Abstract
Context:
Carbohydrate ingestion has recently been associated with elevated core temperature during exercise in the heat when testing for ergogenic effects. Whether the association holds when metabolic rate is controlled is unclear. Such an effect would have undesirable consequences for the safety of the athlete.
Objective:
To examine whether ingesting fluids containing carbohydrate contributed to an accelerated rise in core temperature and greater overall body heat production during 1 hour of exercise at 30°C when the effort was maintained at steady state.
Design:
Crossover design (repeated measures) in randomized order of treatments of drinking fluids with carbohydrate and electrolytes (CHO) or flavored-water placebo with electrolytes (PLA). The beverages were identical except for the carbohydrate content: CHO = 93.7 ± 11.2 g, PLA = 0 g.
Setting:
Research laboratory.
Patients or Other Participants:
Nine physically fit, endurance-trained adult males.
Intervention(s):
Using rectal temperature sensors, we measured core temperature during 30 minutes of rest and 60 minutes of exercise at 65% of maximal oxygen uptake (V̇o2 max) in the heat (30.6°C, 51.8% relative humidity). Participants drank equal volumes (1.6 L) of 2 beverages in aliquots 30 minutes before and every 15 minutes during exercise. Volumes were fixed to approximate sweat rates and minimize dehydration.
Main Outcome Measure(s):
Rectal temperature and metabolic response (V̇o2, heart rate).
Results:
Peak temperature, rate of temperature increase, and metabolic responses did not differ between beverage treatments. Initial hydration status, sweat rate, and fluid replacement were also not different between trials, as planned.
Conclusions:
Ingestion of carbohydrate in fluid volumes that minimized dehydration during 1 hour of steady-state exercise at 30°C did not elicit an increase in metabolic rate or core temperature.
Keywords: rectal temperature, glucose, fructose, thermoregulation, heat stress
Key Points.
Fluid ingestion is a strategy that minimizes dehydration and attenuates the rise in core temperature by maintaining plasma volume. Carbohydrate-electrolyte drinks are often used for this strategy.
The gradient between body temperature and the environment may also be a factor when investigators determine if the effect of extreme environmental conditions, exercise duration and intensity, carbohydrate dose, and compromised hydration status should be considered.
Under controlled conditions, elevated core temperature did not appear to be a risk when beverages containing carbohydrate were ingested at a rate sufficient to maintain hydration during steady-state exercise.
Exercise in warm, humid environments increases core body temperature and can cause heat storage in the body. Heat storage increases sweat rate, which may induce dehydration. Independent of hydration status, severe heat storage promotes fatigue and increases the risk of exertional heat stroke. Fluid ingestion is a strategy that minimizes dehydration and attenuates the rise in core temperature by maintaining plasma volume, which helps to sustain cardiac output and skin blood flow for heat dissipation.1,2 Sports drinks, which contain carbohydrate (CHO), are often used for this strategy.
Presently, the effect of CHO ingestion on core body temperature response during exercise in the heat is unclear. Research indicates that core temperature could be elevated in association with such intake, but studies are confounded by maximal performance efforts or differences in hydration status from uncontrolled fluid ingestion. In several relatively recent studies on exercise performance,3–6 CHO intake was associated with more work or higher power outputs and elevated core temperatures. A higher metabolic rate associated with ergogenicity could explain this; however, one group3 demonstrated that when performance was similar, core temperature was elevated during the CHO trial. Authors of older studies involving sustained exercise that finished with a maximal-effort performance task reported a trend for higher core temperatures for CHO versus placebo,7 no effect of CHO,8 or no differences.9
Results from studies in which ad libitum drinking occurred or the volume was fixed to produce dehydration were also confounded. Fluid intake was typically greater for the beverage containing CHO and electrolytes, resulting in less dehydration compared with the effects of the placebo.10–15 Despite more complete hydration during the CHO trial, the authors consistently failed to show a difference in core temperature response. Enhanced hydration could mask a CHO effect on core temperature if one exists. The larger volume of CHO-electrolyte fluid ingested10 or the composition of the CHO-electrolyte beverage when volume is similar16–18 preserves the plasma volume, which could enhance thermoregulation. In one of the few studies with controlled intake and exercise intensity,19 core temperature did not differ for water or a CHO-electrolyte drink, but all 4 participants experienced a reduction in body weight, and the exercise was done in mild environmental conditions (approximately 25°C).
