Abstract
Objective:
To investigate whether longitudinal sleep duration patterns during early childhood is a risk factor of overweight or obesity at school entry while controlling for a variety of obesogenic environmental factors.
Design, Setting, and Participants:
This is a prospective cohort study (March–December 1998 to December 2004) of a representative sample of infants born in 1997–1998 in the Canadian province of Quebec. Body mass index (BMI) was measured at ages 2.5 and 6 years. Sleep duration was reported yearly from 2.5 to 6 years of age by their mothers. Prenatal, postnatal (5 and 29 months), and lifestyle (6 y) potentially confounding factors for excess weight were assessed by interviews, questionnaires and hospital records. A group-based semiparametric mixture model was used to estimate developmental patterns of sleep duration. The relationship between sleep duration patterns and BMI was tested using multivariate logistic regression models to control for potentially confounding factors on 1138 children.
Results:
Four sleep duration patterns were identified: short persistent (5.2%), short increasing (4.7%), 10-hour persistent (50.7%), and 11-hour persistent (39.4%). After controlling for potentially confounding factors, the risk for overweight or obesity was almost 4.2 times higher for short persistent sleepers (odds ratio [OR], 4.2; 95% confidence interval [CI], 1.6 to 11.1; P = 0.003) than for 11-hour persistent sleepers.
Conclusions:
Persistently short sleep duration (<10 h) during early childhood significantly increases the risk of excess weight or obesity in childhood, and appears to be independent of other obesogenic factors.
Citation:
Touchette E; Petit D; Tremblay RE; Boivin M; Falissard B; Genolini C; Montplaisir JY. Associations between sleep duration patterns and overweight/obesity at age 6. SLEEP 2008;31(11):1507–1514.
Keywords: Sleep duration, childhood, obesity, lifestyle, perinatal factors
CHILDHOOD OBESITY IS A PUBLIC HEALTH PROBLEM THAT IS SWEEPING THE WORLD, ESPECIALLY INDUSTRIAL COUNTRIES.1 A RECENT STUDY SHOWED THAT 10% to 15% of 2- to 5-year-olds are overweight in the United States.2 Furthermore, approximately 60% to 85% of obese children remain obese in adulthood.3 The major risk health problems of childhood obesity are cardiovascular disease (dyslipidemia, hypertension), endocrine dysfunction (type 2 diabetes, glucose intolerance, and insulin resistance) and pulmonary complications (obstructive sleep apnea syndrome, asthma, and exercise intolerance).1
Causes of the obesity are known to be multifactorial. A pediatric twin study suggests that 80% of the variation in body fat percentage and body mass index (BMI) is attributable to genetic factors.4 However, the rapid rise in obesity prevalence among genetically stable populations suggests that environmental factors should also be taken into account. It is recognized that prenatal factors, such as maternal diabetes, smoking during pregnancy, obesity or weight gain during pregnancy, birth weight of the child (as an outcome of intrauterine environment), might affect BMI in early childhood because the behaviors affecting energy balance develop early in life.5,6 In addition, sedentary lifestyles such as excessive television viewing or lack of physical activity contribute to the development of childhood obesity.7
There is growing evidence that sleep duration could be an additional factor. A comparison of 3 birth cohorts (1974,1979, and 1986) from 1 month to 16 years of age from the same Swiss population revealed that time spent in bed decreased (∼40 min) across cohorts particularly among young children.8 Also, an important 3.3-fold increase was observed in the prevalence of childhood (6–11 y) obesity between 1971–1974 and 1999.1 Previous cross-sectional studies have reported a link between short sleep duration and obesity in school-aged children.9–12 Chaput and coworkers (2006)12 found that the percentage of overweight and obese 5- to 10-year-old children was 3.5 times higher in children who slept 8 to 10 h (maternal report) than in children who slept for a total of 12 or 13 h, after adjusting for obesity risk factors such as parental obesity. Moreover, short nighttime sleep duration (<10.5 h) in children aged 30 months was one of 8 risk factors associated with increased obesity prevalence at the age of 7 y.11 However, these studies did not investigate sleep duration in a longitudinal manner.
The aim of our work was to investigate whether sleep duration is a risk factor of overweight or obesity in early childhood. This study has some notable strengths. First, and most importantly, sleep duration was determined by establishing longitudinal sleep duration patterns across early childhood rather than reporting sleep duration at a single point in time (which might not be representative of the entire childhood). Second, the large study sample permitted the simultaneous examination of a variety of potentially confounding factors.
METHODS
Data collection
This research was conducted as part as the Quebec Longitudinal Study of Child Development (started at March 1998), initiated by the Quebec Institute of Statistics. All children were recruited from the Quebec Master Birth Registry managed by the Ministry of Health and Social Services. A randomized 3-level stratified survey design was used to have a representative sample of children born from 1997 to 1998 in Quebec. The 3 levels were as follows: (1) geographical regions of Quebec, (2) each region subdivided into areas representative of the number of births in the region, and (3) number of children selected per area proportional to the number of births and the sex ratio of the area. Families living in the northern part of Quebec, Inuit territories, and First Nations reserves were excluded from the study for technical reasons.
