Abstract
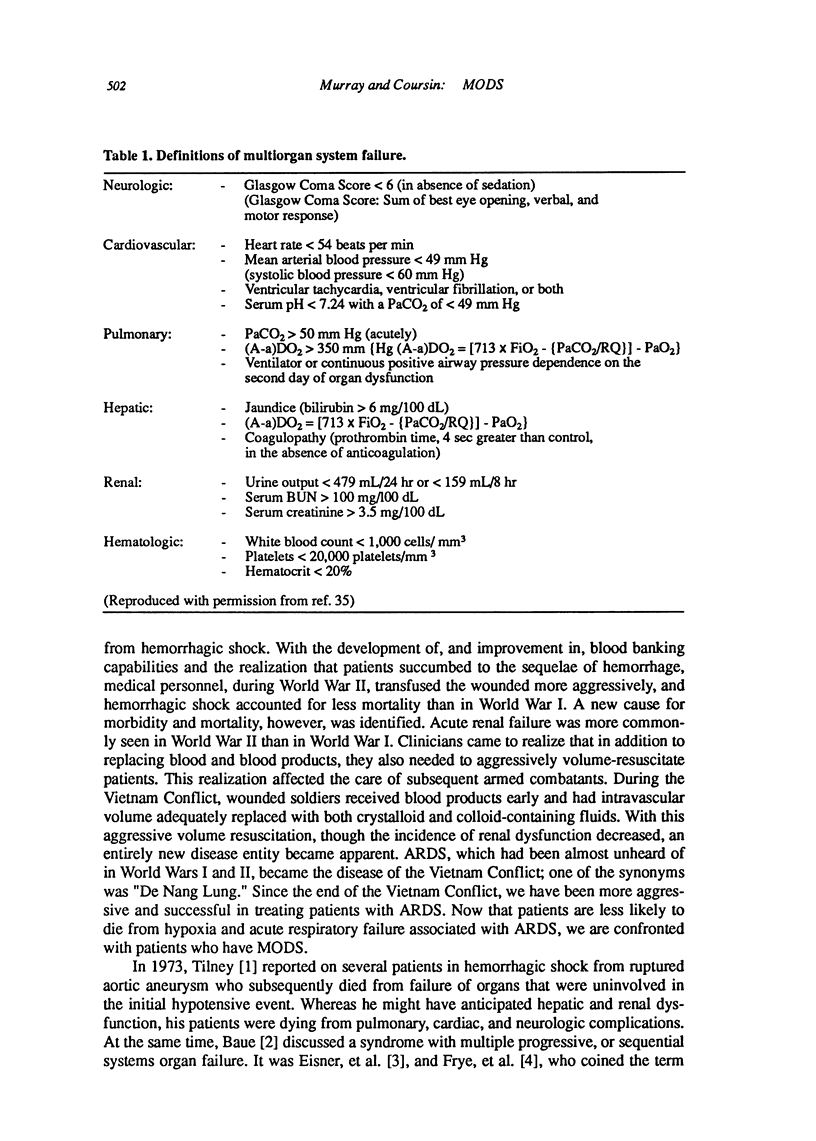
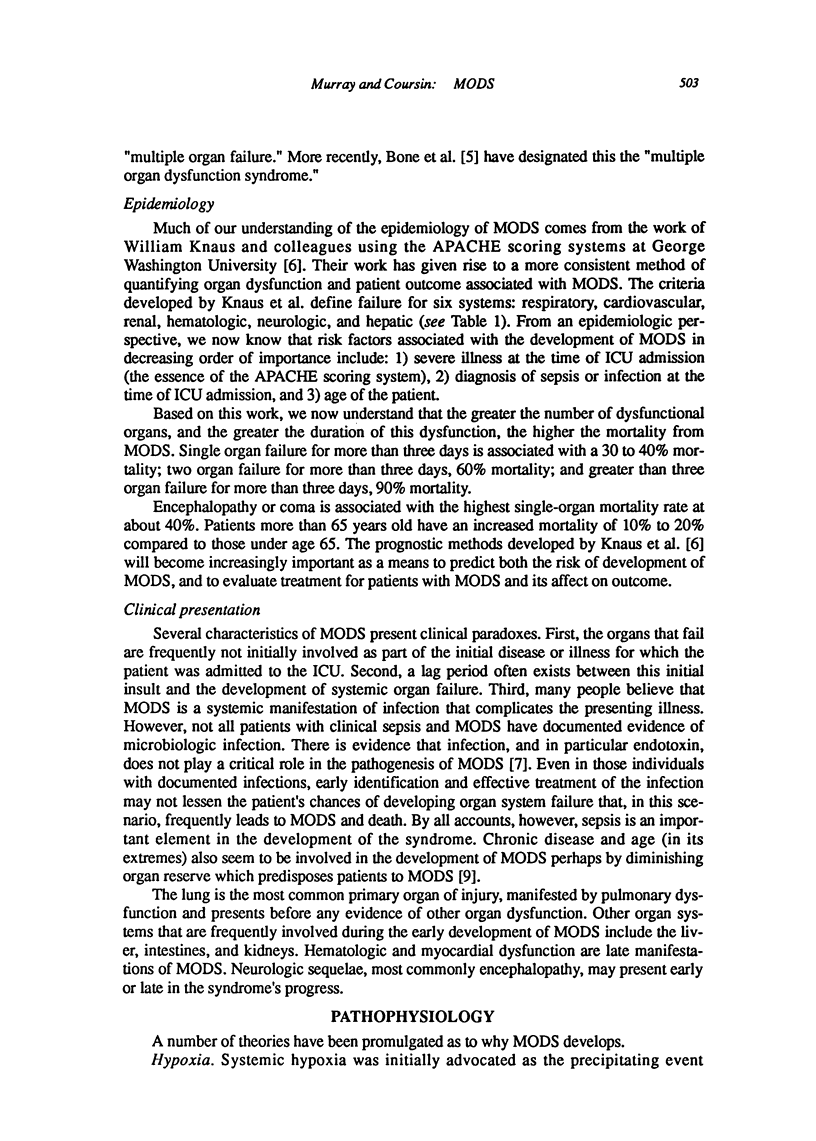
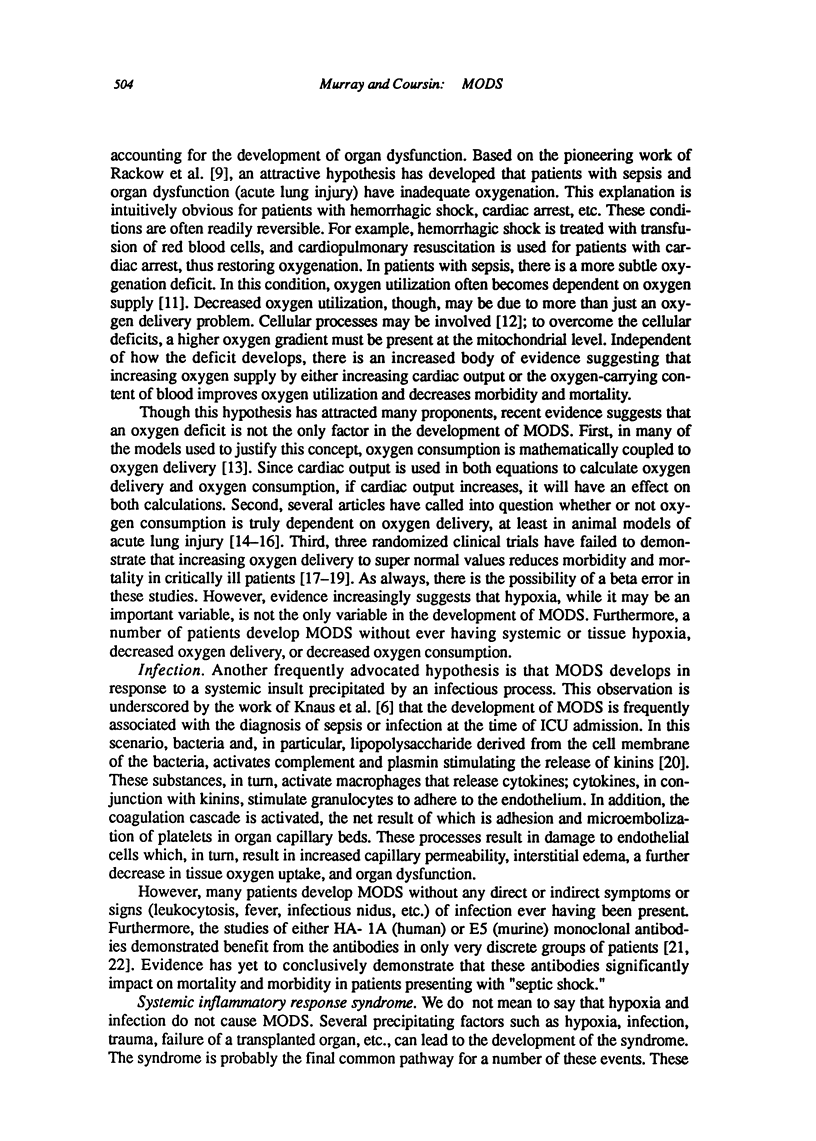
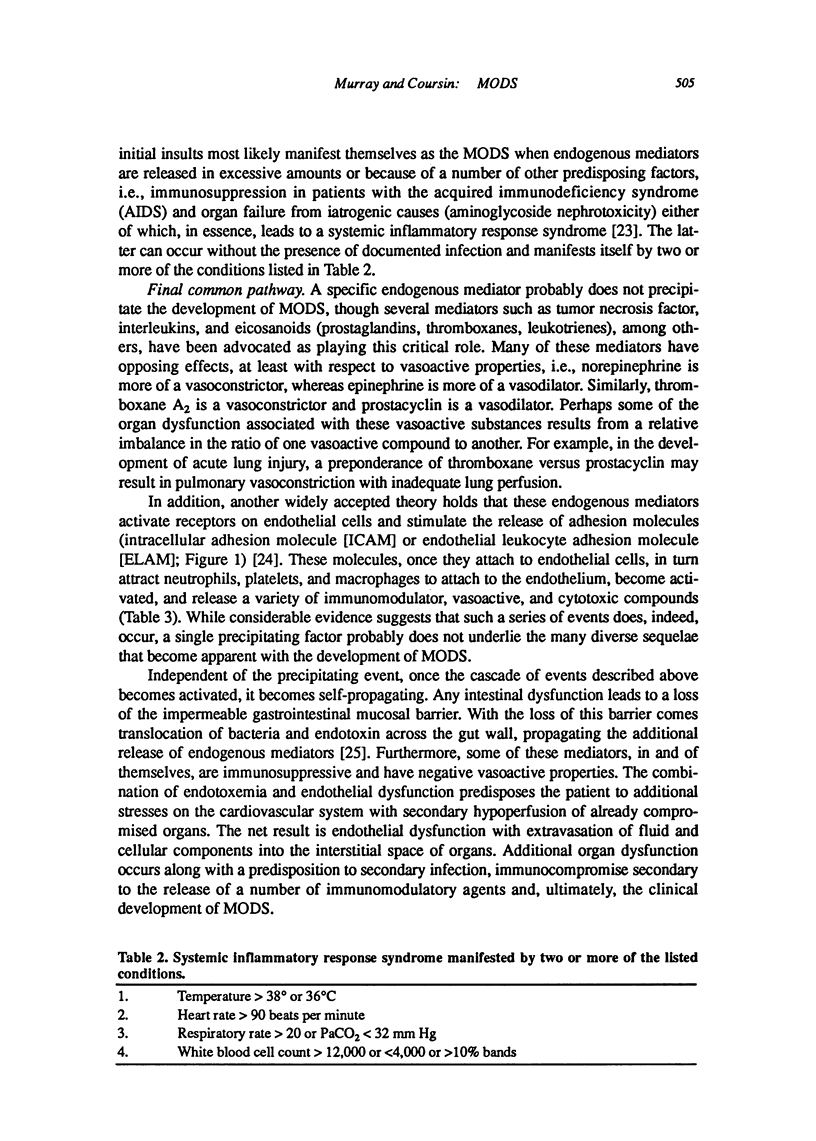
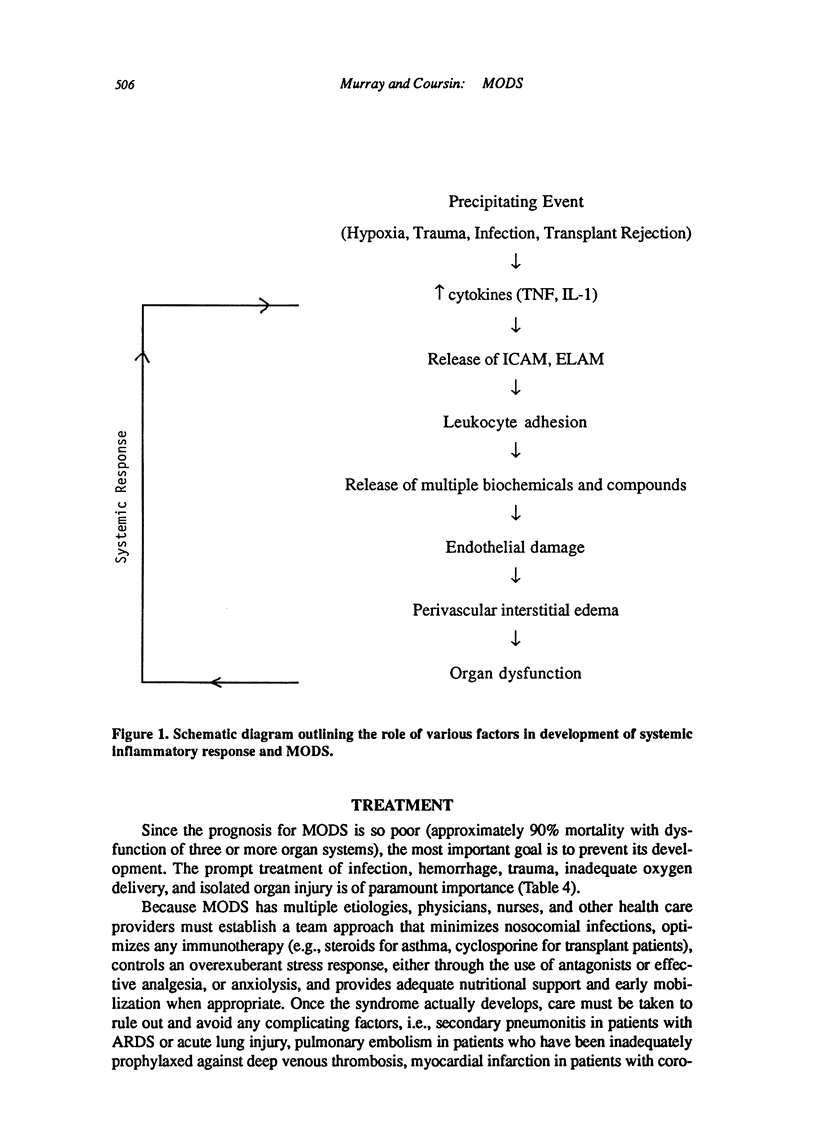
The multiple organ dysfunction syndrome (MODS), though newly described, has manifested itself in intensive care unit (ICU) patients for several decades. As the name implies, it is a syndrome in which more than one organ system fails. Failure of these multiple organ systems may or may not be related to the initial injury or disease process for which the patient was admitted to the ICU. MODS is the leading cause of morbidity and mortality in current ICU practice. While the pathophysiology of MODS is not completely known, much evidence indicates that, during the initial injury which precipitates ICU admission, a chain of events is initiated which results in activation of several endogenous metabolic pathways. These pathways release compounds which, in and of themselves, are usually cytoprotective. However, an over exuberant activation of these endogenous systems results in an inflammatory response which can lead to development of failure in distant organs. As these organs fail, they activate and propagate the systemic inflammatory response. No therapy has proven entirely efficacious at modulating this inflammatory response and the incidence and severity of MODS. In current ICU practice, treatment is focused on prevention and treating individual organ dysfunction as it develops. With increased understanding of the pathophysiology of MODS therapy will come newer modalities which inhibit or interfere with the propagation of the endogenous systemic inflammatory response. These newer therapies hold great promise and already some are undergoing clinical investigation.