Abstract
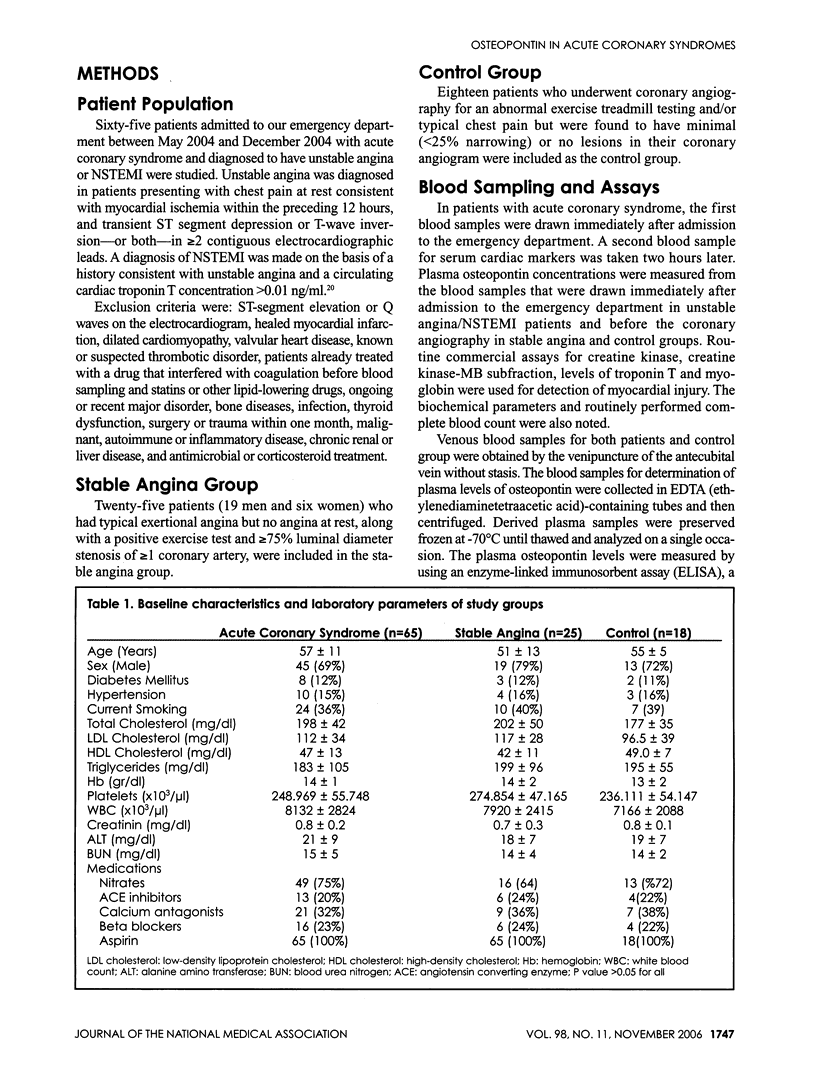
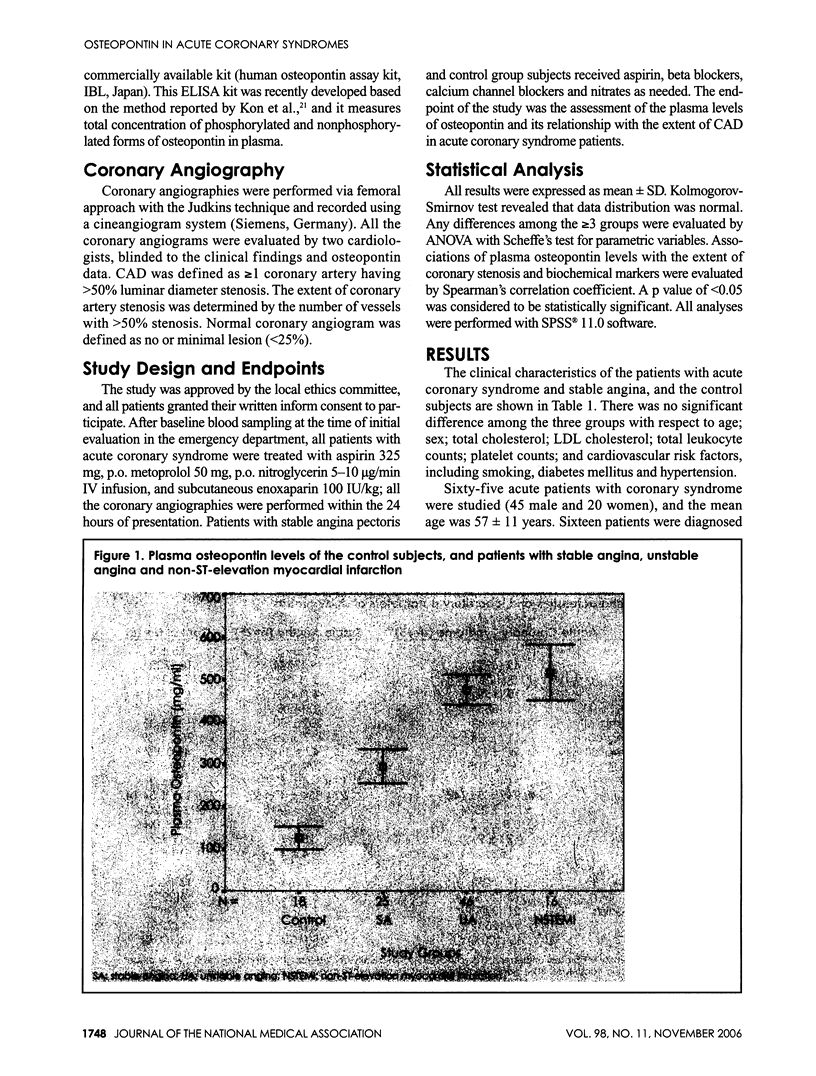
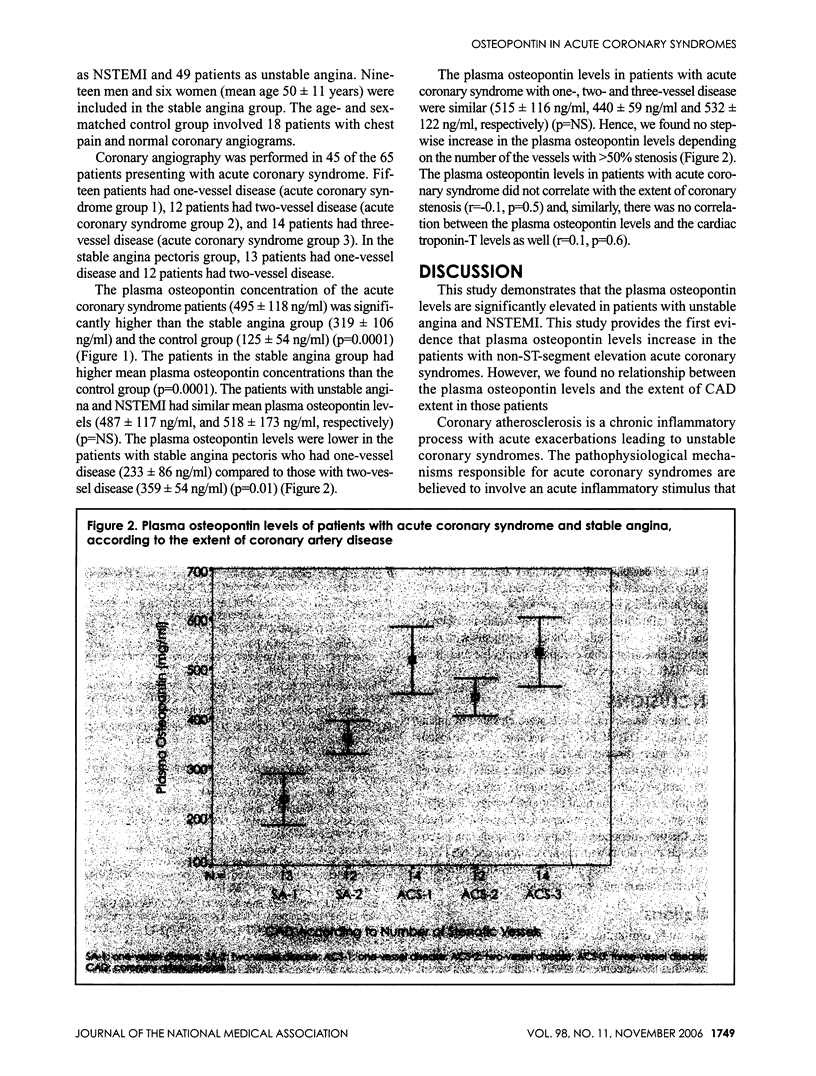
BACKGROUND: The regions of ruptured atherosclerotic plaques have numerous macrophages. Osteopontin that modulates macrophage function has been shown in atherosclerotic plaques. We aimed to study the plasma levels of osteopontin in patients with unstable angina or non-ST-seg ment elevation myocardial infarction (NSTEMI) and the rela tionship between osteopontin and the extent of the coronary artery disease (CAD). METHODS: We studied 65 patients with unstable angina or NSTEMI, 25 patients with stable angina and 18 patients as the control group. The extent of coronary artery stenosis was determined by the number of vessels with >50% stenosis. Plasma osteopontin concentrations were measured from the blood samples that were drawn immediately after admission to the emergency department in unstable angina/NSTEMI patients and before the coronary angiograph in the stable angina and control groups. RESULTS: The plasma osteopontin concentration was (495 118 ng/ml) significantly higher in the patients with unstable angina/NSTEMI compared to the stable angina group (319 106 ng/ml) and control group (125+/-54 ng/ml) (p=0.0001 The plasma osteopontin levels were lower in the patients with stable angina pectoris who had one-vessel disease compared to those with two-vessel disease (p=0.01). How ever, in the unstable angina/NSTEMI group, the plasma osteopontin levels were statistically not different among the patients with one-vessel, and two-vessel and three-vessel disease (p=NS). There was no correlation between the plasma osteopontin levels and the extent of coronary stenosis. CONCLUSIONS: The plasma osteopontin levels are elevatedin patients with unstable angina/NSTEMI, but there appears to be no correlation with the extent of CAD. These results ma suggest that osteopontin may have a role in the pathobiology of ACS.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Atalar E., Aytemir K., Haznedaroğlu I., Ozer N., Ovünç K., Aksöyek S., Kes S., Kirazli S., Ozmen F. Increased plasma levels of soluble selectins in patients with unstable angina. Int J Cardiol. 2001 Mar;78(1):69–73. doi: 10.1016/s0167-5273(00)00473-3. [DOI] [PubMed] [Google Scholar]
