Abstract
Study Objectives:
The aim of this study was to examine the correlates associated with short nocturnal sleep duration and subjective insomnia, including individual factors, family factors, peer factors, school factors, and the problematic use of high-tech devices among a large-scale representative population of Taiwanese adolescents.
Design:
Cross-sectional study.
Setting:
A total of 23 junior high and 29 senior high/vocational schools were randomly selected across southern Taiwan.
Participants:
Eight thousand four adolescent students.
Interventions:
N/A.
Measurements and Results:
The multidimensional correlates associated with short nocturnal sleep duration and subjective insomnia were examined using χ2 automatic interaction detection analysis and logistic regression analysis models. The results indicated that an older age, self-reported depression, being in the third year of school, drinking coffee at night, and problematic Internet use were significantly associated with short nocturnal sleep duration in adolescents. Furthermore, self-reported depression, low school affinity, high family conflict, low connectedness to their peer group, and problematic Internet use were associated with subjective insomnia in adolescents.
Conclusions:
The results of this study indicate that a variety of individual, family, peer, and school factors were associated with short nocturnal sleep duration and subjective insomnia in adolescents. Furthermore, the correlates of short sleep duration were not identical to those of subjective insomnia. Parents and health professionals should be wary of sleep patterns among adolescents who have the identified correlates of short nocturnal sleep duration and subjective insomnia.
Citation:
Yen CF; Ko CH; Yen JY; Cheng CP. The multidimensional correlates associated with short nocturnal sleep duration and subjective insomnia among Taiwanese adolescents. SLEEP 2008;31(11):1515–1525.
Keywords: Adolescent, sleep, insomnia, depression
RESEARCH HAS FOUND THAT ADOLESCENTS FREQUENTLY OBTAIN INSUFFICIENT SLEEP.1 SHORT SLEEP DURATION AND INSOMNIA HAVE BEEN FOUND to impair youths' daytime memory, to reduce cognitive and behavioral functioning,2 to be associated with poor health status,3 and to increase the risk of motor vehicle accident,4 suicide,5 substance use,6 and behavior problems.7 Despite the inherent importance of sleep, there is limited information available on the epidemiology of sleep behavior and sleep disturbance among youths.8 Adolescent development is the result of multisystem interactions,9 and, therefore, investigation of the multidimensional correlates associated with short sleep duration and insomnia among adolescents is a fundamental step toward identifying risk groups, which will allow prevention and intervention.
Among the individual correlates of sleep in adolescents, increased age has been found to be associated with decreased total sleep duration10,11 and increased sleep complaints.12 Low socioeconomic status (SES) has also found to be associated with short sleep duration and insomnia in children.11,13,14 However, the association of other individual factors with short sleep duration and insomnia needs further study. For example, the results of studies on sex differences in sleep duration3,11,15,16 and sleep quality16–18 among adolescents are still inconclusive. Up to the present, very limited studies on the influence of residential background on adolescent sleep exist.3
Depressed mood,1 employment,11 and drinking coffee19 have been found to be associated with short sleep duration or preferring an evening type of sleep in adolescents. Meanwhile, several studies on children have found that short sleep duration increases the risk for being overweight or obese.20 However, compared with studies on children, fewer studies have examined the association between sleep and weight status in adolescents, and the findings are inconsistent.3,21,22 Further studies are needed to examine whether increased body weight is a consistent indicator of short sleep duration and insomnia in adolescents.
Of the constellation of forces that influence adolescent health, the most fundamental are the social context in which adolescents are embedded;23 specifically the family, peer and school contexts are among the most critical. Most adolescents live in a family environment. Recent studies indicate that later bedtimes among teenagers may result from decreased parental enforcement,6,15 which indicate that failing to set limits on an adolescent's bedtime may put them at risk of sleep phase delay and its consequences.19 Family adversity, such as high family conflict and family member substance use, have been suggested as potential causes related to the development of psychopathology amongst adolescents.24 However, their associations with short sleep duration and insomnia in adolescents have not been systemically examined.
Peers also serve as important and influential figures for adolescents.25 Engagement in social activities with their peer group has been hypothesized to partially account for the association between increased age and short sleep duration.1 It seems reasonable to hypothesize that adolescents who have high connectedness to peers and spend more time with peers may be more likely to report short sleep duration. However, to our knowledge, no empirical study has examined this hypothesis.
School is another important environment for adolescents. Previous studies have revealed that adolescents in higher grade levels are more likely than those in lower grade levels to be classified as the “evening type” with respect to sleep-wake patterns.19,26 In Taiwan, compulsory fundamental education currently comprises 6 years of elementary school and 3 years of junior-high education. Upon completion of these 9 years, nearly all students take a national entrance examination for a senior high or vocational school. Then they take another national entrance examination for university after completion of 3 years of study in senior high school.27 Thus, students in both the third year of junior high and the third year of senior high school are involved in a highly stressful period of study. Whether adolescents in the third year of junior or senior high school have shorter sleep duration and more severe insomnia than those in other grades needs further study. At the same time, short sleep duration and insomnia are known to have a bidirectional relationships with low school achievement and high rates of absenteeism.16,28 However, it has not been ascertained whether the relationship remains significant when a variety of individual and psychosocial contexts are examined together.
Computer use and cellular phone use are 2 of the most popular high-tech devices used by adolescents.29 The Internet provides opportunities for the user to chat with others, to participate in Internet activities, to compete with others in online gaming, and to search for the information that people want and, compared with general computer use, has very few limitations. These characteristics of the Internet make Internet use one of the central themes of computer use among adolescents. Problematic Internet use is a maladaptive pattern of Internet use that can result in a negative impact on Internet users, which includes problems related to daily routine, school performance, and family relationships.30 A previous study in Taiwan has found that 19.8% of adolescents have problematic Internet use.30 It has been hypothesized that increased computer and cell phone use may be associated with short sleep duration and sleep disturbance.31 However, although some studies have found excessive computer use to be associated with shortened sleep duration11,31 and sleep disturbance in adolescents,32 other studies have not found such an association3 or found that the association exists only in males.33 Very few studies have examined the association between intensive computer use and sleep problems in adolescents.29 Previous studies have measured the duration or frequency of computer use, which may not represent the real severity of the negative influences of problematic computer use on adolescents' lives.
The aim of this study was to examine the multidimensional correlates related to short nocturnal sleep duration and subjective insomnia in a large-scale representative population of Taiwanese adolescents. The correlations of the individual (sociodemographic characteristics, self-reported depression, part-time job, drinking coffee, and body weight), family (family conflict, family monitoring, and substance use of family members), peer (connectedness to peer group and time spent with friends), school factors (grade, school affinity, and academic achievement) and problematic use of high-tech devices (problematic Internet and cell phone use) with short nocturnal sleep duration and subjective insomnia were examined.