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med. 1992 Jun;20(6):864–874. [PubMed] [Google Scholar]
- Archie J. P., Jr Mathematic coupling of data: a common source of error. Ann Surg. 1981 Mar;193(3):296–303. doi: 10.1097/00000658-198103000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Astiz M. E., Rackow E. C., Falk J. L., Kaufman B. S., Weil M. H. Oxygen delivery and consumption in patients with hyperdynamic septic shock. Crit Care Med. 1987 Jan;15(1):26–28. doi: 10.1097/00003246-198701000-00005. [DOI] [PubMed] [Google Scholar]
- Baue A. E. Multiple, progressive, or sequential systems failure. A syndrome of the 1970s. Arch Surg. 1975 Jul;110(7):779–781. doi: 10.1001/archsurg.1975.01360130011001. [DOI] [PubMed] [Google Scholar]
- Baue A. E. The role of the gut in the development of multiple organ dysfunction in cardiothoracic patients. Ann Thorac Surg. 1993 Apr;55(4):822–829. doi: 10.1016/0003-4975(93)90098-3. [DOI] [PubMed] [Google Scholar]
- Bone R. C., Sibbald W. J., Sprung C. L. The ACCP-SCCM consensus conference on sepsis and organ failure. Chest. 1992 Jun;101(6):1481–1483. doi: 10.1378/chest.101.6.1481. [DOI] [PubMed] [Google Scholar]
- Bone R. C., Slotman G., Maunder R., Silverman H., Hyers T. M., Kerstein M. D., Ursprung J. J. Randomized double-blind, multicenter study of prostaglandin E1 in patients with the adult respiratory distress syndrome. Prostaglandin E1 Study Group. Chest. 1989 Jul;96(1):114–119. doi: 10.1378/chest.96.1.114. [DOI] [PubMed] [Google Scholar]
