Abstract
A sensitive and specific assay for detection of food-borne pathogenic Yersinia pseudotuberculosis was developed. The primer-probe set was designed to target a 157-bp sequence of the chromosomally located gene ail. The complete method, including an internal amplification control, was evaluated for several different food items.
Although a number of Yersinia pseudotuberculosis outbreaks have been reported, the epidemiology of the infection is still unclear (6, 7, 13, 14). One problem is the low isolation rate obtained in naturally contaminated samples, which most probably is due to limited sensitivity of the culture-based methods. PCR methods, which have the advantage of increased sensitivity compared to culture-based methods, have previously been developed for detection of Yersinia pseudotuberculosis; however, most of them are based on conventional end-point PCR (8, 17, 18). TaqMan real-time PCR has overcome several of the limitations of conventional PCR, and we therefore developed such an assay for detection of Y. pseudotuberculosis in food. A real-time PCR method for detection of Y. pseudotuberculosis has previously been published. It is, in contrast to the assay described here, based on the nonspecific DNA binding dye SYBR Green instead of gene-specific TaqMan probes, and it was developed to analyze stool samples only (4).
The chromosomally located gene ail is frequently used as a PCR target for the detection of pathogenic Y. enterocolitica, and it is present also in Y. pseudotuberculosis (10). Whereas only a few of the Y. enterocolitica serotypes are pathogenic, the majority of Y. pseudotuberculosis strains are considered to be human and/or animal pathogens (3). Based on knowledge acquired from previous work at our laboratory using the ail gene as a PCR target for detection of pathogenic Y. enterocolitica serotypes (9, 15), the primer-probe set developed here for detection of Y. pseudotuberculosis was designed with the aim of enabling differentiation of the two species.
Assay development.
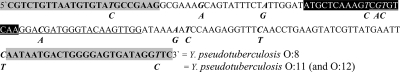
A sequence of the ail gene of a Y. pseudotuberculosis strain (CP000950.1) published in GenBank (www.ncbi.nlm.nih.gov) was used to design the primer-probe sets in this study. Primers were Yps 1 for CGTCTGTTAATGTGTATGCCGAAG (24-mer) and Yps 2 for GAACCTATCACTCCCCAGTCATTATT (26-mer). Probes used were (i) MGB probe NED-ATGCTCAAAGTCGTGTCAA-MGB and (ii) TAMRA probe VIC-CGTGTCAAGGACGATGGGTACAAGTTGG-TAMRA. Primers and probes were designed manually with the aid of Primer Express software (Applied Biosystems, Foster City, CA) and purchased at www.appliedbiosystems.com. Two alternative probes were selected in order to offer the user options, one using patented labeling and one with nonpatented labeling. The former was labeled at the 5′ end with the reporter dye NED, and the latter was labeled at the 3′ end with the chemical compound minor groove binder (MGB). The reason for labeling the probe with NED (and not VIC) was to be able to combine this primer-probe set with, for example, the commercially available TaqMan exogenous internal positive control (Applied Biosystems, Foster City, CA), which is VIC labeled. The selected target sequence, a 157-bp fragment of the ail gene, is shown in Fig. 1.
FIG. 1.
Polymorphism in the 157-bp primer/probe region among a strain, Y. pseudotuberculosis O:8, for which the region was amplified by using the real-time PCR developed in this study, and Y. pseudotuberculosis O:11 (and O:12), which was not amplified by using the real-time PCR. Highlights: gray background = primers, black background = MGB probe, underline = TAMRA probe, bold/italic = nucleotide variants in serotypes O:11 (and O:12) and other serotypes, respectively.
The real-time PCR assay.
