliveries, with 113 (23%) occurring late at night. Physicians retrospectively self-reported an average of 2.8 hours in the hospital for the average delivery, which included 105 (21%) Cesarean deliveries. There were an average of 9.5 prenatal visits with each delivery, and 23% of deliveries occurred late at night (11 p.m.-6 a.m.). The average delivery produced a net revenue of dollar 1,339. Deliveries caused physicians to be absent from the office for 371.5 hours over the four years. After deducting opportunity cost and continuing overhead, net revenue for the 48-month study period was dollar 646,858. Ancillary revenues were beyond the scope of the study design. CONCLUSION: These data suggest that delivery services in this community of urban underserved minorities can be self-supporting. This is the first study in the medical literature to provide data describing the impact of deliveries on physician practices outside of residency. Loss of physician sleep and revenue lost secondary to time away from the office were successfully measured. These data suggest that common beliefs frequently overestimate lifestyle interruptions and underestimate the financial losses of failure to deliver babies in this region. Future studies are suggested.
Full text
PDF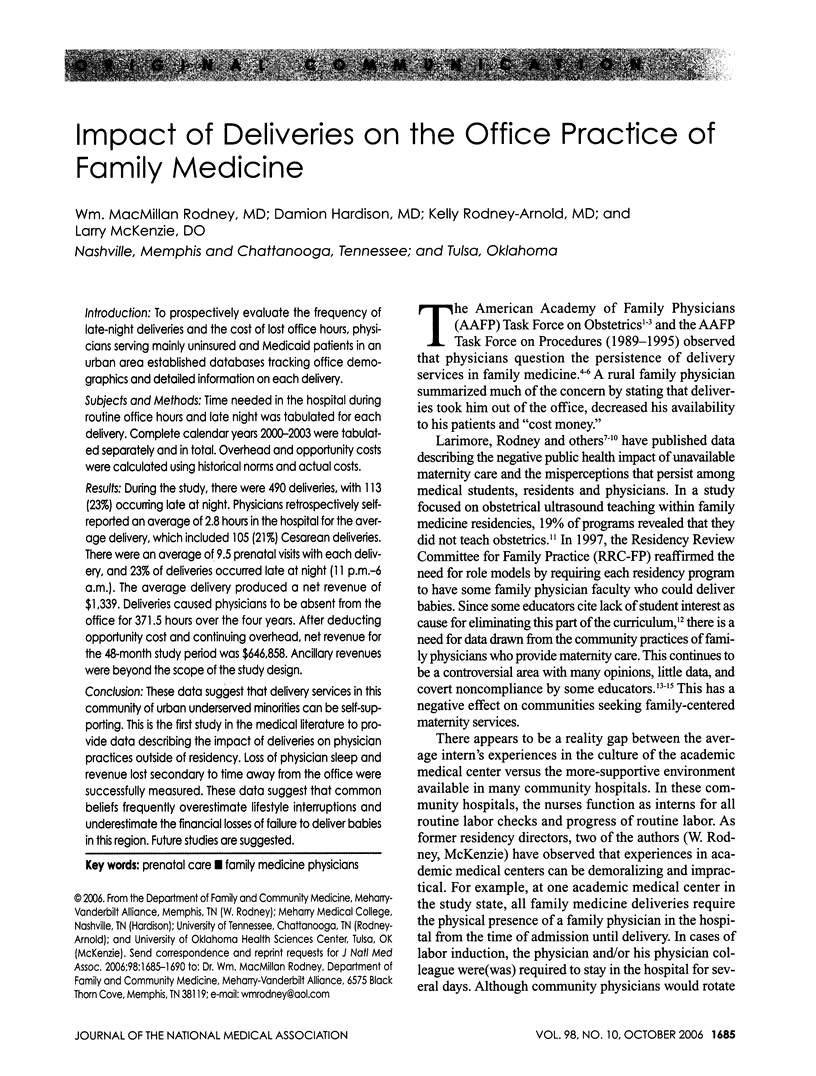


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Allen D. I., Kamradt J. M. Relationship of infant mortality to the availability of obstetrical care in Indiana. J Fam Pract. 1991 Dec;33(6):609–613. [PubMed] [Google Scholar]
- Connor P. D., Deutchman M. E., Hahn R. G. Training in obstetric sonography in family medicine residency programs: results of a nationwide survey and suggestions for a teaching strategy. J Am Board Fam Pract. 1994 Mar-Apr;7(2):124–129. [PubMed] [Google Scholar]
- Dresang Lee T., Rodney William MacMillan, Dees Jason. Teaching prenatal ultrasound to family medicine residents. Fam Med. 2004 Feb;36(2):98–107. [PubMed] [Google Scholar]
- Goldsmith Geoffrey A. Interest in family medicine: 1982 revisited? Fam Med. 2004 Jun;36(6):447–448. [PubMed] [Google Scholar]
- Halvorsen J. G. Who am I, professionally speaking? J Am Board Fam Pract. 1999 Mar-Apr;12(2):173–177. doi: 10.3122/jabfm.12.2.173. [DOI] [PubMed] [Google Scholar]
- Kruse J., Phillips D. M., Wesley R. A comparison of the attitudes of obstetricians and family physicians toward obstetric practice, training, and hospital privileges of family physicians. Fam Med. 1990 May-Jun;22(3):219–225. [PubMed] [Google Scholar]
- Larimore W. L., Sapolsky B. S. Maternity care in family medicine: economics and malpractice. J Fam Pract. 1995 Feb;40(2):153–160. [PubMed] [Google Scholar]
- Manahan Bill. Obstetrics in family practice. J Am Board Fam Pract. 2002 May-Jun;15(3):256–257. [PubMed] [Google Scholar]