Participants
A total of 2223 families thus participated in the initial study when children were approximately 5 months old (one child per family). Children were seen yearly thereafter until age 6 y. In total, 1492 families remained in the study until the children were 6 years old. The relationship between BMI and longitudinal sleep duration patterns was tested on 1138 children (23.7% of the sample at 6 y had missing data on either variable). Compared with the initial sample of 2223 children, the studied sample (n = 1138) had fewer boys (46.8% vs 51.2%; P = 0.02), fewer immigrant mothers (6.2% vs 11.7%; P = 0.001), and fewer families with insufficient income (26.9% vs 28.8%; P = 0.002); but the 2 samples did not differ on birth weight (3.4 ± 0.5 kg vs 3.4 ± 0.5 kg; P = 0.83), percentage of children with a low parental level of education (26.9% vs 28.8%; P = 0.27), or percentage of children living in a modified family structure (16.9% vs 19.0%; P = 0.15). All families received detailed information by mail on the aims and procedures of the Quebec Longitudinal study of Child Development and signed a consent form. The protocol was approved by a hospital-university ethics committee.
Outcome Measures
The most common and noninvasive measure of obesity, BMI (kg/m2) was used when the children were approximately 2.5 and 6 years old. Overweight and obesity were defined according to international standard definitions13 taking sex and age into account. Sleep duration was reported at 2.5, 3.5, 4, 5, and 6 years based on the last month by an open question from the Self-Administered Questionnaire for Mother: “Indicate how long in total your child sleeps during the night (on average). Do not count the hours that your child is awake.” The following potentially confounding prenatal and postnatal factors for excess weight were assessed:
Weight at birth, hospital record: continuous in kilograms
Prematurity (< 37 weeks), hospital record: yes/no14
Low birth weight (< 2.5 kg), hospital record: yes/no14
Sex of the child, hospital record: boys/girls2
Maternal smoking during pregnancy, interview: yes/no6
Weight at 5 months of age, interview: continuous in kilograms
Low parental education, interview: one or both parents without a high school diploma/both parents with at least a high school diploma15
Modified family status, interview: single parent or reconstructed family/intact15
Late age of cereals introduction, interview: after 4 months of age/before 4 months of age16
No breastfeeding at 5 months of age, questionnaire: never/previously breastfed17
Maternal immigrant status, interview: immigrant/non-immigrant.18
Napping at 2.5 years of age, questionnaire: no nap or nap ≤ 45 minutes/nap ≥ 1 h11
Weight at 2.5 years of age, interview: continuous in kilograms
The child's lifestyle variables assessed at 6 years were:
Watching TV during the week, interview: > 3 h daily/≤ 3 h7
Playing video games, interview: ≥ 1 h weekly/< 1 h19
Physical activity in last 12 months, interview: ≤ 1 time per month/≥ 1 time weekly7
Perception of child overeating, interview: sometimes or often/never or seldom20
Snacking between meals, interview: sometimes or often/never or seldom21
Eating sweets (eg. candies, pastries), interview: > 1 time a day/≤ 1 time a day22
Snoring, questionnaire: sometimes or often/never or seldom23
Inadequate income status, interview: inadequate/adequate based on 3 indicators: family income, family size, and regional area (postal code).18
Statistical Analyses
Although sleep duration is generally stable throughout childhood at approximately 10 to 11 h/night,24,25 this pattern may not be typical for all children. Rather than assume that all children follow the same developmental pattern of sleep duration over time, a semiparametric model was used to identify subgroups of children who followed different developmental trajectories for sleep duration.26 Briefly, trajectory methodology uses all available sleep duration data points and assigns individuals to trajectories based on a posterior probability rule. The identified groups represent approximations of an underlying continuous process. For each trajectory group, this probability measures the likelihood of an individual of belonging to that trajectory group based on observations across assessments. In other words, 100% classification accuracy is neither assumed nor required. Participants are assigned to the trajectory group to which they show the highest probability of belonging and analyses are weighted by posterior probabilities. A censored normal model was used; this model is considered appropriate for continuous data that are normally distributed, such as sleep duration. Trajectory models with 2 to 5 trajectories and varied shapes (e.g., intercept, linear, quadratic, or cubic) were compared by PROC TRAJ, an SAS procedure (SAS Institute Inc., Cary, NC).27 To choose the best model, the maximum Bayesian information criterion (BIC) was used to determine the optimal number of groups with shapes that best fit the data. This procedure allows the inclusion of cases with some missing data. Models with either zero, 1, or 2 missing data points for a given subject (over the 5 data points) were tested; the same results were obtained regardless of missing status. Therefore, we chose the model which permitted the inclusion of the greater number of subjects (with up to 2 missing data points).
Analyses were performed with SPSS for Windows (version 14; SPSS Inc, Chicago, ILL). The overweight and obese children were combined in the analyses and compared to those who were not overweight or obese. The association between overweight/obesity at 6 y and longitudinal sleep duration patterns was assessed by a logistic regression. The association between overweight/obesity at 2.5 y and short sleep duration (< 9 h) was assessed by a chi-square test. Chi-squared tests were used to test the relationships between potentially confounding variables and overweight/obesity at 6 y (expressed as odds ratios) and to examine the associations between potentially confounding variables and sleep duration pattern.
Standard logistic regressions were used to estimate the risk while controlling for a variety of obesogenic environmental factors (all potential confounding variables mentioned before without and with weight at 2.5 y). The statistical level to exclude factors from the model was set at P < 0.10. Final models considered factors as having a significant effect on overweight/obesity with a P value ≤ 0.05.