METHODS
The current investigation was based on data from the Project for the Health of Adolescents in Southern Taiwan, which was composed of data collected from 3 metropolitan cities and 4 counties. In 2004, there were 257,873 adolescent students in 209 junior high schools and 202,456 adolescent students in 140 senior high/vocational schools in this area. Based on the definitions of urban and rural districts in the Taiwan Demographic Fact Book34 together with school and grade characteristics, a stratified random sampling strategy was used with the final goal of ensuring that there was proportional representation of districts, schools, and grades. Twelve junior high and 19 senior high/vocational schools were randomly selected from urban districts; likewise, 11 junior high and 10 senior high/vocational schools were randomly selected from rural districts. The classes of these schools were further stratified into 3 levels based on grades in both the junior high and senior high/vocational schools. Then, 207 classes that contained a total of 12,210 adolescent students were randomly selected based on the ratio of students in each grade.
Research assistants explained the purpose and procedure of this study to the students in class, emphasizing respect for their privacy, and encouraged them to participate. Written informed consents were obtained from the adolescents before the study started, and the participants were then invited to complete the research questionnaires anonymously in the classrooms. The protocol was approved by the Institutional Review Board of Kaohsiung Medical University. We also recruited 76 adolescents (40 junior high school students and 36 senior high school students) and their parents into a pilot study to examine the 2-week test-retest reliability of all research instruments (except for the questionnaire on problematic Internet use) and the validity of sleep duration and problematic cell phone use assessments.
Assessment
Sleep Duration and Insomnia
In this study, we collected self-reported data on sleep duration at night and the severity of insomnia problems. The participants were asked: “How many hours of sleep on average have you usually obtained every night over the last month?” which would represent their habitual nocturnal sleep duration. The 2-week test-retest reliability (Pearson correlation r) was 0.72, and correlation between the self-report and the parents' report for the duration of nocturnal sleep (Pearson correlations r) was 0.69 (P < 0.001). Considering 1 standard deviation (SD) below the mean of sleep duration in all participants, we defined total nocturnal sleep duration below the 15th percentile of all participants in this study as short nocturnal sleep duration. We also used the 8-item Athens Insomnia Scale (AIS-8) to assess the severity of subjective insomnia over the last month.35 The first 5 items of the AIS-8 assess difficulty with sleep induction, awakening during the night, early morning awakening, total sleep time, and overall quality of sleep. The last 3 items assessed the next-day consequences of any insomnia, including problems with sense of well-being, functioning, and sleepiness during the day. The items of the AIS-8 correspond with the taxonomies for the diagnosis of insomnia according to International Classification of Diseases-10.36 Each item of the AIS-8 can be rated from 0 to 3, and higher total scores indicate more severe insomnia. The Cronbach α in the present study was 0.67, and the 2-week test-retest reliability was 0.72 (P < 0.001). There is a lack of a cutoff point for diagnosing adolescent insomnia, and, therefore, we defined adolescents whose total AIS-8 score was above the 85th percentile of the population in this study as those with subjective insomnia.
Depression
We used the 20-item Mandarin-Chinese version37 of the Center for Epidemiological Studies' Depression Scale (CES-D)38 to assess the frequency of depressive symptoms in the preceding week. The Cronbach α for the CES-D in the present study was 0.93, and the 2-week test-retest reliability was 0.78. Based on the result of a previous study using the CES-D in a 2-phase survey for depressive disorders among nonreferred adolescents in Taiwan,39 we defined those participants whose total CES-D score was higher than 28 as having self-reported depression. One item in the CES-D inquired about the participants' sleep disturbance; we excluded this item and summed the scores of the other 19 items for analysis. Using the method of linear equating,40, we established a cutoff of 27.11 for the 19-item CES-D on self-reported depression linked to the original cutoff of 28 on the 20-item CES-D. The consistency between the cutoffs on the 19-item and 20-item CES-D was high (κ = 0.961).
Adolescent Family and Social Life Questionnaire
We adapted subscales of the Adolescent Family and Social Life Questionnaire (AFSLQ) to assess the levels of family conflict (3 items), family monitoring (4 items), and subjective perception with respect to the peer group (4 items).41 For example, the family conflict subscale contains 3 items, namely “I conflict with my family members frequently,” “My family members conflict with each other frequently,” and “It is distressing to be home.” Participants scored the items on a 4-point Likert scale, with a higher score indicating more agreement with the statements. The Cronbach α ranged from 0.68 to 0.74, and the 2-week test-retest reliability ranged from 0.64 to 0.71. Higher scores on these 3 items of the AFSLQ indicate greater family conflict, low family monitoring, and low connectedness to the peer group. The AFSLQ also assessed habitual alcohol consumption (alcohol consumption 3 or more times per week) and illicit drug use among parents and siblings, as well as the total hours that the adolescents spent keeping company with friends after school during a week.
Characteristics of School Life
Participants' level of connectedness to school was assessed by 4 questions, namely “I do not enjoy my school life,” “I do not get along well with my teachers,” “I do not get along well with my schoolmates,” and “I skip my classes as much as possible.” Participants scored the items on a 4-point Likert scale, with a higher score indicating more agreement with the statements. The Cronbach α was 0.62, and the 2-week test-retest reliability was 0.69. A high total score indicates low school affinity. The participants' grade (in the first and second years compared with in the third year of the junior or senior high school) and academic achievement (the first two-thirds vs last one-third ranked against their classmates according to the academic performance of the recent semester) were also collected.
High-Tech Device Use
In this study, we collected data on problematic Internet and cell phone use. We used the Chen Internet Addiction Scale (CIAS) to assess the level of problematic Internet use.42 The CIAS contains 26 items on a 4-point Likert scale that assesses Internet-related problems, including symptoms of compulsive use, withdrawal, tolerance, problems in interpersonal relationships, and problems in health and time management.42 The internal reliability of the scale and the subscales ranges from 0.79 to 0.93.42 We developed a diagnostic criterion for Internet addiction that was defined as a subject having 6 or more symptoms of the 9 criteria, including preoccupation, uncontrolled impulse, usage more than intended, tolerance, withdrawal, impairment of control, excessive time and effort spent on the Internet, impairment of decision-making ability, and impaired function.30 According to the diagnostic criteria of Internet addiction, we found the 63/64 cutoff point of the CIAS to have the highest diagnostic accuracy, sensitivity, and specificity.43 Furthermore, we developed a self-administered 12-item Problematic Cellular Phone Use Questionnaire (PCPU-Q) based on the same structure as the substance use dependence subscale found in the DSM-IV-TR44 to determine the occurrence of symptoms of problematic cell phone use. The first 7 questions inquired of participants whether they had the symptoms of problematic cell phone use in the preceding year including increasing the frequency and duration of cell phone use to achieve satisfaction; feeling uncomfortable if no cellular phone can be used; using the cellular phone for a period of time longer or more frequently than intended; persistent desire and/or unsuccessful attempts to cut down or reduce cell phone use; excessive time or effort spent on using or gaining a cellular phone; giving up or reducing important social, academic or recreational activities because of cell phone use; and continuing heavy cell phone use despite knowledge of physical or psychological problems caused by cell phone use. The last 5 questions ascertained participants' subjective functional impairment in the preceding year caused by cell phone use, including compromised academic performance, relationships with classmates and friends, relationships with parents and siblings, physical or psychological health, and having legal problems. An answer of “yes” to the question indicated that participants reported that they had that symptom of problematic cell phone use or a functional impairment caused by cell phone use. The Cronbach α for the 7 symptoms was 0.85, the 2-week test-retest reliability (κ) ranged from 0.41 to 0.78 (P < 0.001), and the κ between participants' self-reports and their parents' reports ranged from 0.26 (P < 0.05) to 0.44 (P < 0.001). The Cohen κ value of 3/4 cutoff point was 0.463, which was higher than that of cutoff 2/3 (0.446) and 4/5 (0.456). It indicated that 3/4 cutoff point had the highest potential to differentiate adolescents with functional impairment caused by problematic cell phone use from those not so affected.
