Abstract
Peptide nucleic acid (PNA) is highly stable and binds to complementary RNA and DNA with high affinity, but it resists cellular uptake, thereby limiting its bioavailability. We investigated whether protective antigen (PA, a non-toxic component of anthrax toxin) could transport antisense PNA oligomers into reporter cells that contain luciferase transgenes with mutant β-globin IVS2 intronic inserts, which permit aberrant pre-mRNA splicing and impair luciferase expression. PNA oligomers antisense to mutant splice sites in these IVS2 inserts induced luciferase expression when effectively delivered into the cells. PNA 18-mers with C-terminal poly-lysine tails [PNA(Lys)8] demonstrated modest sequence-specific antisense activity by themselves at micromolar concentrations in luc-IVS2 reporter cell cultures. However, this activity was greatly amplified by PA. Antisense PNA(Lys)8 with but not without PA also corrected the IVS2-654 β-globin splice defect in cultured erythroid precursor cells from a patient with β-thalassemia [genotype, IVS2-654(β0/βE)], providing further evidence that anthrax PA can effectively transport antisense PNA oligomers into cells.
Keywords: peptide nucleic acid, antisense, anthrax protective antigen
Introduction
Advances in molecular genetics have led to a detailed understanding of the genetic basis of many congenital and acquired diseases, encouraging the development of reagents that can control gene expression selectively, both as experimental tools and candidate therapeutics. Antisense oligonucleotides have been studied extensively in this regard [1–5], and a number of nucleic acid analogs and mimics have been developed as antisense reagents [6–11], including peptide nucleic acid (PNA) [9, 12].
PNA, first described in 1991 by Nielsen et al. [13], is a DNA mimic in which the phosphate deoxyribose backbone of DNA is replaced by a pseudopeptide polymer to which nucleobases are attached via methylene carbonyl linkers. PNA oligomers bind to complementary RNA with very high affinity and specificity, and binding is minimally affected by the secondary structure of RNA transcripts. PNA oligomers also resist nuclease and protease digestion and are biologically stable [1, 9, 13]. Moreover, because PNA oligomers lack a repetitively charged backbone, they do not interact with polyanion-binding proteins, which may complicate the actions of nucleotide analogs when used as gene-targeting agents [14].
While antisense PNA oligomers do not trigger degradation of mRNA transcripts at sites of binding, they can effectively block mRNA translation [9, 12], and they can also control splicing of pre-mRNA transcripts when alternative splice sites are targeted [10, 11]. This latter effect is of particular interest, since many human gene transcripts undergo alternative splicing to generate splice variants with different functions [11].
Despite these positive gene-targeting attributes, unmodified PNA resists cellular uptake and therefore has limited bioavailability [15]. This limitation has impeded its development as a candidate therapeutic, although effective cellular delivery of PNA in vitro has been achieved to some extent by the addition of lysine residues [10, 16] or charged membrane penetrating peptide sequences [15, 17]) or with cationic liposomes as carriers of PNA conjugates [18].
In this study, we examined the ability of anthrax protective antigen (PA) to deliver antisense PNA oligomers into cells. Microbial toxin proteins, such as diphtheria and anthrax toxin, have evolved functional domains that allow them to enter cells via receptor-mediated endocytosis and then access the cytoplasm via trans-endosomal membrane pores [19–23]. Unlike diphtheria toxin (a single protein), anthrax toxin consists of multiple proteins: a non-toxic 83 kD polypeptide [protective antigen (PA)] that mediates cell binding, endocytosis, and trans-membrane pore formation [21,22], and two separate 90 kD proteins [lethal factor (LF) and edema factor (EF)] that mediate cell toxicity. When PA binds a cell through its “receptor binding” domain, a 63 kD fragment (PA-63) is generated by endoproteolysis that forms heptamers, which bind LF and EF and transport them into cells via endocytosis and into the cytoplasm via trans-endosomal pores [22].
We considered PA to be an attractive candidate for study as a vehicle for cellular delivery of PNA because of its bioavailability, lack of toxicity, and potential for modifications that might allow for tissue specificity (e.g. replacement of the cell binding domain with cell-specific ligands [19, 24]).
Materials and Methods
Reagents
Recombinant anthrax PA-63 and PA-83 were obtained from List Laboratories (Campbell, CA). Sense and antisense 18-mer 2'-O-Methyl (2'-O-Me) phosphorothioate oligonucleotides were synthesized by TRI-Link, Inc. (San Diego, CA). PNA 18-mers with and without C-terminal poly-lysines were synthesized by BioSynthesis, Inc. (Lewisville, TX). Oligonucleotide primers for RT-PCR were obtained from Invitrogen (Carlsbad, CA). Cell culture reagents, DMEM/F12 (Dulbecco’s Modified Eagle’s Medium / Nutrient Mixture F-12 Ham's - Liquid Medium with 2 mM L-glutamine) and fetal bovine serum, were obtained from HyClone (Logan, UT).