The PCR mixture consisted of 1× TaqMan Universal PCR master mix (Applied Biosystems, Foster City, CA), 900 nM of the primers designated Yps 1 and Yps 2, 200 nM of the probe (6-carboxytetramethylrhodamine [TAMRA] or MGB labeled), approximately 100 copies of an internal amplification control (IAC; 1 fg of pUC19) (Fermentas, Germany), 500 nM of each of the IAC primers designated IPC_fw and IPC_re (MWG Biotech, Germany), and 200 nM of a Cy5-labeled IAC probe. Finally, the volume was adjusted with sterile Milli-Q water to 20 μl. Five microliters of the test sample (described below) or sterile water as a negative control was added to each reaction. Inclusion of an IAC and a negative control in each PCR run is strongly recommended in the field of PCR analysis (5; Anonymous, unpublished data [ISO/TC 34/SC 9 N752]). The IAC primers were developed by Fricker et al. (2), and the probe was a 27-mer oligonucleotide Cy5-TAAGGAGAAAATACCGCATCAGGCGCC-BBQ (www.tib-molbiol.com). The size of the IAC-PCR product was 119 bp. The PCR cycling was carried out in 96-well plates using the 7500 real-time PCR system (Applied Biosystems, Foster City, CA), and the following program was used: initial denaturation at 95°C for 10 min followed by 45 cycles of denaturation at 95°C for 15 s and primer annealing and extension at 60°C for 1 min.
Selectivity.
The selectivity of the primer-probe sets were tested on genomic DNA from 44 Y. pseudotuberculosis strains and 23 diverse, related strains (Table 1). The isolates were prepared as described previously (16). All strains were tested twice, once with the MGB-labeled probe and once with the TAMRA-labeled probe. All but two of the Y. pseudotuberculosis strains resulted in amplification; Y. pseudotuberculosis serotypes O:11 and O:12 produced negative PCR results. All non-Y. pseudotuberculosis strains did not produce amplification signals. Similar results (absence/presence) were obtained with both probes; however, values for the lower threshold cycle (CT; the cycle number at which the fluorescence passes the threshold) were constantly obtained with the TAMRA probe. Y. pseudotuberculosis serotypes O:11 and O:12 were further tested for the potential to carry a variant of the ail gene. A conventional PCR assay described previously was used (15, 16), and the obtained amplicons were purified and sequenced as described previously (16). The results revealed identical 157-bp fragments for the two serotypes. The sequence is shown in Fig. 1. For comparison, the 157-bp sequence amplified when analyzing Y. pseudotuberculosis O:8 (Table 1) using the real-time PCR was also added. When aligned against the ail sequences in GenBank, the O:11 (and O:12) sequence was found to be unique. Since these two serotypes are encountered (rarely) only in the Far East and are not recognized as pathogens to humans (3, 11), no further efforts were made to adjust the probes to also recognize these two serotypes. This is, to our knowledge, the first time a wide range of Y. pseudotuberculosis serotypes have been screened for the presence of the ail gene.
TABLE 1.
Bacterial strains used for evaluation of the selectivity of the real-time PCR assay using the primers Yps 1 and Yps 2 in combination with the NED/MGB probe or the VIC/TAMRA probea
| Species | Serotype or serovar | PCR results | Source | Country of origin | Strain(s) |
|---|---|---|---|---|---|
| Y. pseudotuberculosis | O:3 | + | Unknown | Belgium | IP 0071 |
| O:2A | + | Unknown | Belgium | IP 0069 | |
| NT | + | Human | Italy | 348/97 | |
| NT | + | Human | Sweden | CCUG 36765 | |
| NT | + | Human | Sweden | CCUG 24522 | |
| NT | + | Unknown | Belgium | IP 0068 | |