Clarifying whether CHO elevates body core temperature during exercise in warm or hot environments requires a fixed volume of fluid consumption, steady-state exercise without performance efforts, and control of hydration status. Our purpose was to determine whether ingesting CHO in a beverage resulted in greater overall heat production, greater peak core temperature, and faster rise in core temperature when steady-state metabolism was maintained throughout 1 hour of exercise in the heat. We compared a CHO beverage with a similarly flavored placebo of equal volume but containing no CHO and standardized the electrolyte content, which has been done previously. We hypothesized that when exercise intensity was maintained at a constant pace and fluid intake prevented dehydration based on body weight change, core temperature would not be elevated by the CHO treatment because the body was capable of absorbing or dissipating any additional heat.
Methods
Participants
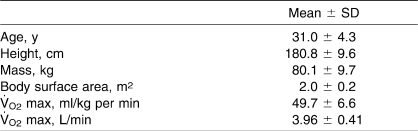
Nine endurance-trained males between the ages of 24 and 37 years who regularly competed in road cycling races participated in the study. Physical characteristics are presented in Table 1. The athletes had no known gastrointestinal, metabolic, cardiovascular, or pulmonary disorders or diseases and no known orthopaedic injury. Before participating, all volunteers read and signed an informed consent approved by the institutional Human Subjects Review Committee (which also approved the study).
Table 1.
Participant Physical Characteristics
Standardization for Experimental Treatments
We conducted all tests during an approximately 4-week period of the same climatic season, with volunteers maintaining a consistent training program to minimize the effects of heat acclimatization. We measured maximal oxygen uptake (V̇o2max) and familiarized participants with the study design and methods during an orientation session before the experimental trials. Maximal oxygen uptake was determined during a ramped cycle ergometer protocol. Indirect calorimetry was used to measure oxygen uptake (V̇o2) and carbon dioxide uptake (Vco2), which were then entered into a regression analysis along with workload data, from which an unknown workload corresponding to 65% V̇o2max was predicted. The cycle ergometer (Excaliber Sport, Lode BV, Groningen, Netherlands) used to determine V̇o2max was also used for the experimental trial.
During the familiarization trial, sweat rate was estimated by adding the mass of fluid ingested ad libitum during 1 hour of exercise to change in body mass as measured by nude weighing of the volunteers. On a per-kilogram of body weight basis, the sweat rate averaged 4 mL/kg. Sweat rate was used to ensure that the total volume of fluid needed during the experimental trials would maintain body weight. A priori, we set fluid intake at 4 mL/kg and divided the total absolute total volume for each participant by 5 to determine the aliquot to be administered at each of 5 feedings. Volunteers were also instructed in the use of a rectal thermister (series 400 9FR; NovaMed, Rye, NY). Before the study, this unit was calibrated against a mercurial thermometer and standard water bath. Participants did not exercise or consume alcohol or caffeine for 1 day before testing.
We instructed volunteers to maintain their normal diet the day before the experiment and to record all foods and beverages consumed. To ensure adequate hydration upon arrival to the laboratory for experimental trials, they consumed a 720-mL bottle of a sports drink and 500-mL bottle of water. Participants consumed the sports drink in addition to normal daily fluid intake over the course of the day and evening before the experiment; the water was consumed during the morning of the experiment, at least 2 hours before the start time. The volunteers did not eat or drink (other than the prescribed water) after midnight the night before the experiment.
Experimental Trials
For each trial, participants arrived at the laboratory before 9:00 am, had their diet records reviewed to assure consistent diet control, and voided their bladders. The urine specific gravity was measured to confirm euhydration, and nude body mass was recorded. Each participant wore a heart rate monitor (model T31; Polar Electro Inc, Lake Success, NY) on the chest and inserted a rectal thermister approximately 10 cm past the anal sphincter. The rectal probe was stabilized using surgical tape on the small of the back in the lower lumbar region. Initial rectal temperature was read to ensure that the resting temperature of all volunteers was in the normal range.