Individual Characteristics
Participants' sex, age (< 15 years old vs ≥ 15 years old), residential background (urban vs rural), and SES were collected. In this study, we used parental education level to represent adolescents' high SES (parental education level > 9 years of compulsory fundamental education) and low SES (parental education level ≤ 9 years of compulsory fundamental education). Participants' body mass index (weight in kilograms/height in meters squared) was calculated from their self-reported weight and height measurements. We also inquired as to whether the participants had a part-time job and whether they drank coffee to reinvigorate themselves at night.
Procedure and Statistical Analysis
The adolescents were asked to anonymously complete the questionnaire after the explanation by the research assistants and under their direction. All students received a gift that was worth 33 NT dollars (1 US dollar) at the end of the assessment. Two different statistical methods were used to analyze the discriminating factors of short nocturnal sleep duration and subjective insomnia in adolescents. First, CHAID analysis using the Answer Tree 3.1 software45 was used to detect mutually exclusive subgroups of the sample that differed markedly in regard to short nocturnal sleep duration and subjective insomnia. The analysis selected the best predictors of the outcome and divided the sample into subgroups based on that variable while merging nonsignificant categories. This process was repeated within each subgroup until no further predictors could significantly contribute to the analysis. Compared with logistic regression analysis, CHAID analysis directly considers the interaction between variables. The continuous variables were transformed into dichotomous variables by their median scores. Since this is an exploratory procedure, we investigated the replicability of the resulting subgroup categories by conducting the analysis on half of the sample (calibration sample) and then examining the reproducibility using the remaining half of the sample (cross-validation sample).46 Second, we used fully entered logistic regression analysis models to confirm the significant correlates identified by the CHAID analysis, the effects of interactions between the significant correlates, and possible discriminating factors that were not identified in the CHAID analysis in the cross-validation sample.46 A 2-tailed P value of less than 0.05 was considered statistically significant. In addition, we used the odds ratio (OR) to estimate the effect of size on the logistic regression analysis. According to Chinn,47 we defined OR values higher than 1.5, 2.5, and 4 or lower than 0.667, 0.4, and 0.25 as having small, medium, and large effects, respectively. An OR that was between 0.667 and 1.5 was not considered to be significant.
RESULTS
A total of 11,111 (91.0%) adolescents returned their written informed consents. Of them, 8004 (72.0%) participants completed all research questionnaires without omission. Those who had missing data in the questionnaires were more likely to be male (χ2 = 54.039, P < 0.001) and from junior high schools (χ2 = 95.487, P < 0.001). The characteristics of sleep, individual, family, peer and school life, depression, and high-tech device use of the 8004 participants who completed all the research questionnaires are shown in Table 1. The mean age was 14.7 years (SD: 1.7 years, range: 12 to 18 years). Their mean nocturnal sleep duration at night was 6.8 hours (SD: 1.3 hours), and the 15th percentile of nocturnal sleep duration was 6 hours. According to the definitions described above, 1047 participants (13.1%) were classified as short nocturnal sleepers. Meanwhile, the mean total score of the AIS-8 was 6.9 (SD: 3.2), and the 85th percentile of the AIS-8 scores was 10. A total of 943 participants (11.8%) were classified as having subjective insomnia.
Table 1.
Adolescent Self-Reported Sleep Pattern, Individual Factors, Family Factors, Peer Factors, School Factors, and Levels of High-Tech Device Use
| No. (%) | Mean (SD) | |
|---|---|---|
| Sleep characteristics | ||
| Short sleep duration (sleep duration < 6 hours) | 1047 (13.1) | |
| Subjective insomnia (AIS-8 score>10) | 943 (11.8) | |
| Individual characteristics | ||
| Male | 3829 (47.8) | |
| Age ≥ 15 years | 4132 (51.6) | |
| Living in a rural area | 3230 (40.4) | |
| Paternal education ≤ 9 years | 2634 (32.9) | |
| Maternal education ≤ 9 years | 3136 (39.2) | |
| Self-reported depression (CES-D score > 27.11) | 979 (12.2) | |
| Having a part-time job | 1544 (19.3) | |
| Drinking coffee | 1288 (16.1) | |
| BMI | 20.8 (3.9) | |
| Family characteristics | ||
| High family conflict | 1.9 (0.5) | |
| Low family monitoring | 1.7 (0.6) | |
| Substance use by family members | 2018 (25.2) | |
| Peer characteristics | ||
| Low connectedness to peer group | 1.8 (0.5) | |
| Time spent with friends (hours) | 10.9 (18.2) | |
| School characteristics | ||
| Low school affinity | 1.8 (0.4) | |
| In the third year of junior or senior high school | 1981 (24.8) | |
| Low academic achievement | 1865 (23.3) | |
| High-tech device use | ||
| Problematic Internet use (CIAS score ≥ 64) | 889 (11.1) | |
| Problematic cellular phone use (symptoms of cellular phone use on the PCPUQ ≥ 4) | 989 (12.4) |
Abbreviations: AIS-8 refers to the Athens Insomnia Scale; CES-D, the Center for Epidemiological Studies-Depression Scale; CIAS, the Chen Internet Addiction Scale; PCPUQ, the Problematic Cellular Phone Use Questionnaire.