RESULTS
The study sample was composed of 93.8% of children whose mothers were non-immigrant Canadians and 6.2% whose mothers were first-generation immigrants. The majority of the sample was Caucasian (95.6%). Black Africans, American Indians, Arabs, and Asians represented 1.1%, 0.1%, 0.7%, and 1.0% of the sample, respectively. Most of the mothers (91.0%) spoke French during the interview; only 9.0% spoke English. A total of 9.1% of children were overweight and 4.7% were obese at age 6. The percentage of overweight/obesity was 14.7% and 12.8% in boys and girls, respectively. No relationship was found between sex of the child and BMI.
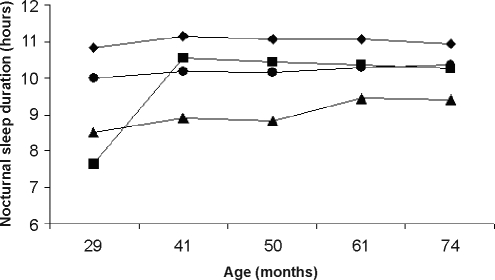
Our study of longitudinal patterns of sleep duration from ages 2.5 to 6 y identified 4 distinctive sleep patterns, illustrated in Figure 1: a short persistent pattern (5.2%) in which children slept < 10 h/night until age 6; a short increasing pattern (4.7%) in which children slept fewer hours in early childhood but increased nocturnal sleep duration at around 41 months and maintained it until 74 months of age; a 10-hour persistent pattern (50.7%) in which children slept persistently 10 h/night; and a 11-hour persistent pattern (39.4%) in which children slept persistently for 11 h/night. The 10-hour and 11-hour sleep patterns were stable from ages 2.5 to 6 y. Table 1 presents the mean sleep duration, standard deviation, and 10th and 90th percentiles for each of the 4 sleep patterns and each of the time points.
Figure 1.
Data courtesy of the Quebec Institute of Statistics. Patterns of sleep duration at 29, 41, 50, 61, and 74 months of age: ▲: short persistent sleepers (n = 59; 5.2%), ▪: short increasing sleepers (n = 54; 4.7%), •: 10-hour persistent sleepers (n = 577; 50.7%), and ♦: 11-hour persistent sleepers (n = 448; 39.4%).
Table 1.
Mean Sleep Duration, Standard Deviation and 10th and 90th Percentiles for Each Data Point in Each of the Four Sleep Patterns
| Short increasing | Short persistent | 10-hour persistent | 11-hour persistent | |
|---|---|---|---|---|
| 29 months | ||||
| Mean (SD) | 7.6 (0.9) | 8.4 (1.1) | 9.9 (0.8) | 10.8 (0.8) |
| 10th – 90th percentile | 6.0 – 8.0 | 7.0 – 10.0 | 9.0 – 11.0 | 10.0 – 12.0 |
| 41 months | ||||
| Mean | 10.5 (1.0) | 8.8 (1.0) | 10.1 (0.7) | 11.2 (0.7) |
| 10th – 90th percentile | 9.5 – 12.0 | 7.6 – 10.0 | 9.0 – 11.0 | 10.5 – 12.0 |
| 50 months | ||||
| Mean | 10.5 (0.9) | 8.9 (0.9) | 10.1 (0.7) | 11.1 (0.6) |
| 10th – 90th percentile | 9.5 – 12.0 | 8.0 – 10.0 | 9.0 – 11.0 | 10.5 – 12.0 |
| 61 months | ||||
| Mean | 10.2 (1.1) | 9.3 (0.9) | 10.2 (0.7) | 11.1 (0.6) |
| 10th – 90th percentile | 8.3 – 11.5 | 8.0 – 10.6 | 9.5 – 11.0 | 10.3 – 12.0 |
| 74 months | ||||
| Mean | 10.3 (0.9) | 9.3 (1.0) | 10.3 (0.7) | 11.0 (0.7) |
| 10th – 90th percentile | 9.0 – 11.0 | 8.0 – 10.4 | 9.5 – 11.0 | 10.0 – 12.0 |
Data courtesy of the Quebec Institute of Statistics.
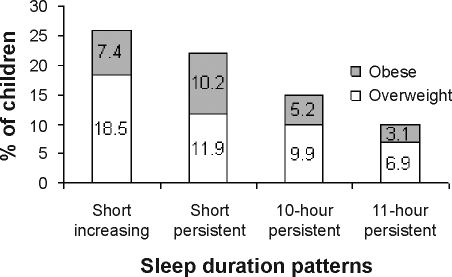
Figure 2 shows a significant difference in the distribution of BMI categories as a function of sleep duration pattern (P = 0.002). More precisely, we observed a greater percentage of overweight and obese children among the short persistent sleepers compared to the 11-hour persistent sleepers (22.1% versus 10.0%, OR: 3.9, CI: 1.7 to 8.8; P = 0.001). We also found a greater percentage of overweight and obese children among the short increasing sleepers compared to the children who slept for 11 h persistently during early childhood (25.9% versus 10.0%, OR: 3.2, CI: 1.4 to 7.6; P = 0.007).
Figure 2.
Data courtesy of the Quebec Institute of Statistics. Percentage of obese and overweight children as a function of longitudinal sleep duration patterns (normal: n = 979, overweight: n = 105, and obese: n = 54).
