Abstract
Purpose
We developed manual-guided, replicable interventions based on common needs and cultural preferences of White and African American family caregivers (CGs) of individuals with dementia, and we evaluated these interventions after a 6-month follow-up.
Design and Methods
We randomly assigned White (n = 70) and African American (n = 48) CGs of individuals with dementia to either a skills training condition or a minimal support control condition.
Results
The degree of treatment implementation was methodically assessed, and findings demonstrated that both interventions were delivered according to protocol and were well received by CGs. CGs in both groups reported decreasing levels of problem behaviors and appraisals of behavioral bother, and increased satisfaction with leisure activities over time. On a measure of appraisal of distress related to behavior problems, White CGs showed more improvement in the minimal support control condition, and African American CGs showed the greatest improvements in the skills training condition. Spouse and nonspouse CGs also showed differential responses to intervention.
Implications
Brief manual-guided interventions can be effective with White and African American CGs, and greater attention should be paid to possible differential responses to interventions by race and relationship to care recipient.
Keywords: Dementia caregiving, Intervention, Racial diversity
Research evaluating the effectiveness of psychosocial interventions for family caregivers (CGs) is of vital importance for guiding clinical practice and public policy. Concerning the impact of interventions, CG intervention research to date has been mixed: whereas CGs generally report high satisfaction with and subjective benefit from interventions, most projects find relatively small effects of intervention on outcomes measuring general well-being such as depression (Bourgeois, Schulz, & Burgio, 1996). Zarit and his colleagues (Zarit, Stephens, Townsend, & Greene, 1998) have argued that CG intervention studies should focus not only on distal and multiply determined outcomes, such as general well-being, but also on proximal outcomes that are the specific focus of intervention and that are feasible to improve. These authors note that the use of a conceptual model to develop interventions may serve not only to focus the intervention but also to point to important intermediate outcomes of intervention worthy of careful study. Thus, it may be advantageous to measure multiple, theoretically relevant outcomes that include direct targets of intervention, and potential mediators of change, as well as measures such as depression that are clinically relevant but more difficult to modify.
In addition, several methodological concerns are noteworthy in developing CG interventions. Although some multicomponent interventions that are highly individualized have proven very effective in reducing CG depression (Mittelman et al., 1995), such interventions may be difficult to standardize and disseminate because they are so flexible and are heavily dependent on clinician judgment. Furthermore, issues of treatment implementation, or the degree to which interventions are shown to be implemented according to protocol, have received insufficient attention in this area and are increasingly recognized as critical (Burgio et al., 2001). Unless theory-based interventions are protocol driven, with proper assessment of implementation of treatment components, it is difficult to interpret outcome and achieve replication.
Another important issue for intervention research is that of racial or ethnic diversity. There is a growing body of literature documenting the ways that race, ethnicity, and culture affect the experience of caregiving (Dilworth-Anderson, Williams, & Gibson, 2002), but we have identified no studies that have examined whether CG interventions are similarly effective across racial-ethnic groups. Still, a number of suggestions have been offered for developing interventions that are responsive to the special needs of African American CGs (Gallagher-Thompson et al., 2000; Henderson, Gutierrez, Mayke, Garcia, & Boyd, 1993). Guided by a stress process model of family caregiving (Haley, Levine, Brown, & Bartolucci, 1987; Haley et al., 1996; Schulz, Gallagher-Thompson, Haley, & Czaja, 2000), our goal was to develop multicomponent interventions intended to address the common needs of White and African American family CGs while remaining responsive to cultural issues. Both White and African American CGs face similar stressors, including primary caregiving stressors such as managing problem behaviors and secondary stressors such as social isolation and health problems in the caregiver. The effects of these stressors on CG well-being can be mediated by factors such as cognitive appraisals (including both appraisals of distress and benefit from caregiving), social support and activity, and coping responses. Interventions that target both stressors and these mediating factors are thought to be of greatest benefit to CGs.
In an effort to affect stressors and to improve variables that may mediate the impact of stressors on well-being, we developed a skills training condition (STC) with three foci. First, we teach CGs behavior management skills and their application to the proximal problem of care recipient (CR) problem behaviors, with the goals of decreasing the frequency of behavioral problems and the caregiver distress that is related to them. Second, we teach CGs problem-solving skills and encourage their use to increase pleasant events such as leisure activities, to enhance social support, and to focus on self-care such as exercise and diet. Finally, we include cognitive restructuring to encourage more benign appraisals of behavior problems that are difficult to control or that worsen over time and to help caregivers find meaning and personal gain from caregiving where possible.
We applied this stress process framework to our intervention, and we offered the following specific goals. First, we worked to develop short-term psychosocial interventions that would be equally well received by White and African American CGs and to standardize the interventions so that we could demonstrate treatment implementation. We hypothesized that we could attain high levels of treatment implementation and receipt for both interventions. Second, at a 6-month follow-up, we compared the effectiveness of an STC that targets improvement of CG behavior management skills, problem solving, and cognitive restructuring to a minimal support control condition (MSC) that provides general telephone support and written information. We expected the STC intervention to be especially effective in improving measures of CR problem behaviors, CG appraisal, and CG social support and activity. We also assessed whether interventions improved more distal measures of well-being, including depression and anxiety, and CGs’ intention to place the CR in a nursing home. Third, we explored the differential impact of the interventions on White and African American CGs to determine whether they showed similar benefits from the interventions, versus differential effectiveness across race.
Methods
Recruitment and Participant Eligibility
The project was based in Birmingham, Alabama. CG–CR dyads were referred to the study from geriatric and memory-disorder clinics operating within the University of Alabama at Birmingham, community-based home health care agencies, Alzheimer’s disease and related disorders (ADRD) service delivery organizations (e.g., adult day care centers), nonprofit organizations serving CGs of individuals with dementia, and self-referrals.
Referrals were eligible for enrollment if they were (a) self-identified as White or African American and (b) at least 21 years of age, and if they (c) lived with and provided care for a relative with ADRD for an average of at least 4 hr of supervision or direct care per day for the past 6 months. CGs were excluded from participation if they were involved in another CG psychosocial intervention study or had an acute illness that would prevent them from participating for at least 6 months.
CR eligibility was based on cognitive, functional, and behavioral characteristics. Enrollment was limited to CRs who (a) possessed a medical diagnosis of probable ADRD or exhibited a Mini-Mental State Exam (MMSE; Folstein, Folstein, & McHugh, 1975) score of less than 24, (b) exhibited at least one limitation in basic activities of daily living (ADLs; Katz, Ford, Moskowitz, Jackson, & Jaffe, 1963) or two dependencies in instrumental activities of daily living (IADLs; Lawton & Brody, 1969) according to CG report, and (c) displayed at least three problem behaviors identified by the primary CG. Other requirements were logistical and included having telephone service, living within a 60-mile radius of the University, and planning to remain in the geographic area for at least 6 months.
