Abstract
OBJECTIVE—A lower in vivo mitochondrial function has been reported in both type 2 diabetic patients and first-degree relatives of type 2 diabetic patients. The nature of this reduction is unknown. Here, we tested the hypothesis that a lower intrinsic mitochondrial respiratory capacity may underlie lower in vivo mitochondrial function observed in diabetic patients.
RESEARCH DESIGN AND METHODS—Ten overweight diabetic patients, 12 first-degree relatives, and 16 control subjects, all men, matched for age and BMI, participated in this study. Insulin sensitivity was measured with a hyperinsulinemic-euglycemic clamp. Ex vivo intrinsic mitochondrial respiratory capacity was determined in permeabilized skinned muscle fibers using high-resolution respirometry and normalized for mitochondrial content. In vivo mitochondrial function was determined by measuring phosphocreatine recovery half-time after exercise using 31P-magnetic resonance spectroscopy.
RESULTS—Insulin-stimulated glucose disposal was lower in diabetic patients compared with control subjects (11.2 ± 2.8 vs. 28.9 ± 3.7 μmol · kg−1 fat-free mass · min−1, respectively; P = 0.003), with intermediate values for first-degree relatives (22.1 ± 3.4 μmol · kg−1 fat-free mass · min−1). In vivo mitochondrial function was 25% lower in diabetic patients (P = 0.034) and 23% lower in first-degree relatives, but the latter did not reach statistical significance (P = 0.08). Interestingly, ADP-stimulated basal respiration was 35% lower in diabetic patients (P = 0.031), and fluoro-carbonyl cyanide phenylhydrazone–driven maximal mitochondrial respiratory capacity was 31% lower in diabetic patients (P = 0.05) compared with control subjects with intermediate values for first-degree relatives.
CONCLUSIONS—A reduced basal ADP-stimulated and maximal mitochondrial respiratory capacity underlies the reduction in in vivo mitochondrial function, independent of mitochondrial content. A reduced capacity at both the level of the electron transport chain and phosphorylation system underlies this impaired mitochondrial capacity.
Skeletal muscle insulin resistance is one of the earliest hallmarks in the development of type 2 diabetes. In recent years, mitochondrial dysfunction has been suggested to underlie the development of insulin resistance and type 2 diabetes (1–5). An impaired mitochondrial function may contribute to increased lipid accumulation in skeletal muscle (intramyocellular lipid [IMCL] content) but also in heart and liver. Lipid intermediates are thought to interfere with the insulin signaling pathway (2). Petersen et al. (3) were the first to report that mitochondrial dysfunction may be a factor in the etiology of insulin resistance. Using noninvasive phosphorus magnetic resonance spectroscopy (31P-MRS), they applied a magnetization saturation transfer method to calculate unidirectional ATP synthesis rate. Using this methodology, they reported that resting muscular ATP synthesis was decreased by ∼40% in insulin-resistant elderly compared with insulin-sensitive young control subjects (3). Similar results were obtained when lean but insulin-resistant offspring of type 2 diabetic patients were compared with insulin-sensitive healthy subjects matched for age, BMI, and habitual physical activity (6). The offspring of type 2 diabetic patients were characterized by an ∼60% lower rate of muscular glucose uptake and 30% lower rates of resting muscular ATP synthesis rate. A decreased mitochondrial function in diabetes-prone subjects like first-degree relatives of type 2 diabetic patients suggests that mitochondrial defects may underlie the pathogenesis of diabetes. Recently, the observations of compromised mitochondrial function in diabetes-prone subjects reflected as reduced ATP synthesis has been extended to nonobese, metabolically well-controlled type 2 diabetic patients (7). However, when this population of type 2 diabetic patients was matched to age-matched control subjects, no differences in ATP synthesis rate were found. In contrast, using an alternative method to measure in vivo mitochondrial function with 31P-MRS, we recently showed an ∼40% lower mitochondrial function in type 2 diabetic patients compared with age- and BMI-matched control subjects (8). With this method, phosphocreatine (PCr) kinetics are evaluated during recovery from submaximal exercise (9,10). During exercise, PCr content decreases to reach a steady state and recovers rapidly after exercise. This PCr resynthesis is driven almost purely oxidatively (11). Therefore, the rate of PCr resynthesis (e.g., the half-time of recovery) reflects in vivo mitochondrial oxidative capacity or function (12). A prolonged PCr resynthesis rate, as found in type 2 diabetic patients (8), therefore indicates decreased mitochondrial function. Both 31P-MRS methods give important information on mitochondrial function, but it should be noted that the two methods should be interpreted differently: the PCr recovery method determines the maximal capacity of the oxidative system, whereas the ATP-saturation transfer method measures the momentary flux of ATP synthesis in the resting state. Taken together, studies examining in vivo mitochondrial function using 31P-MRS point toward diminished mitochondrial function related to type 2 diabetes, although results may vary depending on age and BMI of the control groups.
Why in vivo mitochondrial function is reduced cannot be deduced from 31P-MRS. In fact, a lower in vivo mitochondrial “function” can be the result of several factors, including a reduced mitochondrial density, lower muscle perfusion, but also a true mitochondrial dysfunction (i.e., lower mitochondrial respiratory capacity per mitochondrion). To examine the causes of lower in vivo mitochondrial function, ex vivo determination of mitochondrial function is of particular interest because it allows studying intrinsic mitochondrial capacity under a variety of substrates. So far, three studies have reported mitochondrial function ex vivo in a diabetic population (13–15), with conflicting results. These studies did not determine in vivo mitochondrial function and can therefore not answer the question whether a reduced in vivo mitochondrial function, as has repeatedly been observed in type 2 diabetic patients, can be attributed to a reduced intrinsic mitochondrial respiratory capacity.
Therefore, the aim of the present study was to identify the underlying defects of impaired in vivo mitochondrial function in a comparable diabetic population as in which we previously showed reduced in vivo mitochondrial function. To this end, detailed ex vivo mitochondrial respirometry was combined within the same subject with in vivo mitochondrial function in patients with type 2 diabetes, and results were compared with first-degree relatives and with age- and BMI-matched control subjects.