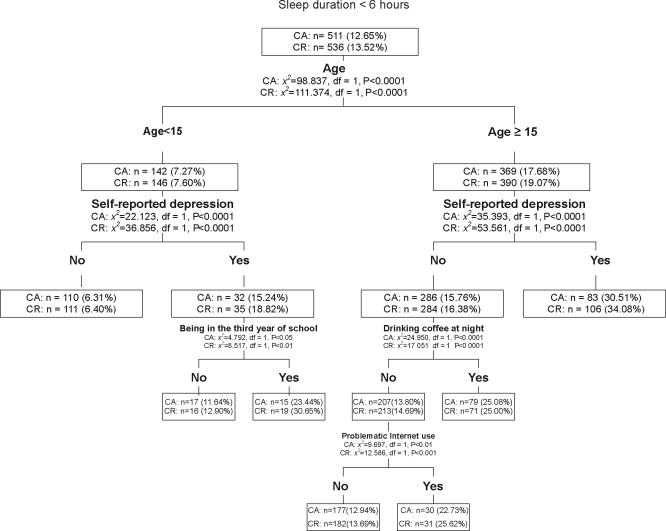
For the purpose of conducting the stepwise CHAID analysis, 4039 participants were randomly selected as the calibration sample and 3965 participants as the cross-validation sample. The results of the stepwise CHAID analysis for the correlates of short nocturnal sleep duration in the calibration and cross-validation samples are shown in Figure 1. In the calibration sample, the first and the most significant variable selected was age. Altogether, 17.68% of the older adolescents (≥ 15 years old) had short nocturnal sleep duration, whereas only 7.27% of the younger adolescents (< 15 years old) had short nocturnal sleep duration (χ2 (df = 1) = 98.837, P < 0.0001). For both the older and younger adolescents, the severity of self-reported depression was another discriminating factor: 30.51% of older adolescents who had self-reported depression (total CES-D score > 27.11) had short nocturnal sleep duration versus 15.76% of older adolescents who had no self-reported depression (total CES-D score ≤ 27.11) (χ2 (df = 1) = 35.393, P < 0.0001); 15.24% of younger adolescents who had self-reported depression had short nocturnal sleep duration versus 6.31% of younger adolescents who had no self-reported depression (χ2 (df = 1) = 22.123, P < 0.0001). Drinking coffee at night was another discriminating factor in the older adolescents without self-reported depression. Among the older nondepressed adolescents, 25.08% of those who drank coffee at night had short nocturnal sleep duration versus 13.80% of those who did not drink coffee at night (χ2 (df = 1) = 24.950, P < 0.0001). Among the older nondepressed adolescents who did not drink coffee at night, problematic Internet use had a further discriminating effect: 22.73% of those who had problematic Internet use had short nocturnal sleep duration versus 12.94% of those who had no problematic Internet use (χ2 (df = 1) = 9.697, P < 0.01). On the other hand, among the younger depressed adolescents, being in the third year of school had a further discriminating effect: 23.44% of those who were in the third year of school had short nocturnal sleep duration versus 11.64% of those who were not in the third year (χ2 (df = 1) = 4.792, P < 0.05). Results in the cross-validation sample are also shown in Figure 1. This indicated that the results of the CHAID analysis were replicable.
Figure 1.
Discriminating factors of sleep duration CA: calibration sample; CR: cross-validation sample
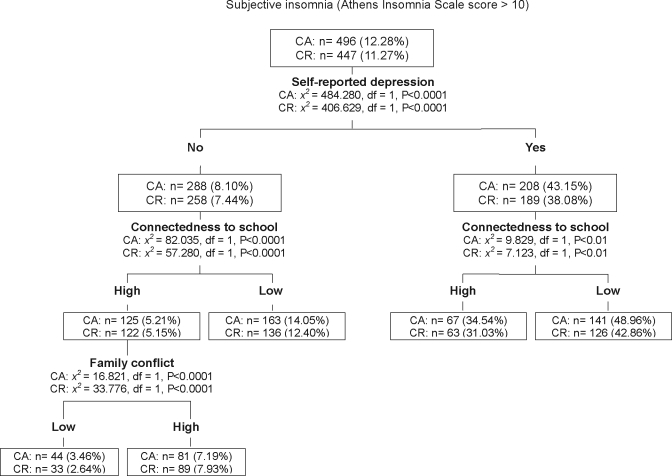
The results of the stepwise CHAID analysis for correlates of subjective insomnia in the calibration and the cross-validation samples are shown in Figure 2. In the calibration sample, the first and the most significant variable selected was the severity of self-reported depression. Altogether, 43.15% of the adolescents with self-reported depression had subjective insomnia, whereas only 8.10% of the adolescents without self-reported depression had subjective insomnia (χ2 (df = 1) = 484.280, P < 0.0001). The level of connectedness to school was another discriminating factor. Among the depressed adolescents, 48.96% of those who had low connectedness to school (median > 1.8) had subjective insomnia versus 34.54% of those who had high connectedness to school (median ≤ 1.8) (χ2 (df = 1) = 9.829, P < 0.005). Among the non-depressed adolescents, 14.05% of those who had low connectedness to school had subjective insomnia versus 5.21% of those who had high connectedness to school (χ2 (df = 1) = 82.035, P < 0.0001). For the nondepressed adolescents who had high connectedness to school, the level of family conflict was a further discriminating factor: 7.19% of those who had high family conflict (median > 2.5) had subjective insomnia versus 3.46% of those who had low family conflict (median ≤ 2.5) (χ2 (df = 1) = 16.821, P < 0.0001). Results in the cross-validation sample are also shown in Figure 2. This indicated that the results of the CHAID analysis were replicable.
Figure 2.
The discriminating factors of subjective insomnia CA: calibration sample; CR: cross-validation sample
The results of the logistic regression analysis model on the correlates of short nocturnal sleep duration are shown in Table 2. Adolescents who were older, had self-reported depression, were in the third year of school, drank coffee at night, and had problematic Internet use were more likely to have short nocturnal sleep duration, which confirmed the findings of the CHAID analysis. We also found that the interaction between self-reported depression and problematic Internet use was negatively associated with short nocturnal sleep duration. Further analysis found that problematic Internet use increased the risk of short nocturnal sleep duration only in the nondepressed adolescents but not in the depressed ones. Although the Wald χ2 values indicated that low paternal education and high family conflict were associated with short nocturnal sleep duration, the OR indicated that the size of their effect on short nocturnal sleep duration was too small to be practically significant.
Table 2.
