Abstract
Context
The emergency department has been described as a promising setting to initiate interventions with assault-injured youth to reduce the risk of re-injury and reactive perpetration. Efforts to intervene have received little study.
Objective
To assess the impact of a mentor-implemented violence prevention intervention on reducing aggression, fighting and re-injury among assault-injured youth.
Design
Randomized controlled trial
Setting
Two large urban hospital emergency departments
Participants
Youth age 10–15 presenting with peer assault injury were recruited and randomly assigned to intervention and comparison groups.
Intervention
Intervention youth received a mentor who implemented a 6 session problem-solving curriculum while parents received 3 home visits with a health educator to discuss family needs and facilitate service use and parental monitoring. The comparison group received a list of community resources with 2 follow-up phone calls to facilitate service use.
Main Outcome Measures
Youth and parents were interviewed at baseline and 6 months to assess attitudes about violence, risk factors, fighting and repeat injury.
Results
227 families were recruited with 23% refusing participation and 4% partial interview completion. 166 families were enrolled with 87 randomized to the intervention group and 79 in the comparison group; 118 (71%) completed both youth and parent follow-up interviews and 113 had usable data. Intervention and comparison groups were not significantly different at baseline on demographics or risk factors except for increased knife carrying and less deviant peers in the intervention group. After adjustment for baseline differences, there was a trend toward significant program effect including reducing misdemeanor activity (rate ratio 0.29, confidence interval 0.08–0.98), youth-reported aggression scores (rate ratio .63, 0.4–1.00) and increasing youth self efficacy (beta=2.28, p<.05). Program impact was associated with number of intervention sessions received.
Conclusions
A community-based, mentor-implemented program with assault-injured youth presenting to the ED trended in the direction of decreased violence with reduced misdemeanors and increased self efficacy. The ED may be an important contact location, and injuries an important context, for augmenting self efficacy for violence prevention.
Keywords: Adolescent health, emergency department, fighting, injury prevention and control, youth violence
INTRODUCTION
Violent injury is a major cause of morbidity and mortality among adolescents. In the United States, homicide is the fourth leading cause of death among 10–14 year olds and the second leading cause of death among 15–24 year olds.1 For African-Americans, homicide ranks third for 10–14 year olds and is the leading cause of death among 15–24 year olds. Youth violence often manifests as peer assault injury presenting to the emergency department (ED). In urban communities like Washington, DC, interpersonal intentional injuries account for 25% of all adolescent injuries, 45% of hospitalizations and 85% of injury deaths.2 Nonfatal violence is a major risk factor for subsequent assault injury and often precedes fatal violence.3,4,5,6 One population-based analysis found that assault victims experience recurrent injury risk 88 times that of unexposed individuals.7 Recurrent intentional injury rates have been reported up to 44% in selected populations, leading some to characterize urban trauma as a chronic disease.8
The 2004 National Institutes of Health State-of-the-Science Conference on Preventing Youth Violence suggested that trauma centers may be important settings to initiate youth violence prevention interventions.9 Some have posited that the ED visit may be a “teachable moment,” a time of introspection and vulnerability following an injury event, and may be an opportune time to intervene with assault-injured youth to reduce violence. The American Academy of Pediatrics has advocated a system of identification, assessment, and treatment of the physical and psychosocial needs of assault victims to reduce the risk of re-injury and reactive perpetration.10 However, there have been few studies of ED interventions addressing youth violence to test this approach. Brief interventions in the ED have proven effective in addressing risky behaviors such as smoking11 and substance use,12,13,14 and in injury prevention with adolescents on seatbelt and bike helmet use.15 The few studies addressing violence have involved older youth and adults and have had mixed results suggesting the need for more intensive intervention with younger adolescents.16,17,18,19
The Centers for Disease Control and Prevention (CDC) “Best Practices of Youth Violence Prevention: A Sourcebook for Community Action” has comprehensively reviewed studies evaluating youth violence prevention programs.20 Interventions were categorized and assessed according to target methodology and scientifically-demonstrated efficacy. The CDC concluded that there are four strategies that offer the best hope for prevention including 1) parent and family based programs, 2) early childhood home visitation, 3) social-cognitive interventions with youth, and 4) mentoring strategies. Multi-level and multi-component interventions incorporating these strategies are needed.
We developed a violence prevention intervention targeting assault-injured youth presenting to the ED and incorporating components of the four CDC best practice strategies including a social cognitive theory framework. We conducted a randomized trial of this intervention to 1) assess the receptiveness of families to violence prevention interventions initiated after an assault injury, and 2) assess the effectiveness of a mentor-implemented youth intervention with parent involvement on reducing risk factors for injury.
METHODS
Subjects
A consecutive sample of youth presenting to two urban EDs for assault injury were identified for a randomized trial of a community-based intervention. Eligibility criteria included: adolescents age 10–15 presenting to either a large urban children’s hospital or urban university hospital; residence in the DC-Baltimore metropolitan area; ED presentation with an interpersonal assault injuries (E960, 961–966, 968–969) excluding sexual assault, child abuse, sibling fights, or legal intervention; and mental, physical, and English-speaking ability of parent and child to participate in the intervention and assessments. Families were recruited over the time period of August 2001 to August 2004. The study protocol was approved by the Institutional Review Board at the two hospitals and the National Institute of Child Health and Human Development.
Study Procedures
We identified eligible youth that presented to the ED for assault injury. Cases were identified from ED logs or chart copies and computer print-outs of hospitalized patients. Research assistants recruited families in the ED, hospital ward or by phone. If eligible, parent informed consent and youth assent were obtained and youth and parents were then independently interviewed during a home visit as soon as possible after the ED visit. Interviews consisted of two components: a verbal response component and an audiotape ("Walkman") component. For the audiotape component, subjects listened to questions asked on the Walkman and wrote numeric answers on an answer sheet that did not have the printed questions.