RESEARCH DESIGN AND METHODS
Ten male type 2 diabetic patients (diabetic patients), 12 male first-degree relatives, and 16 male control subjects (Table 1) were included in this study, which was approved by the institutional medical ethical committee. Subjects were recruited via advertisement in local papers and gave their written informed consent. Before the onset of the study, a medical history and physical examination was performed, and a resting electrocardiogram was taken. Subjects with uncontrolled hypertension, active cardiovascular disease, or liver dysfunction or subjects on medication known to interfere with glucose metabolism (except for diabetic patients) were excluded from participation. Control subjects and first-degree relatives underwent a 2-h oral glucose tolerance test according to World Health Organization criteria. Diabetic patients were diagnosed with type 2 diabetes at least 2 years before the start of the study and had well-controlled diabetes (A1C 7.1 ± 0.2). All diabetic patients were on metformin, and three patients were on sulfonylurea in combination with metformin. Furthermore, none of the diabetic patients followed a prescribed dietary program. Control subjects had no family history of type 2 diabetes; whereas five first-degree relatives had one first-line family member (father, mother, brother, or sister) diagnosed with type 2 diabetes, and seven were multiple relatives. All first-degree relatives were not related to the diabetic patients included in this study. All subjects performed a maximal aerobic capacity test as described previously (16). Body composition was determined using hydrostatic weighing (17).
TABLE 1.
Subject characteristics
| Control subjects | First-degree relatives | Diabetic patients | |
|---|---|---|---|
| Age (years) | 59.2 ± 0.7 | 60.1 ± 0.9 | 61.4 ± 1.6 |
| Body weight (kg) | 92.3 ± 2.6 | 91.6 ± 3.8 | 89.2 ± 3.3 |
| BMI (kg/m2) | 29.1 ± 0.7 | 30.1 ± 1.2 | 28.9 ± 0.7 |
| Fat (%) | 31.4 ± 1.7 | 29.4 ± 1.9 | 27.9 ± 2.3 |
| Fat-free mass (kg) | 62.8 ± 1.9 | 62.5 ± 3.2 | 63.7 ± 2.0 |
| Vo2max (ml · kg−1 · min−1) | 31.2 ± 1.6 | 32.6 ± 9.6 | 28.2 ± 2.3 |
| Glucose (mmol/l) | 6.0 ± 0.2 | 6.0 ± 0.2 | 8.6 ± 0.6*† |
| Insulin (mU/l) | 13.7 ± 2.1 | 14.5 ± 1.8 | 17.5 ± 2.1 |
| NEFA (μmol/l) | 464 ± 22 | 432 ± 41 | 526 ± 49 |
Data are means ± SE.
P < 0.05 diabetic patients vs. control subjects;
P < 0.05 diabetic patients vs. first-degree relatives.
To measure peripheral insulin sensitivity, a 3-h hyperinsulinemic-euglycemic (40 mU · m−2 · min−1) clamp, according to DeFronzo (18), was performed after an overnight fast with primed infusion of [6,6-2H2]glucose (0.04 mg · kg−1 · min−1) to determine rates of glucose appearance (Ra) and disposal (Rd), as previously described (19). One week before the hyperinsulinemic-euglycemic clamp, patients were withdrawn from their antidiabetic medication. Basal and insulin-stimulated measurements were performed, including blood sampling and indirect calorimetry. Type 2 diabetic patients were clamped at higher glucose values than first-degree relatives and control subjects (6.2 ± 0.2, 5.7 ± 0.1, and 5.7 ± 0.1, respectively, P < 0.05) because of their hyperglycemia at the onset of the clamping procedure. Muscle biopsies were taken before the clamp, under local anesthesia (2% lidocaïne), according to the technique of Bergström et al. (20).
On a separate day, at least 1 week before the clamp or after the clamp, subjects performed a knee-extension exercise protocol on a home-built magnetic resonance compatible ergometer with a pulley system in a 1.5-T whole-body scanner (Intera; Philips Medical Systems, Best, the Netherlands), and PCr kinetics were analyzed after exercise, as described previously (8). Exercise was performed for 5 min with a weight corresponding to 60% of maximal capacity, which was determined with an incremental maximal test with the same ergometer on a different day. Low- to medium-intensity exercise was chosen to prevent acidification, which is known to affect PCr recovery. Subjects consumed an early lunch 2 h before the PCr kinetics test. On the same day, 1H-MRS imaging was performed in the m. vastus lateralis to analyze IMCL content, as described in detail previously (8). IMCL content is reported as the percentage of the signal intensity of the CH2 peak of IMCL, compared with the intensity of the water resonance. One diabetic patient, two first-degree relatives, and four control subjects were excluded for in vivo 31P-MRS and 1H-MRS imaging for medical reasons, including metal orthopedic implants, severe claustrophobia, or technical problems.
Isolation and permeabilization of muscle fibers.
A small portion (∼30 mg) was immediately placed in ice-cold biopsy containing preservation medium (BIOPS; OROBOROS Instruments, Innsbruck, Austria). Muscle fibers were permeabilized with saponin according to the technique of Veksler et al. (21). After completion of the permeabilization protocol, muscle fibers were transferred into ice-cold mitochondrial respiration buffer (MiRO5; OROBOROS Instruments). Subsequently, the muscle fibers were transferred to the oxygraph to perform high-resolution respirometry corrected for wet weight.
High-resolution respirometry.
Mitochondrial function ex vivo was quantified by measuring oxygen consumption polarographically using a two-chamber Oxygraph (OROBOROS Instruments). Oxygen consumption reflects the first derivative of the oxygen concentration (nmol/ml) in time in the respiration chambers and is termed oxygen flux [pmol/(s*mg)], corrected for wet weight muscle tissue (2–5 mg) introduced into the chamber. To evaluate oxidative phosphorylation, different substrate inhibition protocols were used. In every protocol applied, first, 4.0 mmol/l malate was added to obtain state 2 respiration followed by addition of 8.0 mmol/l glutamate as a substrate for complex I with or without 40.0 μmol/l palmitoyl-carnitine. In addition, an excess of 1.6 mmol/l ADP was added to evaluate state 3 respiration of complex I. Then 8.0 mmol/l succinate was added to obtain state 3 respiration by activating both complex I and II. Finally, 1.6 μg/ml oligomycin or titrations of the uncoupler 1.0 mmol/l fluoro-carbonyl cyanide phenylhydrazone (FCCP) were added to evaluate state 4 respiration or maximal respiratory capacity, state u, respectively.