| NT | + | Unknown | Sweden | SLV-474 | |
| NT | + | Unknown | Unknown | 2209 DVLCC | |
| NT | + | Unknown | Unknown | 2210 DVLCC | |
| NT | + | Human | Sweden | Y 15/95 (SLV) | |
| NT | + | Human | Sweden | Y 21/03 (SLV) | |
| NT | + | Human | Sweden | Y 921/93 (SLV) | |
| NT | + | Human | Sweden | Y 42/00 (SLV) | |
| O:1 | + | Soil | Finland | TAVA 66 | |
| O:1 | + | Floor swab | Finland | TAVA 77 | |
| O:1 | + | Carrots | Finland | TAVA 80 | |
| O:1 | + | Soil | Finland | TAVA 81 | |
| O:1 | + | Carrot debris | Finland | TAVA 84 | |
| O:1 | + | Floor swab | Finland | TAVA 85 | |
| O2A | + | Unknown | Unknown | H 457/86 (FOI) | |
| O:4A | + | Unknown | Unknown | H 452/86 (FOI) | |
| O:5B | + | Unknown | Unknown | H 450/86 (FOI) | |
| O:6 | + | Unknown | Unknown | H 720/86 (FOI) | |
| O:7 | + | Unknown | Unknown | H 455/86 (FOI) | |
| O:8 | + | Unknown | Unknown | H 448/86 (FOI) | |
| O:9 | + | Unknown | Unknown | H 1112/90 (FOI) | |
| O:10 | + | Unknown | Unknown | H 16/92 (FOI) | |
| O:11 | ND | Unknown | Unknown | H 1093/90 (FOI) | |
| O:12 | ND | Unknown | Unknown | H 917/92 (FOI) | |
| O:13 | + | Unknown | Unknown | H 915/92 (FOI) | |
| O:14 | + | Unknown | Unknown | H 918/92 (FOI) | |
| O:15 | + | Unknown | Unknown | H 6516/94 (FOI) | |
| O:16 | + | Unknown | Unknown | H 1180/95 (FOI) | |
| O:3 | + | Human | Finland | IH 110310 | |
| O:1 | + | Human | Finland | IH 111203 | |
| O:3 | + | Human | Finland | IH 116128 | |
| O:1 | + | Human | Finland | IH 116178 | |
| O:1 | + | Human | Finland | IH 116583 | |
| O:3 | + | Human | Finland | IH 116689 | |
| O:3 | + | Human | Finland | IH 116807 | |
| O:3 | + | Human | Finland | IH 141295 | |
| O:1 | + | Human | Finland | IH 141292 | |
| O:1 | + | Human | Finland | IH 250004 | |
| O:1 | + | Human | Finland | IH 250326 | |
| Y. enterocolitica | 4/O:3 | ND | Pig | Denmark | 2102 (DVLCC) |
| O:9 | ND | Human | Denmark | 2065 (DVLCC) | |
| 4/O:3 | ND | Pork | Sweden | 3a (SLV) | |
| 4/O:3 | ND | Human | Sweden | Y-87M (SLV) | |
| 4/O:3 | ND | Human | England | 2100 (DVLCC) | |
| O:8 | ND | Human | United States | 8238 (SLV) | |
| O:5,27 | ND | Pig | Unknown | 2120 (DVLCC) | |
| O:15 | ND | Unknown | Unknown | 2173 (DVLCC) | |
| O:20 | ND | Unknown | Unknown | 2124 (DVLCC) | |
| Yersinia kristensenii | ND | Human | Denmark | 2126 (DVLCC) | |
| Yersinia frederiksenii | ND | Human | Sweden | 949021 (SLV) | |
| Salmonella enterica | Dublin | ND | Unknown | Unknown | SLV-242 |
| Enterobacter cloacae | ND | Unknown | Unknown | SLV-011; CCUG 43598 | |
| Escherichia coli | O157 | ND | Unknown | Unknown | SLV-479 |
| Citrobacter freundii | ND | Unknown | Unknown | SLV-091; CCUG 43597 | |
| Pseudomonas aeruginosa | ND | Unknown | Unknown | SLV-453; CCUG 551 | |
| ND | Water | Sweden | SLV-395 | ||
| Klebsiella pneumoniae | ND | Non-p. milk | Unknown | SLV-478; CCUG 43603 | |
| Listeria monocytogenes | ND | Non-p. milk | Sweden | SLV-513 | |
| Enterococcus durans | ND | Fresh meat | Unknown | SLV-078 | |
| Staphylococcus aureus | ND | Non-p. milk | Sweden | SLV-438 | |
| Staphylococcus xylosus | ND | Cheese | Unknown | SLV-283 | |
| Bacillus cereus | ND | Couscous | Unknown | SLV-518; CCUG 44741 |
CCUG, Culture Collection University of Gothenburg, Sweden; DVLCC, Danish Veterinary Laboratory Culture Collection; FOI, Swedish Defense Research Agency, Umeå, Sweden; IH, Enteric Bacteria Laboratory, National Public Health Institute (KTL), Finland; IP, Pasteur Institute, University of Louvain, Belgium; SLV, National Food Administration, Sweden; TAVA, Tavastlab, Finland; +, amplification; ND, not detected; Non-p. milk, nonpasteurized milk.