Opaque, sealed envelopes were prepared with random assignment to one of the two groups. Interviewers opened the envelope with the family after completion of the baseline survey. Follow-up assessments were conducted 6 months later by a research assistant. Efforts were made to ensure that this interviewer was blind to group assignment. Families were compensated for completion of baseline ($20)or 6 month assessment ($30). Retention efforts included periodic phone contacts and mailings, reminders to families to contact study staff if they moved, and home visits to families we were unable to reach.
Intervention and Comparison Conditions
Assault-injured youth in the intervention received a mentor who met with them at least six times over the ensuing 2–6 months. Mentors were recruited from a partnering community mentoring organization and from employees at the participating institutions. Eligible mentors were age 21–50 years of age, had a history of working with youth, had no criminal history on their background check and negative drug screen. Mentors were gender-matched to youth with most matched to only one youth during the study. Mentors received extensive training on mentoring youth and on the project curriculum including role playing regarding adolescent communication and conflict scenarios. Mentors were supervised by program staff through regular telephone contacts, monitoring of mentor logs, feedback from the parent and youth, and occasional observation and retraining sessions. Mentors received a small stipend for their time and activity expenses ($240 total).The mentor picked up youth at their home and spent time with them in an activity at their home or in the community. During these visits the mentor and youth completed a six session violence prevention curriculum focusing on skills-building. The curriculum was grounded in social cognitive theory and included sessions on conflict management and “hot buttons,” problem-solving, weapon safety, decision-making and goal setting. The curriculum also included interactive activities, role playing scenarios and a pledge to remain non-violent. Mentors were supervised by project staff through occasional observation and retraining sessions, monitoring of mentor logs and feedback from the parent and child.
Parents of youth in the intervention received three home visits by a health educator. Health educators had master degrees in public health or psychology and were employees of the project. The parent curriculum included sessions reviewing topics covered in the youth curriculum and sessions on parental monitoring and involvement adapted from the Adolescent Transitions Program (ATP) curriculum.21,22
Youth and parents in both the intervention and comparison groups were asked about services they have used and their current service needs in the baseline assessment. Families in both groups received case management services including discussion of sequelae of assault injury, assessment of family needs and facilitated service use. Intervention group participants received this service through the health educator while comparison group participants received 2 calls by phone. Referrals were made to mental health treatment, medical services, addiction treatment, anger management programs, recreational and after school programs, legal aid, tutoring programs and other social services as requested by the family. Participants in both study groups received usual care from clinicians in the ED as well as a list of community resources.
Measures
Outcomes included attitudes and self efficacy regarding violence (attitude about interpersonal violence, attitudes about retaliation, social competence, and self efficacy) and risk factors for violence (number of fights, fight injuries, weapon carrying, misdemeanor problem behavior, friend behavior and aggression). The interview was based primarily on previously published measures. All questions and items included in these analyses were collected at both baseline and 6 month assessments. All scales and indices were coded such that an increased score indicated more of that behavior or trait, that is, an increased score on problem behavior indicated youth reported more frequently engaging in those behaviors, and an increase in self efficacy indicated that youth perceived themselves as more efficacious than someone with a lower score. When scale scores were derived, missing items were replaced by the individual’s mean of non-missing scale items. If the missing items were more than 20% of the component items, the scale was considered as missing.
Youth assessments included questions on demographics, attitudes and self efficacy and risk factors for violence. Youth attitudes toward interpersonal violence were assessed using 6 items from Slaby’s Attitude about Interpersonal Violence Scale (alpha =0.65 baseline, 0.66 follow-up).23,24 Youth also responded to the 8 item retaliation subscale of Perception of Environmental Violence Scale (alpha=0.78 at both baseline and follow-up).25,26 Social competence was assessed using 8 items about problem solving, communication, and peer pressure resistance (alpha=.70 baseline, .75 follow-up).27 A 11-item scale assessed conflict avoidance self efficacy and was modified from a previously validated self efficacy scale (alpha=0.89 baseline, 0.86 follow-up).25 Questions asked how much youth agreed or disagreed that they could use tools to avoid arguments of fights including “thinking about the consequences before I act,” or “taking a time out when I start to get upset.”
Regarding risk factors for violence, youth were queried on how many times in the last thirty days they had been in fights, fights with injury, and had carried a knife (YRBS, Middle school version).28 Misdemeanors were assessed by the sum of 2 items on how many days of the last 30 days youth engaged in damaging property and stealing from a store.25 Youth reported on their friends’ problem behaviors by answering how many days of the last 30 days they hung out with friends “who get you in trouble, use drugs or alcohol, carry a weapon, start fights” and “who you were not supposed to.” Youth physical aggression over the past 30 days was measured using an index based on the fighting subscale of the Modified Aggression Scale.29,30,22 The original scale was expanded to include location (school, home, and neighborhood). A total physical aggression score was computed based on the 12 items (4 behaviors at each location) and used in these analyses. Parents completed the 20 item aggression subscale of the Child Behavior Checklist (alpha = .97).31
To ensure the assessments targeted relevant constructs and were effective with this population, development of the interview included 16 initial focus groups with adolescents on injury and violence,32 review of the literature on adolescent injury, and adaptation of models on adolescent risk-taking behavior.33,34,35 The interview instrument underwent rigorous one-on-one pretesting including in-depth interviews probing how respondents understood and interpreted the study questions. This was followed by pilot testing the study process and completion of the interview under study conditions.