The Correlates of Short Sleep Duration in the Cross-Validation Sample Examined by the Logistic Regression (N = 3965)
| Variables | B | SE | Wald | OR | 95% CI of OR | |
|---|---|---|---|---|---|---|
| Lower |
Upper |
|||||
| Older age | 1.054 | 0.162 | 42.153a | 2.871 | 2.088 | 3.946 |
| Self-reported depression | 1.104 | 0.267 | 17.100a | 3.016 | 1.787 | 5.089 |
| Being in the third year of school | 0.610 | 0.204 | 8.942b | 1.840 | 1.234 | 2.743 |
| Drinking coffee | 0.541 | 0.251 | 4.632c | 1.718 | 1.050 | 2.813 |
| Problematic Internet use | 0.851 | 0.276 | 9.488b | 2.342 | 1.363 | 4.025 |
| Older age × Self-reported depression | −0.220 | 0.264 | 0.693 | 0.802 | 0.478 | 1.347 |
| Older age × Being in the third year of school | −0.151 | 0.229 | 0.435 | 0.860 | 0.549 | 1.346 |
| Older age × Drinking coffee | 0.077 | 0.257 | 0.088 | 1.080 | 0.652 | 1.788 |
| Older age × Problematic Internet use | −0.213 | 0.284 | 0.562 | 0.808 | 0.463 | 1.411 |
| Self-reported depression × Being in the third year of school | −0.193 | 0.271 | 0.507 | 0.825 | 0.485 | 1.402 |
| Self-reported depression × Drinking coffee | 0.127 | 0.272 | 0.217 | 1.135 | 0.666 | 1.936 |
| Self-reported depression × Problematic Internet use | −0.761 | 0.293 | 6.737b | 0.467 | 0.263 | 0.830 |
| Being in the third year of school × Drinking coffee | −0.013 | 0.253 | 0.003 | 0.987 | 0.601 | 1.620 |
| Being in the third year of school × Problematic Internet use | −0.153 | 0.299 | 0.263 | 0.858 | 0.477 | 1.541 |
| Drink coffee × Problematic Internet use | −0.245 | 0.326 | 0.567 | 0.783 | 0.413 | 1.482 |
| Male | −0.139 | 0.105 | 1.759 | 0.870 | 0.708 | 1.069 |
| Living in a rural area | −0.153 | 0.103 | 2.210 | 0.859 | 0.702 | 1.050 |
| Low paternal education | −0.277 | 0.122 | 5.167c | 0.758 | 0.598 | 0.963 |
| Low maternal education | −0.125 | 0.115 | 1.192 | 0.882 | 0.705 | 1.105 |
| Having a part-time job | 0.230 | 0.117 | 3.885c | 1.259 | 1.001 | 1.583 |
| BMI | 0.002 | 0.013 | 0.018 | 1.002 | 0.976 | 1.028 |
| High family conflict | 0.265 | 0.100 | 7.035b | 1.303 | 1.072 | 1.584 |
| Low family monitoring | 0.051 | 0.093 | 0.299 | 1.052 | 0.876 | 1.264 |
| Substance use by family members | −0.037 | 0.114 | 0.103 | 0.964 | 0.771 | 1.206 |
| Low connectedness to peer group | −0.113 | 0.105 | 1.162 | 0.893 | 0.727 | 1.097 |
| Time spent with friends | −0.004 | 0.003 | 1.862 | 0.996 | 0.991 | 1.002 |
| Low connectedness to school | 0.240 | 0.138 | 3.027 | 1.271 | 0.970 | 1.666 |
| Low academic achievement | 0.041 | 0.115 | 0.128 | 1.042 | 0.832 | 1.306 |
| Problematic cellular phone use | 0.258 | 0.137 | 3.557 | 1.295 | 0.990 | 1.694 |
p: < 0.001;
p: < 0.01;
p: < 0.05
OR refers to odds ratio; CI, confidence interval; BMI, body mass index.
The results of the logistic regression analysis model on the correlates of subjective insomnia are shown in Table 3. The adolescents who had self-reported depression, low connectedness to school, and high family conflict were more likely to have subjective insomnia, which confirmed the findings of the CHAID analysis. The results of the logistic regression analysis model further found that low connectedness to peer group (OR = 1.558) and problematic Internet use (OR = 1.656) had a small effect on subjective insomnia. Although the Wald χ2 values indicated that the adolescents who were female, were older, had a part-time job, and had family members with substance use were more likely to have subjective insomnia, the OR indicated that the size of the effect on subjective insomnia was too small to be significant.
Table 3.
The Correlates of Subjective Insomnia in the Cross-Validation Sample Examined by the Logistic Regression (N = 3965)
| Variables | B | SE | Wald | OR | 95% CI of OR | |
|---|---|---|---|---|---|---|
| Lower |
Upper |
|||||
| Self-reported depression | 2.368 | 0.744 | 10.128b | 10.681 | 2.484 | 45.929 |
| Low connectedness to school | 0.996 | 0.180 | 30.567a | 2.706 | 1.901 | 3.852 |
| High family conflict | 0.616 | 0.142 | 18.939a | 1.852 | 1.403 | 2.445 |
| Self-reported depression × Low connectedness to school | −0.369 | 0.299 | 1.528 | 0.691 | 0.385 | 1.241 |
| Self-reported depression × High family conflict | −0.133 | 0.211 | 0.398 | 0.875 | 0.579 | 1.324 |
| Low connectedness to school × High family conflict | −0.356 | 0.201 | 3.125 | 0.701 | 0.472 | 1.039 |
| Male | −0.277 | 0.120 | 5.308c | 0.758 | 0.599 | 0.960 |
| Older age | 0.287 | 0.120 | 5.731c | 1.332 | 1.053 | 1.684 |
| Living in a rural area | −0.166 | 0.116 | 2.062 | 0.847 | 0.675 | 1.062 |
| BMI | −0.018 | 0.015 | 1.380 | 0.983 | 0.954 | 1.012 |
| Having a part-time job | 0.307 | 0.131 | 5.531c | 1.360 | 1.053 | 1.757 |
| Drinking coffee | 0.201 | 0.140 | 2.057 | 1.223 | 0.929 | 1.609 |
| Low paternal education | −0.025 | 0.131 | 0.035 | 0.976 | 0.754 | 1.262 |
| Low maternal education | 0.139 | 0.127 | 1.187 | 1.149 | 0.895 | 1.475 |
| Low family monitoring | 0.140 | 0.100 | 1.938 | 1.150 | 0.945 | 1.399 |
| Substance use of family members | 0.265 | 0.121 | 4.753c | 1.303 | 1.027 | 1.653 |
| Being in the third year of school | −0.054 | 0.132 | 0.165 | 0.948 | 0.732 | 1.228 |
| Low academic achievement | 0.466 | 0.113 | 17.080a | 1.593 | 1.277 | 1.987 |
| Time spent with friends | 0.160 | 0.124 | 1.659 | 1.173 | 0.920 | 1.496 |
| Low connectedness to peer group | 0.003 | 0.003 | 0.826 | 1.003 | 0.997 | 1.008 |
| Problematic cellular phone use | 0.287 | 0.150 | 3.677 | 1.332 | 0.994 | 1.786 |
| Problematic Internet use | 0.529 | 0.150 | 12.530a | 1.698 | 1.266 | 2.276 |
P < 0.001;
P < 0.01;
P < 0.05
OR refers to odds ratio; CI, confidence interval; BMI, body mass index.
DISCUSSION
This study examined the individual, family, peer, and school correlates of short nocturnal sleep duration and subjective insomnia among a large-scale and representative population of Taiwanese adolescents. We found that older age, self-reported depression, being in the third year of school, drinking coffee at night, and problematic Internet use were significantly associated with short nocturnal sleep duration in adolescents. In parallel, self-reported depression, low connectedness to school, high family conflict, low connectedness to peer group, and problematic Internet use were associated with subjective insomnia in adolescents. The OR of these correlated factors indicated that they had effects ranging from small to large on short nocturnal sleep duration or subjective insomnia. The first interesting finding of the present study was that the factors associated with short nocturnal sleep duration were not completely the same as those associated with subjective insomnia. The results indicated that while older age, being in the third year of school, and drinking coffee might shorten the duration of nocturnal sleep, they were not powerfully discriminating factors for subjective insomnia. On the other hand, several social contexts, including low connectedness to school, high family conflict, and low connectedness to peer group were associated with the subjective insomnia but not with the impaired quantity of nocturnal sleep in adolescents.