Reporter Cell Lines
Chinese Hamster Ovary cells (CHO-K1 cells), as used in studies of anthrax toxin biology (21), were obtained from ATCC (American Type Culture Collection, Manassas,VA). A Luc-IVS2-654 reporter transgene was generated by PCR amplification of the human β-globin intron-2 sequence (IVS2) with primers CGCTGCTGGGTGAGTCTATGGGACCCTT and AGGGTTGGCACTGTGGGAGGAAGATAAGAG. The fruit fly luciferase gene was amplified separately from a pGL3-control vector (Promega, San Luis Obispo, CA) into 5’-Luc and 3’-Luc segments using primers TACGATTTGTGCCAGAGTCCTTC and CCATAGACTCACCCAGCAGCGCACTTGAAT, and CCTCCCACAGTGCCAACCCTATTCTCCTTC and GCCCCGACTCTAGAATTACAC, respectively. The PCR product from 5’-Luc was then joined with that of IVS2 by PCR, using flanking primer pairs. The resulting PCR product was then joined with 3’-Luc by PCR using outer flanking primer pairs. The final PCR product, called Luc-IVS2, was digested by Bcl-I and Xba-I and ligated to the Bcl-I and Xba-I digested pGL3-control vector. The Luc-IVS2 gene insert was then released from pGL3-Luc-IVS2 by Hind-III and Xba-I and inserted into a Hind-III and Xba-I digested pcDNA3 vector (Invitrogen). The resulting Luc-IVS2 plasmid was used as a positive control vector for correct splicing of luciferase. It was also mutated (C to T) at position 654 to reproduce the βIVS2-654 β-thalassemia mutation by PCR using primers: TCTGGGTTAAGGTAATAGCAATA and TATTGCTATTACCTTAACCCAGA and the PCR product then digested with Dpn-I, re-annealed, and transformed into E. coli DH5a competent cells (Invitrogen Inc.). DNA sequencing was used to confirm that the resulting plasmid (Luc-IVS2-654) contained the luciferase gene interrupted by the mutant IVS2-654 intron. This plasmid and the control Luc-IVS2 plasmid were transfected into CHO-K1 cells separately using Effectene™ (Qiagen Inc., Valencia, CA). Cells were maintained in selective F12K medium containing G418 (InVivoGen Inc., San Diego, CA) at 400 µg/ml and 10% fetal bovine serum, 2mM L-Glutamate, and 50U of Penicillin/ Streptomycin. Surviving cell colonies were picked from cultures after 10 days of G418 selection, and evaluated for luciferase expression (Promega Inc.). A separate HeLa reporter cell line, stably transfected with a separate luciferase transgene, containing a different mutant β-globin intron-2 insert (Luc-IVS2-705), originally reported by Kang et al. (25), was obtained commercially from GeneTools (Philomath, OR).
Luc-IVS2-654 CHO-K1 cells or Luc-IVS2-705 HeLa cells, from aliquoted frozen stocks, were cultured in DMEM/F12 medium with 10% FBS in 12 and 24-well culture plates (Costar, Fisher Scientific, Pittsburg, PA) for up to 72 hrs. Cells grew as adherent monolayers in culture wells, and seeding concentrations (1–5× 104/mL) were adjusted such that the cells did not become confluent during experimental culture periods. Culture media with reagents, depending upon experimental variables, were replaced every 24 hrs. For certain studies, cells were incubated with 2'-O-Methyl (2'-O-Me) phosphorothioate (PS) oligonucleotides or PNA oligomers, either pre-mixed with Oligofectamine (Invitrogen) or with cell-scraping transfection [26]. For other studies, cells were incubated without physical manipulation in media alone, or in media containing PNA oligomers with or without recombinant anthrax PA-63 or PA-83. Cultured cell protein or RNA was extracted for luciferase assays (Promega, Inc. [27]) or for RT-PCR.
RNA Extraction and Analysis
Total RNA from cultured cells was extracted with TriZOL (Invitrogen). Luc-IVS2 and Luc-IVS2-654 mRNA was amplified by reverse transcription (RT)-PCR using rTth polymerase and primers (TTGATATGTGGATTTCGAGTCGTC and TGTCAATCAGAGTGCTTTTGGCG) hybridized to sequences flanking Luc-IVS2 introns, as described previously [10,24]. PCR products were separated on 7.5% non-denaturing polyacrylamide gels and visualized by ethidium bromide staining [28].