Data Analysis
Analyses were conducted using SAS software (version 9.1, Cary, NC). Descriptive analyses were performed to assess demographics and outcome measures at baseline and at 6 month follow-up. All of the indices of problem and aggressive behavior were heavily skewed toward zero, therefore each was dichotomized such that 0 equaled none/never, and 1 equaled one or more time/days for the purpose of prevalence description. As appropriate pertaining to the type of variable, rate ratios and linear regression coefficients were calculated to examine the difference in outcomes of interest between the intervention and comparison groups. Analyses were performed for outcomes at 6 month follow-up while controlling for participant’s age, gender and baseline/pre-treatment outcome variable. The analyses were conducted according to treatment group assignment at randomization regardless of participants’ adherence to the assigned intervention sessions. Those assigned to the intervention group who failed to start or complete the intervention were included in the analysis. We did not impute outcome data for those lost to follow-up. The adherence level analyses were based on the number of sessions a family actually received, as assessed by number of mentor visits with youth and health educator visits with parents. Those who received six mentor visits with youth and three health educator visits with parents were considered the high adherence group. Those who did not complete the full intervention were considered the low adherence group.
Logistic regression was used to compare demographics between intervention and comparison groups at baseline. Odds ratios and its associated 95% confidence intervals (CI) were calculated. Because certain discrete outcomes were highly skewed and had zero inflated counts (many count responses were zero), negative binomial regression was applied to model these count variables: number of fight injuries, fights, knife carrying, misdemeanor activity, problem behavior of friend and the aggression scores. Given that the outcomes are number of event counts during the 6 month period post intervention, the regression coefficients from the negative binomial regression can be interpreted as the logarithm of the ratios of event rates between intervention and comparison groups. Standard linear regression was applied to model attitude scores, social competence, self efficacy and CBCL aggression subscales.
Due to the varying time to follow-up (6–18 months), a sensitivity analysis using only those people who had follow-up within a year was conducted yielding no differences in results. The study had 75% power with 95% confidence to detect a half standard deviation difference in number of fights and almost 80% power to detect a half standard deviation difference in self-efficacy in two-tailed tests.
RESULTS
Recruitment and Participation
Figure 1 presents the study recruitment yield and follow-up at 6 months. Of the 227 eligible patients where consent was attempted, 23% refused. Of those consenting, 166 completed parent and youth baseline interviews with 4% completing partial interviews. The 166 complete baseline interviews were randomized to the intervention and comparison groups. At six month follow-up, 71% were interviewed, 58 in the intervention group and 60 in the comparison group. Five participants were excluded either because of multiple extreme outlier responses on outcome variables or partial interview.
Figure 1.
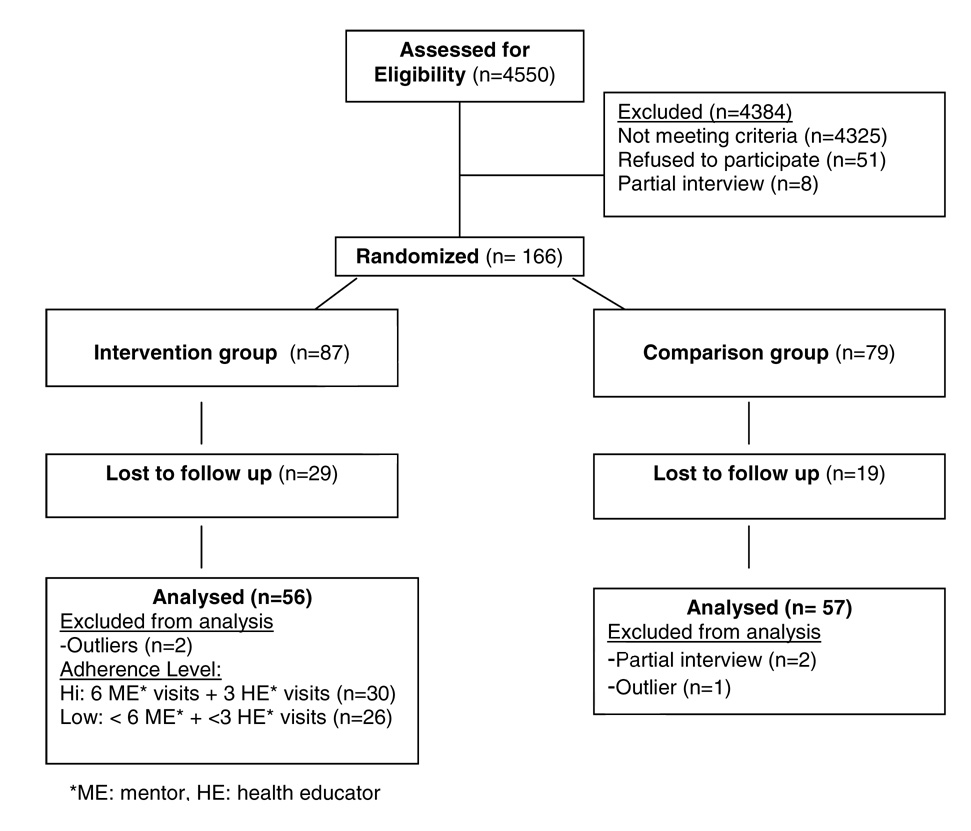
Take Charge! Youth Violence Prevention Project Recruitment Yield
Of the 113 participants in the analysis, the mean age was 13.0 (median = 13; SD=1.41) and 12.9 (median=13; SD=1.55) for the intervention and comparison groups and 66% and 67% of youth were males respectively. There was no difference between intervention and comparison groups on age, gender, race, maternal education, family income or time between discharge from the emergency department and enrollment. The median time between discharge and completion of both parent and youth interview was 51 days. The mean number of months to follow up assessment for both intervention and comparison groups was 8 months. Time to follow-up assessment was not significantly different between intervention (8.6 months) and comparison (7.6 months) groups (p=0.13). There was no difference in demographics or baseline outcome variables between those who completed assessments and those who were lost to follow-up.