Design
This was a two-group comparison design with dyads being minimized (Taves, 1974) to the STC or the MSC on the basis of race, behavior problem severity, cognitive impairment, and gender of the CG. Logistics of the study required that research personnel function as both interventionists and assessors, both of whom attended a weekly clinical case review meeting. Although staff were not blinded to group assignment, for bias to be minimized, intervention and assessment of a dyad were never conducted by the same individual.
Procedures
Screening and Schedule of Assessments
Potential participants were interviewed over the telephone by using a standardized set of screening questions. After informed consent was obtained from CGs and CRs who met entry criteria (proxy consent when appropriate), CGs were administered a core battery of measures in the home through a face-to-face interview. Dyads were then minimized to either the STC or MSC conditions. CGs were subsequently interviewed by using the core battery at 6, 12, and 18 months; however, only 6-month data are reported in this paper. The core battery was modified if the CR died or was placed in a long-term care setting prior to the next scheduled interview. The bereavement and placement batteries eliminated measures that were not relevant to current caregiving concerns, such as number of behavior problems and CG appraisal. Consequently, the analytic sample size reported in this paper varies across outcome measures according to the disposition status of the CG (i.e., active caregiving at home, long-term care placement, or bereaved). The battery of measures used at each testing occasion is described in more detail by Wisniewski and colleagues (in press). All project activities were approved and monitored by the Institutional Review Boards for Human Use of the University of Alabama and the University of Alabama at Birmingham.
For both interventions, we went to considerable effort to make treatments appealing and culturally appropriate for African American and White CGs. These efforts are described in detail in another paper (Gallagher-Thompson et al., 2000), and both treatment manuals are available by request from the authors.
Skills Training Condition
The intervention was delivered through a group workshop followed by 16 in-home treatment sessions over a 12-month period, although the present paper reports only 6-month outcomes. The goal of the workshop was to establish a similar knowledge base for CGs in behavior management, problem solving, and cognitive restructuring.
Participants in the STC first attended a 3-hr group workshop consisting of three to eight CGs. Interactive instructional activities were used to encourage sharing among CGs. CGs were also provided with a skills training notebook and with videotapes that demonstrated critical skill techniques. A TV–VCR was lent to CGs who did not own a VCR.
At standard intervals after the workshop, CGs were visited by a REACH interventionist who assisted them in the application of therapeutic skills. CGs received four weekly home visits during the first month of the intervention and two more visits during the second month. Over the next 10 months, home visits were alternated monthly with therapeutic phone calls during which therapeutic skills were further refined. Home visits were structured to last approximately 1 hr. Between the baseline and 6-month assessments, CGs were scheduled to receive eight home visits and two therapeutic phone calls.
CGs received basic information in behavior management techniques (i.e., identification of environmental antecedents and consequences surrounding a target behavior) as well as instruction and support in the technical application of specific behavioral and environmental treatments. Although an array of behavioral strategies was taught to CGs, frequently used antecedent strategies included communication skills and prosthetic memory aids, as well as reinforcement techniques.
CGs were also given specific instructions in the application of problem solving to achieve personal goals that might ameliorate CG distress. The interventionist encouraged application of these skills to increase pleasant events, social support, and exercise or to improve the CG’s diet. However, CGs were free to choose any goal related to CG distress. Participants were taught to define a problem, generate possible solutions, choose and implement a solution, and monitor progress toward the goal.
Another component was cognitive restructuring. In using this technique, the therapist encouraged more benign appraisals of caregiving stressors, such as more realistic beliefs and goals. For example, it was not uncommon for CGs to display erroneous beliefs about dementia (e.g., the CR is engaging in disruptive behavior to “spite” the CG) or to set unrealistic goals (e.g., to get a relative to provide support on a daily basis). In applying both behavior management and problem solving, the interventionist assisted the CG in focusing on the problems-goals that were most stressful to them. Individually written “behavioral prescriptions” were generated, progress toward achieving goals was tracked, and changes to the prescriptions were made based on progress. New prescriptions could be added if the problem or goal proved intractable or a goal was attained.
Minimal Support Condition
All CGs assigned to the MSC were provided telephone support composed of empathic statements, active listening, and generic written educational materials. The REACH interventionist provided telephone contact to the CGs on the same schedule as the STC. Telephone support calls were brief (target time was 15 min) and structured. Structure was provided by scripted prompts that interventionists used to engage the CG. Prompts focused on the CG’s and CR’s physical health and general problems associated with caregiving (the script is available from L. Burgio). Educational materials were provided in three phases. The first two phases included general information on dementia and dementia caregiving. Materials were mailed during Months 1 and 3. The third-phase materials were delivered on demand, only if a CG voiced concern about a specific problem. Phase 3 materials consisted of single-page fact sheets that presented “suggestions” for addressing problem behaviors such as wandering and repetitive questions. The intent was to provide useful information to MSC CGs in acute distress, but not to provide more specific and individualized “prescriptions” or therapist assistance. Of the MSC CGs, 77% received Phase 3 materials.
Measures
Standardized measures were selected to assess specific variables within the following categories: descriptive and demographic variables, treatment implementation (described in detail in the Results section), CR problem behaviors, CG appraisal, CG social support and activity, CG well-being, and desire to institutionalize.
Descriptive and Demographic Variables
CGs reported age, sex, race, and educational attainment for themselves and for CRs. They also reported on their relationship to the CR. The MMSE (Folstein, et al., 1975) was administered to CRs by trained interviewers to obtain a brief assessment of general cognitive impairment. The NAM–Powers Index of Occupational Status was used as a measure of socioeconomic status (SES; Nam & Terrie, 1998). CGs reported both their own current (or previous, if retired) occupation and that of their spouse, and they scored for occupational prestige on a scale from 0 to 100. For married CGs, the higher score of the couple was used as an index of family SES.
CR Problem Behaviors
Behavior problems were assessed with a modified version of the Revised Memory and Behavior Problem Checklist (RMBPC; Teri et al., 1992), which consists of 24 items that inquire about the problem behaviors of the CR. CGs were asked to indicate whether or not the problem had occurred during the past week (yes or no), yielding a measure of the number of problem behaviors reported. The original version of this measure allowed the recording of frequency of individual behavior problems.
CG Appraisal
CG appraisal of problem behaviors was assessed by the RMBPC. If CGs responded that a particular problem had occurred during the past week, they were then asked to rate how much the problem “bothered or upset” them on a 0 (not at all) to 4 (extremely) scale. A behavioral bother score was obtained by averaging these ratings across all reported problems. Appraisals of benefits from caregiving were assessed with the Positive Aspects of Caregiving (PAC) scale, developed by the REACH investigators. The PAC consisted of nine items phrased as statements about the CG’s mental–affective state in relation to the caregiving experience. Each item began with the stem “Providing help to the CR has …,” followed with specific items (e.g., made me feel useful, enabled me to appreciate life more). Each item was rated on a 1- to 5-point Likert-type scale ranging from “disagree a lot” (1) to “agree a lot” (5). Cronbach’s alpha measure of internal consistency was reported to be .88 for this instrument (Tarlow et al., in press).