- Braunwald Eugene, Antman Elliott M., Beasley John W., Califf Robert M., Cheitlin Melvin D., Hochman Judith S., Jones Robert H., Kereiakes Dean, Kupersmith Joel, Levin Thomas N. ACC/AHA guideline update for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction--2002: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients With Unstable Angina). Circulation. 2002 Oct 1;106(14):1893–1900. doi: 10.1161/01.cir.0000037106.76139.53. [DOI] [PubMed] [Google Scholar]
- Buja L. M., Willerson J. T. Role of inflammation in coronary plaque disruption. Circulation. 1994 Jan;89(1):503–505. doi: 10.1161/01.cir.89.1.503. [DOI] [PubMed] [Google Scholar]
- Davies M. J. Stability and instability: two faces of coronary atherosclerosis. The Paul Dudley White Lecture 1995. Circulation. 1996 Oct 15;94(8):2013–2020. doi: 10.1161/01.cir.94.8.2013. [DOI] [PubMed] [Google Scholar]
- Dhore C. R., Cleutjens J. P., Lutgens E., Cleutjens K. B., Geusens P. P., Kitslaar P. J., Tordoir J. H., Spronk H. M., Vermeer C., Daemen M. J. Differential expression of bone matrix regulatory proteins in human atherosclerotic plaques. Arterioscler Thromb Vasc Biol. 2001 Dec;21(12):1998–2003. doi: 10.1161/hq1201.100229. [DOI] [PubMed] [Google Scholar]
- Falk E., Shah P. K., Fuster V. Coronary plaque disruption. Circulation. 1995 Aug 1;92(3):657–671. doi: 10.1161/01.cir.92.3.657. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick L. A., Severson A., Edwards W. D., Ingram R. T. Diffuse calcification in human coronary arteries. Association of osteopontin with atherosclerosis. J Clin Invest. 1994 Oct;94(4):1597–1604. doi: 10.1172/JCI117501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giachelli C. M., Steitz S. Osteopontin: a versatile regulator of inflammation and biomineralization. Matrix Biol. 2000 Dec;19(7):615–622. doi: 10.1016/s0945-053x(00)00108-6. [DOI] [PubMed] [Google Scholar]