Standard curve and sensitivity.
A standard curve was obtained by analyzing a 10-fold serial dilution of purified genomic DNA from the Y. pseudotuberculosis strain TAVA 81. DNA was extracted and the concentration was measured as described previously (16). The purified, quantified DNA was diluted to achieve 106, 105, 104, 103, 102, 101, and 100 genomic equivalents and amplified using the reaction conditions and cycling parameters described above. Samples were analyzed in triplicate. The DNA concentration was converted to genomic equivalents based on the assumption that single copies of the target sequence were present in the genome. The standard curve slope was −3.444, and the reaction efficiency 95.3%. Positive amplification was achieved in all replicates when 10 or more target molecules were added to the PCR.
Detection in artificially contaminated food.
The PCR assay was evaluated using two food items, carrots (clean and unpeeled) and raw minced meat (beef). A culture of Y. pseudotuberculosis (TAVA 81) was grown in brain heart infusion medium overnight and thereafter serially diluted in peptone water. The total number of viable cells was determined as described previously (16). Food samples were purchased in local stores and stored chilled until the start of analysis, either the same day or the day after arrival. Ten-gram portions of the food were inoculated with Y. pseudotuberculosis at 104, 103, 102, 101, and 100 CFU, respectively. The inoculated food was mixed with 90 ml of tryptone soy broth supplemented with 0.6% yeast (TSBY) and homogenized for 1 min. The homogenates were enriched at 25°C for 18 to 20 h. DNA from 1 ml of each homogenate was extracted as described previously (16), and 5 μl of the genomic DNA was subjected to real-time PCR analysis using the reaction conditions and cycling parameters described above. The samples were analyzed in duplicate. The detection limit per 10 g of carrot and minced meat was 28 and 280 CFU, respectively (Table 2). No amplification was observed in any of the negative-control samples.
TABLE 2.
Sensitivity of detection of Y. pseudotuberculosis using real-time PCR following enrichment and DNA extraction initially inoculated into 10-g portions of two food items
| Y. pseudotuberculosis (CFU inoculated in 10 g of food) |
CT values using different food matricesa
|
|||
|---|---|---|---|---|
| Expt A
|
Expt B
|
|||
| Carrots | Minced beef meat | Carrots | Minced beef meat | |
| 2.8 × 103 | 40.34 ± 0.82 | 38.89 ± 0.25 | 36.32 ± 0.10 | 39.68 ± 1.88 |
| 2.8 × 102 | 40.44b | 44.06 ± 0.87 | 39.81b | 38.58 ± 0.66 |
| 2.8 × 101 | 42.06b | ND | ND | 40.12b |
| 2.8 | ND | ND | ND | ND |
| Negative controlc | ND | ND | ND | ND |
Expt A, only Y. pseudotuberculosis (TAVA 81); Expt B, Y. pseudotuberculosis cocultured with Y. enterocolitica. The CT values are the mean ± one standard deviation of two experiments. ND, not detected.
Only one positive result was obtained with two samples.
Negative-amplification control.