CG Social Support and Activity
To assess the CG’s social support, the REACH project included a 28-item measure that assessed social networks (family, friends, and confidants), received support, satisfaction with support, and negative interactions. Of relevance to this paper were the Lubben Social Network Index (LSNI, Lubben, 1988) and the CG’s satisfaction with support. The LSNI scale was adapted from one developed by Berkman and Syme (1979) for older adults, and it consisted of eight items. Satisfaction with support was assessed with three items, one each concerning the overall satisfaction with tangible, emotional, and informational support received (Krause, 1995; Krause & Markides, 1990).
The Leisure Time Satisfaction measurement was constructed by REACH investigators to measure the level of satisfaction that CGs report concerning the amount of time spent in leisure activities. Six items targeted those activities commonly listed on existing leisure measures and believed to be relevant to the dementia caregiving experience (e.g., hobbies, quiet time, and church attendance). The CGs were asked “over the past month, how satisfied are you with the amount of time you have been able to spend….” Each item was rated on a 3-point scale (0 = not at all, 1 = a little, and 2 = a lot). Total summary scores range from 0 to 12. Evidence for the reliability and validity of this new instrument is reported elsewhere, including a Cronbach’s alpha measure of internal consistency equal to .80 (Stevens et al., 2001).
CG Well-Being
The Center for Epidemiological Studies–Depression Scale (CES-D; Radloff & Teri, 1986) was used as a measure of CG depressive symptoms. For each of the 20 items, CGs rated the frequency of this symptom on a 0 (rarely) to 3 (most of the time) scale. Higher scores are indicative of greater depression, with a score of 16 or more considered to be clinically significant. Cronbach’s alpha was .86 in the REACH sample of over 1,200 CGs.
The ten items on the anxiety subscale of the State-Trait Personality Inventory (Spielberger, 1983) were administered as a measure of the CG’s mental state of anxiety. Response options ranged on a 4-point scale of intensity from “not at all” to “very much” over the past week.
Desire to Institutionalize
A seven-item scale created by Morycz (1985) was used to measure whether or not the CG was considering institutionalization of the CR. Specific questions probed if the CR had spoken with family members, friends, or professionals, or had taken steps to identify a nursing home. Scoring for each item is binary (yes or no). Pruchno and Potashnik (1989) reported a coefficient alpha of .82 for this scale and a strong relationship with actual placement.
Results
Sample Characteristics
Two hundred and eighty-nine CG–CR dyads were screened, 203 were deemed eligible, and 140 consented to participate. Of the 140 participants who consented, 70 were randomized to each group. There were 118 dyads that completed a 6-month assessment, 57 from the MSC and 61 from the STC. Eight of these CRs (3 from the MSC and 5 from the STC; 6 White and 2 African American) had been placed in long-term care settings, and 12 were deceased prior to the 6-month assessment. Thus, their data were obtained from the placement and bereavement batteries, respectively. A total of 22 dyads (13 from the MSC and 9 from the STC) discontinued their participation in the study prior to the 6-month assessment. There was no significant difference in discontinuation rate between the two groups. The resultant sample did not differ from the baseline sample of 140 dyads on key demographic characteristics (CG race, age, and CES-D; CR MMSE, frequency of problem behaviors, and behavioral bother scores).
Demographic characteristics of the sample are shown in Table 1 by condition and racial group. CGs and CRs in the MSC did not differ significantly from those in the STC on any demographic characteristics. Spousal and nonspousal CGs are similarly represented in the predominantly female sample. On average, CGs reported obtaining high levels of formal education and moderate household occupational status (Nam–Powers score). CRs exhibited moderate cognitive impairment. CG and CR race matched for all dyads.
Table 1.
Demographic Characteristics of the Analysis Sample
| Characteristic | MSC | STC | White | African American |
|---|---|---|---|---|
| CG and CR Race (%) | ||||
| White | 28.81 (n = 34) | 30.51 (n = 36) | NA | NA |
| African American | 19.49 (n = 23) | 21.19 (n = 25) | ||
| Spouse or not (%) | ||||
| Spouse | 21.19 (n = 25) | 28.81 (n = 34) | 38.14 (n = 45)*** | 11.86 (n = 14)*** |
| Nonspouse | 27.12 (n = 32) | 22.88 (n = 27) | 21.19 (n = 25) | 28.81 (n = 34) |
| CG Sex (%) | ||||
| Male | 10.17 (n = 12) | 11.86 (n = 14) | 15.25 (n = 18) | 6.78 (n = 8) |
| Female | 38.14 (n = 45) | 39.83 (n = 47) | 44.07 (n = 52) | 33.90 (n = 40) |
| CR Sex (%) | ||||
| Male | 16.10 (n = 19) | 23.73 (n = 28) | 27.12 (n = 32) | 12.71 (n = 15) |
| Female | 32.20 (n = 38) | 27.97 (n = 33) | 32.20 (n = 38) | 27.97 (n = 33) |
| CG education level | ||||
| M
(SD) |
13.30
(2.28) |
13.38
(2.03) |
13.53
(1.93) |
13.06
(2.41) |
| CR education level | ||||
| M
(SD) |
10.68
(3.80) |
11.45
(3.24) |
12.00**
(2.91) |
9.70**
(3.94) |
| Nam–Powers score (dyad) | ||||
| M
(SD) |
67.04
(20.17) |
62.68
(20.39) |
68.59*
(18.91) |
59.17*
(21.21) |
| CR MMSE (baseline) | ||||
| M
(SD) |
13.70
(6.82) |
12.51
(8.12) |
14.53*
(8.18) |
10.98*
(5.88) |
| CG age | ||||
| M
(SD) |
63.51
(10.24) |
62.14
(14.43) |
66.35****
(10.30) |
57.62****
(13.78) |
| CR age | ||||
| M
(SD) |
79.45
(8.24) |
77.96
(8.47) |
78.06
(8.36) |
79.59
(8.36) |
Notes: Analysis sample is N = 118. MSC = minimal support control condition; STC = skills training condition; CG = caregiver; CR = care recipient; MMSE = Mini-Mental State Exam; NA = not applicable.
p = 0.01;
p = .0004;
p = .0002;
p = .0001.
Significant differences between White and African American CGs were noted on several characteristics. CGs differed in relationship to the CRs, that is, χ2 (1,N = 118) = 14.05 and p=.0002, with White CGs more likely to be spouses than nonspouses and African American CGs more likely to be nonspouses than spouses. White CGs were significantly older, that is, t(116) = 3.93 and p=.0001, and reported higher household occupational status, that is, t(116) = 2.51 and p=.01, than African American CGs. African American CRs reported lower educational attainment, that is, t(115) = 3.62 and p=.0004, and demonstrated greater cognitive impairment as measured on the MMSE, that is, t(116) = 2.58 and p=.01, than White CRs. These differences are consistent with those found in previous studies of White and African American CGs (Dilworth-Anderson et al., 2002) and appear to reflect real differences in the CG characteristics by race or ethnicity.