Since this last result supports the notion of an early effect of sleep, we sought to verify whether this relationship was present at 2.5 y. A significant relationship was found between overweight/obesity at 2.5 y and short sleep duration (< 9 h) at 2.5 y. More precisely, a higher percentage of overweight/obese children were found among those who slept < 9 h/night compared to those who slept ≥ 9 h (31.3% versus 24.7%, P = 0.05).
On one hand, several factors, such as weight at 5 months, maternal smoking during pregnancy, modified family status, low parental education, maternal immigrant status, birth weight, weight at 2.5 y, child overeating, low income status, and eating sweets were significantly associated with overweight/obesity at 6 y (Table 2a). On the other hand, several variables were significantly associated with sleep duration patterns and are presented in Table 2b.
Table 2a.
Odds Ratio (OR) and 95% Confidence Intervals (CI) of Different Potential Confounding Factors and Overweight/Obesity in a Sample (N=1138) of Children 6 Years of Age
| Potential confounding factors | Odds ratio of being overweight/obese |
# of missings | P | |
|---|---|---|---|---|
| OR | (95% CI) | |||
| Perinatal variables (birth or 5 months) | ||||
| Weight at 5 months, kg* | 1.42 | (1.20 – 1.67) | 13 | <0.001 |
| Maternal smoking during pregnancy | 1.83 | (1.28 – 2.63) | 6 | 0.001 |
| Family status - modified | 1.82 | (1.22 – 2.71) | 4 | 0.003 |
| Low parental education | 1.66 | (1.14 – 2.40) | 74 | 0.007 |
| Maternal immigrant status | 1.88 | (1.05 – 3.37) | 1 | 0.03 |
| Birth weight, kg* | 1.43 | (1.03 – 1.99) | 6 | 0.04 |
| Not breast-fed | 1.22 | (0.85 – 1.77) | 0 | 0.28 |
| Age cereals introduction - ≥ 4 months | 0.82 | (0.57 – 1.19) | 85 | 0.29 |
| Sex of the child - girl | 1.14 | (0.81 – 1.60) | 0 | 0.44 |
| Child variables (2.5 years) | ||||
| Weight at 2.5 years, kg* | 1.62 | (1.46 – 1.80) | 51 | <0.001 |
| Nap duration - ≤ 45 minutes | 1.35 | (0.79 – 2.32) | 55 | 0.28 |
| Lifestyle variables (6 years) | ||||
| Child overeating - sometimes/often | 7.13 | (4.85 – 10.48) | 28 | <0.001 |
| Income status - insufficient | 1.87 | (1.23 – 2.84) | 44 | 0.003 |
| Eating sweets - ≥ 2 times daily | 0.44 | (0.19 – 1.03) | 28 | 0.05 |
| Snacking - sometimes/often | 0.77 | (0.54 – 1.10) | 28 | 0.15 |
| Snoring - sometimes/often | 1.44 | (0.82 – 2.51) | 100 | 0.20 |
| Watching TV - ≥ 3 h daily | 1.57 | (0.67 – 3.65) | 28 | 0.30 |
| Doing physical activities - < 1 time monthly | 1.17 | (0.76 – 1.80) | 28 | 0.47 |
| Playing video games - ≥ 1 h weekly | 0.84 | (0.48 – 1.48) | 28 | 0.55 |
Data courtesy of the Quebec Institute of Statistics
signifies continous variables.
Table 2b.
Frequencies or Means of Different Potential Confounding Factors and Nocturnal Sleep Duration in a Sample (N=1138) of Children 6 Years of Age
| Prevalence (%) of sleep duration patterns |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Potential confounding factors | Short persistent n=59 (5.2%) |
Short increasing n=54 (4.7%) |
10-hour persistent n=577 (50.7%) |
11-hour persistent n=448 (39.4%) |
P | |||||
| Yes† | No† | Yes† | No† | Yes† | No† | Yes† | No† | |||
| Perinatal variables (birth or 5 months) | ||||||||||
| Maternal immigrant status | 14.1 | 4.6 | 8.5 | 4.5 | 59.2 | 50.2 | 18.3 | 40.7 | <0.001 | |
| Low parental education | 6.6 | 4.8 | 8.0 | 3.0 | 38.1 | 55.7 | 47.2 | 36.6 | <0.001 | |
| Family status - modified | 6.3 | 5.0 | 9.4 | 3.5 | 43.2 | 52.3 | 41.1 | 39.2 | 0.001 | |
| Maternal smoking during pregnancy | 3.3 | 5.8 | 5.2 | 4.4 | 44.3 | 52.8 | 47.2 | 36.9 | 0.01 | |
| Sex of the child - girl | 4.3 | 6.2 | 5.0 | 4.5 | 47.4 | 54.4 | 43.3 | 34.9 | 0.02 | |
| Age cereals introduction - ≥ 4 months | 5.2 | 5.2 | 4.0 | 5.7 | 56.0 | 47.0 | 34.8 | 42.1 | 0.03 | |
| Not breast-fed | 5.4 | 5.1 | 6.1 | 4.3 | 46.1 | 52.3 | 42.4 | 38.3 | 0.25 | |
| Weight at 5 months, kg* | 7.3 (0.9) | 7.2 (1.0) | 7.4 (1.0) | 7.3 (1.0) | 0.59 | |||||
| Birth weight, kg* | 3.3 (0.6) | 3.3 (0.6) | 3.4 (0.5) | 3.4 (0.5) | 0.69 | |||||
| Child variables (2.5 years) | ||||||||||