Rest Phase
Participants were seated (resting) in a semireclined, upright position for approximately 30 minutes after preparation. Immediately after being seated, participants drank the first of the 5 aliquots of 1 of 2 randomly assigned treatment beverages. The drinks administered were a flavored CHO-electrolyte beverage (CHO: 6% CHO, approximately 18 mmol/L Na+, approximately 3 mmol/L K+) and a similarly flavored placebo (PLA: 0% CHO, approximately 18 mmol/L Na+, approximately 3 mmol/L K+). The CHO used was a blend of sucrose, glucose, and fructose, a mixture readily absorbed through active transport mechanisms20–22 and oxidized.23,24 The total CHO amount was small (approximately 93 g) and was spread over the duration of exercise to reflect fluid intake before and during exercise. We chose a 6% concentration of CHO because it represented the level and type of CHO used by the authors3,6 of 2 prior studies of core temperature, and the portion consumed during exercise approximated the recommended level of CHO intake per hour of exercise for exogenous energy provision.25 Participants drank through a straw in a 250-mL flask that was previously immersed in a water bath stabilized at 37°C (98.6°F) to minimize any influence on core temperature measurements. Actual drink temperature was 36.9 ± 0.3°C. Participants were required to ingest the total volume of the assigned beverage within 2 minutes immediately before the designated 30-minute rest period began. Every 5 minutes, we recorded rectal temperatures and heart rates. Every 15 minutes, volunteers rated perceptions of thermal comfort (1 = comfortable to 4 = very uncomfortable) and ambient heat (−4 = very cold to 4 = very hot), according to the survey used by Meyer et al,26 and rated perceived exertion (RPE27; Borg Scale = 6 to 20). Respiratory exchange ratio (RER) and V̇o2 were recorded continuously with a metabolic cart (Quinton QMC; Quinton, Bothell, WA) and used to calculate resting energy expenditure and metabolic heat production. Respiratory gas was collected using a 2-way nonrebreathing valve (model 2700B; Hans Rudolph Inc, Shawnee, KS) with mouthpiece and nose clips. The valve was supported with a headgear (model 2726; Hans Rudolph Inc). Environmental conditions were maintained at 30.6 ± 1.0°C dry bulb temperature and 51.8 ± 6.8% relative humidity.
Exercise Phase
Immediately before transitioning to the exercise period and after 15, 30, and 45 minutes of exercise, participants drank the remaining aliquots of assigned beverage within 2 minutes. They exercised for 60 minutes on a stationary cycle ergometer at an intensity equivalent to 65 ± 0.05% V̇o2max. Heart rate and measures of core temperature were recorded before and every 5 minutes during exercise; RPE and perceptions of thermal comfort ambient heat ratings were recorded every 15 minutes. All measurements were taken before drinking. Expired gases were collected for 2 minutes at 7, 22, 37, and 52 minutes of exercise using Douglas bags. Respiratory gases were analyzed using oxygen and carbon dioxide analyzers (models S-3A/I and CD-3A; AMETEK Inc, Naperville, IL), and gas volume was determined using spirometry (model DTM-32F; Vacumed Inc, Ventura, CA). The V̇o2 and Vco2 measures were taken 5 minutes after drinking was completed. Immediately postexercise, participants dismounted from the bicycle, removed the rectal probe, and dried themselves with towels before being reweighed in the nude.
Analytic Procedures
We took several approaches to quantify core temperature response. The slope of the rate of change in core temperature from the beginning to the end of exercise was determined using linear regression. Heat production, determined using indirect calorimetry at the 4 measurement times, was averaged for 60 minutes of exercise. Using the trapezoid rule and computations of GraphPad Prism (version 4.00 for Windows; GraphPad Software, San Diego, CA), we calculated the area under the curve for core temperature for the rest phase and periods of measurement during exercise.
Statistical Analyses
Using published SDs and rectal temperatures that showed a mean difference of 0.3°C between trials with and without CHO feedings3 and assuming a correlation coefficient of 0.75 to represent an expected consistent temperature response of the participants independent of ingesting fluids with or without CHO, we calculated that a sample size of 7 would provide statistical power of 80% for finding a difference at a probability level of .05 (Power and Precision Software; Biostat, Englewood, NJ). To allow for a margin of error, we tested a sample size of 9 volunteers.
Paired t tests were used to compare the treatment effect on the rate of change of temperature during exercise and for the area under the curve for temperature as estimated by the rectal probe. Knowing that differences would exist between rest and exercise, we analyzed these 2 phases separately for a beverage effect. One-way analysis of variance was used to detect the statistical significance (P < .05) of mean differences between treatments for V̇o2, RER, heart rate, and energy expenditure during rest and during exercise. Two-way analysis of variance, adjusted for repeated measures, was used to evaluate beverage-by-time effects (P < .05) for RPE, perceived thermal comfort, and ambient heat.
Results
When participants reported to the laboratory, their urine specific gravity was not different between trials (CHO = 1.008 ± 0.005, PLA = 1.009 ± 0.008). Average cycling workload was 179 ± 22 W, and no difference was noted in the relative intensity of exercise (%V̇o2max) between CHO (65.3 ± 0.05%) and PLA (65.1 ± 0.05%).