Baseline Characteristics
Table 1 shows that the intervention and comparison groups were comparable at baseline on most demographic variables and risk factors for injury. At baseline, fighting behavior was common in both groups of youth with over half having had a fight in the last 30 days. However, the intervention group had a higher rate of knife carrying and less friends with problem behavior compared to the comparison group. Baseline differences were controlled for in assessment of intervention effect.
Table 1.
Outcome measures of 113 youth by intervention status at baseline and 6 month follow-up
| Percentage of Youth Reporting Ever (≥ 1) on Behavior | ||||
|---|---|---|---|---|
| Baseline | 6 Month Follow-Up | |||
| Comparison | Intervention | Comparison | Intervention | |
| Outcome Behaviors | N=57 | N=56 | N=57 | N=56 |
| # fight injuries past 30 days | 46.4 | 48.2 | 7.8 | 5.7 |
| # fights past 30 days | 55.4 | 53.7 | 33.9 | 32.1 |
| Carry a knife past 30 days | 19.6 | 23.6 | 17.9 | 23.5 |
| Misdemeanor – sum | 33.9 | 23.2 | 23.6 | 11.5 |
| Friend problem behavior – sum | 67.9 | 35.7 | 52.7 | 44.2 |
| Aggression Score Total | 86.0 | 92.9 | 87.7 | 87.5 |
| Mean Score | ||||
| Baseline | 6 Month Follow-Up | |||
| Comparison | Intervention | Comparison | Intervention | |
| Outcome Scales | N=57 | N=56 | N=57 | N=56 |
| Attitude about interpersonal violence | 18.3 | 17.7 | 18.1 | 18.1 |
| Attitudes toward retaliation | 19.5 | 18.0 | 19.4 | 18.9 |
| Social competence | 23.4 | 22.8 | 23.4 | 23.3 |
| Conflict Avoidance Self Efficacy | 34.1 | 34.4 | 34.2 | 36.6 |
| CBCL Aggression subscale, parent report1 | 16.6 | 15.3 | 17.1 | 15.1 |
= Child Behavior Checklist
Program Impact
Of the 56 families in the intervention group analysis, most (N=30; 54%) received the full intervention with six mentor visits with youth and three health educator visits with parents (high adherence group). Those who did not complete the full intervention were considered the low adherence intervention group. Intervention youth and parents reported high levels of satisfaction with the intervention. The vast majority of youth respondents agreed that “my mentor understands my needs” (94%) and “cares about me” (89%). Parents were asked how well the health educator understood their needs and/or concerns with 88% of respondents stating the health educator understood them “very well”. When asked “How satisfied were you with the services that the health educator provided?” 73% were very satisfied.
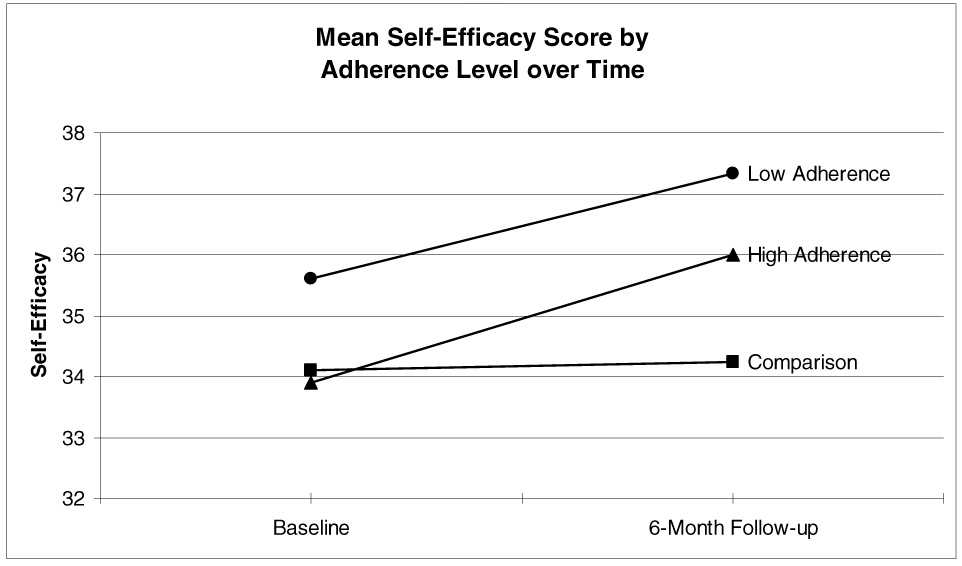
As seen in Table 2, after adjustment for baseline group differences, there was significant program effect reducing misdemeanor activity (rate ratio=0.29, CI 0.08–0.98) and increasing youth general self efficacy (beta=2.28, p<.05). Program impact varied by number of intervention sessions completed as demonstrated in Figure 2 and Figure 3. When comparing the low adherence group to the comparison group, only self efficacy was significantly improved in the intervention group (beta=2.66, p<.05). When comparing the high adherence group to the comparison group, greater program impact was seen with decreased physical aggression score (rate ratio=.51, CI 0.29–0.90) and decreased misdemeanor activity (rate ratio=.09, CI 0.01–0.63). Figure 2 demonstrates that the comparison group had increased aggression over time, but the intervention moderated this effect. The prevalence of fighting in the last 30 days did decrease in both groups over time.
Table 2.