β-thalassemia erythroid cells
Citrate-anticoagulated blood samples from a non-transfused β-thalassemia intermedia patient [IVS2-654(βo)/βE genotype] were generously provided to us by Dr. Edmond Ma at the Queen Mary Hospital of the University of Hong Kong. This sample was obtained from the patient following informed consent and shipped on ice via FedEx, arriving within 48 hrs. Light density mononuclear cells were separated from the blood sample by density gradient centrifugation (lymphocyte separation medium, MB Biologicals, Solon, OH) and were cultured with recombinant erythropoietin (EPO) and c-Kit ligand (SCF), as described by Lacerra et al. [29]. Fresh medium containing cytokines + antisense PNA(Lys)8 (300 nM), + PA-63 (300 ng/mL) was added on days 8 and 12 of culture, and cells were harvested on day 15. RNA was isolated from the cells, and radiolabelling PCR was performed [29]. Total cellular RNA was isolated with TriZOL (Invitrogen) and analyzed by RT-PCR using rTth DNA polymerase (PerkinElmer Life Sciences, Norwalk, CT) and 0.2 µCi of [α-32P]dATP per sample. Aberrant and correct splicing of human IVS2-654 β-globin pre-mRNA in the IVS2-654(βo)/βE compound heterozygote were detected using a forward allele-specific βA primer, spanning positions 50–79 of human β-globin exon 1, and a reverse primer, spanning positions 6–28 of exon 3 of the human β-globin gene, as described [29].
Results and Discussion
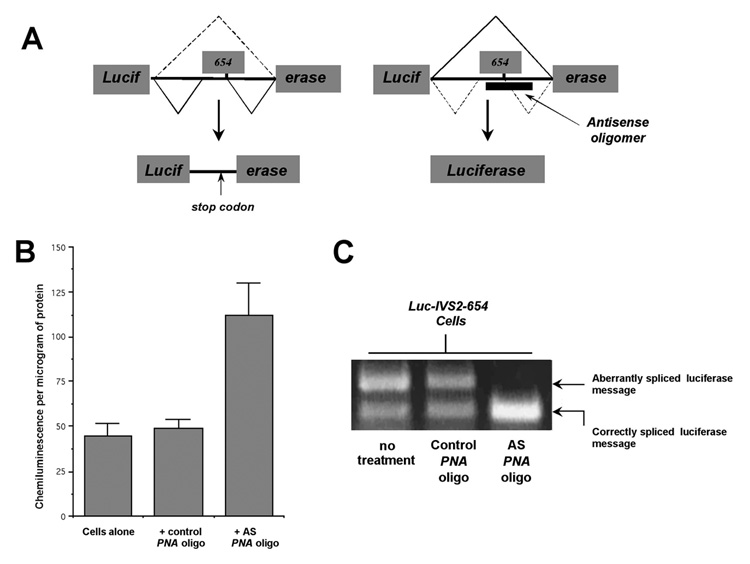
To evaluate the ability of PA to deliver antisense PNA oligomers into cells, we developed an antisense reporter system using CHO-K1 cells. These cells express abundant anthrax PA receptors and have been used extensively to study anthrax toxin biology and PA receptors [21]. Following a strategy reported previously [10, 11, 16], we generated a CHO-K1 cell line (Luc-IVS2-654 CHO) that expressed a modified luciferase gene containing a human thalassemia β-globin gene intronic insert (IVS2-654). This intron encodes an alternative splice site that allows incorrect splicing of pre-mRNA transcripts thereby preventing the translation of transcripts to full-length protein (Figure 1A). This IVS2-654 intronic mutation is a common cause of β-thalassemia in Asia. Binding of antisense oligonucelotides to the aberrant splice site in the IVS2-654 intron has been shown to correct β-globin pre-mRNA splicing and to permit expression of normal full-length β-globin in thalassemic erythroid precursor cells that carry this mutation [29].
Figure 1.
(A) Diagrammatic depiction of the effect of a mutant β-globin intron-2 (IVS2-654) insert in the luciferase gene coding sequence on luciferase expression. Blockade of the aberrant IVS2-654 splice site by an antisense oligomer (right-hand diagram) permits expression of a correctly spliced gene product and active enzyme. Adapted from Kang et al. [25] and Sazani et al. [10]. (B) Induction of luciferase expression and (C) correction of pre-mRNA splicing in Luc-IVS2-654 CHO cells following 48 hrs incubation with 1.0µM antisense (AS) PNA(Lys)8 oligomers delivered to the cells by cell scraping transfection [16] and oligofectamine. Results in B represent mean values ± SEM for 4 replicate studies.