In addition, the real-time PCR method was used in three experiments with the following slightly different conditions. (i) Samples (25 g) of mixed salad inoculated with a serial dilution of Y. pseudotuberculosis were enriched in 225 ml of TSBY and incubated for 24 h. DNA from 1 ml of enrichment was thereafter extracted with the MasterPure complete DNA purification kit (Epicentre Biotechnology, Madison, WI) prior to PCR analysis. An ABI 7300 real-time PCR system and a TaqMan exogenous internal positive control (Applied Biosystems, Foster City, CA) were used. Finally, the TAMRA-labeled probe (however, labeled at the 5′ end with 6-carboxyfluorescein [FAM]) was used. In this experiment, the obtained detection limit instead was 0.9 CFU. (ii) The real-time PCR method was compared to a culture method described previously (14). In this experiment, 25-g samples of minced meat, nonpasteurized milk and mixed salad were tested (Table 3). The samples were inoculated with 13 to 17 CFU or 200 CFU of Y. pseudotuberculosis (TAVA 80) and simultaneously analyzed by the real-time PCR and the culture method. DNA extraction and PCR were performed as described above in item “i.” The relative sensitivity (1) of the culture method was only 60% compared to 100% for that of the real-time PCR method. The difference in obtained CT values between the two experiments presented in Table 2 and Table 3 when using minced meat as a food matrix is probably due to the use of different enrichment times, 18 to 20 h and 24 h, respectively. Thus, a longer enrichment time than 18 to 20 h seems to be advantageous. (iii) Twenty-five natural food samples, of which 9 were involved in outbreak investigations, were analyzed by using both the real-time PCR method and the culture method (samples were treated and DNA extraction and PCR were performed as described above in item “i”) (14) (Table 4). Whereas 6 of the analyzed food samples were positive for Y. pseudotuberculosis as indicated by PCR amplification, all 25 were negative when analyzed by the culture method.
TABLE 3.
Comparison of detection of Y. pseudotuberculosis (TAVA 80) initially inoculated into 25-g portions of three food items by using real-time PCR following enrichment and DNA extraction and by culture methoda
| Method | Inoculum | No. of samplesb | Minced beef meatc
|
Nonpasteurized milk
|
Grated carrots and iceberg lettuce (mixed)d
|
|||
|---|---|---|---|---|---|---|---|---|
| No. of positive samples | CT value | No. of positive samples | CT value | No. of positives | CT value | |||
| Real-time PCR | 200 CFU (high) | 30 | 10/10 | 29.48 ± 0.30 | 10/10 | 24.17 ± 0.67 | 10/10 | 29.01 ± 0.36 |
| 13-17 CFU (low) | 30 | 10/10 | 34.07 ± 0.24 | 10/10 | 29.81 ± 1.04 | 10/10 | 32.73 ± 0.34 | |
| None | 30 | ND | ND | ND | ||||
| Culture | 200 CFU (high) | 30 | 10/10 | 10/10 | 10/10 | |||
| 13-17 CFU (low) | 30 | 1/10 | 3/10 | 2/10 | ||||
| None | 30 | ND | ND | ND | ||||
DNA extraction was performed by using the MasterPure complete DNA purification kit (Epicentre Biotechnology, Madison, WI). The culture method was performed by using cold enrichment at 4°C in phosphate-buffered saline broth supplemented with 1% mannitol and 0.15% bile salts for 14 days (14). The CT values are the mean ± one standard deviation of five parallel samples and two parallel runs for each sample. ND, not detected.
Each sample type contained 10 samples, which were analyzed in parallel with the culture method.
Samples were filtrated by filter paper (7.5 μm) before DNA extraction.
Sample DNA was diluted 1:10 before the run.
TABLE 4.
Comparison of detection of Y. pseudotuberculosis in 25-g portions of natural food samples by using real-time PCR following enrichment and DNA extraction and by culture methoda
| Sample no. | Sample type | CT Ypd | CT IPCd | PCR | Culture |
|---|---|---|---|---|---|
| 1 | Grated carrotsb,c | 39.58 | + | − | |
| 2 | Grated carrotsb,c | 36.68 | + | − | |
| 3 | Grated carrots and Swedish turnip saladb,c | 38.85 | + | − | |
| 4 | Grated Chinese cabbage, carrots, and cabbage saladb,c | 32.81 | − | − | |
| 5 | Carrots in cubesb,c | 34.63 | − | − | |
| 6 | Carrotsb,c | 39.66 | − | − | |
| 7-15 | Iceberg lettuce | 31.45-33.70 | − | − | |
| 16 | Mixed iceberg lettuce and red lettuce | 31.49 | − | − | |
| 17 | Grated carrots | 31.85 | − | − | |
| 18 | Pumpkin | 33.42 | − | − | |
| 19 | Grated carrots | 34.32 | − | − | |
| 20 | Chinese cabbage | 33.35 | − | − | |
| 21 | Tomatoes in cubes | 33.15 | − | − | |
| 22 | Grated cabbage | 33.33 | − | − | |
| 23 | Grated carrots and onionsb | 39.03 | + | − | |
| 24 | Grated carrots and onionsb | 37.98 | + | − | |
| 25 | Carrotsb | 33.11 | + | − |
DNA extraction was performed by using the MasterPure complete DNA purification kit (Epicentre Biotechnologies, Madison, WI). The culture method was performed by using cold enrichment at 4°C in phosphate-buffered saline broth supplemented with 1% mannitol and 0.15% bile salts for 14 days (14). Extracted DNA was diluted prior to PCR run by 1/10 for samples 7-24 and 1/80 for samples 6 and 25.