Measures of mitochondrial density.
For citrate synthase activity, 10 mg m. vastus lateralis muscle biopsy was cut with a cryostat (−20°C), dissolved in 100 μl cold SET buffer (containing 250 mmol/l sucrose, 2 mmol/l EDTA, and 10 mmol/l Tris-HCl, adjusted pH at 7.4), and processed for spectrophotometric analysis of citrate synthase activity according to Shephard and Garland (22).
Mitochondrial DNA (mtDNA) copy number was determined as a marker for mitochondrial density using quantitative real-time PCR, based on the TaqMan probe method. TaqMan primers and probes are shown in Table 2. mtDNA copy number was calculated from the ratio of NADH dehydrogenase subunit 1 (ND1) to lipoprotein lipase (LPL) (mtDNA/nuclear DNA), as described previously (23).
TABLE 2.
Primers/probes used in quantitative RT-PCR for quantification of mtDNA copy number
| Gene | Forward primer | Probe | Reverse primer |
|---|---|---|---|
| ND1 | CCC TAA AAC CCG CCA CAT CT | CCA TCA CCC TCT ACA TCA CCG CCC | GAG CGA TGG TGA GAG CTA AGG T |
| LPL | CGA GTC GTC TTT CTC CTG ATG AT | ACA TTC ACC AGA GGG TC | TTC TGG ATT CCA ATG CTT CGA |
Plasma assays.
Blood collected in tubes containing EDTA was immediately centrifuged at high speed, and plasma was frozen in liquid nitrogen and stored at −80°C until assayed. Plasma nonesterified fatty acids (NEFAs) and glucose were measured with enzymatic assays automated on a Cobas Fara/Mira (NEFA: Wako Nefa C test kit; Wako Chemicals, Neuss, Germany) (glucose: hexokinase method; LaRoche, Basel, Switzerland). Insulin concentration was determined using a radioimmunoassay (Linco Reseach, St. Charles, MO). Isotopic enrichment of plasma glucose was determined by electron ionization gas chromatography–mass spectrometry and expressed as tracer-to-tracee ratio.
Calculations.
Steele's single-pool non–steady-state equations were used to calculate glucose Ra and Rd (24). Volume of distribution was assumed to be 0.160 l/kg for glucose. Endogenous glucose production (EGP) was calculated as Ra minus exogenous glucose infusion rate. Both in the basal state and during insulin stimulation, substrate oxidation was measured by indirect calorimetry. Fat and carbohydrate oxidation were calculated using stoichiometric equations according to Frayn (25) with the assumption that protein oxidation was negligible. Nonoxidative glucose disposal was calculated as Rd minus carbohydrate oxidation. Metabolic flexibility was expressed as the change in respiratory quotient from the fasted state to the insulin-stimulated condition.
Statistics.
Data are reported as means ± SE. Statistical analyses were performed using the statistical computer program SPSS 11.0.4 for Mac OS X. Differences between groups were analyzed by one-way ANOVA with a Tukey's honestly significant difference post hoc correction. We computed Spearman correlation coefficients to correlate parameter values. Differences were considered significant when P < 0.05.
RESULTS
Subjects.
All groups were carefully matched for age and BMI (age 61.4 ± 1.6, 60.1 ± 0.9, and 59.2 ± 0.7 years; BMI 28.9 ± 0.7, 30.1 ± 1.2, and 29.1 ± 0.7 kg/m2, respectively, for diabetic patients, first-degree relatives, and control subjects) (Table 1). Maximal aerobic capacity (Vo2max) was not different between groups (Vo2max 28.2 ± 2.3, 32.6 ± 9.6, and 31.2 ± 1.6 ml · kg−1 · min−1, respectively, in diabetic patients, first-degree relatives, and control subjects) (Table 1). By definition, fasting plasma glucose concentration was significantly higher in diabetic patients compared with first-degree relatives and control subjects (Table 1). Fasting plasma insulin and NEFA concentrations were not different between groups (Table 1).
Insulin-mediated glucose uptake.
Basal glucose uptake (Rd) was significantly higher in diabetic patients compared with control subjects (Table 3; P = 0.024). Insulin-stimulated glucose disposal, expressed as Rd during insulin infusion minus basal Rd, was significantly decreased in diabetic patients compared with control subjects (Table 3; P = 0.003). First-degree relatives had intermediate values for basal Rd and insulin-stimulated glucose disposal; however, these values were not different from control subjects or diabetic patients. A reduced insulin-stimulated glucose oxidation (P = 0.05) and nonoxidative glucose uptake (P = 0.03) accounted for the lower insulin-stimulated glucose disposal in diabetic patients (Table 3). Also, for these parameters, values reported for first-degree relatives were in between control subjects and diabetic patients. Basal EGP, reflecting hepatic glucose output, was higher in diabetic patients compared with control subjects (Table 3; P = 0.028), with intermediate values for first-degree relatives. EGP was almost completely suppressed during insulin infusion in all groups (Table 3). Diabetic patients had significantly lower insulin-suppressed lipid oxidation values compared with control subjects (Table 3; P = 0.028).
TABLE 3.