Luc-IVS2-654 CHO cells expressed both correctly spliced and incorrectly spliced luciferase mRNA (Figure 1C and Figure 2B), and background luciferase activity was measurable in cell extracts (Figure 1B and Figure 2A). Both antisense 2'-O-Methyl (2'-O-Me) phosphorothioate (PS) 18-mer oligonucleotides (not shown) and antisense PNA 18-mers (with sequences complementary to an 18-nucleobase region of the mutant β-globin intron-2 that flanked position 654) were found to correct the aberrant splicing of Luc-IVS2-654 pre-mRNA, when transfected into the cells, and also to increase substantially the expression of luciferase activity in the cells (Figures 1B and 1C).
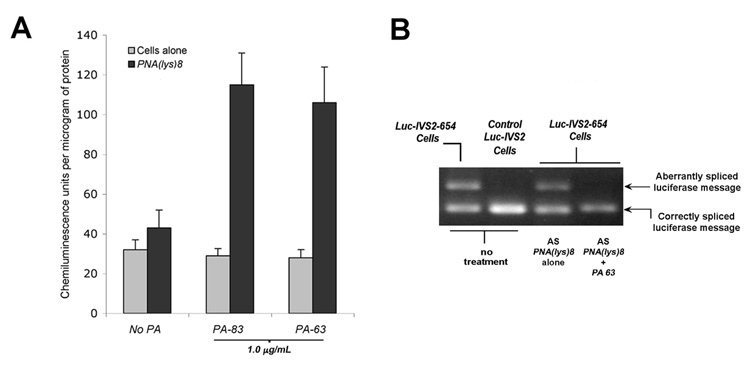
Figure 2.
(A) Induction of luciferase activity in Luc-IVS2-654 CHO cells by antisense PNA(lys)8 (0.3µM) following 72 hours’ incubation with PA-63 or PA-83 (1.0µg/mL). Results represent mean values ± SEM for 4 replicate studies. (B) Correction of pre-mRNA splicing in Luc-IVS2-654 CHO cells following incubation with 1.0µM antisense PNA(Lys)8 oligomers with but not without PA-63 (1.0µg/mL).
Using Luc-IVS2-654 CHO cells to detect sequence specific antisense activity, we next determined whether an antisense PNA 18-mer with a C-terminal eight-lysine oligopeptide tail [PNA(Lys)8] could be shown to induce luciferase activity without transfection when incubated with Luc-IVS2-654 CHO cells along with anthrax PA. Antisense PNA(Lys)8 oligomers used for these studies [GCTATTACCTTAACCCAG-O-(Lys)8 with base, A, corresponding to the mutant T at IVS2 position 654] had the same nucleotide binding sequence as did the unmodified antisense PS oligonucleotides and PNA oligomers used to validate the Luc-IVS2-654 CHO reporter cell system, as shown in Figure 1. A C-terminal poly-lysine tail was added to the PNA oligomers because of a finding reported by Blanke et al. [24] that C-terminal poly-lysines added to a polypeptide fragment derived from the catalytic domain of diphtheria toxin permitted this otherwise non-toxic polypeptide to use anthrax PA to enter and kill cells. A sense 18-mer PNA(Lys)8 served as a control in these studies.
Both recombinant, full-length PA-83 and “nicked” PA-63 were evaluated, and neither form of PA by itself affected luciferase expression in Luc-IVS2-654 CHO cells. Control sense PNA(Lys)8 oligomers also did not affect luciferase expression in these cells, with or without PA, under any condition of reagent dose or incubation time examined. However, antisense PNA(Lys)8 was found to induce a modest degree of luciferase expression by itself, and this effect was substantially enhanced by both PA-83 and PA-63 (Figure 2A). Enhanced luciferase expression by antisense PNA(Lys)8 oligomers in the presence of PA was also associated with a shift in luciferase mRNA detected by RT-PCR to the correctly spliced form, as in control Luc-IVS2 CHO cells containing a luciferase transgene with a wild-type, non-mutant β-IVS2 insert (Figure 2B).