In this study, self-reported depression was 1 of the 2 factors that were associated with both short nocturnal sleep duration and subjective insomnia in adolescents. Although the changes of sleep duration and insomnia are the components of depressive symptoms in the DSM-IV-TR,44 they can also predict the development of depression in the future.48 A longitudinal study on adolescents even found that sleep problems could predict persistent depressive symptoms over a 4-year follow-up period.49 From the results of this study, we suggest that intervention to control sleep problems and depression are necessary. Previous studies have found that cognitive behavior therapy and short-term medication treatment for insomnia can relieve depressive symptoms.50 On the other hand, effective treatment of depression can also be a critical aspect of improving sleep problems.1
Problematic Internet use was another factor that was associated with both short nocturnal sleep duration and subjective insomnia in adolescents. Our previous study found that adolescents with problematic Internet use had more severe psychopathology than those without problematic Internet use, and this included depression.51 In this study, problematic Internet use had an independent role that affected short nocturnal sleep duration and subjective insomnia after adjusting for the effect of self-reported depression. A number of explanations for the relationship between problematic computer use and sleep patterns have been put forward.31 First, problematic computer use leads directly to a reduction in total sleep time by substituting for it.52 Playing online games and online chatting are the 2 most common Internet activities for adolescents51; these are characterized as being without predefined stopping points and, as such, are more likely to bring about time displacements.53 Second, it may be the content of Internet use that provokes sleep problems. Late playing of online games and online chatting can cause high arousal and alertness in the brain, thus interfering with the calming effect that is necessary to bring about sleep,54 and this might delay the onset of sleep.18 Third, intensive computer use may also contribute to health-related problems, particularly neck, shoulder, and low back pain,55 which may have a negative effect on sleep. The results of this study indicate that, with regard to adequate sleep quality and quantity, it is necessary to help adolescents develop control over Internet-use behavior and prevent the development of problematic Internet use.
In this study, older age was the first factor that discriminated adolescents with short nocturnal sleep duration from those with ordinary sleep duration. The result supported the findings of previous studies that total nocturnal sleep time considerably decreases during adolescence.3,10,11 The association may be accounted for by the multidimensionality of the developmental changes during adolescence, which include a modification of sleep/wake regulation and sleep patterns, transition to an earlier school start time and a desire to stay up late at night to engage in adult-like social activities, self-determined bed times, and easy access to a vast range of stimulating and arousing activities.1 This study also found that adolescents who were in the third year of junior or senior high school were more likely to report short nocturnal sleep duration than were those who were in the first or second year. This finding may be attributable to the upcoming entrance examination that increased academic workloads and social demands related to school grade levels; this may lead to a delayed bedtime and an earlier rising time among students in higher grades.15 This study found that drinking coffee was associated with short nocturnal sleep duration in adolescents. A previous study also found that drinking coffee was associated with preferring an evening type of sleep in adolescents.19 Adolescents may drink coffee to keep up their spirits during studying or while carrying out entertaining activities. Given the importance of adequate sleep on healthy adolescent development, parents and health professionals should be aware of adolescents' sleep patterns and this correlation between short nocturnal sleep duration and various activities; they may need to intervene to improve the adolescents' sleep behavior.
One of the unique contributions of this study was an examination of the association of psychosocial contexts with sleep in adolescents. We found that a variety of psychosocial contexts, including high family conflict, low connectedness to school, and low connectedness to their peer group were associated with subjective insomnia in adolescents. Although the causal relationships between subjective insomnia and these adverse psychosocial experiences could not be determined in this cross-sectional study, we hypothesized that there might be bidirectional relationships between these 2 factor clusters. For example, although escalating conflict in troubled parent-youth, teacher-student, and intrapeer group relationships may lead to poor mental health and sleep disturbance,56,57 disturbed sleep patterns may increase the risk of behavior or emotional problems, such as aggression and delinquent behavior. These lead to social problems,7,58 which may further exacerbate the conflicts between youth and their families, school teachers, peers, and classmates. Both insomnia and adverse psychosocial contexts need intervention to interrupt the vicious circle and improve the adolescents' mental health and psychosocial experiences.
Several individual (sex, residential background, SES, having a part-time job, and body mass index), family (family monitoring and family members' substance use), peer (time spent with friends), school characteristics (academic achievement), and problematic cellular phone use were not significantly associated with short nocturnal sleep duration or insomnia in adolescents when a variety of individual and psychosocial contexts were examined together in this large-scale of adolescent population. However, these factors might be significantly associated with short nocturnal sleep duration and subjective insomnia among some adolescents, and individual differences need to be taken into account. The associations between nocturnal sleep duration and subjective insomnia and these factors need to be examined further in future studies.
Methodologic Considerations
The first strength of this study is that it is one of the few studies to examine and compare the correlates of sleep quantity and quality at the same time. Second, it is the first one to examine the association of short nocturnal sleep duration and subjective insomnia with a variety of individual factors, family factors, peer factors, school factors, and high-tech device use in a large-scale population of adolescents. Third, selection bias is minimized by sampling the participants in a nonreferred representative school-based sample. Fourth, we used 2 statistical methods (CHAID analysis and logistic regression analysis) to examine the correlates of short nocturnal sleep duration and subjective insomnia in adolescents.
However, some limitations of this study need to be brought forward. Firstly, the cross-sectional research design of this study limited our ability to draw conclusions regarding the causal relationships between sleep patterns and correlates. Secondly, the data were provided by the adolescents themselves, and the authenticity vis-à-vis validity of some data such as the severity of subjective insomnia cannot be easily quantified. Although a previous study found that self-reported sleep-duration estimates are similar to those obtained through wrist actigraphy,59 another study found that the correlation between time-diary sleep and self-reported sleep was weak.60 The validity of the AIS-8 and the Problematic Cellular Phone Use Questionnaire when used on an adolescent population need further study. Thirdly, this study investigated the duration of nocturnal sleep but did not include diurnal sleep; at the same time, this study did not separately assess weekday and weekend sleep. Fourthly, this study recruited adolescent students as the research population; however, adolescents who had dropped out of school and those who were the students at a night school were not recruited into this study. Although, in Taiwan, this proportion of the adolescent population is small, they may have different patterns of sleep, and the correlates may vary compared with the adolescents recruited in this study. Fifthly, the analytical approach using CHAID is exploratory, and the models presented are simply descriptive. Although we used standard processes, including a cross-validation sample and logistic regression analysis to confirm the results from the calibration sample,46 there might be alternative models that fit the data in a statistically or theoretically acceptable manner. Sixthly, those who had missing data were more likely to be male and from junior high schools. This needs further study to examine whether the adolescents with missing data showed different sleep patterns and correlates, compared with those who completed the questionnaires. The results of this study support the idea that the association between sleep and a range of multidimensional factors among adolescents warrants further investigation, and we suggest that future studies should incorporate objective measures of sleep, should be longitudinal, and should be designed to address causal direction. Further studies also need to be carried out on adolescents who have dropped out of school and who are studying at night school.