- Carlile P. V., Gray B. A. Effect of opposite changes in cardiac output and arterial PO2 on the relationship between mixed venous PO2 and oxygen transport. Am Rev Respir Dis. 1989 Oct;140(4):891–898. doi: 10.1164/ajrccm/140.4.891. [DOI] [PubMed] [Google Scholar]
- Cerra F. B., Lehmann S., Konstantinides N., Dzik J., Fish J., Konstantinides F., LiCari J. J., Holman R. T. Improvement in immune function in ICU patients by enteral nutrition supplemented with arginine, RNA, and menhaden oil is independent of nitrogen balance. Nutrition. 1991 May-Jun;7(3):193–199. [PubMed] [Google Scholar]
- Cockerill F. R., 3rd, Muller S. R., Anhalt J. P., Marsh H. M., Farnell M. B., Mucha P., Gillespie D. J., Ilstrup D. M., Larson-Keller J. J., Thompson R. L. Prevention of infection in critically ill patients by selective decontamination of the digestive tract. Ann Intern Med. 1992 Oct 1;117(7):545–553. doi: 10.7326/0003-4819-117-7-545. [DOI] [PubMed] [Google Scholar]
- Duff J. H., Groves A. C., McLean A. P., LaPointe R., MacLean L. D. Defective oxygen consumption in septic shock. Surg Gynecol Obstet. 1969 May;128(5):1051–1060. [PubMed] [Google Scholar]
- Eiseman B., Beart R., Norton L. Multiple organ failure. Surg Gynecol Obstet. 1977 Mar;144(3):323–326. [PubMed] [Google Scholar]
- Engelberts I., Samyo S. K., Leeuwenberg J. F., van der Linden C. J., Buurman W. A. A role for ELAM-1 in the pathogenesis of MOF during septic shock. J Surg Res. 1992 Aug;53(2):136–144. doi: 10.1016/0022-4804(92)90025-u. [DOI] [PubMed] [Google Scholar]