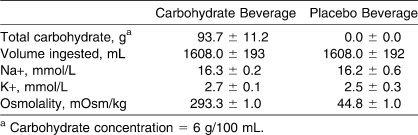
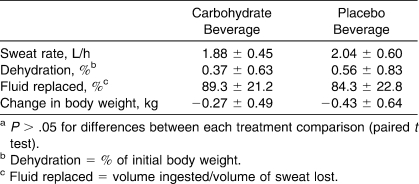
The volume of beverage consumed was controlled (Table 2), and the total amount of CHO ingested during the CHO trial was 93.76 ± 11.23 g. No beverage treatment effects were seen for sweat loss (CHO = 1.88 ± 0.45 L, PLA = 2.04 ± 0.60 L, P > .05), percentage of sweat loss replaced (CHO = 89.3 ± 21.2%, PLA = 84.3 ± 22.8%, P > .05), or percentage of body weight lost due to dehydration (Table 3). As planned, the drinking protocol resulted in minimal change in body weight.
Table 2.
Beverage Treatments (Mean ± SD)
Table 3.
Fluid Balance Data (Mean ± SD)a
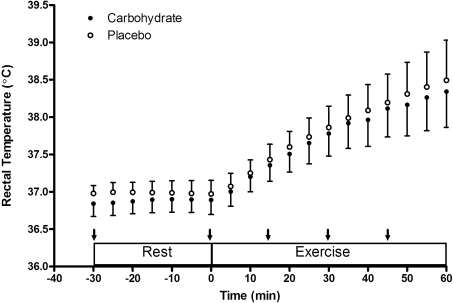
Rectal temperature data are presented in Figure 1. No differences due to the drink treatments were detected for mean or peak temperatures at rest or during exercise (Table 4). The rate of increase in core temperature during exercise was 0.025 ± 0.002°C·min−1 during CHO and 0.026 ± 0.002°C·min−1 during PLA (P > .05). The effect size for the rate of core temperature increase was 0.5, whereas the effect size for peak temperature was 0.29.
Figure 1. Rectal temperature (mean ± SD) during rest and exercise. Arrows indicate the timing of beverage administration. Rest versus exercise, P < .05; no difference between treatments, P > .05.
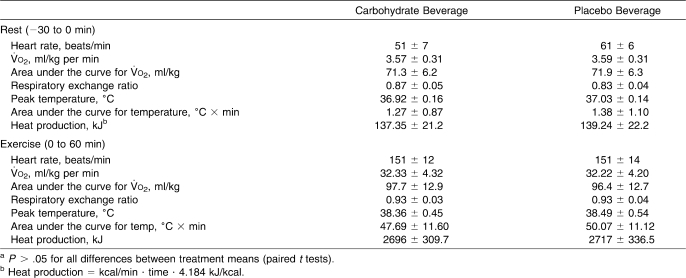
Table 4.
Cardiovascular and Metabolic Responses (Mean ± SD)a
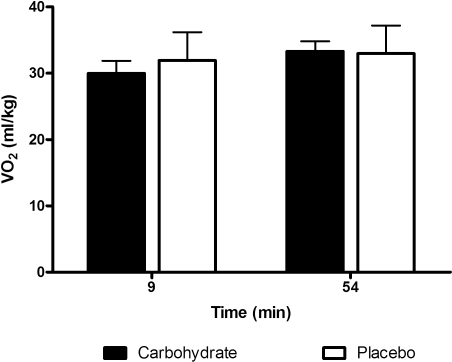
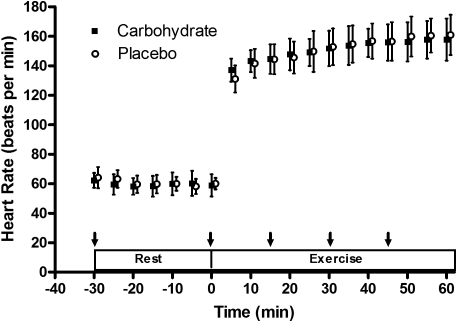
Results for heart rate, metabolic rate, and heat production are presented in Table 4. As expected, these variables increased during exercise. However, no differences were observed between beverage treatments at rest or during exercise. We calculated the area under the curve for the V̇o2 response and core temperature and found no differences in mean values for the beverage treatments within the rest or exercise phases. Figure 2 confirms the similarity of mean V̇o2 measurements during the first and final measurements for the treatments. Figure 3 shows the consistency of the heart rate response for the treatments. A slight elevation in RER during rest for the CHO trial was not statistically different from that for the PLA.