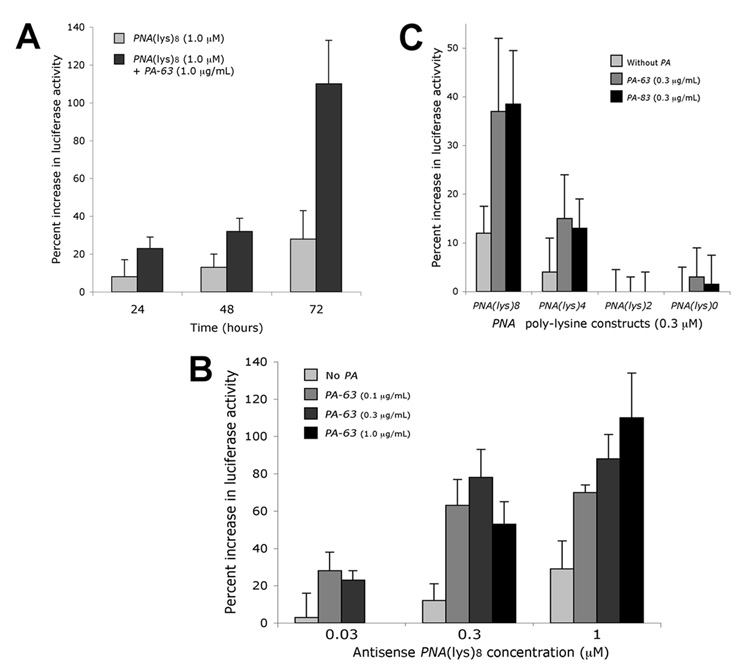
Sazani et al. [10] reported previously that the addition of a short, C-terminal (Lys)4 oligopeptide tail to PNA oligomers allowed detectable cellular uptake of PNA at micromolar concentrations. Given this report, we anticipated that antisense PNA(Lys)8 might have some activity by itself at such concentrations, as observed. However, this activity was significantly enhanced by both PA-83 and PA-63 in a time and dose-dependent manner (Figures 3A and 3C). Moreover, antisense PNA(Lys)8 at concentrations as low as 30 nM was found to induce detectable increases in luciferase expression when incubated with Luc-IVS2-654 CHO cells together with PA.
Figure 3.
(A) Induced luciferase expression in Luc-IVS2-654 CHO cells incubated for 24 – 72 hrs with antisense PNA(Lys)8 oligomers at 1.0µM with and without PA-63, 1.0µg/mL. (B) Luciferase expression in Luc-IVS2-654 CHO cells incubated for 72 hrs with antisense PNA(Lys)8 oligomers at 0.03, 0.3, and 1.0µM both with and without PA-63 at varying concentrations (0.1 – 1.0–g/mL). (C) Induction of luciferase activity in Luc-IVS2-654 CHO cells by antisense PNA oligomers with poly-lysine tails of varying lengths [0.3µM, PNA(Lys)8, PNA(Lys)4, PNA(Lys)2, and PNA(Lys)0] with and without PA-63 (0.3µg/mL). Results represent mean values ± SEM for 4 to 6 replicate studies.
The apparent ability of both PA-63 and PA-83 to facilitate delivery of antisense PNA(Lys)8 into reporter cells required the C-terminal polylysine tail on PNA (Figure 3B). Induction of luciferase expression in cell cultures by antisense PNA with PA was reduced when the number of lysine residues in the poly-lysine tail was decreased from 8 to 4 and lost completely when C-terminal lysines were reduced to 2 or eliminated.
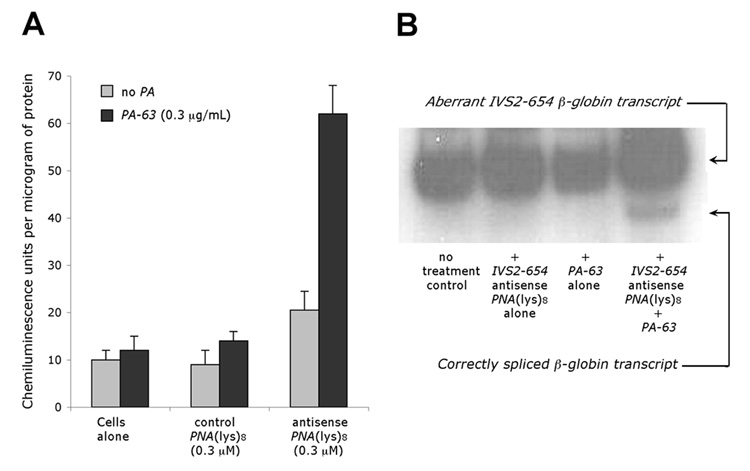
PA-mediated cellular delivery of antisense PNA(Lys)8 oligomers was also observed in human erythroid progenitor cells and in a HeLa cell line (Luc-IVS2-705 HeLa) [25], which expressed a luciferase transgene with a mutant β-globin IVS2 intronic insert (IVS2-705) different from the one expressed by Luc-IVS2-654 CHO reporter cells. Effective antisense blockade of the aberrant splice site in Luc-IVS2-705 HeLa cells has been shown to induce expression of luciferase activity [25], as in Luc-IVS2-654 CHO cells described above. While HeLa cells are known to be sensitive to anthrax toxin [30], they have not been studied as extensively as CHO cells with regard to PA receptor expression. Nonetheless, Luc-IVS2-705 HeLa cells also demonstrated PA-facilitated cellular delivery of antisense PNA (Figure 4A). While antisense PNA(Lys)8 oligomers induced modest increases in luciferase expression in Luc-IVS2-705 HeLa cells in the absence of PA, induction of luciferase was substantially enhanced when PA-63 was added to Luc-IVS2-705 HeLa cell cultures, as in the CHO reporter cells.