Samples related to outbreak investigations.
Samples were cultured in 2006, after which point they were stored in the freezer and reanalyzed by PCR in 2008 (starting with enrichment in TSBY for 24 h).
IPC, internal positive control. CT values are mean of two replicates.
Multiplex PCR.
A culture of pathogenic Y. enterocolitica (SLV-408) was grown in parallel with the Y. pseudotuberculosis strain TAVA 81. In this experiment, the two microorganisms were inoculated together (and thus cocultured) in 10-g portions of the two food items, carrot and minced meat, to provide numbers of 104, 103, 102, 101, and 100 CFU of each. Samples were cultured and DNA was extracted as described above. The same PCR and cycling conditions as mentioned above in “The real-time PCR assay” were used with the exception that a volume of the Milli-Q water was replaced by a primer-probe set for detection of pathogenic Y. enterocolitica (16). Thus, Y. pseudotuberculosis was analyzed in a multiplex PCR. The detection limit for Y. pseudotuberculosis was 280 and 28 CFU per 10 g of carrot and minced meat, respectively. In contrast to the previous experiments, the detection limit here was lower for minced meat. The results are presented in Table 2. The IAC indicated no inhibition of amplification, and no amplification was observed in any of the negative-control samples.
In this brief report, we describe the development of a rapid, sensitive, and specific TaqMan-based real-time PCR method for screening food samples for the presence of Y. pseudotuberculosis. This method could also be used for simultaneous detection and differentiation of Y. pseudotuberculosis and pathogenic Y. enterocolitica using a multiplex PCR assay.
Acknowledgments
We gratefully thank Merja Sukki and other microbiology staff at TavastLab (Finland) and at the National Food Administration (Sweden) for their skillful technical assistance in the investigations. Also, we thank Mats Lindblad for reviewing the text and Sara Garbom for improving the English, both of whom work at the National Food Administration (Sweden).
Footnotes
Published ahead of print on 29 August 2008.
REFERENCES
- 1.Anonymous. 2007. NMKL procedure no. 20: evaluation of results from qualitative methods. National Veterinary Institute, Oslo, Norway.
- 2.Fricker, M., U. Messelhausser, U. Busch, S. Scherer, and M. Ehling-Schulz. 2007. Diagnostic real-time PCR assays for the detection of emetic Bacillus cereus strains in foods and recent food-borne outbreaks. Appl. Environ. Microbiol. 73:1892-1898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fukushima, H., Y. Matsuda, R. Seki, M. Tsubokura, N. Takeda, F. N. Shubin, I. K. Paik, and X. B. Zheng. 2001. Geographical heterogeneity between Far Eastern and Western countries in prevalence of the virulence plasmid, the superantigen Yersinia pseudotuberculosis-derived mitogen, and the high-pathogenicity island among Yersinia pseudotuberculosis strains. J. Clin. Microbiol. 39:3541-3547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fukushima, H., Y. Tsunomori, and R. Seki. 2003. Duplex real-time SYBR green PCR assays for detection of 17 species of food- or waterborne pathogens in stools. J. Clin. Microbiol. 41:5134-5146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hoorfar, J., and N. Cook. 2003. Critical aspects of standardization of PCR. Methods Mol. Biol. 216:51-64. [DOI] [PubMed] [Google Scholar]