- Fry D. E., Pearlstein L., Fulton R. L., Polk H. C., Jr Multiple system organ failure. The role of uncontrolled infection. Arch Surg. 1980 Feb;115(2):136–140. doi: 10.1001/archsurg.1980.01380020006003. [DOI] [PubMed] [Google Scholar]
- Greenman R. L., Schein R. M., Martin M. A., Wenzel R. P., MacIntyre N. R., Emmanuel G., Chmel H., Kohler R. B., McCarthy M., Plouffe J. A controlled clinical trial of E5 murine monoclonal IgM antibody to endotoxin in the treatment of gram-negative sepsis. The XOMA Sepsis Study Group. JAMA. 1991 Aug 28;266(8):1097–1102. [PubMed] [Google Scholar]
- Gutierrez G., Palizas F., Doglio G., Wainsztein N., Gallesio A., Pacin J., Dubin A., Schiavi E., Jorge M., Pusajo J. Gastric intramucosal pH as a therapeutic index of tissue oxygenation in critically ill patients. Lancet. 1992 Jan 25;339(8787):195–199. doi: 10.1016/0140-6736(92)90002-k. [DOI] [PubMed] [Google Scholar]
- Halushka P. V., Wise W. C., Cook J. A. Protective effects of aspirin in endotoxic shock. J Pharmacol Exp Ther. 1981 Aug;218(2):464–469. [PubMed] [Google Scholar]
- Hinshaw L. B., Solomon L. A., Freeny P. C., Reins D. A. Endotoxin shock. Hemodynamic and survival effects of methylprednisolone. Arch Surg. 1967 Jan;94(1):61–66. doi: 10.1001/archsurg.1967.01330070063014. [DOI] [PubMed] [Google Scholar]
- Holaday J. W., Faden A. I. Naloxone reversal of endotoxin hypotension suggests role of endorphins in shock. Nature. 1978 Oct 5;275(5679):450–451. doi: 10.1038/275450a0. [DOI] [PubMed] [Google Scholar]
- Inoue S., Epstein M. D., Alexander J. W., Trocki O., Jacobs P., Gura P. Prevention of yeast translocation across the gut by a single enteral feeding after burn injury. JPEN J Parenter Enteral Nutr. 1989 Nov-Dec;13(6):565–571. doi: 10.1177/0148607189013006565. [DOI] [PubMed] [Google Scholar]