Figure 4.
(A) Induced luciferase expression in Luc-IVS2-705 HeLa cells by 0.3µM antisense (IVS2-705) PNA(Lys)8 with and without PA-63 (1.0µg/mL). Results represent mean values ± SEM for 6 replicate studies. (B) Correction of aberrantly spliced βA-globin mRNA in erythroid cells of a β-thalassemia patient with the βIVS2-654 mutation by antisense PNA(Lys)8 (0.3µM) after incubation with the cells with and without PA-63 (0.3µg/mL).
PA also promoted effective delivery of antisense PNA(Lys)8 oligomers into erythroid precursor cells from a patient with β-thalassemia intermedia [IVS2-654(βo)/βE genotype]. Erythroid cells from this patient expressed β-globin genes with the IVS2-654 mutation on one allele, and incorrectly spliced β-globin gene transcripts resulting from this mutation could be detected in the cells by PCR. When antisense PNA(Lys)8 (as used in the studies of Luc-IVS2-654 CHO cells described above) was added to cultures of erythroid cells from this patient by itself, no change in aberrant β-globin splicing was evident. However, correctly spliced β-globin transcripts were clearly detectable when antisense PNA(Lys)8 was added to cultures together with PA-63 (Figure 4B).
These studies indicate that anthrax PA can serve as a vehicle for effective delivery of antisense PNA oligomers into various types of cells at nanomolar concentrations. While others have reported that the trans-membrane pore forming domain of diphtheria toxin can mediate delivery of oligonucleotides into cells [31], this finding has not been confirmed, and no studies of the delivery of PNA oligomers into cells by microbial toxin proteins have been reported previously.
Our interest in studying PNA and anthrax PA was based on several considerations. First, PNA oligomers are intrinsically stable and their pseudopeptide structure is amenable to modifications whereby peptide sequences can be added either during or following synthesis [1,9,15]. Second, anthrax PA, available as a recombinant protein, is known to be biocompatible and non-toxic by itself. Moreover, prior studies of anthrax PA provided cogent leads regarding modifications of PNA (e.g. addition of C-terminal lysines) that might allow PNA to interact with PA and use it as a vehicle for entry into cells [23], and it is possible that alternative adducts, such as peptide sequences derived from the LF (anthrax “lethal factor”) high-affinity PA binding site [20,23], might increase the efficiency of PA-mediated cellular delivery of PNA oligomers beyond that observed with PNA(Lys)8.
An additional attraction of PA as a vehicle for delivering antisense PNA oligomers into cells is that it may be amenable to modifications that confer cell selectivity to PNA delivery. The fusion toxin, DAB389IL-2 (or Ontak®), now used as an anti-cancer and immunosuppressive drug, exemplifies the potential pliability of microbial toxin proteins to achieve tissue specificity. Ontak®, a modified form of diphtheria toxin in which the native cell receptor-binding domain of the toxin has been replaced by the cytokine, IL-2, interacts only with cells that express high affinity IL-2 receptors [24,32,33]. Analogous modifications of the cell receptor-binding domain of anthrax PA might similarly allow tissue specific delivery of antisense PNA into cells. Replacement of the native cell receptor-binding domain of PA could also be advantageous to its potential for in vivo bioavailability by removing neutralizing antigenic epitopes [34].