Figure 2. Oxygen uptake (V̇o2) values (mean ± SD) measured early and late during exercise under each treatment condition. No differences existed for time or between treatments (P >.05).
Figure 3. Heart rate (mean ± SD) measured at rest and during exercise during intake of fluids with carbohydrate and placebo. Arrows indicate the timing of the beverage administration. Rest versus exercise, P < .05; no differences existed between treatments (P > .05).
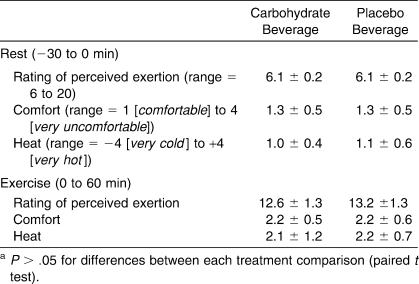
Mean values for the ratings of perceived comfort, heat, and perceived exertion during rest and exercise are presented in Table 5. All ratings increased during exercise but were unaffected by the drink treatments (P >.05).
Table 5.
Perceptual Responses and Ratings (Mean ± SD)a
Discussion
The purpose of our study was to determine whether CHO in fluid ingested during 1 hour of steady-state exercise in the heat would accelerate the rise in core temperature or elicit greater heat production, resulting in an elevated core temperature. This concern was raised by Montain and Coyle,1 who examined graded dehydration by feeding participants with fluids containing CHO but did not test for a CHO effect because they did not include a CHO-free control beverage. Subsequently, several groups3–6 have reported elevations in core temperature during exercise performance testing when CHO was ingested. These studies involved various durations of exercise sessions (60–130 minutes) and included performance testing at varied intensities4–6; hence, the design of these studies did not allow for a clear conclusion regarding a CHO effect. The potential for CHO intake to elevate core temperature during exercise warranted further investigation because of implicated effects on overheating, fatigue, and the risk of heat illness in athletes.
The protocol for our study consisted of consuming fluid 30 minutes before and every 15 minutes during steady-state exercise, a pattern that was based on recommendations to prevent dehydration during exercise25,28,29 and similar to that used in earlier research in which core temperature elevation was reported.3–6 Our participants ingested a total of 93.7 g of CHO immediately before 30 minutes of rest and during the first 45 minutes of the 1-hour bout of exercise. Carbohydrate concentration of the fluid was similar to that in prior studies, and CHO was administered to our volunteers at a comparable rate (g/kg body weight).3,6 Our participants received 0.016 g CHO/kg body weight·min−1 during the observation, which was within the range of the 0.012 to 0.023 g/kg·min−1 used previously by authors3–6 reporting the CHO effect on core temperature. Exercise increased core temperature as expected, but we did not detect a difference in core temperature when comparing the 2 beverage treatments, which differed only by the presence of CHO. The effect size for the CHO influence on core temperature ranged from 0.3 to 0.5, with variability (SD) exceeding the mean difference in the rate of change of core temperature. In addition, we did not observe an increase in mean V̇o2 at rest or during exercise as a result of the CHO feeding.
Aside from varying exercise intensity and metabolic rate during exercise, other factors exist to explain the rise in core temperature observed previously in association with CHO feedings. In prior research,3–6 body mass was not maintained during exercise. The acute reduction in body mass ranged from 0.7% to 4.4%, suggesting that dehydration might have an effect and promote an elevation in core temperature. The findings of Fritzsche et al3 support an interaction with hydration. Within the trials that produced similar power output, ingesting CHO without fluids during 2 hours of exercise resulted in elevated core temperature compared with the temperature when ingesting nothing. Both trials resulted in similar dehydration amounts of 4%.3 When the same dose of CHO was ingested with fluid to minimize dehydration (1% reduction in body mass), core temperature was approximately 0.75°C lower than when CHO was ingested without fluids. Interestingly, during the CHO trial with fluids, volunteers generated more metabolic work (greater power output). We designed our investigation to control for dehydration and minimize the change in body mass during exercise to remove this potential confounding factor.
The gradient between body temperature and the environment may also be a factor in establishing whether CHO ingested during exercise raises core temperature. In one of the earlier studies19 on steady-state exercise in which core temperature was similar with and without CHO, participants severely underconsumed beverage and experienced dehydration of approximately 5%. However the environment was much milder than in more recent studies (approximately 25°C). Similar to previous authors,3–6 we reported the CHO-induced core temperature elevation using environmental conditions that were more extreme. As they did, we controlled the relative intensity, and volunteers sustained efforts at 65% of peak V̇o2. Subsequent researchers should investigate the interactive effects of more extreme environmental conditions, exercise duration and intensity, CHO dose, and compromised hydration status to clarify the feeding effect of CHO during exercise on core temperature response.