| Nap duration - ≤ 45 minutes | 1.0 | 5.0 | 6.9 | 4.7 | 34.7 | 53.1 | 57.4 | 37.3 | <0.001 | |
| Weight at 2.5 years, kg* | 13.8 (1.8) | 13.8 (2.0) | 13.9 (1.8) | 13.6 (1.7) | 0.05 | |||||
| Lifestyle variables (6 years) | ||||||||||
| Snacking - sometimes/often | 8.3 | 3.2 | 6.4 | 3.6 | 51.3 | 50.1 | 34.0 | 43.1 | <0.001 | |
| Playing video games - ≥ 1 h weekly | 12.2 | 4.3 | 3.3 | 4.9 | 53.7 | 50.2 | 30.9 | 40.7 | 0.001 | |
| Watching TV - ≥ 3 h daily | 14.3 | 4.8 | 11.4 | 4.5 | 31.4 | 51.2 | 42.9 | 39.5 | 0.007 | |
| Income status - insufficient | 5.8 | 5.1 | 9.7 | 3.8 | 43.9 | 51.6 | 40.6 | 39.6 | 0.008 | |
| Child overeating - sometimes/often | 7.1 | 4.8 | 6.4 | 4.4 | 53.8 | 50.0 | 32.7 | 40.8 | 0.17 | |
| Eating sweets - ≥ 2 times daily | 5.8 | 5.1 | 1.2 | 5.0 | 57.0 | 50.0 | 36.0 | 39.9 | 0.31 | |
| Snoring - sometimes/often | 7.6 | 5.1 | 5.4 | 4.3 | 52.2 | 50.8 | 34.8 | 39.7 | 0.62 | |
| Doing physical activities - < 1 time monthly | 5.5 | 5.0 | 6.0 | 4.4 | 50.3 | 50.6 | 38.2 | 40.0 | 0.77 | |
Data courtesy of the Quebec Institute of Statistics.
Percentages or means reported for each potential confounding factors associated with the description of the first column.
Signifies continuous variables.
The effect of sleep duration pattern on overweight/obesity remained significant after adjusting for confounding variables (Table 3). The risk of being overweight or obese was 4.2 times higher for short persistent sleepers (OR, 4.2; 95% CI, 1.6 to 11.1; P = 0.003) and 1.8 times higher for 10-h persistent sleepers (OR, 1.8; CI, 1.1 to 2.9; P = 0.03) than for 11-h persistent sleepers. Four other factors remained significant after a standard logistic regression: (1) perception of child overeating at 6 y, (2) weight at 5 months, (3) maternal smoking during pregnancy, and (4) being a girl. The risk of being overweight or obese at 6 y was almost 6-fold higher for children who were perceived as overeating (OR, 6.4; 95% CI, 3.9 to 10.5; P = 0.001), was 1.6 times higher for each kilogram gained at 5 months (OR, 1.6; 95% CI, 1.3 to 2.1; P = 0.001), was twice as high when mothers smoked during pregnancy (OR, 2.0; 95% CI, 1.2 to 3.3; P = 0.009) and was 1.8 times higher for girls (OR, 1.8; 95% CI, 1.1 to 2.9; P = 0.02).
Table 3.
Significant Risk Factors Associated with Overweight/Obesity in 6-Year-Old Children After Controlling for Obesogenic Variables in Logistic Regression Models
| Risk factors | OR* | (95% CI)* | P |
|---|---|---|---|
| Adjusted (without weight at 2.5 years of age)† | |||
| Sleep duration pattern - ref 11-hour persistent | |||
| Short increasing duration | 2.4 | (0.9 – 6.4) | 0.08 |
| Short persistent duration | 4.2 | (1.6 – 11.1) | 0.003 |
| 10-hour persistent duration | 1.8 | (1.1 – 2.9) | 0.03 |
| Being a girl | 1.8 | (1.1 – 2.9) | 0.02 |
| Maternal smoking during pregnancy | 2.0 | (1.2 – 3.3) | 0.009 |
| Weight at 5 months of age | 1.6 | (1.3 – 2.1) | <0.001 |
| Perception of child overeating sometime/often | 6.4 | (3.9 – 10.5) | <0.001 |
| N=846 | |||
| Adjusted (with weight at 2.5 years of age)† | |||
| Sleep duration pattern - ref 11-hour persistent | |||
| Short increasing duration | 1.9 | (0.6 – 5.6) | 0.24 |
| Short persistent duration | 2.9 | (1.0 – 8.5) | 0.05 |
| 10-hour persistent duration | 1.5 | (0.9 – 2.5) | 0.17 |
| Being a girl | 2.1 | (1.3 – 3.6) | 0.005 |
| Weight at 2.5 years of age | 1.6 | (1.4 – 1.9) | <0.001 |
| Perception of child overeating sometime/often | 4.9 | (2.9 – 8.4) | <0.001 |
| N=815 |
Data courtesy of the Quebec Institute of Statistics;
Data are given as odds ratio (OR) and 95% confidence interval (CI);
Adjusted on birth weight, prematurity, low birth weight, sex of the child, maternal smoking during pregnancy, weight at 5 months, low parental education, modified family structure, late cereal introduction, not breast-fed, immigrant mother, naptime at 2.5 years, watching TV at 6 years, playing video games at 6 years, doing physical activities, overeating at 6 years, snacking at 6 years, eating sweets at 6 years, snoring at 6 years, low income status at 6 years.