Substrate kinetics
| Control subjects | First-degree relatives | Diabetic patients | |
|---|---|---|---|
| Rd glucose (μmol · kg−1 fat-free mass · min−1) | |||
| Basal | 12.1 ± 1.0 | 14.2 ± 1.8 | 17.3 ± 1.3* |
| Clamp | 41.0 ± 3.7 | 36.2 ± 3.5 | 28.4 ± 2.7* |
| Change (Rd clamp–Rd basal) | 28.9 ± 3.7 | 22.1 ± 3.4 | 11.2 ± 2.8* |
| EGP (μmol · kg−1 fat-free mass · min−1) | |||
| Basal | 11.9 ± 1.0 | 11.7 ± 1.4 | 16.3 ± 1.1* |
| Clamp | 2.0 ± 1.2 | 2.4 ± 1.2 | 4.1 ± 1.5 |
| Change (EGP basal–EGP clamp) | 9.8 ± 1.5 | 9.3 ± 0.9 | 12.2 ± 1.5 |
| Carbohydrate oxidation (μmol · kg−1 fat-free mass · min−1) | |||
| Basal | 8.9 ± 0.5 | 11.6 ± 1.9 | 10.6 ± 0.9 |
| Clamp | 20.6 ± 2.3 | 19.6 ± 1.3 | 15.3 ± 0.6 |
| Change (CHO ox clamp–CHO ox basal) | 11.7 ± 2.5 | 8.1 ± 1.5 | 4.6 ± 0.8* |
| NOGD (μmol · kg−1 fat-free mass · min−1) | |||
| Basal | 2.9 ± 1.3 | 2.7 ± 2.2 | 6.6 ± 1.6 |
| Clamp | 22.6 ± 3.3 | 16.4 ± 3.3 | 13.2 ± 2.9 |
| Change (NOGD clamp–NOGD basal) | 19.7 ± 3.7 | 13.7 ± 3.7 | 6.5 ± 2.6* |
| Lipid oxidation (μmol · kg−1 fat-free mass · min−1) | |||
| Basal | 5.1 ± 0.3 | 4.8 ± 0.4 | 4.9 ± 0.2 |
| Clamp | 3.0 ± 0.3 | 2.8 ± 0.4 | 3.8 ± 0.2 |
| Change (lipid ox basal–lipid ox clamp) | 2.3 ± 0.3 | 2.0 ± 0.3 | 1.1 ± 0.2* |
Data are means ± SE. NOGD, nonoxidative glucose disposal.
P < 0.05 between diabetic patients and control subjects. CHOox, carbohydrate oxidation.
Metabolic flexibility.
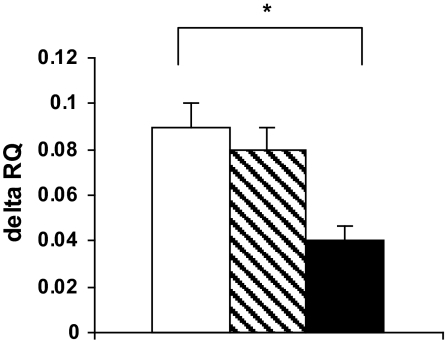
Metabolic flexibility, i.e., the increase in respiratory quotient (ΔRQ) from basal to insulin stimulation, was significantly lower in diabetic patients compared with control subjects (0.04 ± 0.01 vs. 0.09 ± 0.01, respectively; P = 0.014). First-degree relatives did not significantly differ from control subjects or diabetic patients (Fig. 1).
FIG. 1.
Metabolic flexibility, measured as the change in respiratory quotient from the fasted state to the insulin-stimulated condition, in control subjects, first-degree relatives, and diabetic patients. □, control; , FDR; ▪, type 2 diabetic patients. *P < 0.05 compared with diabetic patients.
, FDR; ▪, type 2 diabetic patients. *P < 0.05 compared with diabetic patients.
Intramyocellular lipid content.
No differences were found for IMCL content between groups (1.0 ± 0.2, 0.9 ± 0.1, and 0.8 ± 0.1%, respectively, for diabetic patients, first-degree relatives, and control subjects).
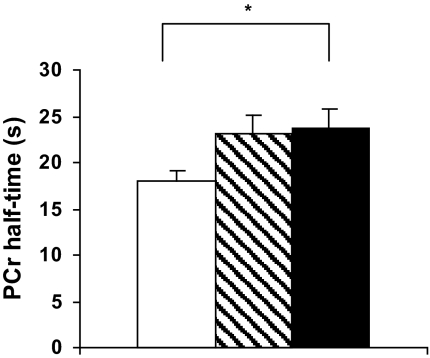
In vivo mitochondrial function.
Mean PCr recovery half-time (PCr-t1/2) was prolonged by 25% in diabetic patients compared with control subjects (23.8 ± 2.0 vs. 17.9 ± 1.2 s, respectively; P = 0.034) (Fig. 2), indicating impaired in vivo mitochondrial function in diabetic patients. First-degree relatives had a 23% longer PCr-t1/2 compared with control subjects (23.1 ± 2.0 s vs. 17.9 ± 1.2 s; Fig. 2), however, this did not reach statistical significance (P = 0.08). PCr levels decreased during knee-extension exercise until a steady state was reached. None of the subjects showed acidification at the end of the exercise protocol, and the pH decreased similarly from rest to end-exercise in all groups (end-exercise pH 7.02 ± 0.02, 7.01 ± 0.03, and 7.05 ± 0.03; ΔpH 0.08 ± 0.02, 0.08 ± 0.03, and 0.07 ± 0.03, respectively, in diabetic patients, first-degree relatives, and control subjects).
FIG. 2.
In vivo mitochondrial function expressed as PCr half-time (s) in control subjects, first-degree relatives, and diabetic patients. □, control; , FDR; ▪, type 2 diabetic patients. *P < 0.05 compared with diabetic patients.
, FDR; ▪, type 2 diabetic patients. *P < 0.05 compared with diabetic patients.
Mitochondrial density.
Mitochondrial density measured as mtDNA copy number and as citrate synthase activity was not different between groups (mtDNA copy number 5,813 ± 388, 5,573 ± 716, and 5,621 ± 430 arbitrary units; citrate synthase activity 92 ± 4.8, 103 ± 13.0, and 89 ± 7.4 μmol · g−1 protein · min−1, respectively, in diabetic patients, first-degree relatives, and control subjects; NS).
Ex vivo mitochondrial function.