- Nesbitt Thomas S. Obstetrics in family medicine: can it survive? J Am Board Fam Pract. 2002 Jan-Feb;15(1):77–79. [PubMed] [Google Scholar]
- Papp Klara K., Stoller Eleanor P., Sage Paulette, Aikens James E., Owens Judith, Avidan Alon, Phillips Barbara, Rosen Raymond, Strohl Kingman P. The effects of sleep loss and fatigue on resident-physicians: a multi-institutional, mixed-method study. Acad Med. 2004 May;79(5):394–406. doi: 10.1097/00001888-200405000-00007. [DOI] [PubMed] [Google Scholar]
- Pauwels Judith, Oliveira Andrew, Stevens Nancy. Benchmarking the costs of residency training in family practice. Fam Med. 2003 May;35(5):330–336. [PubMed] [Google Scholar]
- Phillips Robert L., Jr, Green Larry A. Making choices about the scope of family practice. J Am Board Fam Pract. 2002 May-Jun;15(3):250–254. [PubMed] [Google Scholar]
- Ratcliffe Stephen D., Newman Steven R., Stone Mary Bishop, Sakornbut Ellen, Wolkomir Michael, Thiese Steven M. Obstetric care in family practice residencies: a 5-year follow-up survey. J Am Board Fam Pract. 2002 Jan-Feb;15(1):20–24. [PubMed] [Google Scholar]
- Rodney W. M., Crown L. A., Hahn R., Martin J. Enhancing the family medicine curriculum in deliveries and emergency medicine as a way of developing a rural teaching site. Fam Med. 1998 Nov-Dec;30(10):712–719. [PubMed] [Google Scholar]
- Rodney W. M. Obstetric malpractice fee phobia among medical students in the United States. Fam Pract. 1986 Jun;3(2):113–116. doi: 10.1093/fampra/3.2.113. [DOI] [PubMed] [Google Scholar]
- Rodney Wm MacMillan, Hahn Ricardo G. Impact of the limited generalist (no hospital, no procedures) model on the viability of family practice training. J Am Board Fam Pract. 2002 May-Jun;15(3):191–200. [PubMed] [Google Scholar]
- Rosen Ilene M., Bellini Lisa M., Shea Judy A. Sleep behaviors and attitudes among internal medicine housestaff in a U.S. university-based residency program. Acad Med. 2004 May;79(5):407–416. doi: 10.1097/00001888-200405000-00009. [DOI] [PubMed] [Google Scholar]
- Saultz John W., David Alan K. Is it time for a 4-year family medicine residency? Fam Med. 2004 May;36(5):363–366. [PubMed] [Google Scholar]
- Schneeweiss R., Ellsbury K., Hart L. G., Geyman J. P. The economic impact and multiplier effect of a family practice clinic on an academic medical center. JAMA. 1989 Jul 21;262(3):370–375. [PubMed] [Google Scholar]
- Smith M. A., Howard K. P. Choosing to do obstetrics in practice: factors affecting the decisions of third-year family practice residents. Fam Med. 1987 May-Jun;19(3):191–194. [PubMed] [Google Scholar]
- Topping Daniel B., Hueston William J., MacGilvray Phyllis. Family physicians delivering babies: what do obstetricians think? Fam Med. 2003 Nov-Dec;35(10):737–741. [PubMed] [Google Scholar]