Overall intervention effect and adherence level effect at 6 month follow-up: unadjusted and adjusted Rate Ratios and Beta values, controlling for baseline value, age and gender
| Intervention Impact |
Adherence Level Analysis |
|||||||
|---|---|---|---|---|---|---|---|---|
| Comparison (N=57) Mean | Intervention (N=56) Mean | Intervention versus Comparison at Follow-up | Low Adherence versus Comparison N=26 | High Adherence versus Comparison N=30 | ||||
| Negative Binomial Regression | ||||||||
| Outcome Behaviors | Adj. RR | 95%CI | Adj. RR | 95%CI | Adj. RR | 95%CI | ||
| # fight injuries past 30 days | 0.14 | 0.08 | 0.58 | 0.09,3.94 | 1.24 | 0.13,11.92 | 0.22 | 0.01,3.34 |
| # fights past 30 days | 1.61 | 0.78 | 0.76 | 0.29,2.00 | 0.55 | 0.16,1.85 | 1.00 | 0.31,3.25 |
| Carry a knife past 30 days | 1.04 | 1.61 | 0.70 | 0.16,2.96 | 0.51 | 0.08,3.21 | 0.90 | 0.15,5.38 |
| Misdemeanor – sum | 0.85 | 0.24 | 0.29 * | 0.08,0.98 | 0.52 | 0.12,2.19 | 0.09 * | 0.01,0.63 |
| Friend behavior – sum | 6.78 | 6.34 | 1.51 | 0.64,3.58 | 1.12 | 0.37,3.42 | 1.80 | 0.67,4.82 |
| Aggression Score Total | 21.8 | 14.6 | 0.63 | 0.40,1.00 | 0.76 | 0.43,1.36 | 0.51 * | 0.29,0.90 |
| Linear Regression | ||||||||
| Outcome Scales | Beta | Beta | Beta | |||||
| Attitude about interpersonal violence | 18.1 | 18.1 | 0.22 | −0.35 | 0.75 | |||
| Attitudes toward retaliation | 19.4 | 18.9 | 0.43 | 0.79 | 0.11 | |||
| Social competence | 23.4 | 23.3 | 0.17 | 0.43 | −0.04 | |||
| Conflict Avoidance Self efficacy | 34.2 | 36.6 | 2.28 * | 2.66 * | 2.01 | |||
| CBCL Aggression subscale, parent report1 | 17.1 | 15.1 | −0.98 | −0.73 | −1.20 | |||
p-value <0.05
= Child Behavior Checklist
Figure 2.
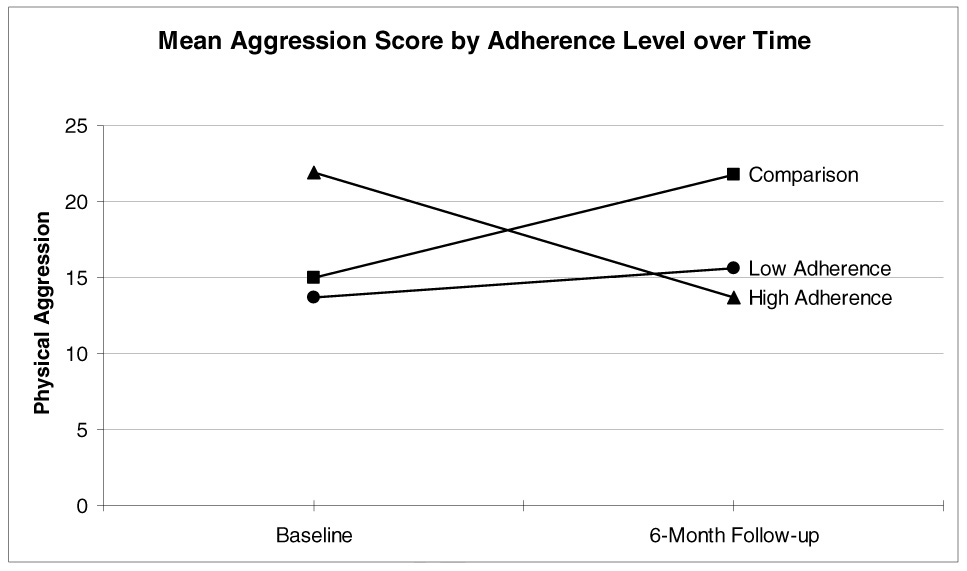
Figure 3.
A rate ratio of 0.76 for 30-day report of fighting at follow-up translates into an additional 24% reduction (38.6 fights per 100 persons, CI 0.29–2.00) in the mean 30-day report of fights for those in the intervention group compared to the control group, controlling for baseline number of fights. Regarding fight injuries, the additional reduction for those in the intervention group was 42% (5.9 fight injuries per 100 persons, CI 0.09–3.94).
COMMENT
This study found that assault-injured youth and their families were receptive to violence prevention intervention initiated after an ED visit. The study also found that intervention may reduce aggression and problem behavior and increase self efficacy. Literature suggests that these youth are at high risk for repeated visits and injury,5 have significant psychosocial needs,36,37 and are less likely to have advised follow-up after ED treatment.38 The ED may be an important access point to these high risk youth and provides an opportunity to intervene. When these participants were asked, “How likely is it that [you/your child] may have another physical fight with the same people who caused [your/his/her] injury?” 28% of youth and 36% of parents stated this was somewhat or very likely.39 Previous studies have found that many youth assault injuries are related to long-standing, repeated disagreements that may not be over after an ED visit.40 Retaliatory feelings may fuel violence.41,42 Interrupting the cycle of reactive perpetration and traumatic re-injury could reduce the burden of injury among adolescents.
Though there has been a call to address the psychosocial needs of assault-injured youth presenting to the ED, there has been limited evaluation of this approach. ED protocols and programs have been developed, but few have published outcomes. Zun and colleagues tested an ED case management model with assault-injured individuals age 10–24 and found some increased social service utilization but no change in attitudes, delinquency or return visits to the ED.43,44,45 With follow-up at 6 and 12 months they found a reduction in self-reported reinjury rate in the intervention group but no program impact on arrests, incarceration or state-reported re-injuries via the trauma registry. They concluded that there was need for a more intensive intervention with a younger population and over a longer time period. Our study suggested that focusing on a younger population and using a family approach offers promise.