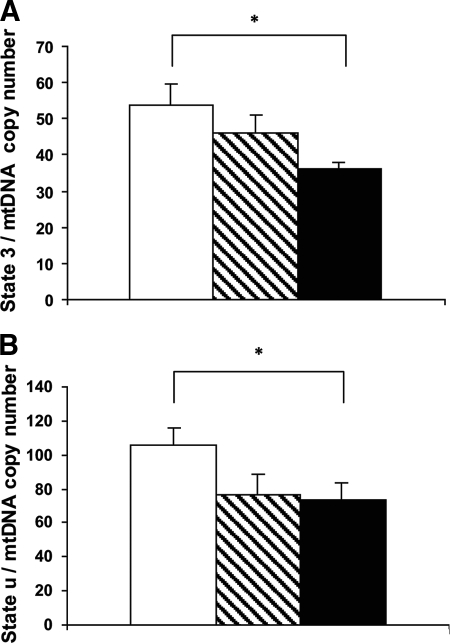
Unnormalized basal ADP-stimulated state 3 respiration was significantly lower in diabetic patients compared with control subjects [20.1 ± 1.0 vs. 27.0 ± 1.8 pmol/(s*mg), respectively; P = 0.024]. First-degree relatives did not significantly differ from control subjects or diabetic patients [24.9 ± 2.1 pmol/(s*mg)]. No difference in respiration was found between groups when ATP synthase was blocked with oligomycin (non-ADP–stimulated state 4 respiration) [12.1 ± 0.9, 11.0 ± 0.9, and 11.7 ± 0.8 pmol/(s*mg), respectively, for diabetic patients, first-degree relatives, and control subjects]. Although maximal respiratory capacity (FCCP-driven state u) was lower in diabetic patients compared with control subjects, differences between groups did not reach statistical significance [40.5 ± 3.3, 45.1 ± 5.3, and 51.9 ± 4.3 pmol/(s*mg), respectively, for diabetic patients, first-degree relatives, and control subjects]. When palmitoyl-carnitine was added as a substrate, similar tendencies were found (data not shown). To obtain intrinsic mitochondrial function, all O2 fluxes were normalized for mtDNA copy numbers, a marker for mitochondrial density, expressed as pmol/(s*mg)/mtDNA copy numbers × 10.000 (Table 4). Similar results were obtained when ex vivo data were normalized for citrate synthase activity (data not shown). After normalization, state 3 respiration was lower by 35% in diabetic patients compared with control subjects (P = 0.031; Table 4; Fig. 3A). Values in first-degree relatives were not significantly different from control subjects or diabetic patients (46.1 ± 4.8; Table 4; Fig. 3A). State 4 respiration was not different between groups (Table 4). Maximal respiratory capacity (FCCP-driven state u) after normalization was significantly lower in diabetic patients compared with control subjects (P = 0.05; Table 4; Fig. 3B) and tended to be lower in first-degree relatives compared with control subjects (P = 0.10; Table 4; Fig. 3B). When palmitoyl-carnitine was added as a substrate, similar tendencies were found: State 3 respiration (on malate plus palmitoyl-carnitine plus glutamate plus succinate addition) tended to be lower in diabetic patients compared with control subjects with no difference in first-degree relatives (Table 4). No differences were found between diabetic patients, first-degree relatives, and control subjects for state 4 respiration on addition of palmitoyl-carnitine (Table 4). Maximal respiratory capacity in the presence of palmitoyl-carnitine tended to be lower in first-degree relatives compared with control subjects (P < 0.1; Table 4). The value in diabetic patients was not significantly different (Table 4).
TABLE 4.
Normalized ex vivo mitochondrial respiration
| Control subjects | First-degree relatives | Diabetic patients | |
|---|---|---|---|
| State 3 on malate + glutamate + succinate | 53.8 ± 5.7 | 46.1 ± 4.8 | 35.1 ± 1.7* |
| State 4 | 23.0 ± 2.1 | 20.1 ± 2.0 | 20.8 ± 1.6 |
| State u | 105.8 ± 9.5 | 77.5 ± 11.4 | 72.8 ± 6.9* |
| State 3 on malate + palmitoyl-carnitine + glutamate + succinate | 60.8 ± 6.9 | 55.5 ± 4.6 | 42.1 ± 2.8 |
| State 4 | 34.4 ± 2.8 | 32.2 ± 4.3 | 28.6 ± 2.0 |
| State u | 113.8 ± 14.4 | 80.2 ± 6.4 | 88.8 ± 9.9 |
Data are means ± SE and are pmol/(s*mg)/(mtDNA copy numbers × 10,000).
P < 0.05 diabetic patients vs. control subjects.
FIG. 3.
Ex vivo state 3 (A) and state u respiration (B) normalized for mitochondrial content expressed as pmol · (s · mg)−1 · mtDNA copy number−1 (×10.000) in control subjects, first-degree relatives, and diabetic patients. □, control; , FDR; ▪, type 2 diabetic patients. *P < 0.05 compared with diabetic patients.
, FDR; ▪, type 2 diabetic patients. *P < 0.05 compared with diabetic patients.
Correlations.
A strong correlation was found between in vivo mitochondrial function (i.e., PCr-t1/2) and Vo2max (correlation coefficient −0.597, P = 0.000). Also, in vivo mitochondrial function correlated with mtDNA copy numbers (correlation coefficient −0.477, P = 0.007). Furthermore, in vivo mitochondrial function correlated with insulin-stimulated glucose oxidation (correlation coefficient −0.424, P = 0.020). Unnormalized state 3 respiration (on malate plus glutamate plus succinate addition) correlated negatively with fasting glucose (correlation coefficient −0.408, P = 0.016) and with in vivo mitochondrial function (PCr-t1/2) (correlation coefficient −0.373, P = 0.05). Metabolic flexibility expressed as ΔRQ correlated with unnormalized state 3 respiration (on addition of malate plus glutamate plus palmitoyl-carnitine plus succinate) (correlation coefficient 0.338, P = 0.047) and with in vivo mitochondrial function (PCr-t1/2) (correlation coefficient −0.368, P = 0.042). No correlations were found for in vivo or ex vivo mitochondrial function with insulin-stimulated Rd or with IMCL and/or free fatty acid levels.