Treatment Implementation
Lichstein’s model (Burgio et al., 2001; Lichstein, Riedel, & Grieve, 1994) was used to guide treatment implementation (TI) induction and assessment strategies. Thus, we measured three aspects of TI: treatment delivery, the interventionists’ ability to present the intervention to the CG as intended; treatment receipt, the extent to which the CG learns and understands the intended intervention; and treatment enactment, the degree to which the CG demonstrates changes in therapeutic behaviors in the natural environment.
Treatment Delivery
Eleven interventionists were trained to performance criterion in treatment delivery established by the investigators and achieved certification by the REACH Coordinating Center in Pittsburgh. Detailed treatment manuals were used and feedback on accuracy was provided in the weekly clinical case review meetings. Additionally, all therapeutic contacts were audiotaped, with 20% of the tapes coded for accuracy of delivery by the project manager in accordance with a standardized checklist. The mean accuracy rates across interventionists were 85% (SD = 10.32) and 95% (SD = 5.0) for the STC and MSC, respectively. Interventionists did not differ in accuracy when delivering the intervention to African American and White CGs. Thus, the data suggest highly accurate delivery of treatment protocols.
Treatment Receipt
The number and duration of therapeutic contacts with the CGs were measured. These variables were influenced heavily by the availability of the CGs. CGs controlled their availability to the therapist and could terminate a phone or home session prior to the predetermined length. In the STC, CGs received an average of 10 contacts (SD = 2.74) with an average home visit duration of 50.06 min (SD = 13.67). MSC CGs received an average of 9.83 (SD = 1.75) contacts with an average duration of 11.69 min (SD = 3.84). Racial differences in these variables did not emerge except in the MSC for duration. African American CGs spent an average of 2 fewer minutes per MSC phone call than Whites, M = 10.50 and SD = 3.47, versus M = 12.50 and SD = 3.94, respectively; t(63) = 2.05 and p=.04. These data suggest that actual treatment receipt by the CGs was similar to that intended in the protocol.
Treatment Enactment
Four basic components of the STC intervention were identified: CG data collection, homework assignments, use of videotapes and notebooks, and use of written prescriptions. (Enactment was not measured in the MSC group.) During each session the interventionists recorded their impression of the number of components engaged in since the prior session (0–4). The mean enactment score assigned by interventionists to the STC group was 2.25 components (SD = .88; Mode = 3). However, it should be noted that CG data collection was not emphasized by the interventionists if the CG appeared overburdened by this activity, and this was often the case. A closer inspection of the data shows that nearly half (48%) of the sessions showed good to excellent enactment (3 or 4), nearly one third (31%) showed poor enactment (0 or 1), and 21% showed moderate enactment (2). Racial differences were not found on this treatment enactment measure.
Primary Outcomes
The impact of intervention was analyzed in two steps. First, the effects of treatment condition (STC vs. MSC), race (African American vs. White), and their interaction on outcome were examined by conducting analyses of covariance (ANCOVAs) on the 6-month outcome scores with baseline scores serving as the only covariate. In a second step conducted in order to determine whether general effects occurred across time for both treatment conditions, change scores (i.e., 6-month – baseline) were calculated and tested to see if significant change was observed across both groups. We used intent to treat analyses, a conservative approach that does not require minimum levels of TI. Descriptive data for these outcome variables are displayed in Table 2.
Table 2.
Means and Standard Deviations for Outcome Measures by Race and Group Assignment
| MSC White
|
MSC AA
|
STC White
|
STC AA
|
|||||
|---|---|---|---|---|---|---|---|---|
| Outcome Var. | Baseline | 6 months | Baseline | 6 months | Baseline | 6 months | Baseline | 6 months |
| Behavioral problems | ||||||||
| RMBPC No. of prob. behaviors | ||||||||
| n | 30 | 30 | 20 | 20 | 27 | 27 | 20 | 20 |
| M
(SD) |
11.23
(3.55) |
9.61
(4.56) |
10.50
(4.88) |
9.89
(5.30) |
10.79
(3.10) |
9.64
(3.60) |
11.95
(3.47) |
10.23
(3.33) |
| Appraisal | ||||||||
| RMBPC behav. bother | ||||||||
| n | 29 | 29 | 20 | 20 | 27 | 27 | 20 | 20 |
| M
(SD) |
1.50
(0.88) |
1.15
(0.83) |
1.73
(1.18) |
1.77
(1.14) |
1.62
(1.06) |
1.54
(1.02) |
1.35
(1.10) |
0.91
(0.88) |
| Pos. aspects of caregiving | ||||||||
| n | 30 | 30 | 20 | 20 | 27 | 27 | 21 | 21 |
| M
(SD) |
32.30
(9.07) |
32.06
(10.04) |
36.10
(7.75) |
37.40
(8.29) |
32.81
(9.56) |
34.11
(8.68) |
37.48
(8.55) |
40.67
(5.14) |
| Social support and activity | ||||||||
| Social network | ||||||||
| n | 32 | 32 | 21 | 21 | 31 | 31 | 22 | 22 |
| M
(SD) |
19.06
(5.42) |
18.25
(5.49) |
18.43
(4.97) |
16.67
(6.58) |
18.10
(6.12) |
18.42
(4.57) |
16.45
(5.70) |
17.32
(5.96) |
| Satis. social supp. | ||||||||
| n | 32 | 32 | 21 | 21 | 31 | 31 | 22 | 22 |
| M
(SD) |
6.28
(2.32) |
6.44
(1.97) |
5.76
(2.00) |
4.67
(2.31) |
5.23
(2.26) |
5.65
(2.21) |
5.77
(2.83) |
5.55
(2.63) |
| Satis. leisure act. | ||||||||
| n | 34 | 34 | 23 | 23 | 36 | 36 | 25 | 25 |
| M
(SD) |
5.82
(3.02) |
6.24
(3.13) |
4.83
(3.24) |
5.26
(3.32) |
5.06
(2.56) |
6.32
(2.45) |
4.76
(3.99) |
5.48
(3.43) |
| Well-being | ||||||||
| CES-D | ||||||||
| n | 34 | 34 | 23 | 23 | 36 | 36 | 25 | 25 |
| M
(SD) |
9.44
(8.70) |
10.03
(9.27) |
14.48
(10.57) |
14.79
(10.76) |
16.53
(9.03) |
14.10
(11.48) |
14.60
(9.99) |
12.93
(11.86) |
| Anxiety | ||||||||
| n | 34 | 34 | 23 | 23 | 36 | 36 | 25 | 25 |
| M
(SD) |
18.03
(6.24) |
18.12
(7.36) |
19.91
(7.17) |
19.04
(6.79) |
22.17
(5.93) |
22.61
(7.64) |
21.68
(7.92) |
19.16
(8.01) |
| Desire to Institutionalize | ||||||||
| Desire to Inst. | ||||||||
| n | 28 | 28 | 20 | 20 | 25 | 25 | 21 | 21 |
| M
(SD) |
0.71
(1.30) |
1.46
(1.57) |
0.60
(1.14) |
0.55
(1.28) |
1.04
(1.37) |
1.32
(1.07) |
1.00
(1.30) |
1.00
(1.10) |
Note: MSC = minimal support control condition; STC = skills training condition; AA = African American; RMBPC = Revised Memory and Behavior Problem Checklist; CES-D = Center for Epidemiological Studies–Depression scale.