Even if a significant relationship was found between short sleep duration and overweight/obesity at 2.5 y already, the model was also tested with an adjustment for weight at 2.5 years. The association between short sleep duration and BMI at 6 y remains significant for the short persistent group (bottom half of Table 3).
Finally, to verify the assumption that child overeating may mediate the association between sleep time and obesity, the final model (adjusted for weight at 2.5 y) was also run without adjusting for overeating. Compared to the 11-h persistent pattern, the risk of being overweight or obese was 3.1 times greater (CI, 1.1 to 8.8; P = 0.03) in the short-persistent group (compared to 2.9 times when adjusted). There was still no significant risk of being overweight or obese in the short-increasing (OR: 2.2; CI, 0.8 to 6.1; P = 0.13) and the 10-h persistent (OR: 1.6; CI, 0.9 to 2.7; P = 0.08) groups when adjustment for overeating was removed. The small increase in the odds ratio for the short persistent group signifies that overeating (at 6 y) contributes a small role in the association between short sleep duration and BMI but would not be a major mediator of the effect.
DISCUSSION
To our knowledge, this is the first paper to investigate sleep duration longitudinally and relate it to BMI. It strongly suggests that persistently short sleepers during early childhood (sleeping < 10 h/night) are at greater risk for developing overweight or obesity compared to children who sleep ≥ 11 h/night, even after adjusting for a wide range of potentially confounding factors.
The overall prevalence of overweight/obesity in the present study (13.8%) is consistent with the 10% estimation made by the International Association for the Study of Obesity for school-age children.2 Among the variables studied, only sleep duration pattern, perception of child overeating at 6 y, weight at 5 months, maternal smoking during pregnancy, and being a girl remained significantly associated with being overweight/obese at 6 y. The association between perception of child overeating and overweight/obesity is likely bidirectional—both variables were measured at 6 y. This supports the findings of a prior study20 that reported a link between high maternal concern about child overeating and higher adiposity at 5 y. It had been shown that weight at 8 months was a predictor of the risk of obesity at 7 years of age.11 As previously demonstrated, maternal smoking during pregnancy increased the risk of obesity at school entry.6 Finally, a higher proportion of overweight and obese girls compared to boys has been reported previously in Canadian studies.12,28
More importantly, our results indicate that sleep duration was independently associated with overweight/obesity in early childhood. This study strongly suggests that sleeping less than 10 h persistently throughout early childhood significantly increases the risk of overweight/obesity. There is reason to believe that the effect of short sleep duration in infancy on body weight is already present at 2.5 years. In the present study, a significant relationship was found between short sleep duration (< 9 h) and overweight/obesity at 2.5 years. In addition, a longitudinal study recently demonstrated that short sleep duration in infancy (weighted mean of daily sleep at 6 months, 1 y, and 2 y) is a risk factor for overweight at 3 years of age.29 Nonetheless, when the present model was adjusted for weight at 2.5 y, the association between short sleep duration and BMI at years was still significant (albeit weaker) for the short persistent sleepers. This suggests that the effect of short sleep duration on BMI is probably cumulative over time.
The study also highlights the importance of correcting childhood sleep problems early. Although some effect of short sleep duration on weight could be seen at 2.5 y, the risk of being overweight or obese at 6 y was not significantly increased in the short increasing group who improved their sleep duration to approximately 10 h after 2.5 years. This means that correcting sleep problems early could not only prevent childhood obesity but also all related health consequences.
An emerging explanation is the potential role of metabolic hormones in the association between habitual short sleep duration and increased BMI. It is increasingly recognized that sleep affects the endocrine axes and metabolic pathways. Short sleep duration produces an increase in ghrelin levels, a peptide produced predominantly by the stomach that stimulates food intake and fat storage, along with a decrease in leptin levels, a hormone released by the adipocytes that provides information to hypothalamic centers about energy balance.30 This suggests that the combination of low leptin and high ghrelin is likely to stimulate the appetite, which in turn leads to weight gain. Another hypothesis, suggested by Locard and colleagues,9 is that longer sleep duration might increase the secretion of the growth hormone (GH) produced by the hypothalamo-pituitary-adrenocortical system during slow wave sleep (stages 3 and 4), thereby reducing the risk of overweight and obesity. These two mechanisms could be also connected, because ghrelin promotes both slow wave sleep and the release of GH. Schüssler and coworkers31 suggested that a slight increase in ghrelin is sleep promoting, whereas higher levels may disrupt sleep due to hunger. Controlled studies are needed to better understand the mechanisms underlying the sleep related regulation of the neuroendocrine control of appetite, specifically glucose metabolism, serotonin release involved in satiety, and hypocretin secretion.
The present study is limited by the reliance on a subjective measure of sleep duration, which may overestimate the true sleep time. Fortunately, many studies have shown high agreement between parental reports and actigraphy measures of sleep duration.32,33 Moreover, although a variety of potentially confounding variables were taken into account, the possibility remains that the relationship between sleep duration and obesity may be explained by other variables not considered here. For example, it could be a genetic phenomenon; a “program” that would trigger both the obesity and the short sleep duration. To that effect, it would have been interesting to consider parental BMI, but the data were unavailable. It could also be a hypothalamic dysfunction (hormonal or otherwise) that affects both sleep and satiety centers. One should also keep in mind that the subjects were generally non-immigrant French-speaking Caucasians, and the results should therefore be replicated in other populations.