DISCUSSION
Mitochondrial dysfunction has recently been implicated in the etiology of insulin resistance and type 2 diabetes. This suggestion is mainly based on studies that determined in vivo mitochondrial function (6–8). However, it is not yet elucidated whether intrinsic mitochondrial defects cause this lower in vivo mitochondrial function in type 2 diabetic patients and first-degree relatives. Ex vivo studies on mitochondrial function in type 2 diabetic patients appear less conclusive (13–15); however, in these studies, in vivo mitochondrial function was not assessed. To identify the true nature of reduced mitochondrial function in type 2 diabetic patients, the combination of in vivo and ex vivo measurements are of importance. Thus, impaired in vivo mitochondrial function might be caused by an impaired intrinsic capacity per mitochondrion or lower mitochondrial content. In this study, we performed both in vivo and ex vivo measurement of mitochondrial function in male diabetic patients, first-degree relatives, and control subjects, all matched for age and BMI.
We confirmed our previous finding (8) of compromised in vivo mitochondrial function, determined as the rate of PCr recovery after exercise in type 2 diabetic patients compared with age- and BMI-matched control subjects, and we extend these findings to a tendency to reduced in vivo mitochondrial function in normoglycemic first-degree relatives. In fact, this reduction in in vivo mitochondrial function was more pronounced in the seven subjects with multiple type 2 diabetic relatives (data not shown). Lower basal ATP synthesis rate in insulin-resistant first-degree relatives has been reported previously (6) when compared with insulin-sensitive healthy control subjects. Here, we report tendency to compromised mitochondrial function in first-degree relatives who possessed (nonsignificant) intermediate values of insulin sensitivity (the Rd of glucose, EGP, and nonoxidative glucose disposal) compared with age- and BMI-matched control subjects. This may suggest that a compromised mitochondrial function is an early defect in the pathogenesis of type 2 diabetes.
Interestingly, using high-resolution respirometry in permeabilized skinned muscle fibers, we identified lower ADP-driven state 3 respiration as an intrinsic mitochondrial defect (ex vivo) that underlies the mitochondrial dysfunction observed in vivo. However, mitochondrial dysfunction was not related to insulin sensitivity or IMCL content, and the latter was not different between groups. This is in line with earlier findings, in which no differences in IMCL were found between BMI-matched overweight diabetic patients and control subjects (8). Most likely, the combination of low oxidative capacity and fat content in muscle will lead to the accumulation of fatty acid intermediates, leading to muscular insulin resistance. Interestingly, the compromised ex vivo mitochondrial function could not be attributed to the mitochondrial density because the differences across groups remained on normalization to mtDNA copy number or citrate synthase. Moreover, even if in vivo mitochondrial function was adjusted for mtDNA copy number, differences between groups remained similar, as could be deduced from the similarity in mtDNA copy number between groups (data not shown). Thus, here, we show intrinsic mitochondrial defects in type 2 diabetic patients and similar tendencies in diabetes-prone first-degree relatives, which may underlie the mitochondrial dysfunction found in vivo.
The interesting, novel outcome of our study is the finding that intrinsic mitochondrial function, if also normalized to mitochondrial content, is lower in type 2 diabetic patients, and tended to be lower in first-degree relatives. Thus, both ADP-stimulated state 3 respiration and FCCP-driven maximal state u respiration were significantly lower (∼30%) in diabetic patients compared with control subjects. ADP-stimulated state 3 respiration reflects the capacity of the mitochondria to reduce the tricarboxylic acid cycle and β-oxidation–derived reducing equivalents NADH and FADH2 in the electron transport chain (ETC), resulting in oxidative phosphorylation of ADP to synthesize ATP at the level of ATP synthase. Under physiological conditions, the rate of state 3 respiration is limited by, or under control of, the activity of the phosphorylation system (including ATP synthase and ANT). Thus, bypassing the phosphorylation system ex vivo by the use of the chemical uncoupler FCCP results in a stimulation of respiration, called state u respiration. State u respiration hence reflects the maximal capacity of the ETC and the upstream dehydrogenases (malate, glutamate, and succinate dehydrogenase) involved in hydrolysis of the substrates supplied. This can therefore be referred to as maximal, uncontrolled mitochondrial oxidative capacity. The reduction of ∼30% in state u respiration as observed in type 2 diabetic patients therefore indicates a reduced maximal mitochondrial oxidative capacity in these patients that may reside at the level of the ETC and the upstream dehydrogenases. However, we found that state 3 respiration was also affected to a similar extent. Although, this could theoretically be explained by the reduced maximal mitochondrial capacity mentioned above (and thus at the level of the ETC and/or dehydrogenases), it should be noted that respiration was still stimulated on FCCP addition, in fact to a similar extent in type 2 diabetic patients and control subjects. Thus, state u respiration (ETC activity and upstream dehydrogenases) exceeds the level of state 3 respiration in all groups, indicating that also in type 2 diabetic patients, state 3 respiration is being limited by the phosphorylation system. Therefore, the 30% reduction in state 3 in diabetic patients indicates that the capacity of the phosphorylation systems is also reduced in these patients. Therefore, taken together, these data point toward a reduced intrinsic mitochondrial defect that resides both at the level of the ETC activity and/or upstream dehydrogenases and at the level of the phosphorylation system.
In first-degree relatives, the tendency to a lower in vivo mitochondrial function was accompanied by a tendency to a lower maximal respiratory capacity (state u), but no defect in state 3 respiration. A lower state u respiration, with unaffected state 3 respiration, points toward a reduced maximal ETC activity, without a reduction in the phosphorylation system. Thus, a tendency toward lower state u respiration in first-degree relatives suggests that mitochondria of first-degree relatives are capable of compensating the reduced maximal mitochondrial capacity by respiring on a higher percentage of the ETC capacity, i.e., with less tight control by the phosphorylation system.