- Kaufman B. S., Rackow E. C., Falk J. L. The relationship between oxygen delivery and consumption during fluid resuscitation of hypovolemic and septic shock. Chest. 1984 Mar;85(3):336–340. doi: 10.1378/chest.85.3.336. [DOI] [PubMed] [Google Scholar]
- Knaus W. A., Wagner D. P., Draper E. A., Zimmerman J. E., Bergner M., Bastos P. G., Sirio C. A., Murphy D. J., Lotring T., Damiano A. The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest. 1991 Dec;100(6):1619–1636. doi: 10.1378/chest.100.6.1619. [DOI] [PubMed] [Google Scholar]
- Knaus W. A., Wagner D. P. Multiple systems organ failure: epidemiology and prognosis. Crit Care Clin. 1989 Apr;5(2):221–232. [PubMed] [Google Scholar]
- Register S. D., Downs J. B., Stock M. C., Kirby R. R. Is 50% oxygen harmful? Crit Care Med. 1987 Jun;15(6):598–601. doi: 10.1097/00003246-198706000-00012. [DOI] [PubMed] [Google Scholar]
- Ronco J. J., Fenwick J. C., Wiggs B. R., Phang P. T., Russell J. A., Tweeddale M. G. Oxygen consumption is independent of increases in oxygen delivery by dobutamine in septic patients who have normal or increased plasma lactate. Am Rev Respir Dis. 1993 Jan;147(1):25–31. doi: 10.1164/ajrccm/147.1.25. [DOI] [PubMed] [Google Scholar]
- Ronco J. J., Phang P. T., Walley K. R., Wiggs B., Fenwick J. C., Russell J. A. Oxygen consumption is independent of changes in oxygen delivery in severe adult respiratory distress syndrome. Am Rev Respir Dis. 1991 Jun;143(6):1267–1273. doi: 10.1164/ajrccm/143.6.1267. [DOI] [PubMed] [Google Scholar]