In all ANCOVAs, the covariate effect was highly significant statistically (p < .0001), indicating that baseline scores were highly correlated with the 6-month outcome scores. With regard to the independent variables, there were no significant main effects for treatment condition on the covariate adjusted 6-month outcome scores for any variable (all p values >.10). Significant main effects for race and significant treatment by race interaction effects for the ANCOVAs are reported in the following paragraphs by category, along with the significant main effects for time (i.e., baseline vs. 6-month scores across both treatment conditions).
Problem Behaviors
Although no significant effects were found for race, treatment group, or their interaction, a significant effect for time was found on the RMBPC Problem Behavior scale, that is, F(1,96) = 14.68 and p = .0002. The mean number of problem behaviors declined over time, from 11.11 (SD = 3.71) at baseline to 9.80 (SD = 4.19) at 6 months after baseline.
CG Appraisal
A significant main effect was found for race on the PAC scale, that is, F(1,93) = 5.95 and p = .02. African Americans showed increases on this measure from baseline (M = 36.80; SD = 8.10) to 6-month outcome (M = 39.07; SD = 6.97), whereas more stable values were observed for Whites (M = 32.54 and SD = 9.22 and M = 33.03 and SD = 9.40, respectively).
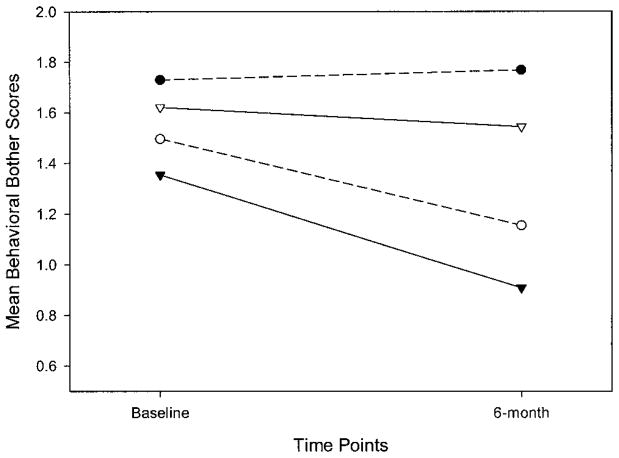
A significant main effect for time was found for the RMBPC Behavioral Bother scale, that is, F(1,95) = 6.40 and p = .01, with scores declining in both groups. More importantly, a statistically significant treatment by race interaction effect was found from the ANCOVA on the RMBPC Behavioral Bother score, that is, F(1,91) = 9.97 and p = .002. This interaction effect is depicted in Figure 1. The STC was more effective for reducing the bother ratings of African Americans, whereas the MSC was more effective for White CGs. Post hoc pairwise comparisons on the covariate-adjusted 6-month outcome scores revealed that African Americans in the STC achieved significantly lower 6-month behavioral bother scores (M = .91; SD = .88) than either African Americans in the MSC, that is, M = 1.77, SD = 1.14, t(91) = −2.78, and p < .01, or Whites in the STC, that is, M = 1.54, SD = 1.02, t(91) = −2.23, and p < .05. In addition, Whites in the MSC had lower 6-month behavioral bother scores than African Americans in the MSC, that is, M = 1.15 and SD = .83 and M = 1.77 and SD = 1.14, respectively; t(91) = −2.26 and p < .05.
Figure 1.
Revised Memory and Behavior Problem Checklist behavioral bother scores: caregiver race by group interaction effect. (MSC and STC = minimal support control and skills training conditions, respectively.) —●— MSC Black; —○— MSC White; —▼— STC Black; —▽— STC White.
Social Network, Social Support, and Activity
A significant main effect for race was found in the ANCOVA for satisfaction with social support, that is, F(1,101) = 5.96 and p = .02. African Americans reported decreases in satisfaction with social support (M = 5.77 and SD = 2.43, and M = 5.12 and SD = 2.49, for baseline and 6 months), whereas White participants were found to have a stable level on this variable (M = 5.76 and SD = 2.33, and M = 6.05 and SD = 2.11, for baseline and 6 months). Social network was not affected by treatment, race, or their interaction.
A significant change was found over time for the Leisure Time Satisfaction scale, that is, F(1,117) = 5.75 and p = .02, with significant increases from the baseline to 6-month assessments (M = 5.17 and SD = 3.16 to M = 5.91 and SD = 3.04, respectively) across both intervention groups.
Well-Being
No significant effects were found for race, treatment group, their interaction, or time for either the CES-D or anxiety measure.
Desire to Institutionalize
A significant main effect was found for race, that is, F(1,89) = 5.39 and p = .02. Whites showed increases in the desire to institutionalize from baseline (M = .87; SD = 1.33) to 6 months (M = 1.40; SD = 1.35), whereas scores for African Americans on this measure remained stable (M = .80 and SD = 1.23, and M = .78 and SD = 1.19, for baseline and 6 months). There were no differences by intervention group.
Effects of the Relationship Between CG and CR
Secondary analyses were conducted to examine the effects of the relationship between the CG and CR on outcome scores. CGs were classified as either spouses (n = 59) or nonspouses (n = 59), and this variable was added as an additional independent variable along with treatment condition and race in additional ANCOVA models.
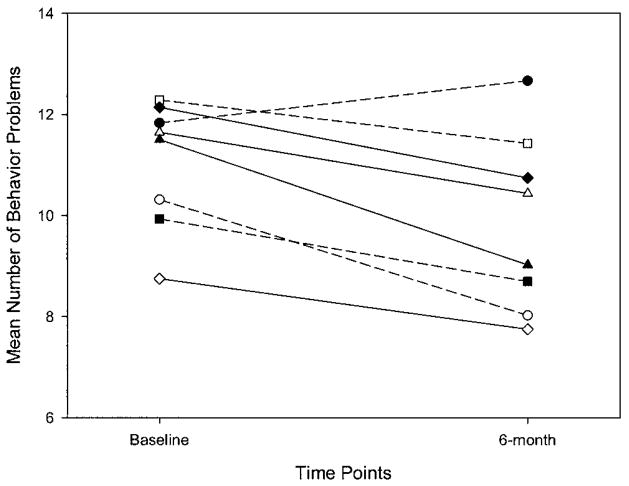
A statistically significant treatment by race by relationship interaction effect was found for the number of problem behaviors on the RMBPC, that is, F(1,88) = 5.19 and p = .03. This effect is illustrated in Figure 2, where it is evident that the largest decreases in the number of problem behaviors were observed for White spouses in the MSC and African American spouses in the STC. Post hoc pairwise comparisons on the covariate-adjusted 6-month outcome scores indicated that White spouses in the MSC had significantly lower outcome scores than African American spouses in the MSC, that is, M = 8.57 and SD = 4.07, and M = 12.67 and SD = 5.32, respectively; t(88) = −2.34 and p < .05. African American spouses in the MSC actually showed modest increases in the number of behavior problems from baseline to 6-month outcome (M = 11.83 and SD = 5.04 to M = 12.67 and SD = 5.32).