Based on enrollment into the study and reported satisfaction with the intervention, families were receptive to violence prevention intervention after assault injury. There were trends toward differences between intervention and comparison groups on youth-reported aggression, misdemeanor problem behavior and self efficacy at 6 months. This study did not find significant impact of the intervention on youth reports of fighting and weapons carrying in the last 30 days, nor on parent report of youth aggression. No differences were found for other intervention targets, including social competence and attitudes about retaliation. However, study power was limited and all outcomes trended in the direction of decreased risk for violence. In addition, in adherence level analysis there was an adherence response association between treatment group and youth-reported outcomes. Our analyses addressed program effectiveness, not efficacy. Overall program impact was likely diminished because some intervention families did not start or complete all sessions, however, these families were included in analyses if follow-up assessment was completed. Also, the comparison group received limited case management services beyond what was usual care from the participating EDs and this minimal intervention may have been beneficial. This would have reduced our ability to detect effects and may partially account for the decrease in fighting in both groups at 6 months.
Our intervention incorporated components of CDC’s Best Practices in Youth Violence Prevention including a mentoring relationship with youth, home visitation, involvement of parents and a social cognitive approach. It is difficult to know which component had the greatest impact or whether the combination of strategies accounted for youth change. However, study staff felt that the relationship-based mentoring aspect of the intervention was powerful and youth and parents were very positive about their mentors. The presence of a positive trusted adult role model has been recognized as a protective factor against violence and other maladaptive outcomes among youth. Studies have found that mentoring can significantly improve academic achievement, school attendance, reduce violent behavior and drug use, and improve family and peer relationships.46,47,48 Mentoring program evaluations have found that more frequent mentoring contacts, knowing families and longer mentoring relationships are associated with better outcomes.45 Though there was a trend toward program impact at follow-up, it is not known if effects would be sustained since some mentoring relationships did not continue after completion of the curriculum. Finding a supply of reliable and committed mentors was a challenge in this study and in other mentoring programs.45 Further study of mentoring models that go beyond the traditional one-on-one method and utilizes other means of contact (e.g. group mentoring, instant messaging, phone contact) and targeted efforts to high risk populations are needed.
Limitations of this study include concern regarding generalizability, validity of data, study recruitment and attrition, and limited power. The study was conducted in two high-risk communities and results may not be generalizable to other regions. The validity of self-report data is a persistent concern in behavioral research. Additionally, because of the limited number of validated measures in the field at the time, the need to adapt measures was another potential limitation. However, during pre-testing we found that participants’ responses had face validity and internal consistency.
It is possible that there existed bias in convenience sampling and nonparticipation. Despite our best efforts, only 71% of families completed follow-up assessments further limiting power to show a difference. The varying time to follow-up past six months is also of concern but might be expected to underestimate program effect. Those who did and did not complete follow-up did not differ with regard to baseline demographics or violence risk factors. Recognizing that many families were very mobile and had complex and difficult family circumstances made this research especially challenging, however, the refusal rate and attrition in our study were similar to other studies of assault-injured youth.17 Our refusal rate of 23% was also consistent with school-based violence prevention studies with high risk middle schoolers in the Multisite Violence Prevention Study (participation rate 55–80%).49 These high risk populations of assault-injured youth deserve support and study and we present lessons learned. Finally, despite limited study power and a comparison group that received some intervention, we were able to identify trends of an effect of the intervention.
This study is one of the first studies evaluating a violence prevention intervention with assault-injured youth presenting to the ED. We found that a community-based, mentor-implemented program with assault-injured youth presenting to the ED demonstrated trends toward reduced aggression scores and misdemeanors and increased self efficacy. Further, the ED may be an important contact location, and injuries an important context, for augmenting self efficacy for violence prevention.
Implications
Despite the call 12 years ago by the American Academy of Pediatrics to intervene with assault victims in emergency departments, there has been a paucity of research. This study demonstrates the promise of intervention with this population. Additional research is needed to corroborate associations found and to further explore the potential of social cognitive and mentoring approaches to youth violence prevention. Research should also focus on engagement of high risk populations, cost-effectiveness, and use of administrative databases (e.g. juvenile justice records) for additional measures and participant tracking.50
Acknowledgments
Funding:
This project was supported by the Maternal and Child Health Bureau (Title V Social Security Act), Health Resources and Services Administration, Department of Health and Human Services, R40MC00174, 4H34MC00025, and the DC-Baltimore Research Center on Child Health Disparities Grant Number P20 MD00165 from the National Center on Minority Health and Health Disparities. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the funding agency. The funders did not have a role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review or approval of the manuscript.
Footnotes
Conflict of Interest:
None. Authors do not have any affiliation, financial agreement, or other involvement with any company whose product figures prominently in the submitted manuscript.
Randomized Trial: Clinicaltrials.gov identifier: NCT00444197
References
- 1.Centers for Disease Comparison and Prevention. [Accessed February 20, 2007];Web-based Injury Statistics Query and Reporting System (WISQARS) http://webappa.cdc.gov/cgi-bin/broker.exe.