- Shoemaker W. C., Appel P. L., Kram H. B. Hemodynamic and oxygen transport responses in survivors and nonsurvivors of high-risk surgery. Crit Care Med. 1993 Jul;21(7):977–990. doi: 10.1097/00003246-199307000-00010. [DOI] [PubMed] [Google Scholar]
- Tilney N. L., Bailey G. L., Morgan A. P. Sequential system failure after rupture of abdominal aortic aneurysms: an unsolved problem in postoperative care. Ann Surg. 1973 Aug;178(2):117–122. doi: 10.1097/00000658-197308000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran D. D., Groeneveld A. B., van der Meulen J., Nauta J. J., Strack van Schijndel R. J., Thijs L. G. Age, chronic disease, sepsis, organ system failure, and mortality in a medical intensive care unit. Crit Care Med. 1990 May;18(5):474–479. doi: 10.1097/00003246-199005000-00002. [DOI] [PubMed] [Google Scholar]
- Tsuno K., Prato P., Kolobow T. Acute lung injury from mechanical ventilation at moderately high airway pressures. J Appl Physiol (1985) 1990 Sep;69(3):956–961. doi: 10.1152/jappl.1990.69.3.956. [DOI] [PubMed] [Google Scholar]
- Tuchschmidt J., Fried J., Astiz M., Rackow E. Elevation of cardiac output and oxygen delivery improves outcome in septic shock. Chest. 1992 Jul;102(1):216–220. doi: 10.1378/chest.102.1.216. [DOI] [PubMed] [Google Scholar]
- Ziegler E. J., Fisher C. J., Jr, Sprung C. L., Straube R. C., Sadoff J. C., Foulke G. E., Wortel C. H., Fink M. P., Dellinger R. P., Teng N. N. Treatment of gram-negative bacteremia and septic shock with HA-1A human monoclonal antibody against endotoxin. A randomized, double-blind, placebo-controlled trial. The HA-1A Sepsis Study Group. N Engl J Med. 1991 Feb 14;324(7):429–436. doi: 10.1056/NEJM199102143240701. [DOI] [PubMed] [Google Scholar]