A final, but unlikely, possibility for an exaggerated elevation in core temperature associated with CHO intake in prior studies is because of the thermogenic effect of feeding.30–32 With glucose ingestion, metabolic rate increases by 5% to 6% of the energy content of the feeding (75 g of glucose ingested in 5 minutes) and 5% to 10% over basal metabolic rate.30,33,34 Fructose can also increase resting metabolism by as much as 10%.33,34 In our study, the CHO sources were sucrose, glucose, and fructose in amounts that contributed nearly a 50:50 mixture of glucose and fructose. This blend is rapidly absorbed20–22 and oxidized during exercise at higher rates than a single form of carbohydrate.23,24 Given that heat production during exercise is dramatically greater than at rest,35 either any thermogenic effect of feeding is likely within the error of our measurements or volunteers were capable of absorbing or dissipating this small amount of heat without raising core temperature. Unlike rest conditions, CHO would not be expected to elicit an elevation in metabolic rate during exercise of more than 1% of the energy production in our study.
Conclusions
We found no evidence that the acute intake of CHO immediately before and during 1 hour of exercise altered the core temperature response compared with a no-CHO trial. This was likely due to maintaining a constant metabolic rate for the treatments throughout exercise and preventing differences in hydration by administering adequate fluid intake to replace sweat loss, unlike authors of previous studies, who varied hydration status and intensity of exercise. We did not observe a core temperature or metabolic response with the CHO feeding, which may have resulted from the modest dose of CHO provided intermittently over 75 minutes of rest and exercise and the body's ability to dissipate or absorb such a small amount of heat without raising core temperature. Ingesting sufficient fluid to minimize dehydration during exercise optimizes heat dissipation. It is not clear whether an ergogenic effect supported by CHO ingestion could raise core temperature to a level of safety concern. However, the reported elevation in core temperature associated with physical performance benefits when fluid with CHO is ingested is relatively small3–6 compared with the response of core temperature when fluid intake is avoided and significant dehydration occurs.1,3 Based on our findings, elevated core temperature does not appear to be a risk when beverages containing CHO are ingested at a rate to maintain hydration during steady-state exercise.
Acknowledgments
Craig A. Horswill, PhD, and John R. Stofan, MS, are employees of the Gatorade Company and work as scientists at the Gatorade Sports Science Institute (GSSI). Shannon C. Lovett and Chris Hannasch were interns who worked on this project at GSSI.
Footnotes
Craig A. Horswill, PhD, contributed to conception and design; analysis and interpretation of the data; and drafting, critical revision, and final approval of the manuscript. John R. Stofan, MS, contributed to conception and design; acquisition and analysis and interpretation of the data; and drafting, critical revision, and final approval of the article. Shannon C. Lovett contributed to conception and design, acquisition and analysis and interpretation of the data, and final approval of the article. Chris Hannasch contributed to acquisition and analysis and interpretation of the data and drafting and final approval of the article.
References
- 1.Montain S.J, Coyle E.F. Influence of graded dehydration on hyperthermia and cardiovascular drift during exercise. J Appl Physiol. 1992;73(4):1340–1350. doi: 10.1152/jappl.1992.73.4.1340. [DOI] [PubMed] [Google Scholar]
- 2.Pitts G.C, Johnson R.E, Consolazio F.C. Work in the heat as affected by intake of water, salt, and glucose. Am J Physiol. 1944;142:253–259. [Google Scholar]