- 6.Jalava, K., M. Hakkinen, M. Valkonen, U. M. Nakari, T. Palo, S. Hallanvuo, J. Ollgren, A. Siitonen, and J. P. Nuorti. 2006. An outbreak of gastrointestinal illness and erythema nodosum from grated carrots contaminated with Yersinia pseudotuberculosis. J. Infect. Dis. 194:1209-1216. [DOI] [PubMed] [Google Scholar]
- 7.Jalava, K., S. Hallanvuo, U. M. Nakari, P. Ruutu, E. Kela, T. Heinasmaki, A. Siitonen, and J. P. Nuorti. 2004. Multiple outbreaks of Yersinia pseudotuberculosis infections in Finland. J. Clin. Microbiol. 42:2789-2791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaneko, S., N. Ishizaki, and Y. Kokubo. 1995. Detection of pathogenic Yersinia enterocolitica and Yersinia pseudotuberculosis from pork using the polymerase chain reaction. Contrib. Microbiol. Immunol. 13:153-155. [PubMed] [Google Scholar]
- 9.Lambertz, S. T., K. Granath, M. Fredriksson-Ahomaa, K. E. Johansson, and M. L. Danielsson-Tham. 2007. Evaluation of a combined culture and PCR method (NMKL-163A) for detection of presumptive pathogenic Yersinia enterocolitica in pork products. J. Food Prot. 70:335-340. [DOI] [PubMed] [Google Scholar]
- 10.Miller, V. L., J. J. Farmer III, W. E. Hill, and S. Falkow. 1989. The ail locus is found uniquely in Yersinia enterocolitica serotypes commonly associated with disease. Infect. Immun. 57:121-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nagano, T., T. Kiyohara, K. Suzuki, M. Tsubokura, and K. Otsuki. 1997. Identification of pathogenic strains within serogroups of Yersinia pseudotuberculosis and the presence of non-pathogenic strains isolated from animals and the environment. J. Vet. Med. Sci. 59:153-158. [DOI] [PubMed] [Google Scholar]
- 12.Reference deleted.
- 13.Nuorti, J. P., T. Niskanen, S. Hallanvuo, J. Mikkola, E. Kela, M. Hatakka, M. Fredriksson-Ahomaa, O. Lyytikainen, A. Siitonen, H. Korkeala, and P. Ruutu. 2004. A widespread outbreak of Yersinia pseudotuberculosis O:3 infection from iceberg lettuce. J. Infect. Dis. 189:766-774. [DOI] [PubMed] [Google Scholar]
- 14.Rimhanen-Finne, R., T. Niskanen, S. Hallanvuo, P. Makary, K. Haukka, S. Pajunen, A. Siitonen, R. Ristolainen, H. Poyry, J. Ollgren, and M. Kuusi. 2008. Yersinia pseudotuberculosis causing a large outbreak associated with carrots in Finland, 2006. Epidemiol. Infect. 4:1-6. [DOI] [PubMed] [Google Scholar]
- 15.Thisted Lambertz, S., and M. L. Danielsson-Tham. 2005. Identification and characterization of pathogenic Yersinia enterocolitica isolates by PCR and pulsed-field gel electrophoresis. Appl. Environ. Microbiol. 71:3674-3681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thisted Lambertz, S., C. Nilsson, S. Hallanvuo, and M. Lindblad. 2008. Real-time PCR method for detection of pathogenic Yersinia enterocolitica in food. Appl. Environ. Microbiol. 74:6060-6067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thoerner, P., C. I. Bin Kingombe, K. Bogli-Stuber, B. Bissig-Choisat, T. M. Wassenaar, J. Frey, and T. Jemmi. 2003. PCR detection of virulence genes in Yersinia enterocolitica and Yersinia pseudotuberculosis and investigation of virulence gene distribution. Appl. Environ. Microbiol. 69:1810-1816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Trebesius, K., D. Harmsen, A. Rakin, J. Schmelz, and J. Heesemann. 1998. Development of rRNA-targeted PCR and in situ hybridization with fluorescently labeled oligonucleotides for detection of Yersinia spp. J. Clin. Microbiol. 36:2557-2564. [DOI] [PMC free article] [PubMed] [Google Scholar]