Implications
This study found that a variety of individual, family, peer, and school factors were associated with short sleep duration and subjective insomnia in adolescents. Given the importance of adequate sleep quantity and quality on healthy adolescent development, we suggest that parents and health professionals should show awareness with regard to sleep duration and quality among adolescents, and this is especially true for adolescents who exhibit the correlates of short sleep duration and subjective insomnia as identified in this study.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
This study was supported by grant NSC 93-2413-H- 037-005-SSS awarded by the National Science Council, Taiwan (ROC).
REFERENCES
- 1.Dahl RE. Pathways to adolescent health: sleep regulation and behavior. J Adolesc Health. 2002;31:175–84. doi: 10.1016/s1054-139x(02)00506-2. [DOI] [PubMed] [Google Scholar]
- 2.Maquet P. The role of sleep in learning and memory. Science. 2001;294:1048–52. doi: 10.1126/science.1062856. [DOI] [PubMed] [Google Scholar]
- 3.Chen MY. Adequate sleep among adolescents is positively associated with health status and health-related behaviors. BMC Public Health. 2006;6:59. doi: 10.1186/1471-2458-6-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carskadon MA. Regulation of adolescent sleep: implications for behavior. Ann N Y Acad Sci. 2004;1021:276–91. doi: 10.1196/annals.1308.032. [DOI] [PubMed] [Google Scholar]
- 5.Liu X. Sleep and youth suicidal behavior: a neglected field. Curr Opin Psychiatry. 2006;19:288–93. doi: 10.1097/01.yco.0000218600.40593.18. [DOI] [PubMed] [Google Scholar]
- 6.Carskadon MA. Patterns of sleep and sleepiness in adolescents. Pediatrician. 1990;17:5–12. [PubMed] [Google Scholar]
- 7.Stein MA. Sleep and behavior problems in school-aged children. Pediatrics. 2001;107:E60. doi: 10.1542/peds.107.4.e60. [DOI] [PubMed] [Google Scholar]
- 8.Ohayon MM. Prevalence and patterns of problematic sleep among older adolescents. J Am Acad Child Adolesc Psychiatry. 2000;39:1549–56. doi: 10.1097/00004583-200012000-00019. [DOI] [PubMed] [Google Scholar]
- 9.Lerner RM. Contemporary developmental theory and adolescence: Developmental systems and applied developmental science. J Adolesc Health. 2002;31:122–35. doi: 10.1016/s1054-139x(02)00495-0. [DOI] [PubMed] [Google Scholar]
- 10.Carskadon MA. Regulation of sleepiness in adolescents: update, insights and speculation. Sleep. 2002;25:606–14. doi: 10.1093/sleep/25.6.606. [DOI] [PubMed] [Google Scholar]
- 11.Dorofaeff TF. Sleep and adolescence. Do New Zealand teenagers get enough? J Paediatr Child Health. 2006;42:515–20. doi: 10.1111/j.1440-1754.2006.00914.x. [DOI] [PubMed] [Google Scholar]
- 12.Liu X. Prevalence and correlates of self-reported sleep problems among Chinese adolescents. Sleep. 2000;23:27–34. [PubMed] [Google Scholar]
- 13.BaHammam A. Sleep duration and its correlates in a sample of Saudi elementary school children. Singapore Med J. 2006;47:875–81. [PubMed] [Google Scholar]
- 14.Ford DE. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention. JAMA. 1989;262:1479–84. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- 15.Gau SF. Sleep problems of junior high school students in Taipei. Sleep. 1995;18:667–73. doi: 10.1093/sleep/18.8.667. [DOI] [PubMed] [Google Scholar]
- 16.Lazaratou H. Sleep problems in adolescence. A study of senior high school students in Greece. Eur Child Adolesc Psychiatry. 2005;14:237–43. doi: 10.1007/s00787-005-0460-0. [DOI] [PubMed] [Google Scholar]
- 17.Gaina A. Gender and temporal differences in sleep–wake patterns in Japanese schoolchildren. Sleep. 2005;28:337–42. [PubMed] [Google Scholar]
- 18.Manni R, et al. Poor sleep in adolescents: a study of 869 17-year-old Italian secondary school students. J Sleep Res. 1997;6:44–9. doi: 10.1046/j.1365-2869.1997.00025.x. [DOI] [PubMed] [Google Scholar]
- 19.Gau SS. Correlates of sleep-wake patterns among children and young adolescents in Taiwan. Sleep. 2004;27:512–9. [PubMed] [Google Scholar]
- 20.Reilly J, et al. Early life risk factors for obesity in childhood: cohort study. BMJ. 2005;330:1357. doi: 10.1136/bmj.38470.670903.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Beebe DW, et al. Sleep in overweight adolescents: shorter sleep, poorer sleep quality, sleepiness and sleep-disordered breathing. J Pediatr Psychol. 2007;32:69–79. doi: 10.1093/jpepsy/jsj104. [DOI] [PubMed] [Google Scholar]
- 22.Knutson KL. Sex differences in the association between sleep and body mass index in adolescents. J Pediatr. 2005;147:830–4. doi: 10.1016/j.jpeds.2005.07.019. [DOI] [PubMed] [Google Scholar]
- 23.Rutter M. Resilience: some conceptual considerations. J Adolesc Health. 1993;14:626–39. doi: 10.1016/1054-139x(93)90196-v. [DOI] [PubMed] [Google Scholar]
- 24.Goebert D, et al. Cumulative effect of family environment on psychiatric symptomatology among multiethnic adolescents. J Adolesc Health. 2000;27:34–42. doi: 10.1016/s1054-139x(00)00108-7. [DOI] [PubMed] [Google Scholar]
- 25.Gemelli R. Washington, DC: American Psychiatric Press; 1996. Normal child and adolescent development. [Google Scholar]
- 26.Gau SF. The transition of sleep phase preference in early adolescence. Sleep. 2003;26:449–55. doi: 10.1093/sleep/26.4.449. [DOI] [PubMed] [Google Scholar]
- 27.Ministry of Education (MOE) An Introduction to the Ministry of Education of the R.O.C. [Accessed August 4, 2008]; Available at: http://english.moe.gov.tw/ct.asp?xItem=263&CtNode=782&mp=1. Updated June 2, 2006.