This paper stresses the importance of giving the child the opportunity to sleep at least 10 h per night, as suggested by the National Sleep Foundation Poll, for optimal development in the cognitive sphere,34 behavioral expression,34 and physical fitness. Therefore, strong recommendations to get a good night's sleep, in addition to promoting more physical exercise, might be in order to tackle the epidemic problem of overweight and obesity. Future studies should assess the effects of sleep-promoting interventions on appetite and body weight.
DISCLOSURE STATEMENT
This was not an industry supported study. Dr. Montplaisir has received research support from Sanofi-Aventis, Jazz, and GlaxoSmithKline; has consulted for Pfizer and GlaxoSmithKline; and has participated in speaking engagements for Boehringer Ingelheim and Shire. Dr. Petit has participated as a sub-investigator in clinical trials sponsored by Orphan Medical, Jazz, GlaxoSmithKline, Sanofi-Aventis, and Aventis and has consulted for XenoPort. The other authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors wish to thank the children and families whose ongoing participation made this study possible. We acknowledge the considerable contribution of the coordinators of the Quebec Longitudinal Study of Child Development and the Quebec Institute of Statistics, and the tireless work of all the interviewers who assessed the mothers and children during the course of this study. We are thankful to Miguel Chagnon, PhD, for his valuable suggestions and statistical expertise.
Author Contributions
Study concept and design: Touchette, Petit, Boivin, Tremblay, Montplaisir.
Data acquisition: Quebec Institute of Statistics.
Data analysis and interpretation: Touchette, Petit.
Manuscript drafting: Touchette.
Critical manuscript revision for important intellectual content: Petit, Boivin, Tremblay, Falissard, Genolini, Montplaisir.
Statistical expertise: Touchette, Falissard, Genolini.
Fundraising: Touchette, Boivin, Tremblay, Montplaisir.
Administrative, technical, and material support: Public Health Network and the Quebec Institute of Statistics.
Study supervision: Quebec Institute of Statistics.
Funding/Support
This study was funded by the Ministry of Health and Social Services (Quebec City, Quebec, Canada); the Canadian Institutes of Health Research (Ottawa, Ontario, Canada); the Social Sciences and Humanities Research Council of Canada (Ottawa, Ontario, Canada); the Quebec Fund for Research on Society and Culture (Quebec City, Quebec, Canada); the Quebec Fund for Research on Nature and Technology (Quebec City, Quebec, Canada); the Health Research Fund of Quebec (Montreal, Quebec, Canada); the Molson Foundation (Montreal, Quebec, Canada); the Ministry of Research, Science and Technology (Quebec City, Quebec, Canada); Human Resources Development Canada (Ottawa, Ontario, Canada); the Canadian Institute for Advanced Research (Toronto, Ontario, Canada); Health Canada (Ottawa, Ontario, Canada); the National Science Foundation (Arlington, VA, USA); University of Montreal (Montreal, Quebec, Canada); Laval University (Quebec City, Quebec, Canada); and McGill University (Montreal, Quebec, Canada). Drs. Montplaisir and Tremblay hold a Canadian Government Chair on Sleep disorders and on Child development, respectively. The corresponding author had full access to all data in the study and had final responsibility for the decision to submit for publication.
REFERENCES
- 1.Ebbeling CB. Childhood obesity: public-health crisis, common sense cure. Lancet. 2002;360:473–82. doi: 10.1016/S0140-6736(02)09678-2. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–55. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 3.Kiess W, et al. Clinical aspects of obesity in childhood and adolescence. Obes Rev. 2001;2:29–36. doi: 10.1046/j.1467-789x.2001.00017.x. [DOI] [PubMed] [Google Scholar]
- 4.Faith MS. Evidence for independent genetic influences on fat mass and body mass index in a pediatric twin sample. Pediatrics. 1999;104:61–7. doi: 10.1542/peds.104.1.61. [DOI] [PubMed] [Google Scholar]
- 5.Whitaker R. Role of the prenatal environment in the development of obesity. J Pediatr. 1998;132:768–76. doi: 10.1016/s0022-3476(98)70302-6. [DOI] [PubMed] [Google Scholar]
- 6.Al Mamun A. Does maternal smoking during pregnancy have a direct effect on future offspring obesity? Evidence from a prospective birth cohort study. Am J Epidemiol. 2006;164:317–25. doi: 10.1093/aje/kwj209. [DOI] [PubMed] [Google Scholar]
- 7.Anderson RE. Relationship of physical activity and television watching with body weight and level of fatness among children: results from the Third National Health and Nutrition Examination Survey. JAMA. 1998;279:938–42. doi: 10.1001/jama.279.12.938. [DOI] [PubMed] [Google Scholar]
- 8.Iglowstein I. Sleep duration from infancy to adolescence: reference values and generational trends. Pediatrics. 2003;111:302–7. doi: 10.1542/peds.111.2.302. [DOI] [PubMed] [Google Scholar]