Mitochondrial entrance of fatty acids via the carnitine shuttle system is classically believed to be rate limiting for β-oxidation. Using palmitoyl-carnitine, this putative limitation in fat oxidation is circumvented, thereby maximizing the flow through the β-oxidation. Through the addition of palmitoyl-carnitine to the substrate cocktail, additional reducing equivalents not requiring malate, glutamate, or succinate dehydrogenases are fed into the ETC. The addition of palmitoyl-carnitine, however, did not rescue the defects detected when using malate, glutamate, or succinate as substrates. This is an important observation suggesting that the defects observed in type 2 diabetic patients are unlikely to be localized in the malate, glutamate, and succinate dehydrogenases but are more likely to be located at the level of the ETC and the phosphorylation system. This indicates a lower overall intrinsic mitochondrial oxidative capacity. The reason for the latter is unknown but may involve ultrastructural mitochondrial changes. In that respect, smaller mitochondria have been reported for type 2 diabetic patients (1), and mitochondrial size was related to insulin sensitivity (1,26). Whether mitochondrial size determines overall mitochondrial capacity in these patients needs further investigation.
A putatively confounding factor when studying mitochondrial function is the level of physical activity of the subjects. In our study, we included sedentary subjects and type 2 diabetic patients without comorbidities. All subjects filled out a physical activity questionnaire indicating low levels of physical activity without differences between groups. Also maximal aerobic performance, which is a reflection of physical fitness, was similar between groups. This suggests that in the present study, the lower mitochondrial function in type 2 diabetes and tendency in first-degree relatives was not due to differences in level of habitual physical activity. Because physical activity is the major driver of mitochondrial biogenesis (27), the low and comparable level of physical activity may also explain why we did not observe any differences in mitochondrial content (determined by citrate synthase activity and mtDNA copy number) among diabetic patients, first-degree relatives, and control subjects.
Mitochondrial dysfunction implicated in type 2 diabetes, as shown in the present study, may alter substrate oxidation and might underlie the blunted increase in fat oxidation under conditions such as fasting, despite the presence of high circulating plasma levels of NEFA (28). This defect has been termed “metabolic inflexibility” and can also be observed as a reduced response to insulin, i.e., a reduced enhancement of glucose oxidation during insulin stimulation (29). A previous study indicated a link between defects in substrate switching and mitochondrial defects as shown in young, sedentary, healthy first-degree relatives (30). In their study, first-degree relatives were metabolic inflexible after consuming a high-fat diet, suggesting a decreased ability to enhance fat oxidation. In the present study, we observed metabolic inflexibility in type 2 diabetic patients, but not in first-degree relatives, together with a (tendency to) reduced in vivo mitochondrial function in both type 2 diabetic patients and first-degree relatives. Therefore, our data do not entirely match with the suggestion that mitochondrial dysfunction underlies this metabolic inflexibility. However, the change in respiratory quotient on insulin stimulation is more likely to be a reflection of reduced skeletal muscle insulin sensitivity.
In conclusion, the present study supports the hypothesis that intrinsic mitochondrial dysfunction is implicated in the etiology of type 2 diabetes. In vivo mitochondrial function was accompanied by lower ADP-driven mitochondrial respiration, if corrected for mitochondrial density. These mitochondrial aberrations are located at the level of both electron-transport chain capacity and oxidative phosphorylation system. Our data suggest that a reduced intrinsic ADP-stimulated mitochondrial respiration is an important factor in the pathogenesis of type 2 diabetes.
Acknowledgments
M.K.C.H. has received a Vidi grant for innovative research from the Netherlands Organization for Scientific Research (Grant 016.066.359). P.S. has received a grant from the Dutch Royal Academy of Arts and Sciences. This work has received Dutch Diabetes Research Foundation Grant 2004.00.059.
We thank Sanne van der Made and Sabine Baumgartner for practical help with the study.
Published ahead of print at http://diabetes.diabetesjournals.org on 4 August 2008.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
REFERENCES
- 1.Kelley DE, He J, Menshikova EV, Ritov VB: Dysfunction of mitochondria in human skeletal muscle in type 2 diabetes. Diabetes 51: 2944–2950, 2002 [DOI] [PubMed] [Google Scholar]
- 2.Shulman GI: Cellular mechanisms of insulin resistance. J Clin Invest 106: 171–176, 2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Petersen KF, Befroy D, Dufour S, Dziura J, Ariyan C, Rothman DL, DiPietro L, Cline GW, Shulman GI: Mitochondrial dysfunction in the elderly: possible role in insulin resistance. Science 300: 1140–1142, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patti ME, Butte AJ, Crunkhorn S, Cusi K, Berria R, Kashyap S, Miyazaki Y, Kohane I, Costello M, Saccone R, Landaker EJ, Goldfine AB, Mun E, DeFronzo R, Finlayson J, Kahn CR, Mandarino LJ: Coordinated reduction of genes of oxidative metabolism in humans with insulin resistance and diabetes: potential role of PGC1 and NRF1. Proc Natl Acad Sci U S A 100: 8466–8471, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mootha VK, Lindgren CM, Eriksson KF, Subramanian A, Sihag S, Lehar J, Puigserver P, Carlsson E, Ridderstrale M, Laurila E, Houstis N, Daly MJ, Patterson N, Mesirov JP, Golub TR, Tamayo P, Spiegelman B, Lander ES, Hirschhorn JN, Altshuler D, Groop LC: PGC-1alpha-responsive genes involved in oxidative phosphorylation are coordinately downregulated in human diabetes. Nat Genet 34: 267–273, 2003 [DOI] [PubMed] [Google Scholar]