- Koguchi Yoshinobu, Kawakami Kazuyoshi, Uezu Kaori, Fukushima Kiyoyasu, Kon Sigeyuki, Maeda Masahiro, Nakamoto Atsushi, Owan Isoko, Kuba Mutsuo, Kudeken Norifumi. High plasma osteopontin level and its relationship with interleukin-12-mediated type 1 T helper cell response in tuberculosis. Am J Respir Crit Care Med. 2003 Feb 5;167(10):1355–1359. doi: 10.1164/rccm.200209-1113OC. [DOI] [PubMed] [Google Scholar]
- Kon Shigeyuki, Yokosaki Yasuyuki, Maeda Masahiro, Segawa Tatsuya, Horikoshi Yuko, Tsukagoshi Hiroe, Rashid Mohammod M., Morimoto Junko, Inobe Manabu, Shijubo Noriharu. Mapping of functional epitopes of osteopontin by monoclonal antibodies raised against defined internal sequences. J Cell Biochem. 2002;84(2):420–432. doi: 10.1002/jcb.10039. [DOI] [PubMed] [Google Scholar]
- Lendon C. L., Davies M. J., Born G. V., Richardson P. D. Atherosclerotic plaque caps are locally weakened when macrophages density is increased. Atherosclerosis. 1991 Mar;87(1):87–90. doi: 10.1016/0021-9150(91)90235-u. [DOI] [PubMed] [Google Scholar]
- Moreno P. R., Falk E., Palacios I. F., Newell J. B., Fuster V., Fallon J. T. Macrophage infiltration in acute coronary syndromes. Implications for plaque rupture. Circulation. 1994 Aug;90(2):775–778. doi: 10.1161/01.cir.90.2.775. [DOI] [PubMed] [Google Scholar]
- Nasu K., Ishida T., Setoguchi M., Higuchi Y., Akizuki S., Yamamoto S. Expression of wild-type and mutated rabbit osteopontin in Escherichia coli, and their effects on adhesion and migration of P388D1 cells. Biochem J. 1995 Apr 1;307(Pt 1):257–265. doi: 10.1042/bj3070257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Brien E. R., Garvin M. R., Stewart D. K., Hinohara T., Simpson J. B., Schwartz S. M., Giachelli C. M. Osteopontin is synthesized by macrophage, smooth muscle, and endothelial cells in primary and restenotic human coronary atherosclerotic plaques. Arterioscler Thromb. 1994 Oct;14(10):1648–1656. doi: 10.1161/01.atv.14.10.1648. [DOI] [PubMed] [Google Scholar]