Figure 2.
Revised Memory and Behavior Problem Checklist mean number of behavior problems by caregiver race, relationship, and group interaction effect. (MSC and STC = minimal support control and skills training conditions, respectively.) —○— MSC White Spouse; —△— STC White Spouse; —●— MSC Black Spouse; —▲— STC Black Spouse; —□— MSC White Nonspouse; —⋄— STC White Nonspouse; —■— MSC Black Nonspouse; —◆— STC Black Nonspouse.
A statistically significant race by relationship interaction effect was found for the LSNI, that is, F(1,97) = 5.82 and p = .02. This effect is illustrated in Figure 3. White spouses had the highest LSNI scores at baseline. Their scores, as well as the scores of African American nonspouses and White non-spouses, remained relatively stable from baseline to the 6-month assessment. African American spouses had the lowest scores and were found to decrease markedly from baseline to 6 months. Post hoc pairwise comparisons on the covariate-adjusted 6-month scores indicated a significant difference between White and African American spouses, that is, M = 19.41 and SD = 4.45, and M = 14.42 and SD = 6.95, respectively; t(97) = 2.28 and p < .05.
Figure 3.
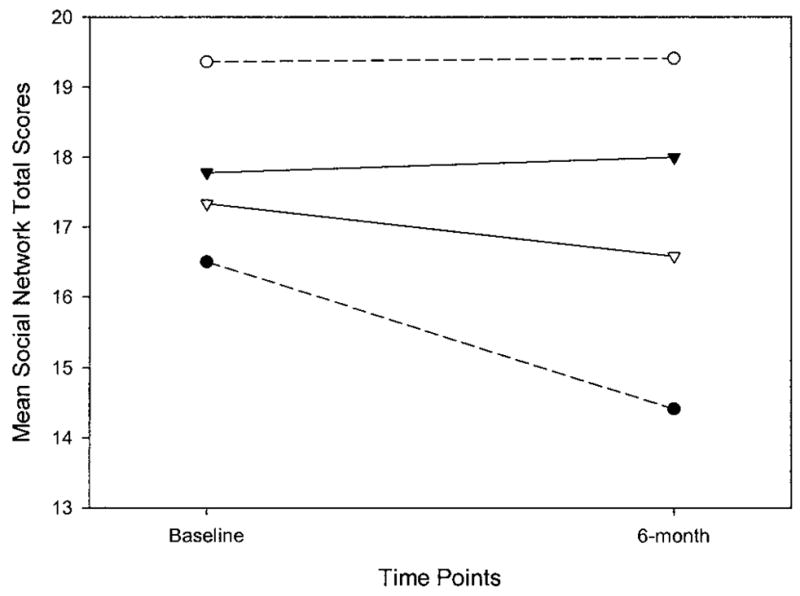
Mean social network scores on the Lubben Social Network Index: caregiver race by relationship interaction effect. —○— White Spouse; —●— Black Spouse; —▽— White Non-Spouse; —▼— Black Nonspouse.
Discussion
Through careful collection of TI data (Burgio et al., 2001), we showed that interventionists can apply multicomponent treatments accurately and that CGs are receptive to receiving up to eight home visits and two therapeutic phone calls over a 6-month period. CGs in the MSC group were somewhat less receptive to the brief phone contacts offering nonspecific support, with calls lasting approximately only 10 of the 15 scheduled min. Moreover, African Americans were significantly less receptive to the MSC phone contacts, with calls lasting an average of 2 fewer min in duration than those to Whites. Note that our treatment delivery data indicate that interventionists were equally accurate in delivering this intervention to African American and White caregivers; thus, this finding cannot be attributed to TI differences. Interventionists’ evaluations of treatment enactment suggest that 79% of the CGs showed moderate to good adherence to the skills training intervention. Notably, except for the racial difference found for duration of MSC phone contacts, our interventions, designed to be culturally sensitive, were applied and accepted similarly by African American and White CGs.
The outcome data show no change in distal outcomes of depression and anxiety over the 6-month period. Results do show significant therapeutic changes over time for three proximal targets of intervention: number of problem behaviors, average bother per behavior problem, and satisfaction with leisure activities. More specifically, CGs in both intervention groups reported significantly fewer problem behaviors, less behavioral bother, and an increase in satisfaction with leisure activities. Because of the absence of group differences, we do not know whether these therapeutic changes are related to participation in treatment or whether they are due to extraexperimental factors (e.g., regression to the mean or more experience in the CG role). However, studies that have used a no-treatment control group report either no change or worsening in number of problem behaviors and behavioral bother over similar time intervals (Ostwald et al., 1999; Quayhagan et al., 2000). Similarly, researchers have not reported therapeutic changes in leisure activities over time.
In addition, Goode, Haley, Roth, and Ford (1998) and Roth, Haley, Owen, Clay, and Goode (2001) studied White and African American dementia CGs in Birmingham by using many measures similar to those in the current project, and they found increased numbers of problem behaviors and no significant changes in appraisals or social activities over a 1-year period, further suggesting that the positive changes found in the present project are due to intervention and not the passage of time.
When race and relationship of CG were added to the analyses, an interesting pattern of results emerged. Figure 1 shows a treatment by race interaction for behavioral bother, with African American CGs in the more active STC group reporting less behavioral bother over time compared with White CGs in the STC and African Americans in the MSC. Figure 2 suggests that, for the number of problem behaviors, the differential treatment effects were most pronounced for spouse CGs. White spouse CGs in the MSC reported the largest decrease in number of problem behaviors; African American spouse CGs in the MSC actually reported an increase in problem behaviors.
On the basis of our clinical observations, we believe that African Americans were more responsive than Whites to the therapeutic relationship established in the one-on-one STC sessions. Although the psychotherapy literature clearly shows the importance of establishing a therapeutic alliance in achieving positive outcomes (Wampold et al., 1997), racial differences have not been examined. It is also possible that Whites were more willing or able to use the written information provided in the MSC, or they may have been more responsive to the brief non-specific support offered by phone. Our finding that the duration of phone contacts was significantly longer for Whites offers some support for this latter point. The hypothesis that Whites might have been more able to use written information is not supported by the finding of similar education levels for our White and African American CGs (M = 13.3 years, SD = 2.1 and M = 12.7 years, SD = 2.5, respectively).