- 6.Petersen KF, Dufour S, Befroy D, Garcia R, Shulman GI: Impaired mitochondrial activity in the insulin-resistant offspring of patients with type 2 diabetes. N Engl J Med 350: 664–671, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Szendroedi J, Schmid AI, Chmelik M, Toth C, Brehm A, Krssak M, Nowotny P, Wolzt M, Waldhausl W, Roden M: Muscle mitochondrial ATP synthesis and glucose transport/phosphorylation in type 2 diabetes. PLoS Med 4: e154, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schrauwen-Hinderling VB, Kooi ME, Hesselink MK, Jeneson JA, Backes WH, van Echteld CJ, van Engelshoven JM, Mensink M, Schrauwen P: Impaired in vivo mitochondrial function but similar intramyocellular lipid content in patients with type 2 diabetes mellitus and BMI-matched control subjects. Diabetologia 50: 113–120, 2007 [DOI] [PubMed] [Google Scholar]
- 9.Kemp GJ, Radda GK: Quantitative interpretation of bioenergetic data from 31P and 1H magnetic resonance spectroscopic studies of skeletal muscle: an analytical review. Magn Reson Q 10: 43–63, 1994 [PubMed] [Google Scholar]
- 10.Meyer RA: A linear model of muscle respiration explains monoexponential phosphocreatine changes. Am J Physiol 254: C548–C553, 1988 [DOI] [PubMed] [Google Scholar]
- 11.Sahlin K, Harris RC, Hultman E: Resynthesis of creatine phosphate in human muscle after exercise in relation to intramuscular pH and availability of oxygen. Scand J Clin Lab Invest 39: 551–558, 1979 [DOI] [PubMed] [Google Scholar]
- 12.Kemp GJ, Thompson CH, Barnes PR, Radda GK: Comparisons of ATP turnover in human muscle during ischemic and aerobic exercise using 31P magnetic resonance spectroscopy. Magn Reson Med 31: 248–258, 1994 [DOI] [PubMed] [Google Scholar]
- 13.Mogensen M, Sahlin K, Fernstrom M, Glintborg D, Vind BF, Beck-Nielsen H, Hojlund K: Mitochondrial respiration is decreased in skeletal muscle of patients with type 2 diabetes. Diabetes 56: 1592–1599, 2007 [DOI] [PubMed] [Google Scholar]
- 14.Boushel R, Gnaiger E, Schjerling P, Skovbro M, Kraunsoe R, Dela F: Patients with type 2 diabetes have normal mitochondrial function in skeletal muscle. Diabetologia 50: 790–796, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stump CS, Short KR, Bigelow ML, Schimke JM, Nair KS: Effect of insulin on human skeletal muscle mitochondrial ATP production, protein synthesis, and mRNA transcripts. Proc Natl Acad Sci U S A 100: 7996–8001, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kuipers H, Verstappen FT, Keizer HA, Geurten P, van Kranenburg G: Variability of aerobic performance in the laboratory and its physiologic correlates. Int J Sports Med 6: 197–201, 1985 [DOI] [PubMed] [Google Scholar]
- 17.Siri WE: The gross composition of the body. Adv Biol Med Phys 4: 239–280, 1956 [DOI] [PubMed] [Google Scholar]
- 18.DeFronzo RA, Tobin JD, Andres R: Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol 237: E214–E223, 1979 [DOI] [PubMed] [Google Scholar]
- 19.Mensink M, Blaak EE, van Baak MA, Wagenmakers AJ, Saris WH: Plasma free fatty acid uptake and oxidation are already diminished in subjects at high risk for developing type 2 diabetes. Diabetes 50: 2548–2554, 2001 [DOI] [PubMed] [Google Scholar]
- 20.Bergstrom J, Hermansen L, Hultman E, Saltin B: Diet, muscle glycogen and physical performance. Acta Physiol Scand 71: 140–150, 1967 [DOI] [PubMed] [Google Scholar]
- 21.Veksler VI, Kuznetsov AV, Sharov VG, Kapelko VI, Saks VA: Mitochondrial respiratory parameters in cardiac tissue: a novel method of assessment by using saponin-skinned fibers. Biochim Biophys Acta 892: 191–196, 1987 [DOI] [PubMed] [Google Scholar]
- 22.Shephard D, Garland PB: Citrate synthase from rat liver. Methods Enzymol 11–16, 1969
- 23.Kaaman M, Sparks LM, van Harmelen V, Smith SR, Sjolin E, Dahlman I, Arner P: Strong association between mitochondrial DNA copy number and lipogenesis in human white adipose tissue. Diabetologia 50: 2526–2533, 2007 [DOI] [PubMed] [Google Scholar]
- 24.Steele R: Influences of glucose loading and of injected insulin on hepatic glucose output. Ann N Y Acad Sci 82: 420–430, 1959 [DOI] [PubMed] [Google Scholar]
- 25.Frayn KN: Calculation of substrate oxidation rates in vivo from gaseous exchange. J Appl Physiol 55: 628–634, 1983 [DOI] [PubMed] [Google Scholar]
- 26.Toledo FG, Watkins S, Kelley DE: Changes induced by physical activity and weight loss in the morphology of intermyofibrillar mitochondria in obese men and women. J Clin Endocrinol Metab 91: 3224–3227, 2006 [DOI] [PubMed] [Google Scholar]
- 27.Menshikova EV, Ritov VB, Ferrell RE, Azuma K, Goodpaster BH, Kelley DE: Characteristics of skeletal muscle mitochondrial biogenesis induced by moderate-intensity exercise and weight loss in obesity. J Appl Physiol 103: 21–27, 2007 [DOI] [PubMed] [Google Scholar]
- 28.Kelley DE, Goodpaster B, Wing RR, Simoneau JA: Skeletal muscle fatty acid metabolism in association with insulin resistance, obesity, and weight loss. Am J Physiol 277: E1130–E1141, 1999 [DOI] [PubMed] [Google Scholar]
- 29.Storlien L, Oakes ND, Kelley DE: Metabolic flexibility. Proc Nutr Soc 63: 363–368, 2004 [DOI] [PubMed] [Google Scholar]
- 30.Ukropcova B, Sereda O, de Jonge L, Bogacka I, Nguyen T, Xie H, Bray GA, Smith SR: Family history of diabetes links impaired substrate switching and reduced mitochondrial content in skeletal muscle. Diabetes 56: 720–727, 2007 [DOI] [PubMed] [Google Scholar]