- 28.Wolfson AR. Sleep schedules and daytime functioning in adolescents. Child Dev. 1998;69:875–87. [PubMed] [Google Scholar]
- 29.Gaina A, et al. Morning–evening preference: sleep patterns spectrum and lifestyle habits among junior high school pupils. Chronobiol Int. 2006;23:1–15. doi: 10.1080/07420520600650646. [DOI] [PubMed] [Google Scholar]
- 30.Ko CH. Proposed diagnostic criteria of internet addiction for adolescents. J Nerv Ment Dis. 2005;193:728–33. doi: 10.1097/01.nmd.0000185891.13719.54. [DOI] [PubMed] [Google Scholar]
- 31.Eggermont S. Nodding off or switching off? The use of popular media as a sleep aid in secondary-school children. J Pediatr Child Health. 2006;42:428–33. doi: 10.1111/j.1440-1754.2006.00892.x. [DOI] [PubMed] [Google Scholar]
- 32.Gaina A, et al. Epidemiological aspects of self-reported sleep onset latency in Japanese junior high school children. J Sleep Res. 2006;15:266–75. doi: 10.1111/j.1365-2869.2006.00530.x. [DOI] [PubMed] [Google Scholar]
- 33.Punamäki RL. Use of information and communication technical (ICT) and perceived health in adolescence: the role of sleeping habits and waking-time tiredness. J Adolesc. 2007;30:569–85. doi: 10.1016/j.adolescence.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 34.Ministry of the Interior. Taipei: Executive Yuan, Taiwan; 2002. 2001 Taiwan-Fukien Demographic Fact Book, Republic of China. [Google Scholar]
- 35.Soldatos CR. Athens Insomnia Scale: validation of an instrument based on ICD-10 criteria. J Psychosom Res. 2000;48:555–60. doi: 10.1016/s0022-3999(00)00095-7. [DOI] [PubMed] [Google Scholar]
- 36.World Health Organization. Geneva, Switzerland: WHO; 1992. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. [Google Scholar]
- 37.Chien CP. Depression in Taiwan: epidemiological survey utilizing CES-D. Seishin Shinkeigaku Zasshi. 1985;87:335–8. [PubMed] [Google Scholar]
- 38.Radloff LS. The CSE-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 39.Yang HJ. Using the CES-D in a two-phase survey for depressive disorders among nonreferred adolescents in Taipei: a stratum-specific likelihood ratio analysis. J Affect Disord. 2004;82:419–30. doi: 10.1016/j.jad.2004.04.008. [DOI] [PubMed] [Google Scholar]
- 40.Crocke L. New York, NY: Holt, Rinehart & Winston; 1986. Introduction to Classical and Modern Test Theory. [Google Scholar]
- 41.Yen CF. Correlates of methamphetamine use for Taiwanese adolescents. Psychiatry Clin Neurosci. 2006;60:160–7. doi: 10.1111/j.1440-1819.2006.01481.x. [DOI] [PubMed] [Google Scholar]
- 42.Chen SH. Development of the Chinese Internet addiction scale and its psychometric study. Chinese J Psychol. 2003;45:279–94. [Google Scholar]
- 43.Ko CH. Screening for internet addiction: an empirical research on cut-off points for the Chen Internet Addiction Scale. Kaohsiung J Med Sci. 2005;21:545–54. doi: 10.1016/S1607-551X(09)70206-2. [DOI] [PubMed] [Google Scholar]
- 44.American Psychiatric Association. Washington, DC: American Psychiatric Association; 2000. Diagnostic and Statistical Manual of Mental Disorders, 4th ed, Text Revision. [Google Scholar]
- 45.SPSS Inc. Chicago, IL: SPSS Inc; 2001. Answer Tree 3 User's Guide. [Google Scholar]
- 46.Lemon SC. Classification and regression tree analysis in public health: methodologic review and comparison with logistic regression. Ann Behav Med. 2003;26:172–81. doi: 10.1207/S15324796ABM2603_02. [DOI] [PubMed] [Google Scholar]
- 47.Chinn S. A simple method for converting an odds ratio to effect size for use in meta-analysis. Stat Med. 2000;19:3127–31. doi: 10.1002/1097-0258(20001130)19:22<3127::aid-sim784>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 48.Breslau N. Sleep disturbances and psychiatric disorders: a longitudinal epidemiology study of young adults. Biol Psychiatry. 1996;39:411–8. doi: 10.1016/0006-3223(95)00188-3. [DOI] [PubMed] [Google Scholar]
- 49.Patten CA. Persistence of depressive symptoms in adolescents. Neuropsychopharmacology. 2001;25:89–90. doi: 10.1016/S0893-133X(01)00323-2. [DOI] [PubMed] [Google Scholar]
- 50.Dahl RE. The psychobiology of adolescent depression. In: Cicchetti D, editor. Adolescence: Opportunities and Challenges. Vol. 7. Rochester, NY: University of Rochester Press; 1996. pp. 197–232. [Google Scholar]
- 51.Yen JY. The comorbid psychiatric symptoms of Internet addiction: attention deficit and hyperactivity disorder (ADHD), depression, social phobia and hostility. J Adolesc Health. 2007;41:93–8. doi: 10.1016/j.jadohealth.2007.02.002. [DOI] [PubMed] [Google Scholar]
- 52.Owens J. Television-viewing habits and sleep disturbance in schoolchildren. Pediatrics. 1999;104:e27. doi: 10.1542/peds.104.3.e27. [DOI] [PubMed] [Google Scholar]
- 53.Van den Bulck J. Is television bad for your health? Behavior and body image of the adolescent ‘couch potato’. J Youth Adolesc. 2000;29:273–88. [Google Scholar]
- 54.Spear LP. The adolescent brain and age-related behavioral manifestations. Neurosci Biobehav Rev. 2000;24:417–63. doi: 10.1016/s0149-7634(00)00014-2. [DOI] [PubMed] [Google Scholar]
- 55.Hakala PT. Frequent computer-related activities increase the risk of neck–shoulder and low back pain in adolescents. Eur J Public Health. 2006;16:536–41. doi: 10.1093/eurpub/ckl025. [DOI] [PubMed] [Google Scholar]
- 56.Borowsky IW. Suicide attempts among American Indian and Alaska Native youth: risk and protective factors. Arch Pediatr Adolesc Med. 1999;153:573–80. doi: 10.1001/archpedi.153.6.573. [DOI] [PubMed] [Google Scholar]
- 57.Patterson GR. Antisocial parents: unskilled and vulnerable. In: Cowan PA, editor. Family Transitions. Hillsdale, NJ: Lawrence Erlbaum Associates; 1991. pp. 195–218. [Google Scholar]
- 58.Gau SS. Association between morningness-eveningness and behavioral/emotional problems among adolescents. J Biol Rhythms. 2007;22:268–74. doi: 10.1177/0748730406298447. [DOI] [PubMed] [Google Scholar]
- 59.Wolfson AR, et al. Evidence for the validity of a sleep habits survey for adolescents. Sleep. 2003;26:213–6. doi: 10.1093/sleep/26.2.213. [DOI] [PubMed] [Google Scholar]
- 60.Knutson KL. Sleep duration and overweight in adolescents: self-reported sleep hours versus time diaries. Pediatrics. 2007;119:e1056–62. doi: 10.1542/peds.2006-2597. [DOI] [PubMed] [Google Scholar]