Acknowledgments
The authors are indebted to Dr. David Chui, Professor of Medicine and Pathology, Boston University Medical Center, and to Dr. Edmond S.K. Ma, Assoc. Professor of Medicine, Division of Haematology, University of Hong Kong, Queen Mary Hospital, Hong Kong, PRC, for helping us obtain a blood sample from an untransfused patient with β-thalassemia intermedia [IVS2-654(βo)/βE genotype] for study. This work was supported in part by a grant from the National Cancer Institute, NIH: R21CA11228.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Eckstein F. The versatility of oligonucleotides as potential therapeutics. Expert Opin. Biol. Ther. 2007;7:1021–1034. doi: 10.1517/14712598.7.7.1021. [DOI] [PubMed] [Google Scholar]
- 2.Braasch DA, Corey DR. Novel antisense and nucleic acid strategies for controlling gene expression. Biochemistry. 2002;41:4503–4510. doi: 10.1021/bi0122112. [DOI] [PubMed] [Google Scholar]
- 3.Tamm I, Dorken B, Hartmann G. Antisense therapy in oncology: new hope for an old idea? Lancet. 2001;358:489–497. doi: 10.1016/S0140-6736(01)05629-X. [DOI] [PubMed] [Google Scholar]
- 4.Crooke ST. Molecular mechanisms of action of antisense drugs. Biochim. Biophys. Acta. 1999;1489:31–44. doi: 10.1016/s0167-4781(99)00148-7. [DOI] [PubMed] [Google Scholar]
- 5.Sazani P, Vacek MM, Kole R. Short-term and long-term modulation of gene expression by antisense therapeutics. Curr. Opin. Biotechnol. 2002;13:468–472. doi: 10.1016/s0958-1669(02)00366-x. [DOI] [PubMed] [Google Scholar]
- 6.Eckstein F. Phosphorothioate oligodeoxynucleotides: What is their origin and what is unique about them? Antisense Nucleic Acid Drug Dev. 2000;10:117–121. doi: 10.1089/oli.1.2000.10.117. [DOI] [PubMed] [Google Scholar]
- 7.Summerton J. Morpholino antisense oligomers: the case for an RNase H-independent structural type. Biochem. Biophys. Acta. 1999;1489:141–158. doi: 10.1016/s0167-4781(99)00150-5. [DOI] [PubMed] [Google Scholar]
- 8.Sohail M, Southern EM. Selecting optimal antisense reagents. Adv. Drug Delivery Rev. 2000;44:23–34. doi: 10.1016/s0169-409x(00)00081-8. [DOI] [PubMed] [Google Scholar]
- 9.Ray A, Norden AB. Peptide nucleic acid (PNA): its medical and technical applications and promise for the future. FASEB J. 2000;14:1041–1060. doi: 10.1096/fasebj.14.9.1041. [DOI] [PubMed] [Google Scholar]
- 10.Sazani P, Kang SH, Maier MA, Wei C, Dillman J, Summerton J, Manoharan M, Kole R. Nuclear antisense effects of neutral, anionic and cationic oligonucleotide analogs. Nucleic Acids Res. 2001;29:3965–3974. doi: 10.1093/nar/29.19.3965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sazani P, Kole R. Therapeutic potential of antisense oligonucleotides as modulators of alternative splicing. J. Clin. Invest. 2003;112:481–486. doi: 10.1172/JCI19547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Doyle DF, Braasch DA, Simmons CG, Janowski BA, Corey DR. Inhibition of gene expression inside cells by peptide nucleic acids: Effect of mRNA target sequence, mismatched bases, and PNA length. Biochemistry. 2001;40:53–64. doi: 10.1021/bi0020630. [DOI] [PubMed] [Google Scholar]
- 13.Nielsen PE, Egholm M, Berg RH, Buchardt O. Sequence selective recognition of DNA by strand displacement with a thymine substituted polyamide. Science. 1991;254:1497–1500. doi: 10.1126/science.1962210. [DOI] [PubMed] [Google Scholar]
- 14.Stein CA. Two problems in antisense biotechnology: in vitro delivery and the design of antisense experiments. Biochim. Biophys. Acta. 1999;1489:45–52. doi: 10.1016/s0167-4781(99)00143-8. [DOI] [PubMed] [Google Scholar]
- 15.Koppelhus U, Nielsen PE. Cellular delivery of peptide nucleic acid (PNA) Adv. Drug Delivery Rev. 2003;55:267–280. doi: 10.1016/s0169-409x(02)00182-5. [DOI] [PubMed] [Google Scholar]
- 16.Sazani P, Gemignani F, Kang S-H, Maier MA, Manoharan M, Persmark M, Bortner D, Kole R. Systemically delivered antisense oligomers upregulate gene expression in mouse tissues. Nature Biotechnol. 2002;20:1228–1233. doi: 10.1038/nbt759. [DOI] [PubMed] [Google Scholar]
- 17.Cutrona G, Carpaneto EM, Ulivi M, Roncella S, Landt O, Ferrarini M, Boffa LC. Effect in live cells of a c-myc anti-gene PNA linked to a nuclear localization signal. Nature Biotechnol. 2000;18:300–303. doi: 10.1038/73745. [DOI] [PubMed] [Google Scholar]
- 18.Rasmussen FW, Bendifallah N, Zachar V, Shiraishi T, Fink T, Ebbesen P, Nielsen PE, Koppelhus U. Evaluation of transfection protocols for unmodified and modified peptide nucleic acid (PNA) oligomers. Oligonucleotides. 2006;16:43–57. doi: 10.1089/oli.2006.16.43. [DOI] [PubMed] [Google Scholar]