Regarding the differential treatment effects for spouses and nonspouses, Schulz, O’Brien, Bookwala, and Fleissner (1995) suggest that spouse CGs provide greater levels of personal care and are more adversely affected by the caregiving experience than nonspouse CGs. Spouses might have the most to gain from an intervention they find to be helpful. Receiving an intervention not perceived to be therapeutic could add one more source of burden to an already burdensome situation. Data in Figure 1 show that White CGs are most responsive to the MSC; however, the MSC offered no therapeutic effects for African Americans. In this context, one would predict that White spouse CGs in the STC group—the individuals with the most to gain from a therapeutic intervention—would perceive the largest decrease in number of problem behaviors (Figure 2). Similarly, it is not surprising that African American spouse CGs in the MSC group—the individuals with the most to lose from receiving what was, for them, an ineffective intervention—perceived an increase in number of problem behaviors over time.
Our data also uncovered interesting main effects for race. Numerous studies have shown that African American CGs report more benefits or gains from the caregiving experience than Whites (Rapp & Chao, 2000). The African American CGs in our study reported a significant increase in positive aspects of caregiving over time, whereas Whites showed stable values. A possible interpretation is that, for African Americans, receiving an intervention can render the caregiving experience more positive and hopeful.
Prior research has also established that White CGs are more likely to place their impaired relatives in a nursing home than African Americans. A component of both of our interventions was to supply CGs with information to facilitate nursing home placement if they requested this information. Provision of this information might have resulted in a significant increase for Whites in the desire to institutionalize their relative over time. Any effects of this information on African Americans could have been suppressed by the strong cultural expectation against nursing home placement.
Finally, and unexpectedly, African American CGs reported a decrease in satisfaction with social support, with stability of White CGs over time. The results also showed a decrease in social network, but only for African American spouse caregivers. As already discussed, increasing social support was a direct aim of this study. Several previous longitudinal studies have shown significant declines in caregiver social networks and supports over time (Goode et al., 1998; Kiecolt-Glaser, Dura, Speicher, Task, & Glaser, 1991), suggesting that the stability found in White CGs may represent a preventive effect of the intervention for these CGs.
We believe that this home-based intervention can be administered with minimal modification through home health care agencies by either social workers or nurses. We are examining this strategy in an ongoing study utilizing social workers (MSWs), working through home health care agencies, to deliver a combined cognitive behavior therapy and problem-solving intervention to improve the quality of life of rural, medically fragile elders (Scogin, Kaufman, Burgio, Rohen, & Fisher, 2000).
A weakness of the current study was our inability to blind study personnel to group assignment. Maintaining blinding in psychosocial intervention trials is notoriously difficult because participants often spontaneously discuss their intervention experiences with assessors. In addition, intervention materials such as external memory aids and written instructions can be present in the home during assessment. Research has shown that even when attempts are made to blind assessors, 86% can accurately guess which participants have received active intervention in a randomized trial, but that only subjective assessor clinical rating measures (not used in this study) are affected by knowledge of group assignment (Carroll, Rounsaville, & Nich, 1994). Nevertheless, the issue of how to effectively blind assessors in studies of this type, and the impact of blinding on outcomes, deserves greater attention in future caregiver intervention studies.
In conclusion, our results suggest that both interventions, skills training (STC) and brief supportive phone calls plus written information (MSC), can reduce the number of problem behaviors and the bother associated with these problems; they can also increase satisfaction with leisure activities. Substantial prior research by the REACH team and other investigators indicates that none of these outcomes improve without intervention over a 6-month period of time.
However, the results suggest that the interventions were differentially effective based on these race and relationship factors. We believe that it is overly simplistic to think that interventions that are successful with CGs of one particular ethnic or cultural background would be equally effective with those from very different circumstances. Thus, the results of this study suggest the need to develop interventions with multiple components that are appropriately targeted to individuals who might benefit most from such interventions, with appropriate modifications made to maximize their relevance to subgroups of CGs based on relevant CG characteristics.
Acknowledgments
This project was funded by Grant NR04261 from the National Institute for Nursing Research to Louis Burgio and William Haley. We thank Susan Fisher, Debbie Turpin, and John Gerstle for assistance in manuscript preparation. Videotapes were provided to the caregivers through a special arrangement with Aspen Publishers and Ross Laboratories. We thank Aspen Publishers and Ross Laboratories for their generous support of the Alabama REACH Project.
Footnotes
Decision Editor: Laurence G. Branch, PhD
References
- Berkman LF, Syme SL. Social networks, host resistance, and mortality: A nine-year follow-up study of Alameda County residents. American Journal of Epidemiology. 1979;109:186–204. doi: 10.1093/oxfordjournals.aje.a112674. [DOI] [PubMed] [Google Scholar]
- Bourgeois MS, Schulz R, Burgio L. Intervention for caregivers of patients with Alzheimer’s disease: A review and analysis of content, process, and outcomes. International Journal of Human Development. 1996;43:35–92. doi: 10.2190/AN6L-6QBQ-76G0-0N9A. [DOI] [PubMed] [Google Scholar]
- Burgio L, Corcoran M, Lichstein KL, Nichols L, Czaja S, Gallagher-Thompson D, et al. Judging outcomes in psychosocial interventions for dementia caregivers: The problem of treatment implementation. The Gerontologist. 2001;41:481–489. doi: 10.1093/geront/41.4.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Rounsaville BJ, Nich C. Blind man’s bluff: Effectiveness and significance of psychotherapy and pharmacotherapy blinding procedures in a clinical trial. Journal of Consulting and Clinical Psychology. 1994;62:276–280. doi: 10.1037//0022-006x.62.2.276. [DOI] [PubMed] [Google Scholar]
- Dilworth-Anderson P, Williams IC, Gibson BE. Issues of race, ethnicity, and culture in caregiving research: A 20-year review (1980–2000) The Gerontologist. 2002;42:237–272. doi: 10.1093/geront/42.2.237. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. Mini-mental state: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Gallagher-Thompson D, Areán P, Menendez A, Takagi K, Haley WE, Arguelles T, et al. Development and implementation of intervention strategies for culturally diverse caregiving populations. In: Schulz R, editor. Handbook on dementia caregiving: Evidence-based interventions for family caregivers. New York: Springer; 2000. pp. 151–186. [Google Scholar]