- 3.Fritzsche R.G, Switzer T.W, Hodgkinson B.J, Lee S.H, Martin J.C, Coyle E.F. Water and carbohydrate ingestion during prolonged exercise increase maximal neuromuscular power. J Appl Physiol. 2000;88(2):730–737. doi: 10.1152/jappl.2000.88.2.730. [DOI] [PubMed] [Google Scholar]
- 4.Gant N, Leiper J.B, Williams C. Gastric emptying of fluids during variable-intensity running in the heat. Int J Sport Nutr Exerc Metab. 2007;17(3):270–283. doi: 10.1123/ijsnem.17.3.270. [DOI] [PubMed] [Google Scholar]
- 5.Millard-Stafford M.L, Sparling P.B, Rosskopf L.B, Snow T.K. Should carbohydrate concentration of a sports drink be less than 8% during exercise in the heat. Int J Sport Nutr Exerc Metab. 2005;15(2):117–130. doi: 10.1123/ijsnem.15.2.117. [DOI] [PubMed] [Google Scholar]
- 6.Morris J.G, Nevill M.E, Thompson D, Collie J, Williams C. The influence of a 6.5% carbohydrate-electrolyte solution on performance of prolonged intermittent high-intensity running at 30 degrees C. J Sport Sci. 2003;21(5):371–381. doi: 10.1080/0264041031000071191. [DOI] [PubMed] [Google Scholar]
- 7.Davis J.M, Lamb D.R, Pate R.R, Slentz C.A, Burgess W.A, Bartoli W.P. Carbohydrate-electrolyte drinks: effects on endurance cycling in heat. Am J Clin Nutr. 1988;48(4):1023–1030. doi: 10.1093/ajcn/48.4.1023. [DOI] [PubMed] [Google Scholar]
- 8.Davis J.M, Burgess W.A, Slentz C.A, Bartoli W.P, Pate R.R. Effects of ingesting 6% and 12% glucose/electrolyte beverages during prolonged intermittent cycling in the heat. Eur J Appl Physiol Occup Physiol. 1988;57(5):563–569. doi: 10.1007/BF00418463. [DOI] [PubMed] [Google Scholar]
- 9.Murray R, Paul G.L, Seifert J.G, Eddy D.E. Responses to varying rates of carbohydrate ingestion during exercise. Med Sci Sports Exerc. 1991;23(6):713–718. [PubMed] [Google Scholar]
- 10.Baker L.B, Munce T.A, Kenney W.L. Sex differences in voluntary fluid intake by older adults during exercise. Med Sci Sports Exerc. 2005;37(5):789–796. doi: 10.1249/01.mss.0000162622.78487.9c. [DOI] [PubMed] [Google Scholar]
- 11.Clapp A.J, Bishop P.A, Smith J.F, Mansfield E.R. Effects of carbohydrate-electrolyte content of beverages on voluntary hydration in a simulated industrial environment. Am Ind Hyg Assoc J. 2000;61(5):692–699. doi: 10.1080/15298660008984579. [DOI] [PubMed] [Google Scholar]
- 12.Clapp A.J, Bishop P.A, Walker J.L. Fluid replacement preferences in heat-exposed workers. Am Ind Hyg Assoc J. 1999;60(6):747–751. doi: 10.1080/00028899908984497. [DOI] [PubMed] [Google Scholar]
- 13.Rivera-Brown A, Gutierrez R, Gutierrez J.C, Frontera W, Bar-Or O. Drink composition, voluntary drinking, and fluid balance in exercising, trained, heat-acclimatized boys. J Appl Physiol. 1999;86(1):78–84. doi: 10.1152/jappl.1999.86.1.78. [DOI] [PubMed] [Google Scholar]
- 14.Wilk B, Bar-Or O. Effect of drink flavor and NaCl on voluntary drinking and hydration in boys exercising in the heat. J Appl Physiol. 1996;80(4):1112–1117. doi: 10.1152/jappl.1996.80.4.1112. [DOI] [PubMed] [Google Scholar]
- 15.Wilk B, Kriemler S, Keller H, Bar-Or O. Consistency in preventing voluntary dehydration in boys who drink a flavored carbohydrate-NaCI beverage during exercise in the heat. Int J Sport Nutr. 1998;8(1):1–9. doi: 10.1123/ijsn.8.1.1. [DOI] [PubMed] [Google Scholar]
- 16.Below P.R, Mora-Rodriguez R, Gonzalez-Alonso J, Coyle E.F. Fluid and carbohydrate ingestion independently improve performance during 1 h of intense exercise. Med Sci Sports Exerc. 1995;27(2):200–210. [PubMed] [Google Scholar]
- 17.Candas V, Libert J.P, Bradenberger G, Sagot J.C, Amoros C, Kahn JM. Hydration during exercise: effects on thermal and cardiovascular adjustments. Eur J Appl Physiol. 1986;55:113–122. doi: 10.1007/BF00714992. [DOI] [PubMed] [Google Scholar]
- 18.Carter J.E, Gisolfi C.V. Fluid replacement during and after exercise in the heat. Med Sci Sports Exerc. 1989;21(5):532–539. [PubMed] [Google Scholar]