- 9.Locard E. Risk factors of obesity in a five year old population. Parental versus environmental factors. Int J Obes. 1992;16:721–9. [PubMed] [Google Scholar]
- 10.von Kries R. Reduced risk for overweight and obesity in 5- and 6-y-old children by duration of sleep – a cross-sectional study. Int J Obes Relat Metab Disord. 2002;26:710–16. doi: 10.1038/sj.ijo.0801980. [DOI] [PubMed] [Google Scholar]
- 11.Reilly JJ, et al. Avon Longitudinal Study of Parents and Children Study Team. Early life risk factors for obesity in childhood: cohort study. BMJ. 2005;330:1357. doi: 10.1136/bmj.38470.670903.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chaput JP. Relationship between short sleeping hours and childhood overweight/obesity: results from the “Québec en Forme” Project. Int J Obes (Lond) 2006;30:1080–5. doi: 10.1038/sj.ijo.0803291. [DOI] [PubMed] [Google Scholar]
- 13.Cole TJ. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320:1240–3. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mericq V. Prematurity and insulin sensitivity. Horm Res. 2006;65:131–6. doi: 10.1159/000091518. [DOI] [PubMed] [Google Scholar]
- 15.Strauss RS. Influence of the home environment on the development of obesity in children. Pediatrics. 1999;103:e85. doi: 10.1542/peds.103.6.e85. [DOI] [PubMed] [Google Scholar]
- 16.Agras WS. Influence of early feeding style on adiposity at 6 years of age. J Pediatr. 1990;116:805–9. doi: 10.1016/s0022-3476(05)82677-0. [DOI] [PubMed] [Google Scholar]
- 17.von Kries R, et al. Breast feeding and obesity: cross sectional study. BMJ. 1999;319:147–50. doi: 10.1136/bmj.319.7203.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Whitaker RC. Obesity among US urban preschool children: relationships to race, ethnicity, and socioeconomic status. Arch Pediatr Adolesc Med. 2006;160:578–84. doi: 10.1001/archpedi.160.6.578. [DOI] [PubMed] [Google Scholar]
- 19.Stettler N. Electronic games and environmental factors associated with childhood obesity in Switzerland. Obes Res. 2004;12:896–903. doi: 10.1038/oby.2004.109. [DOI] [PubMed] [Google Scholar]
- 20.Burdette HL. Maternal infant-feeding style and children's adiposity at 5 years of age. Arch Pediatr Adolesc Med. 2006;160:513–20. doi: 10.1001/archpedi.160.5.513. [DOI] [PubMed] [Google Scholar]
- 21.O'Brien T. Naturalistic observation of the snack-selecting behavior of obese and nonobese children. Addict Behav. 1982;7:75–7. doi: 10.1016/0306-4603(82)90028-4. [DOI] [PubMed] [Google Scholar]
- 22.Brekke HK. Predictors and dietary consequences of frequent intake of high-sugar, low-nutrient foods in 1-year-old children participating in the ABIS study. Br J Nutr. 2007;97:176–81. doi: 10.1017/S0007114507244460. [DOI] [PubMed] [Google Scholar]
- 23.Redline S. Risk factors for sleep-disordered breathing in children: associations with obesity, race, and respiratory problems. Am J Respir Crit Care Med. 1999;159:1527–32. doi: 10.1164/ajrccm.159.5.9809079. [DOI] [PubMed] [Google Scholar]
- 24.Thorleifsdottir B. Sleep and sleep habits from childhood to young adulthood over a 10-year period. J Psychosom Res. 2002;53:529–37. doi: 10.1016/s0022-3999(02)00444-0. [DOI] [PubMed] [Google Scholar]
- 25.Spruyt K. Odds, prevalence and predictors of sleep problems in school-age normal children. J Sleep Res. 2005;14:163–76. doi: 10.1111/j.1365-2869.2005.00458.x. [DOI] [PubMed] [Google Scholar]
- 26.Nagin DS. Cambridge, MA: Harvard University Press; 2005. Group based modeling of development. [Google Scholar]
- 27.Jones BL. A SAS procedure based on mixture models for estimating developmental trajectories. Sociol Methods Res. 2001;29:374–93. [Google Scholar]
- 28.Young TK. Childhood obesity in a population at high risk for type 2 diabetes. J Pediatr. 2000;136:365–9. doi: 10.1067/mpd.2000.103504. [DOI] [PubMed] [Google Scholar]
- 29.Taveras EM. Short sleep duration in infancy and risk of childhood overweight. Arch Pediatr Adolesc Med. 2008;162:305–11. doi: 10.1001/archpedi.162.4.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Taheri S. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;1:e62. doi: 10.1371/journal.pmed.0010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schüssler P, et al. Nocturnal ghrelin, ACTH, GH and cortisol secretion after sleep deprivation in humans. Psychoneuroendocrinology. 2006;31:915–923. doi: 10.1016/j.psyneuen.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 32.Sadeh A. Assessment of intervention for infant night waking: Parental reports and activity-based home monitoring. J Consult Clin Psychol. 1994;62:63–8. doi: 10.1037//0022-006x.62.1.63. [DOI] [PubMed] [Google Scholar]
- 33.Sekine M. The validity of sleeping hours of healthy young children as reported by their parents. J Epidemiol. 2002;12:237–42. doi: 10.2188/jea.12.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Touchette E. Associations between sleep duration patterns and behavioral/cognitive functioning at school entry. Sleep. 2007;30:1213–9. doi: 10.1093/sleep/30.9.1213. [DOI] [PMC free article] [PubMed] [Google Scholar]