- 19.vanderSpek JC, Mindel J, Finkelstein A, Murphy JR. Structure function analysis of the transmembrane domain of the interleukin-2 receptor targeted fusion toxin DAB389IL-2: The amphipathic helical region of the transmembrane is essential for the efficient delivery of the catalytic domain to the cytosol of target cells. J. Biol. Chem. 1993;268:12077–12082. [PubMed] [Google Scholar]
- 20.Ratts R, Zeng H, Berg EA, Blue C, McComb ME, Costello CE, vanderSpek JC, Murphy JR. The cytosolic entry of diphtheria toxin catalytic domain requires a host cell cytosolic translocation factor complex. J. Cell Biol. 2003;160:1139–1150. doi: 10.1083/jcb.200210028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Escuyer V, Collier RJ. Anthrax protective antigen interacts with a specific receptor on the surface of CHO-K1 cells. Infect. Immun. 1991;59:3381–3386. doi: 10.1128/iai.59.10.3381-3386.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wesche J, Elliott JL, Falnes PO, Olsnes SZ, Collier RJ. Characterization of membrane translocation by anthrax protective antigen. Biochemistry. 1998;37:15737–15746. doi: 10.1021/bi981436i. [DOI] [PubMed] [Google Scholar]
- 23.Blanke SR, Milne JC, Benson EL, Collier RJ. Fused polycationic peptide mediates delivery of diphtheria toxin A chain to the cytosol in the presence of anthrax protective antigen. Proc. Natl. Acad. Sci. (USA) 1996;93:8437–8442. doi: 10.1073/pnas.93.16.8437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Williams D, Parker K, Bishai W, Borowski M, Genbauffe F, Strom TB, Murphy JR. Diphtheria toxin receptor binding domain substitution with interleukin-2: genetic construction and properties of the diphtheria toxin-related interleukin-2 fusion protein. Protein Engn. 1987;1:493–498. doi: 10.1093/protein/1.6.493. [DOI] [PubMed] [Google Scholar]
- 25.Kang S-H, Cho M-J, Kole R. Up-regulation of luciferase expression with antisense oligonucleotides: Implications and applications in functional assay development. Biochemistry. 1998;37:6235–6239. doi: 10.1021/bi980300h. [DOI] [PubMed] [Google Scholar]
- 26.Partridge M, Vincent A, Matthews P, Puma J, Stein D, Summerton J. A simple method for delivering morpholino antisense oligos into the cytoplasm of cells. Antisense Nucleic Acid Drug Dev. 1996;6:169–175. doi: 10.1089/oli.1.1996.6.169. [DOI] [PubMed] [Google Scholar]
- 27.Brasier AR, Tate JE, Habener JF. Optimized use of the firefly luciferase assay as a reporter gene in mammalian cell lines. BioTechniques. 1989;7:1116–1122. [PubMed] [Google Scholar]
- 28.Harriman WD, Wabl M. A video technique for quantification of DNA in gels stained with ethidium bromide. Anal. Biochem. 1995;228:336–342. doi: 10.1006/abio.1995.1360. [DOI] [PubMed] [Google Scholar]
- 29.Lacerra G, Sierakowska H, Carestia C, Fucharoen S, Suumerton J, Weller D, Kole R. Restoration of hemoglobin A synthesis in erythroid cells from peripheral blood of thalassemic patients. Proc. Natl. Acad. Sci.(USA) 2000;97:9591–9596. doi: 10.1073/pnas.97.17.9591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chen KH, Liu S, Bankston LA, Liddington RC, Leppla SH. Selection of anthrax toxin protective antigen variants that discriminate between the cellular receptors TEM8 and CMG2 and achieve targeting of tumor cells. J. Biol. Chem. 2007;282:9834–9845. doi: 10.1074/jbc.M611142200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Uherek C, Fominaya J, Wels W. A modular DNA carrier protein based on the structure of Diphtheria toxin mediates target cell-specific gene delivery. J. Biol. Chem. 1998;273:8835–8841. doi: 10.1074/jbc.273.15.8835. [DOI] [PubMed] [Google Scholar]
- 32.Foss F. Clinical experience with denileukin diflitox (ONTAK) Semin. Oncol. 2006;33:S11–S16. doi: 10.1053/j.seminoncol.2005.12.017. [DOI] [PubMed] [Google Scholar]
- 33.Bolanos-Meade J, Vogelsang GB. Novel strategies for steroid-refractory acute graft versus host disease. Curr. Opin. Hematol. 2005;12:40–44. doi: 10.1097/01.moh.0000148763.12733.bb. [DOI] [PubMed] [Google Scholar]
- 34.Brossier F, Lévy M, Landier A, Lafaye P, Mock M. Functional analysis of Bacillus anthracis protective antigen by using neutralizing monoclonal antibodies. Infect. Immun. 2004;72:6313–6317. doi: 10.1128/IAI.72.11.6313-6317.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]