- Goode KT, Haley WE, Roth DL, Ford GR. Predicting longitudinal changes in caregiver physical and mental health: A stress process model. Health Psychology. 1998;17:190–198. doi: 10.1037//0278-6133.17.2.190. [DOI] [PubMed] [Google Scholar]
- Haley WE, Levine EG, Brown SL, Bartolucci AA. Stress, appraisal, coping, and social support as predictors of adaptational outcome among dementia caregivers. Psychology and Aging. 1987;27:323–330. doi: 10.1037//0882-7974.2.4.323. [DOI] [PubMed] [Google Scholar]
- Haley WE, Roth DL, Coleton MI, Ford GR, West CAC, Collins RP, et al. Appraisal, coping, and social support as mediators of well-being in black and white family caregivers of patients with Alzheimer’s disease. Journal of Consulting and Clinical Psychology. 1996;64:121–129. doi: 10.1037//0022-006x.64.1.121. [DOI] [PubMed] [Google Scholar]
- Henderson JN, Gutierrez-Mayka M, Garcia J, Boyd S. A model for Alzheimer’s disease support group development in African American and Hispanic populations. The Gerontologist. 1993;33:409–414. doi: 10.1093/geront/33.3.409. [DOI] [PubMed] [Google Scholar]
- Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffee MW. Studies of illness in the aged. The index of ADL: A standardized measure of biological and psychosocial function. Journal of the American Medical Association. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Dura JR, Speicher CE, Task OJ, Glaser R. Spousal caregivers of dementia victims: Longitudinal changes in immunity and health. Psychosomatic Medicine. 1991;53:345–362. doi: 10.1097/00006842-199107000-00001. [DOI] [PubMed] [Google Scholar]
- Krause N. Negative interaction and satisfaction with social support among older adults. Journal of Gerontology: Psychological Sciences. 1995;50B:P59–P73. doi: 10.1093/geronb/50b.2.p59. [DOI] [PubMed] [Google Scholar]
- Krause N, Markides K. Measuring social support among older adults. International Journal of Aging and Human Development. 1990;30:37–53. doi: 10.2190/CY26-XCKW-WY1V-VGK3. [DOI] [PubMed] [Google Scholar]
- Lawton MP, Brody E. Assessment of older people: Self-maintaining and instrumental activities of daily living. The Gerontologist. 1969;9:179–186. [PubMed] [Google Scholar]
- Lichstein KL, Riedel BW, Grieve R. Fair tests of clinical trials: A treatment implementation model. Advances in Behaviour Research and Therapy. 1994;16(1):1–29. [Google Scholar]
- Lubben JE. Assessing social networks among elderly populations. Family and Community Health. 1988;11:42–52. [Google Scholar]
- Mittelman MS, Ferris SH, Shulman E, Steinberg G, Ambinder A, Mackell JA, et al. A comprehensive support program: Effect on depression in spouse-caregivers of AD patients. The Gerontologist. 1995;35:792–802. doi: 10.1093/geront/35.6.792. [DOI] [PubMed] [Google Scholar]
- Morycz RK. Caregiving strain and the desire to institutionalize family members with Alzheimer’s disease. Possible predictors and model development. Research on Aging. 1985;7:329–361. doi: 10.1177/0164027585007003002. [DOI] [PubMed] [Google Scholar]
- Nam CB, Terrie EW. 1980-based Nam-Powers Occupational Status scores, Working paper, Series 88-48) Tallahassee, FL: Florida State University, Center for the Study of Population; 1988. [Google Scholar]
- Ostwald S, Hepburn KW, Caron W, Burns T, Mantell R. Reducing caregiver burden: A randomized psychoeducational intervention for caregivers of persons with dementia. The Gerontologist. 1999;39:299–309. doi: 10.1093/geront/39.3.299. [DOI] [PubMed] [Google Scholar]
- Pruchno RA, Potashnik SL. Caregiving spouses: Physical and mental health in perspective. Journal of the American Geriatrics Society. 1989;37:697–705. doi: 10.1111/j.1532-5415.1989.tb02230.x. [DOI] [PubMed] [Google Scholar]
- Quayhagen MP, Quayhagen M, Corbeil RR, Hendrix RC, Jackson JE, Snyder L, et al. Coping with dementia: Evaluation of four nonpharmacologic interventions. International Psychogeriatrics. 2000;12(2):249–265. doi: 10.1017/s1041610200006360. [DOI] [PubMed] [Google Scholar]
- Radloff LS, Teri L. Use of the Center for Epidemiological Studies–Depression scale with older adults. In: Brink TL, editor. Clinical gerontology: A guide to assessment and intervention. New York: Hayworth Press; 1986. pp. 119–136. [Google Scholar]
- Rapp SR, Chao D. Appraisals of strain and of gain: Effects on psychological well being of caregivers of dementia patients. Aging & Mental Health. 2000;4:142–147. [Google Scholar]
- Roth DL, Haley WE, Owen JE, Clay OJ, Goode KT. Latent growth models of the longitudinal effects of dementia caregiving: A comparison of African-American and White family caregivers. Psychology and Aging. 2001;16:427–436. [PubMed] [Google Scholar]
- Schulz R, Gallagher-Thompson D, Haley W, Czaja S. Understanding the interventions process: A theoretical/conceptual framework for intervention approaches to caregiving. In: Schulz R, editor. Handbook of dementia caregiving. New York: Springer; 2000. pp. 33–60. [Google Scholar]
- Schulz R, O’Brien AT, Bookwala J, Fleissner K. Psychiatric and physical morbidity effects of dementia caregiving: Prevalence, correlates, and causes. The Gerontologist. 1995;35:771–791. doi: 10.1093/geront/35.6.771. [DOI] [PubMed] [Google Scholar]
- Scogin FR, Kaufman AV, Burgio LD, Rohen N, Fisher S. Quality of life and older rural health care recipients; 2000, November; Paper presented at the 53rd Annual Scientific Meeting of The Gerontological Society of America; Washington, DC. [Google Scholar]
- Spielberger CD. Manual for the State-Trait Anxiety Inventory (Form Y) Palo Alto, CA: Consulting Psychologists Press; 1983. [Google Scholar]
- Stevens AB, Arguelles S, Belle S, Coon D, Haley WE, Mendelsohn A, et al. Measurement of leisure time satisfaction in family caregivers, Unpublished manuscript. University of Alabama; Birmingham: 2001. [DOI] [PubMed] [Google Scholar]
- Tarlow B, Belle S, Wisniewski S, Ory M, Gallagher-Thompson D, Rubert M. Developing improved measures: Positive aspects of caregiving. Journal of Clinical Psychology (in press). [Google Scholar]
- Taves DR. Minimization: A new method of assigning patients to treatment and control groups. Clinical Pharmacology and Therapeutics. 1974;15:443–453. doi: 10.1002/cpt1974155443. [DOI] [PubMed] [Google Scholar]
- Teri L, Truax P, Logsdon R, Uomoto J, Zarit S, Vitaliano PP. Assessment of behavioral problems in dementia: The Revised Memory and Behavior Problems Checklist (RMBPC) Psychology and Aging. 1992;7:622–631. doi: 10.1037//0882-7974.7.4.622. [DOI] [PubMed] [Google Scholar]
- Wampold BE, Mondin GW, Moody M, Stich F, Benson K, Ahn H. A meta-analysis of outcome studies comparing bona fide psychotherapies: Empirically, “all must have prizes. Psychological Bulletin. 1997;122:203–215. [Google Scholar]
- Wisniewski SR, Belle SH, Coon DW, Marcus SM, Ory M, Schulz R. The Resources for Enhancing Alzheimer’s Caregiver Health (REACH) project design and baseline characteristics. Psychology and Aging. doi: 10.1037/0882-7974.18.3.375. (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarit SH, Stephens MAP, Townsend A, Greene R. Stress reduction for family caregivers: Effects of adult day care use. Journal of Gerontology: Social Sciences. 1998;53B:S267–S277. doi: 10.1093/geronb/53b.5.s267. [DOI] [PubMed] [Google Scholar]