- 2.Cheng TL, Wright JL, Fields CB, et al. Violent injuries among adolescents: declining morbidity & mortality in an urban population. Ann Emerg Med. 2001;37:292–300. doi: 10.1067/mem.2001.111763. [DOI] [PubMed] [Google Scholar]
- 3.Luckenbill DF. Criminal homicide as a situated transaction. Social Problems. 1977;25:176–186. [Google Scholar]
- 4.Moeller TG. Youth aggression and violence: A psychological approach. Mahwah, NJ: Lawrence Erlbaum Associates; 2001. [Google Scholar]
- 5.Cheng TL, Schwarz D, Brenner R, et al. Adolescent assault injury: risk & protective factors and locations of contact for intervention: A matched case-control study. Pediatrics. 2003;112(4):931–938. doi: 10.1542/peds.112.4.931. [DOI] [PubMed] [Google Scholar]
- 6.Redeker N, Smeltzer S, Kirkpatrick J, Parchment S. Risk factors of adolescent and young adult trauma victims. Am J Crit Care. 1995;4(5):370–378. [PubMed] [Google Scholar]
- 7.Dowd MD. Consequences of violence. Premature death, violence recidivism, and violent criminality. Pediatr Clin North Am. 1998;45(2):333–340. doi: 10.1016/s0031-3955(05)70009-2. [DOI] [PubMed] [Google Scholar]
- 8.Buss TF, Abdu R. Repeat victims of violence in an urban trauma center. Violence Vict. 1995;10(3):183–194. [PubMed] [Google Scholar]
- 9.National Institutes of Health State-of-the-Science Conference Statement: Preventing Violence and Related Health-Risking Social Behaviors in Adolescents: an NIH State-of-the-Science Conference; October 13–15, 2004; http://consensus.nih.gov/2004/2004YouthViolencePreventionSOS023html.htm. [DOI] [PubMed] [Google Scholar]
- 10.Task Force on Adolescent Assault Victim Needs. American Academy of Pediatrics. Adolescent assault victim needs: a review of issues and a model protocol. Pediatrics. 1996;98:991–1001. [PubMed] [Google Scholar]
- 11.Bernstein SL, Becker BM. Preventive care in the ED: diagnosis and management of smoking and smoking-related illness in the ED: a systematic review. Acad Emerg Med. 2002 Jul;9(7):720–729. doi: 10.1111/j.1553-2712.2002.tb02153.x. [DOI] [PubMed] [Google Scholar]
- 12.Bazargan-Hejazi S, Bing E, Bazargan M, et al. Evaluation of a brief intervention in an inner-city ED. Ann Emerg Med. 2005 Jul;46(1):67–76. doi: 10.1016/j.annemergmed.2004.10.014. [DOI] [PubMed] [Google Scholar]
- 13.Dinh-Zarr T, Goss C, Heitman E, Roberts I, DiGuiseppi C. Interventions for preventing injuries in problem drinkers. Cochrane Database Syst Rev. 2004;(3):CD001857. doi: 10.1002/14651858.CD001857.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.D'Onofrio G, Degutis LC. Preventive care in the ED: screening and brief intervention for alcohol problems in the ED: a systematic review. Acad Emerg Med. 2002 Jun;9(6):627–638. doi: 10.1111/j.1553-2712.2002.tb02304.x. [DOI] [PubMed] [Google Scholar]
- 15.Johnston BD, Rivara FP, Droesch RM, Dunn C, Copass MK. Behavior change counseling in the emergency department to reduce injury risk: a randomized, comparison led trial. Pediatrics. 2002 Aug;110(2 Pt 1):267–274. doi: 10.1542/peds.110.2.267. [DOI] [PubMed] [Google Scholar]
- 16.De Vos E, Stone DA, Goetz MA, Dahlberg LL. Evaluation of a hospital-based youth violence intervention. Am J Prev Med. 1996;12:101–108. [PubMed] [Google Scholar]
- 17.Zun LS, Downey L, Rosen J. The effectiveness of an ED-based violence prevention program. Am J Emerg Med. 2006;24:8–13. doi: 10.1016/j.ajem.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 18.Becker MG, Hall JS, Ursic CM, Jain S, Calhoun D. Caught in the crossfire: the effects o a peer-based intervention program vor violently injured youth. J Adolesc Health. 2004;34:177–183. doi: 10.1016/j.jadohealth.2003.04.001. [DOI] [PubMed] [Google Scholar]
- 19.Cheng TL, Wright JL, Markakis D, Copeland-Linder N, Menvielle E. Randomized trial of a case management program for assault-injured youth: Impact on service utilization and risk for reinjury. Pediatr Emerg Care. 2008;24 doi: 10.1097/PEC.0b013e3181666f72. in press. [DOI] [PubMed] [Google Scholar]
- 20.Thornton TN, Craft CA, Dahlberg LL, Lynch BS, Baer K. Best Practices of Youth Violence Prevention: A Sourcebook for Community Action. Atlanta: Centers for Disease Comparison and Prevention, National Center for Injury Prevention and Comparison; 2002. [Google Scholar]
- 21.Dishion TJ, Kavanagh K. Intervening in adolescent problem behavior: A family-centered approach. New York: Guilford; 2003. [Google Scholar]
- 22.Adolescent Transitions Program. Child and Family Center, University of Oregon; [accessed February 26, 2007]. http://cfc.uoregon.edu/atp.htm. [Google Scholar]
- 23.Slaby RG, Guerra NG. Cognitive mediators of aggression in adolescent offenders: Assessment. Developmental Psychology. 1988;24(4):580–588. [Google Scholar]
- 24.Dahlberg LL, Toal SB, Behrens CB. Measuring Violence-Related Attitudes, Beliefs, and Behaviors Among Youths: A Compendium of Assessment Tools. Atlanta GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 1998. [Google Scholar]
- 25.Hill HM, Madere S. Exposure to violence and African American children: A multidimensional model of risks and resources. J Comm Psychology. 1996;24:26–43. [Google Scholar]
- 26.Hill HM, Noblin V. Children’s Perceptions of Environmental Violence. Washington, DC: Howard University; 1991. [Google Scholar]
- 27.Simons-Morton B, Crump A, Haynie D, Saylor KE, Eitel P, Yu K. Psychosocial, school, and parent factors associated with recent smoking among early adolescent boys and girls. Preventive Medicine. 1999;28:138–148. doi: 10.1006/pmed.1998.0404. [DOI] [PubMed] [Google Scholar]
- 28.Whalen LG, Grunbaum JA, Kinchen S, McManus T, Shanklin SL, Kann L. Centers for Disease Control and Prevention. [Accessed February 26, 2007];US Department of Health and Human Services 2005; Middle School Youth Risk Behavior Survey 2003. http://www.cdc.gov/healthyyouth/yrbs/middleschool2003/pdf/fullreport.pdf.