- 19.Costill D.L, Krammer W.F, Fisher A. Fluid ingestion during distance running. Arch Environ Health. 1970;21(4):520–525. doi: 10.1080/00039896.1970.10667282. [DOI] [PubMed] [Google Scholar]
- 20.Ryan A.J, Lambert G.P, Shi X, Chang R.T, Summers R.W, Gisolfi C.V. Effect of hypohydration on gastric emptying and intestinal absorption during exercise. J Appl Physiol. 1998;84(5):1581–1588. doi: 10.1152/jappl.1998.84.5.1581. [DOI] [PubMed] [Google Scholar]
- 21.Schedl H.P, Maughan R.J, Gisolfi C.V. Intestinal absorption during rest and exercise: implications for formulating an oral rehydration solution (ORS) Med Sci Sports Exerc. 1994;26(3):267–280. [PubMed] [Google Scholar]
- 22.Shi X, Summers R.W, Schedl H.P, Flanagan S.W, Chang R, Gisolfi C.V. Effects of carbohydrate type and concentration and solution osmolality on water absorption. Med Sci Sports Exerc. 1995;27(12):1607–1615. [PubMed] [Google Scholar]
- 23.Adopo E, Peronnet F, Massicotte D, Brisson G.R, Hillaire-Marcel C. Respective oxidation of exogenous glucose and fructose given in the same drink during exercise. J Appl Physiol. 1994;76(3):1014–1019. doi: 10.1152/jappl.1994.76.3.1014. [DOI] [PubMed] [Google Scholar]
- 24.Jentjens R.L, Underwood K, Achten J, Currell K, Mann C.H, Jeukendrup A.E. Exogenous carbohydrate oxidation rates are elevated after combined ingestion of glucose and fructose during exercise in the heat. J Appl Physiol. 2006;100(3):807–816. doi: 10.1152/japplphysiol.00322.2005. [DOI] [PubMed] [Google Scholar]
- 25.American College of Sports Medicine; Sawka MN, Burke LM, Eichner ER, Maughan RJ, Montain SJ, Stachenfeld NS. Position stand: exercise and fluid replacement. Med Sci Sports Exerc. 2007;39(2):377–90. doi: 10.1249/mss.0b013e31802ca597. [DOI] [PubMed] [Google Scholar]
- 26.Meyer F, Bar-Or O, Wilk B. Children's perceptual responses to ingesting drinks of different compositions during and following exercise in the heat. Int J Sport Nutr. 1995;5(1):13–24. doi: 10.1123/ijsn.5.1.13. [DOI] [PubMed] [Google Scholar]
- 27.Borg G. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5):377–381. [PubMed] [Google Scholar]
- 28.American College of Sports Medicine; Convertino VA, Armstrong LE, Coyle EF, et al. Position stand: exercise and fluid replacement. Med Sci Sports Exerc. 1996;28(1):i–vii. doi: 10.1097/00005768-199610000-00045. [DOI] [PubMed] [Google Scholar]
- 29.Casa D.J, Armstrong L.A, Hillman S.K, Montain S.J, Reiff R.V, Rich B.S.E, et al. National Athletic Trainers' Association position statement: fluid replacement for athletes. J Athl Train. 2000;35(2):212–224. [PMC free article] [PubMed] [Google Scholar]
- 30.Acheson K.J, Ravussin E, Wahren J, Jequier E. Thermic effect of glucose in man: obligatory and facultative thermogenesis. J Clin Invest. 1984;74(5):1572–1580. doi: 10.1172/JCI111573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jacobs I, Martineau L, Vallerand A.L. Thermoregulatory thermogenesis in humans during cold. Exerc Sport Sci Rev. 1994:221–250. [PubMed] [Google Scholar]
- 32.Jequier E. Thermogenesis and its role in energy metabolism. Biblthca Nutrition Dietetica. 1986;39:6–12. [PubMed] [Google Scholar]
- 33.Tappy L, Jequier E. Fructose and dietary thermogenesis. Am J Clin Nutr. 1993;58(5 suppl):766S–770S. doi: 10.1093/ajcn/58.5.766S. [DOI] [PubMed] [Google Scholar]
- 34.Tappy L, Randin JP, Felber JP, Chiolero R, Simonson D.C, Jequier E, et al. Comparison of thermogenic effect of fructose and glucose in normal humans. Am J Physiol. 1986;250(6 pt 1):E718–E724. doi: 10.1152/ajpendo.1986.250.6.E718. [DOI] [PubMed] [Google Scholar]
- 35.Nadel E.R. Temperature regulation and prolonged exercise. In: Lamb D.R, Murray R, editors. Perspectives in Exercise Science and Sports Medicine: Prolonged Exercise. Vol. 1988. Carmel, IN: Benchmark Press; pp. 125–151. [Google Scholar]