- Ohmori Reiko, Momiyama Yukihiko, Taniguchi Hiroaki, Takahashi Rie, Kusuhara Masatoshi, Nakamura Haruo, Ohsuzu Fumitaka. Plasma osteopontin levels are associated with the presence and extent of coronary artery disease. Atherosclerosis. 2003 Oct;170(2):333–337. doi: 10.1016/s0021-9150(03)00298-3. [DOI] [PubMed] [Google Scholar]
- Suezawa Chisato, Kusachi Shozo, Murakami Takashi, Toeda Kenichi, Hirohata Satoshi, Nakamura Keigo, Yamamoto Keizo, Koten Kazuya, Miyoshi Toru, Shiratori Yasushi. Time-dependent changes in plasma osteopontin levels in patients with anterior-wall acute myocardial infarction after successful reperfusion: correlation with left-ventricular volume and function. J Lab Clin Med. 2005 Jan;145(1):33–40. doi: 10.1016/j.lab.2004.08.007. [DOI] [PubMed] [Google Scholar]
- Takemoto M., Yokote K., Nishimura M., Shigematsu T., Hasegawa T., Kon S., Uede T., Matsumoto T., Saito Y., Mori S. Enhanced expression of osteopontin in human diabetic artery and analysis of its functional role in accelerated atherogenesis. Arterioscler Thromb Vasc Biol. 2000 Mar;20(3):624–628. doi: 10.1161/01.atv.20.3.624. [DOI] [PubMed] [Google Scholar]
- Tamura Akira, Shingai Maki, Aso Nobuko, Hazuku Takayuki, Nasu Masaru. Osteopontin is released from the heart into the coronary circulation in patients with a previous anterior wall myocardial infarction. Circ J. 2003 Sep;67(9):742–744. doi: 10.1253/circj.67.742. [DOI] [PubMed] [Google Scholar]
- Tyson Kerry L., Reynolds Joanne L., McNair Rosamund, Zhang Qiuping, Weissberg Peter L., Shanahan Catherine M. Osteo/chondrocytic transcription factors and their target genes exhibit distinct patterns of expression in human arterial calcification. Arterioscler Thromb Vasc Biol. 2003 Jan 30;23(3):489–494. doi: 10.1161/01.ATV.0000059406.92165.31. [DOI] [PubMed] [Google Scholar]
- van der Wal A. C., Becker A. E., van der Loos C. M., Das P. K. Site of intimal rupture or erosion of thrombosed coronary atherosclerotic plaques is characterized by an inflammatory process irrespective of the dominant plaque morphology. Circulation. 1994 Jan;89(1):36–44. doi: 10.1161/01.cir.89.1.36. [DOI] [PubMed] [Google Scholar]