- 29.Orpinas P. Skills Training and social influences for violence prevention in middle schools, a curriculm evaluation. Doctoral Dissertation. Houston TX: University of Texas Health Science Center at Houston School of Public Health; 1993. [Google Scholar]
- 30.Bosworth K, Espelage D. Teen Conflict Survey. Bloomington, IN: Center for Adolescent Studies, Indiana University; 1995. (Unpublished) [Google Scholar]
- 31.Achenbach TM. Manual for the Child Behavior Checklist 2/3 and 1992 profile. Burlington: University of Vermont, Department of Psychiatry; 1992. [Google Scholar]
- 32.Johnson SB, Frattaroli S, Wright JL, Fields CB, Ricardo I, Cheng TL. Urban youths’ perspectives on violence and the necessity of fighting. Injury Prevention. 2004;10:287–291. doi: 10.1136/ip.2004.005793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jessor R, Jessor Sl. Problem Behavior and Psychosocial Development: A Longitudinal Study of Youth. New York: Academic Press; 1977. [Google Scholar]
- 34.Office of the Surgeon General. [Accessed June 19, 2002];Youth Violence: A Report of the Surgeon General. Released January 17, 2001. www.surgeongeneral.gov/library/youthviolence/report.html. [PubMed]
- 35.Irwin CE, Cataldo MF, Matheny AP, Peterson L. Health consequences of behaviors: injury as a model. Pediatrics. 1992;90:798–807. [PubMed] [Google Scholar]
- 36.Zun LS, Rosen J. Psychosocial needs of young persons who are victims of interpersonal violence. Pediatr Emerg Care. 2003;19:15–19. doi: 10.1097/00006565-200302000-00004. [DOI] [PubMed] [Google Scholar]
- 37.McCart MR, Davies WH, Phielps LF, Heuermann W, Melzer-Lange MD. Pediatr Emerg Care. 2006;22:154–159. doi: 10.1097/01.pec.0000202453.42108.f1. [DOI] [PubMed] [Google Scholar]
- 38.Melzer-Lange M, Lye PS, Calhoun AD. Advised follow-up after emergency treatment of adolescents with violence-related injuries. Pediatr Emerg Care. 1998;14:334–336. [PubMed] [Google Scholar]
- 39.Johnson SB, Bradshaw CP, Wright JL, Haynie DL, Simons-Morton BG, Cheng TL. Preliminary validation of the teachable moment construct among assault-injured youth and their parents". Pediatr Emerg Care. doi: 10.1097/PEC.0b013e31812c6687. In Press. [DOI] [PubMed] [Google Scholar]
- 40.Cheng TL, Johnson SB, Wright JL, Brenner RA, Scheidt PA. Assault-injured adolescents presenting to the ED: Causes and Circumstances. Acad Emerg Med. 2006;13:610–616. doi: 10.1197/j.aem.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 41.Rich J, Stone D. The experience of violent injury for young African-American men: the meaning of being a "sucker". J Gen Intern Med. 1996;11(2):77–82. doi: 10.1007/BF02599582. [DOI] [PubMed] [Google Scholar]
- 42.Johnson SB, Frattaroli S, Wright JL, Fields CB, Cheng TL. Urban youths' perspectives on violence and the necessity of fighting. Inj Prevention. 2004;10(5):287–291. doi: 10.1136/ip.2004.005793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zun LS, Downey L, Rosen J. Violence prevention in the ED: linkage of the ED to a social service agency. Am J Emerg Med. 2003;21:454–457. doi: 10.1016/s0735-6757(03)00102-5. [DOI] [PubMed] [Google Scholar]
- 44.Zun LS, Downey L, Rosen J. An ED-based program to change attitudes of youth toward violence. J Emerg Med. 2004;2:247–241. doi: 10.1016/j.jemermed.2003.06.008. [DOI] [PubMed] [Google Scholar]
- 45.Mitka M. Hospital study offers hope of changing lives prone to violence. JAMA. 2002;287:576–577. [PubMed] [Google Scholar]
- 46.Furano K, Roaf PA, Styles MB, Branch AY. Big Brothers/Big Sisters: A Study of Program Practice. Philadelphia: Public/Private Ventures; 1993. [Google Scholar]
- 47.Jekielek SM, Moore KA, Hair EC, Scarupa HJ. Mentoring: A promising strategy for youth development. [Accessed February 26, 2007];Child Trends Research Brief. 2002 February; http://12.109.133.224/Files/MentoringBrief2002.pdf.
- 48.Sheehan K, DiCara JA, LeBailly S, Christoffel KK. Adapting the gang model: peer mentoring for violence prevention. Pediatrics. 1999;104:50–54. doi: 10.1542/peds.104.1.50. [DOI] [PubMed] [Google Scholar]
- 49.Miller-Johnson S, Sullivan TN, Simon TR. Multisite Violence Prevention Project. Evaluating the impact of interventions in the Multisite Violence Prevention Study. Am J Preventive Med. 2004;26(1S):48–61. doi: 10.1016/j.amepre.2003.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Romero EG, Teplin LA, McClelland GM, Abram KM, Welty LJ, Washburn JJ. A longitudinal study of the prevalence, development, and persistence of HIV/Sexually transmitted infection risk behaviors in delinquent youth: implications for health care in the community. Pediatrics. 2007;119:e1126–e1141. doi: 10.1542/peds.2006-0128. [DOI] [PMC free article] [PubMed] [Google Scholar]


